Mechanical Performance of Extensive Restorations Made with Short Fiber-Reinforced Composites without Coverage: A Systematic Review of In Vitro Studies
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
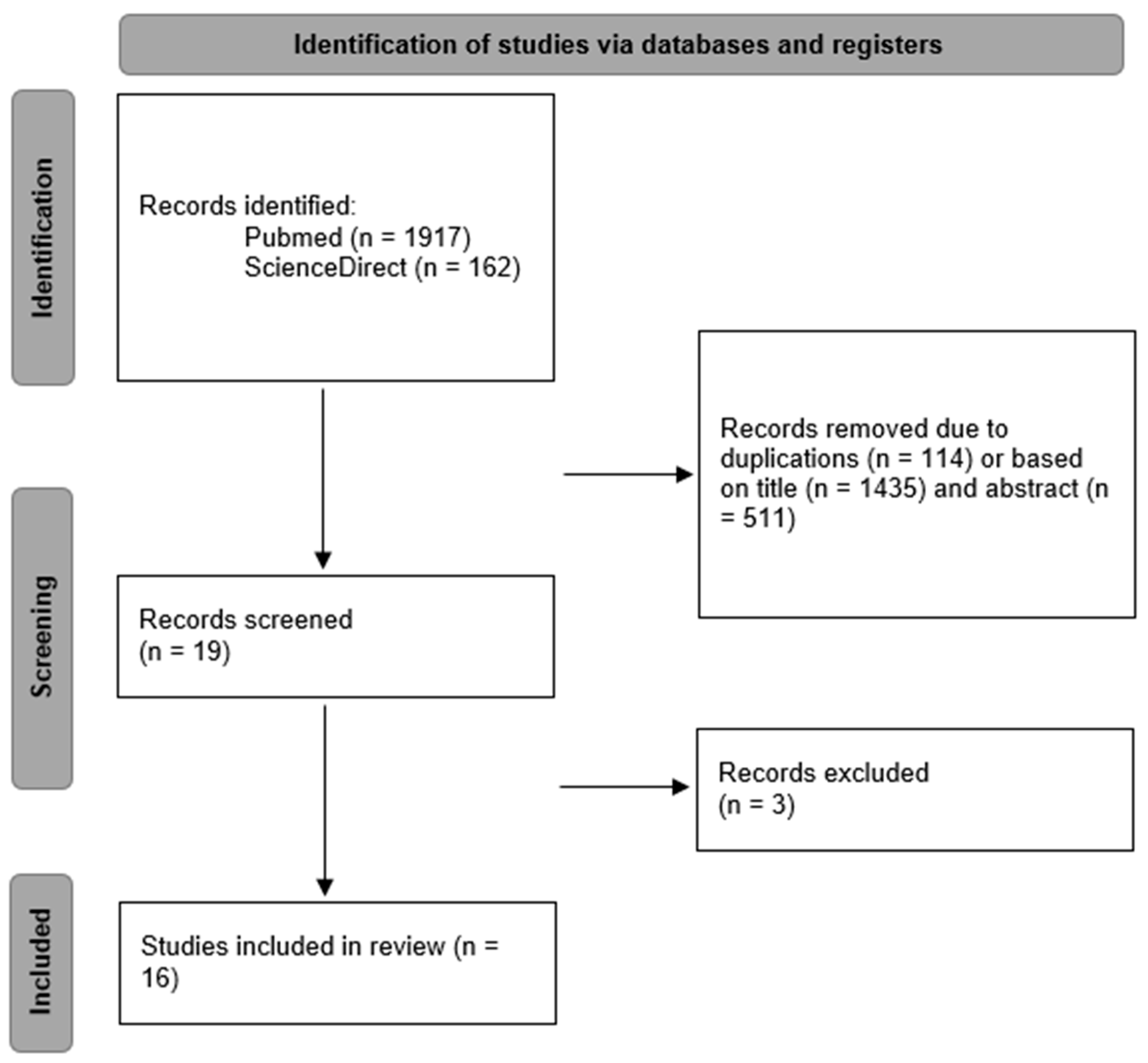
2.2. Study Screening and Selection
2.3. Eligibility Criteria
2.4. Data Synthesis
2.5. Quality Assessment
3. Results
3.1. Quality Assessment of the Included In Vitro Trials
3.2. Quantitative Assessment of the Included Publications
4. Discussion
4.1. Fracture Resistance
4.2. Fracture Pattern
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bonilla, E.D.; Hayashi, M.; Pameijer, C.H.; Le, N.V.; Morrow, B.R.; Garcia-Godoy, F. The Effect of Two Composite Placement Techniques on Fracture Resistance of MOD Restorations with Various Resin Composites. J. Dent. 2020, 101, 103348. [Google Scholar] [CrossRef]
- Haak, R.; Näke, T.; Park, K.-J.; Ziebolz, D.; Krause, F.; Schneider, H. Internal and Marginal Adaptation of High-Viscosity Bulk-Fill Composites in Class II Cavities Placed with Different Adhesive Strategies. Odontology 2019, 107, 374–382. [Google Scholar] [CrossRef]
- Valizadeh, S.; Ranjbar Omrani, L.; Deliperi, S.; Sadeghi Mahounak, F. Restoration of a Nonvital Tooth with Fiber Reinforce Composite (Wallpapering Technique). Case Rep. Dent. 2020, 2020, 9619787. [Google Scholar] [CrossRef]
- Gaeta, C.; Marruganti, C.; Mignosa, E.; Franciosi, G.; Ferrari, E.; Grandini, S. Influence of Methodological Variables on Fracture Strength Tests Results of Premolars with Different Number of Residual Walls. A Systematic Review with Meta-Analysis. Dent. J. 2021, 9, 146. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.; Bhuva, B.; Bose, R. Present Status and Future Directions: Vertical Root Fractures in Root Filled Teeth. Int. Endod. J. 2022, 55, 804–826. [Google Scholar] [CrossRef] [PubMed]
- Daher, R.; Ardu, S.; Di Bella, E.; Rocca, G.T.; Feilzer, A.J.; Krejci, I. Fracture Strength of Non-Invasively Reinforced MOD Cavities on Endodontically Treated Teeth. Odontology 2021, 109, 368–375. [Google Scholar] [CrossRef]
- Magne, P.; Carvalho, M.A.; Milani, T. Shrinkage-Induced Cuspal Deformation and Strength of Three Different Short Fiber-Reinforced Composite Resins. J. Esthet. Restor. Dent. 2023, 35, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Magne, P.; Milani, T. Short-Fiber Reinforced MOD Restorations of Molars with Severely Undermined Cusps. J. Adhes. Dent. 2023, 25, 99–106. [Google Scholar] [CrossRef] [PubMed]
- Sidhu, P.; Sultan, O.S.; Math, S.Y.; Malik, N.A.; Wilson, N.H.F.; Lynch, C.D.; Blum, I.R.; Daood, U. Current and Future Trends in the Teaching of Direct Posterior Resin Composites in Malaysian Dental Schools: A Cross-Sectional Study. J. Dent. 2021, 110, 103683. [Google Scholar] [CrossRef] [PubMed]
- European Society of Endodontology developed by:; Mannocci, F.; Bhuva, B.; Roig, M.; Zarow, M.; Bitter, K. European Society of Endodontology Position Statement: The Restoration of Root Filled Teeth. Int. Endod. J. 2021, 54, 1974–1981. [Google Scholar] [CrossRef]
