Investigation on the Biaxial Flexural Strength of Universal Shade Resin-Based Composites
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
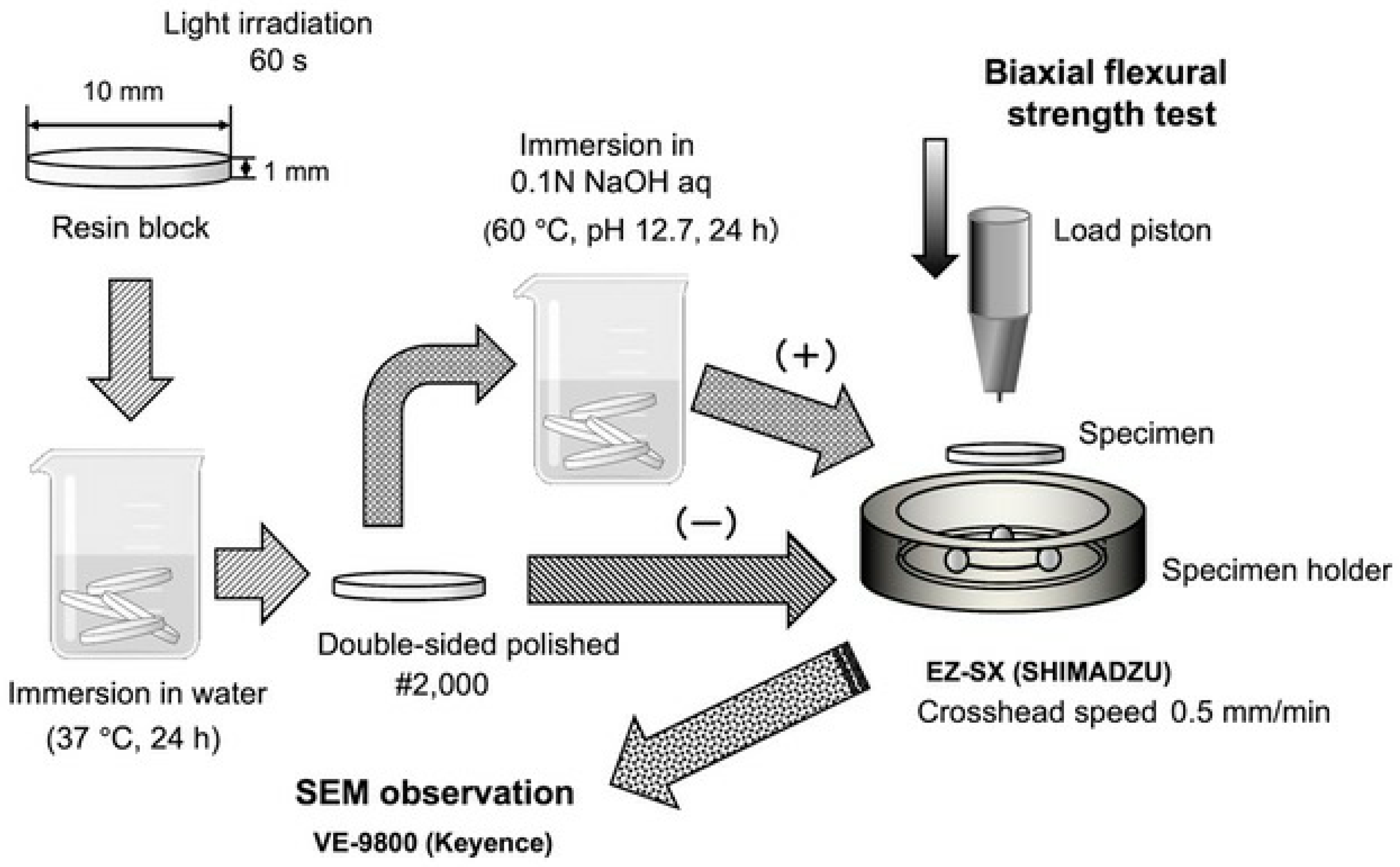
2.2. Sample Preparation
2.3. Biaxial Flexural Test
2.4. Scanning Electron Microscopy (SEM) Observation
2.5. Statistical Analysis
3. Results and Discussion
3.1. Biaxial Flexural Strength