- Sadr, A.; Bakhtiari, B.; Hayashi, J.; Luong, M.N.; Chen, Y.-W.; Chyz, G.; Chan, D.; Tagami, J. Effects of Fiber Reinforcement on Adaptation and Bond Strength of a Bulk-Fill Composite in Deep Preparations. Dent. Mater. 2020, 36, 527–534. [Google Scholar] [CrossRef]
- Lempel, E.; Szebeni, D.; Őri, Z.; Kiss, T.; Szalma, J.; Lovász, B.V.; Kunsági-Máté, S.; Böddi, K. The Effect of High-Irradiance Rapid Polymerization on Degree of Conversion, Monomer Elution, Polymerization Shrinkage and Porosity of Bulk-Fill Resin Composites. Dent. Mater. 2023, 39, 442–453. [Google Scholar] [CrossRef]
- Tseng, P.-C.; Chuang, S.-F.; Kaisarly, D.; Kunzelmann, K.-H. Simulating the Shrinkage-Induced Interfacial Damage around Class I Composite Resin Restorations with Damage Mechanics. Dent. Mater. 2023, 39, 513–521. [Google Scholar] [CrossRef]
- Ohmori, K.; Tasaki, T.; Kimura, S.; Hori, A.; Sakaeda, N.; Hanabusa, M.; Yamamoto, T. Residual Polymerization Stresses in Human Premolars Generated with Class II Composite Restorations. J. Mech. Behav. Biomed. Mater. 2020, 104, 103643. [Google Scholar] [CrossRef]
- Tsertsidou, V.; Mourouzis, P.; Dionysopoulos, D.; Pandoleon, P.; Tolidis, K. Fracture Resistance of Class II MOD Cavities Restored by Direct and Indirect Techniques and Different Materials Combination. Polymers 2023, 15, 3413. [Google Scholar] [CrossRef]
- Lassila, L.; Keulemans, F.; Säilynoja, E.; Vallittu, P.K.; Garoushi, S. Mechanical Properties and Fracture Behavior of Flowable Fiber Reinforced Composite Restorations. Dent. Mater. 2018, 34, 598–606. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Silikas, N.; Watts, D.C. Polymerization and Shrinkage Kinetics and Fracture Toughness of Bulk-Fill Resin-Composites. Dent. Mater. 2022, 38, 1934–1941. [Google Scholar] [CrossRef]
- Fráter, M.; Sáry, T.; Jókai, B.; Braunitzer, G.; Säilynoja, E.; Vallittu, P.K.; Lassila, L.; Garoushi, S. Fatigue Behavior of Endodontically Treated Premolars Restored with Different Fiber-Reinforced Designs. Dent. Mater. 2021, 37, 391–402. [Google Scholar] [CrossRef] [PubMed]
- Heintze, S.D.; Ilie, N.; Hickel, R.; Reis, A.; Loguercio, A.; Rousson, V. Laboratory Mechanical Parameters of Composite Resins and Their Relation to Fractures and Wear in Clinical Trials—A Systematic Review. Dent. Mater. 2017, 33, e101–e114. [Google Scholar] [CrossRef] [PubMed]
- Escobar, L.B.; Pereira da Silva, L.; Manarte-Monteiro, P. Fracture Resistance of Fiber-Reinforced Composite Restorations: A Systematic Review and Meta-Analysis. Polymers 2023, 15, 3802. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Sheth, V.H.; Shah, N.P.; Jain, R.; Bhanushali, N.; Bhatnagar, V. Development and Validation of a Risk-of-Bias Tool for Assessing in Vitro Studies Conducted in Dentistry: The QUIN. J. Prosthet. Dent. 2022, S0022391322003456. [Google Scholar] [CrossRef] [PubMed]
- Garoushi, S.; Vallittu, P.K.; Lassila, L.V.J. Direct Restoration of Severely Damaged Incisors Using Short Fiber-Reinforced Composite Resin. J. Dent. 2007, 35, 731–736. [Google Scholar] [CrossRef] [PubMed]
- Bijelic, J.; Garoushi, S.; Vallittu, P.K.; Lassila, L.V.J. Short Fiber Reinforced Composite in Restoring Severely Damaged Incisors. Acta Odontol. Scand. 2013, 71, 1221–1231. [Google Scholar] [CrossRef] [PubMed]
- Garoushi, S.K.; Hatem, M.; Lassila, L.V.J.; Vallittu, P.K. The Effect of Short Fiber Composite Base on Microleakage and Load-Bearing Capacity of Posterior Restorations. Acta Biomater. Odontol. Scand. 2015, 1, 6–12. [Google Scholar] [CrossRef] [PubMed]
- Garoushi, S.; Akbaşak-Sungur, A.Ö.; Erkut, S.; Vallittu, P.K.; Uctasli, S.; Lassila, L. Evaluation of Fracture Behavior in Short Fiber-Reinforced Direct and Indirect Overlay Restorations. Clin. Oral Investig. 2023, 27, 5449–5458. [Google Scholar] [CrossRef] [PubMed]
- Lassila, L.; Säilynoja, E.; Prinssi, R.; Vallittu, P.K.; Garoushi, S. Fracture Behavior of Bi-Structure Fiber-Reinforced Composite Restorations. J. Mech. Behav. Biomed. Mater. 2020, 101, 103444. [Google Scholar] [CrossRef] [PubMed]
- Lassila, L.; Säilynoja, E.; Prinssi, R.; Vallittu, P.K.; Garoushi, S. Bilayered Composite Restoration: The Effect of Layer Thickness on Fracture Behavior. Biomater. Investig. Dent. 2020, 7, 80–85. [Google Scholar] [CrossRef]
- Bijelic, J. Fracture Load of Tooth Restored with Fiber Post and Experimental Short Fiber Composite. Open Dent. J. 2011, 5, 58–65. [Google Scholar] [CrossRef]
- Cekic-Nagas, I.; Egilmez, F.; Ergun, G.; Vallittu, P.K.; Lassila, L.V.J. Load-Bearing Capacity of Novel Resin-Based Fixed Dental Prosthesis Materials. Dent. Mater. J. 2018, 37, 49–58. [Google Scholar] [CrossRef]
- Garoushi, S.; Vallittu, P.K.; Lassila, L.V.J. Use of Short Fiber-Reinforced Composite with Semi-Interpenetrating Polymer Network Matrix in Fixed Partial Dentures. J. Dent. 2007, 35, 403–408. [Google Scholar] [CrossRef]
- Nagata, K.; Garoushi, S.K.; Vallittu, P.K.; Wakabayashi, N.; Takahashi, H.; Lassila, L.V.J. Fracture Behavior of Single-Structure Fiber-Reinforced Composite Restorations. Acta Biomater. Odontol. Scand. 2016, 2, 118–124. [Google Scholar] [CrossRef] [PubMed]
- Keulemans, F.; Lassila, L.V.J.; Garoushi, S.; Vallittu, P.K.; Kleverlaan, C.J.; Feilzer, A.J. The Influence of Framework Design on the Load-Bearing Capacity of Laboratory-Made Inlay-Retained Fibre-Reinforced Composite Fixed Dental Prostheses. J. Biomech. 2009, 42, 844–849. [Google Scholar] [CrossRef]
- Bijelic-Donova, J.; Garoushi, S.; Vallittu, P.K.; Lassila, L.V.J. Mechanical Properties, Fracture Resistance, and Fatigue Limits of Short Fiber Reinforced Dental Composite Resin. J. Prosthet. Dent. 2016, 115, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Garoushi, S.; Mangoush, E.; Vallittu, M.; Lassila, L. Short Fiber Reinforced Composite: A New Alternative for Direct Onlay Restorations. Open Dent. J. 2013, 7, 181–185. [Google Scholar] [CrossRef]
- Lassila, L.; Mangoush, E.; Vallittu, P.K.; Garoushi, S. Fracture Behavior of Discontinuous Fiber-Reinforced Composite Inlay-Retained Fixed Partial Denture before and after Fatigue Aging. J. Prosthodont. Res. 2023, 67, 271–277. [Google Scholar] [CrossRef]
- Mangoush, E. Influence of Short Fiber Reinforced Composites on Fracture Resistance of Single-Structure Restorations. Eur. J. Prosthodont. Restor. Dent. 2020, 189. [Google Scholar] [CrossRef]
- Lassila, L.; Haapsaari, A.; Vallittu, P.K.; Garoushi, S. Fracture Resistance of Anterior Crowns Reinforced by Short-Fiber Composite. Polymers 2022, 14, 1809. [Google Scholar] [CrossRef]
- Ferracane, J.L.; Lawson, N.C. Probing the Hierarchy of Evidence to Identify the Best Strategy for Placing Class II Dental Composite Restorations Using Current Materials. J. Esthet. Restor. Dent. 2021, 33, 39–50. [Google Scholar] [CrossRef]
- Hofsteenge, J.W.; Scholtanus, J.D.; Özcan, M.; Nolte, I.M.; Cune, M.S.; Gresnigt, M.M.M. Clinical Longevity of Extensive Direct Resin Composite Restorations after Amalgam Replacement with a Mean Follow-up of 15 Years. J. Dent. 2023, 130, 104409. [Google Scholar] [CrossRef]
- Magne, P.; Belser, U. Biomimetic Restorative Dentistry, 2nd ed.; Quintessence Publishing Co., Inc.: Batavia, IL, USA, 2021; ISBN 978-0-86715-572-3. [Google Scholar]
- Alshabib, A.; Jurado, C.A.; Tsujimoto, A. Short Fiber-Reinforced Resin-Based Composites (SFRCs); Current Status and Future Perspectives. Dent. Mater. J. 2022, 41, 647–654. [Google Scholar] [CrossRef]
- Fagundes, T.C.; Barata, T.J.E.; Carvalho, C.A.R.; Franco, E.B.; Van Dijken, J.W.V.; Navarro, M.F.L. Clinical Evaluation of Two Packable Posterior Composites. J. Am. Dent. Assoc. 2009, 140, 447–454. [Google Scholar] [CrossRef]
- Van Dijken, J.W.V.; Sunnegårdh-Grönberg, K. Fiber-Reinforced Packable Resin Composites in Class II Cavities. J. Dent. 2006, 34, 763–769. [Google Scholar] [CrossRef] [PubMed]
- Aram, A.; Hong, H.; Song, C.; Bass, M.; Platt, J.A.; Chutinan, S. Physical Properties and Clinical Performance of Short Fiber Reinforced Resin-Based Composite in Posterior Dentition: Systematic Review and Meta-Analysis. Oper. Dent. 2023, 48, E119–E136. [Google Scholar] [CrossRef] [PubMed]
- Lassila, L.; Säilynoja, E.; Prinssi, R.; Vallittu, P.; Garoushi, S. Characterization of a New Fiber-Reinforced Flowable Composite. Odontology 2019, 107, 342–352. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Garcia, F.C.P.; De Araújo, P.A.; Franco, E.B.; Mondelli, R.F.L. Wear Resistance of Packable Resin Composites after Simulated Toothbrushing Test. J Esthet Restor Dent 2004, 16, 303–314. [Google Scholar] [CrossRef] [PubMed]
- Garoushi, S.; Gargoum, A.; Vallittu, P.K.; Lassila, L. Short Fiber-Reinforced Composite Restorations: A Review of the Current Literature. J. Investig. Clin. Dent. 2018, 9, e12330. [Google Scholar] [CrossRef] [PubMed]
- Tiu, J.; Belli, R.; Lohbauer, U. Rising R-Curves in Particulate/Fiber-Reinforced Resin Composite Layered Systems. J. Mech. Behav. Biomed. Mater. 2020, 103, 103537. [Google Scholar] [CrossRef] [PubMed]
- Selvaraj, H.; Krithikadatta, J.; Shrivastava, D.; Onazi, M.A.A.; Algarni, H.A.; Munaga, S.; Hamza, M.O.; Saad Al-Fridy, T.; Teja, K.V.; Janani, K.; et al. Systematic Review Fracture Resistance of Endodontically Treated Posterior Teeth Restored with Fiber Reinforced Composites—A Systematic Review. BMC Oral Health 2023, 23, 566. [Google Scholar] [CrossRef]
- Scotti, N.; Coero Borga, F.A.; Alovisi, M.; Rota, R.; Pasqualini, D.; Berutti, E. Is Fracture Resistance of Endodontically Treated Mandibular Molars Restored with Indirect Onlay Composite Restorations Influenced by Fibre Post Insertion? J. Dent. 2012, 40, 814–820. [Google Scholar] [CrossRef] [PubMed]
- Soares, L.M.; Razaghy, M.; Magne, P. Optimization of Large MOD Restorations: Composite Resin Inlays vs. Short Fiber-Reinforced Direct Restorations. Dent. Mater. 2018, 34, 587–597. [Google Scholar] [CrossRef] [PubMed]
- Aregawi, W.A.; Fok, A.S.L. Shrinkage Stress and Cuspal Deflection in MOD Restorations: Analytical Solutions and Design Guidelines. Dent. Mater. 2021, 37, 783–795. [Google Scholar] [CrossRef] [PubMed]
| Database | Search Strategy |
|---|---|
| Pubmed | ((((Fiber reinforcement [Title/Abstract]) OR (fiber-reinforced composite [Title/Abstract])) OR (fiber-reinforced restoration [Title/Abstract])) OR (SFRC [Title/Abstract])) OR (EverX [Title/Abstract]) |
| ScienceDirect | in title/abstract: (“tooth” OR “teeth”) AND (“Fiber reinforcement” OR “fiber-reinforced composite” OR “fiber-reinforced restoration” OR “sfrc” OR “everx”) |
| First Author | Type of SFRC | Type of Restoration | Type of Mechanical Testing | Tested Parameters | Main Conclusion |
|---|---|---|---|---|---|
| L. Lassila [27] | EverX Flow | Posterior crown | Statical loading | LBC + FT + FP | “Restorations combining a fiber-reinforced composite core and a surface layer of conventional composite, displayed promising performance related to fracture-behavior.” |
| I. Cekic-Nagas [30] | EverX Posterior, SFRC CAD-CAM | IRFPD | Statical loading | LBC + FP | “FRC had significantly affected load-bearing capacity of tested inlay-retained FDPs” |
| L. Lassila [36] | EverX Flow, SFRC CAD-CAM | IRFDP | Dynamic and statical loading | LBC + FP | “CAD/CAM-fabricated IRFPDs made of experimental SFRC blocks have shown promising performance in clinical testing in terms of fracture behavior”. |
| S. Garoushi [23] | Experimental FRC | Anterior crown | Statical loading | LBC + FP | “Short glass fiber reinforced semi-IPN composite resin demonstrated improved load-bearing capacity compared with conventional particulate filler restorative composite resin”. |
| L. Lassila [28] | EverX Flow | Posterior crown | Statical loading | LBC + FP | “Restorations combining a thick FRC-core and a thin surface layer of PFC (0.5–1 mm), displayed promising performance related to fracture-behavior and load-bearing capacity”. |
| E. Mangoush [37] | EverX Flow, SFRC CAD-CAM | Anterior crown | Statical loading | LBC + FT + FM | “Within the limitation of this study, single-structure CAD/CAM fabricated restorations made of experimental SFRC blocks displayed promising performance related to fracture-behavior”. |
| S. Garoushi [31] | Experimental FRC | FDP | Statical loading | LBC + FP | “Short glass fiber reinforced semi-IPN composite resin revealed improvement in load-bearing capacity compared with the conventional particulate filler veneering composite”. |
| K. Nagata [32] | EverX Posterior, SFRC CAD-CAM | Anterior crown | Statical loading | LBC + FP | “Single-structure FRC restorations showed higher fracture resistance than the restorations made from PFC, leucite-reinforced ceramic, and lithium disilicate”. |
| J. Bijelic [29] | Experimental FRC | Anterior crown | Statical loading | LBC + FP | “…individually formed fiber-reinforced (FRC) root canal post improved the fracture load of the post-crown system and significantly contributed to the reinforcement and strengthening the restored teeth”. |
| S. Garoushi [35] | EverX Posterior | Onlay | Statical loading | LBC + FP | “Onlay restorations combining base of short fiber reinforced composite resin as substructure and surface layer of conventional composite resin displayed promising performance in high load-bearing areas”. |
| L. Lassila [38] | EverX Flow | Anterior crown | Statical loading | LBC + FP | “Using SFC as core material with conventional PFC veneering composite to strengthen anterior crown restoration proved to be a promising strategy for further testing”. |
| J. Bijelic [24] | Experimental FRC | Anterior crown | Statical loading | LBC + FP | “...the use of SFC as a restorative material of choice for fabricating the direct composite post-core-crown restorations of severely damaged incisors provided an improved load-bearing capacity greater than CC…” |
| F. Keulemans [33] | Experimental FRC | Inlay-retained FDP | Statical loading | LBC + FP | “…S-FRC seems to be a viable material for improving the framework of FRC-FDPs...” |
| J. Bijelic [34] | EverX Posterior | Anterior crown | Dynamic and statical loading | LBC + FT + FM + FP | “SFC crowns showed good performance under static and fatigue loading. FT was the only in vitro test method that filtered as a clinically relevant parameter”. |
| S. Garoushi [25] | EverX Posterior | Class II filling and onlay | Statical loading | MGF + LBC + FP | “Based on the microleakage and compressive loading tests, base of short FRC resin and surface layer of conventional composite resin is the best combination”. |
| S. Garoushi [26] | EverX Flow | Overlay | Dynamic and statical loading | LBC + FP | “The most effective method for restoring large MOD cavities was found to be direct restoration using SFC either alone or as a bulk core in combination with PFC composite”. |
| First Author | Clearly Stated Aims/Objectives | Sample Size Calculation | Explanation of Sampling Technique | Details of Control Group | Explanation of Methodology | Operator Details | Randomization | Method of Measurement of Outcome | Outcome Assessor Details | Blinding | Statistical Analysis | Presentation of Results | Risk of Bias |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| L. Lassila [27] | 2 | 0 | 2 | 2 | 2 | 0 | NA | 2 | 0 | NA | 2 | 2 | Medium |
| I. Cekic-Nagas [30] | 2 | 0 | 2 | 1 | 2 | 0 | NA | 2 | 0 | NA | 2 | 2 | Medium |
| L. Lassila [36] | 2 | 0 | 2 | 1 | 2 | 0 | NA | 2 | 0 | NA | 2 | 2 | Medium |
| S. Garoushi [23] | 2 | 0 | 2 | 2 | 2 | 0 | NA | 2 | 0 | NA | 2 | 2 | Medium |
| L. Lassila [28] | 2 | 0 | 2 | 2 | 2 | 0 | NA | 2 | 0 | NA | 2 | 2 | Medium |
| E. Mangoush [37] | 2 | 0 | 2 | 1 | 2 | 0 | NA | 2 | 0 | NA | 2 | 2 | Medium |
| S. Garoushi [31] | 2 | 0 | 2 | 2 | 2 | 0 | NA | 2 | 0 | NA | 2 | 2 | Medium |
| K. Nagata [32] | 2 | 0 | 2 | 1 | 2 | 0 | NA | 2 | 0 | NA | 2 | 2 | Medium |
| J. Bijelic [29] | 2 | 0 | 2 | 2 | 2 | 0 | NA | 2 | 0 | NA | 2 | 2 | Medium |
| S. Garoushi [35] | 2 | 0 | 2 | 2 | 2 | 0 | NA | 2 | 0 | NA | 2 | 2 | Medium |
| L. Lassila [38] | 2 | 0 | 2 | 1 | 2 | 2 | NA | 2 | 1 | NA | 2 | 2 | Low |
| J. Bijelic [24] | 2 | 0 | 2 | 2 | 2 | 1 | NA | 2 | 1 | NA | 2 | 2 | Low |
| F. Keulemans [33] | 2 | 0 | 2 | 1 | 2 | 0 | NA | 2 | 0 | NA | 2 | 2 | Medium |
| J. Bijelic [34] | 2 | 0 | 2 | 2 | 2 | 0 | NA | 2 | 0 | NA | 2 | 2 | Medium |
| S. Garoushi [25] | 2 | 0 | 2 | 2 | 2 | 0 | NA | 2 | 0 | NA | 2 | 2 | Medium |
| S. Garoushi [26] | 2 | 0 | 2 | 2 | 2 | 2 | NA | 2 | 2 | NA | 2 | 2 | Low |
| First Author | Statical Loading | Dynamical Loading | ||
|---|---|---|---|---|
| Direction of Loading | Crosshead Speed | Loading Tip Diameter | ||
| L. Lassila [27] | Vertical (long axis) | 1 mm/min | 5 mm | No |
| I. Cekic-Nagas [30] | Vertical (long axis) | 1 mm/min | 6 mm | No |
| L. Lassila [36] | Vertical (long axis) | 1 mm/min | NA | 10,000 cycles, Fmax = 500 N for 20 s, 1.2 Hz |
| S. Garoushi [23] | 45° Oblique | 1 mm/min | 2 mm | No |
| L. Lassila [28] | Vertical (long axis) | 1 mm/min | 5 mm | No |
| E. Mangoush [37] | 45° Oblique | 1 mm/min | NA | No |
| S. Garoushi [31] | Vertical (long axis) | 1 mm/min | 6 mm | No |
| K. Nagata [32] | 45° Oblique | 1 mm/min | NA | No |
| J. Bijelic [29] | 45° Oblique | 1 mm/min | NA | No |
| S. Garoushi [35] | Vertical (long axis) | 1 mm/min | 3 and 6 mm | No |
| L. Lassila [38] | 45° Oblique | 1 mm/min | NA | No |
| J. Bijelic [24] | 45° Oblique | 1 mm/min | NA | No |
| F. Keulemans [33] | Vertical (long axis) and Oblique (buccal cusp) | 1 mm/min | 6 mm | No |
| J. Bijelic [34] | 45° Oblique | 1 mm/min | NA | Dynamic: 10,000 cycles, 1.0 Hz |
| S. Garoushi [25] | Vertical (long axis) | 1 mm/min | 5 mm | No |
| S. Garoushi [26] | Vertical (long axis) | 1 mm/min | 5 mm | 500,000 cycles, Fmax = 150 N, 1.5 Hz |
| First Author | LBC SFRC Group | LBC Control Group | Significance |
|---|---|---|---|
| L. Lassila [27] | 3866 ± 263 N | 1750–2250 N | p < 0.05 |
| I. Cekic-Nagas [30] | CAD-CAM FRC: 896.1 ± 30.3 N | 476.9 ± 20.3 N | p < 0.05 |
| L. Lassila [36] | Paste SFRC: 476.9 ± 20.3 N | - | |
| S. Garoushi [23] | Before aging SFRC CAD-CAM: 2624 ± 463 N | 1427 ± 409 N | p < 0.05 |
| L. Lassila [28] | Before aging SFRC Flow: 2521 ± 371 N | p < 0.05 | |
| E. Mangoush [37] | After aging SFRC CAD-CAM: 2775 ± 297 N | 1599 ± 397 N | p < 0.05 |
| S. Garoushi [31] | After aging SFRC Flow: 2404 ± 357 N | p < 0.05 | |
| K. Nagata [32] | 349 N | 173 N | p < 0.05 |
| J. Bijelic [29] | 3990 ± 330 N | 1098 ± 179 N | p < 0.05 |
| S. Garoushi [35] | SFRC CAD-CAM: 1650 ± 230 N | 850–950 N | p < 0.05 |
| L. Lassila [38] | SFRC Flow: 1310 ± 397 N | p < 0.05 | |
| J. Bijelic [24] | 2171 N | 1482 N | p < 0.05 |
| F. Keulemans [33] | Paste SFRC: 1145 ± 89.6 | 580 ± 40 N | p < 0.05 |
| J. Bijelic [34] | SFRC CAD-CAM: 913.6 ± 86.3 | p < 0.05 | |
| S. Garoushi [25] | Without post: 238 N | Without post: 158 N | |
| With post: 199 N | With post: 265 N | ||
| L. Lassila [27] | 1733 N | 1081 N | p < 0.05 |
| I. Cekic-Nagas [30] | ~1700 N | ~900 N | p < 0.05 |
| L. Lassila [36] | 515.8 ± 241.6 N | 164.8 ± 95.1 N | p < 0.05 |
| S. Garoushi [23] | Central fossa: 800 N | Central fossa: 702 ± 86 N | |
| L. Lassila [28] | Buccal cusp: 643 ± 8 N | Buccal cusp: 403 ± 62 N | p < 0.05 |
| E. Mangoush [37] | 954 ± 121 N | 415 ± 75 N | p < 0.05 |
| S. Garoushi [31] | 1528 N | ~900 N | p < 0.05 |
| K. Nagata [32] | 2674 ± 465 N | ~1800 N | p < 0.05 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jakab, A.; Palkovics, D.; T. Szabó, V.; Szabó, B.; Vincze-Bandi, E.; Braunitzer, G.; Lassila, L.; Vallittu, P.; Garoushi, S.; Fráter, M. Mechanical Performance of Extensive Restorations Made with Short Fiber-Reinforced Composites without Coverage: A Systematic Review of In Vitro Studies. Polymers 2024, 16, 590. https://doi.org/10.3390/polym16050590
Jakab A, Palkovics D, T. Szabó V, Szabó B, Vincze-Bandi E, Braunitzer G, Lassila L, Vallittu P, Garoushi S, Fráter M. Mechanical Performance of Extensive Restorations Made with Short Fiber-Reinforced Composites without Coverage: A Systematic Review of In Vitro Studies. Polymers. 2024; 16(5):590. https://doi.org/10.3390/polym16050590
Chicago/Turabian StyleJakab, András, Dániel Palkovics, Veronika T. Szabó, Balázs Szabó, Eszter Vincze-Bandi, Gábor Braunitzer, Lippo Lassila, Pekka Vallittu, Sufyan Garoushi, and Márk Fráter. 2024. "Mechanical Performance of Extensive Restorations Made with Short Fiber-Reinforced Composites without Coverage: A Systematic Review of In Vitro Studies" Polymers 16, no. 5: 590. https://doi.org/10.3390/polym16050590
APA StyleJakab, A., Palkovics, D., T. Szabó, V., Szabó, B., Vincze-Bandi, E., Braunitzer, G., Lassila, L., Vallittu, P., Garoushi, S., & Fráter, M. (2024). Mechanical Performance of Extensive Restorations Made with Short Fiber-Reinforced Composites without Coverage: A Systematic Review of In Vitro Studies. Polymers, 16(5), 590. https://doi.org/10.3390/polym16050590









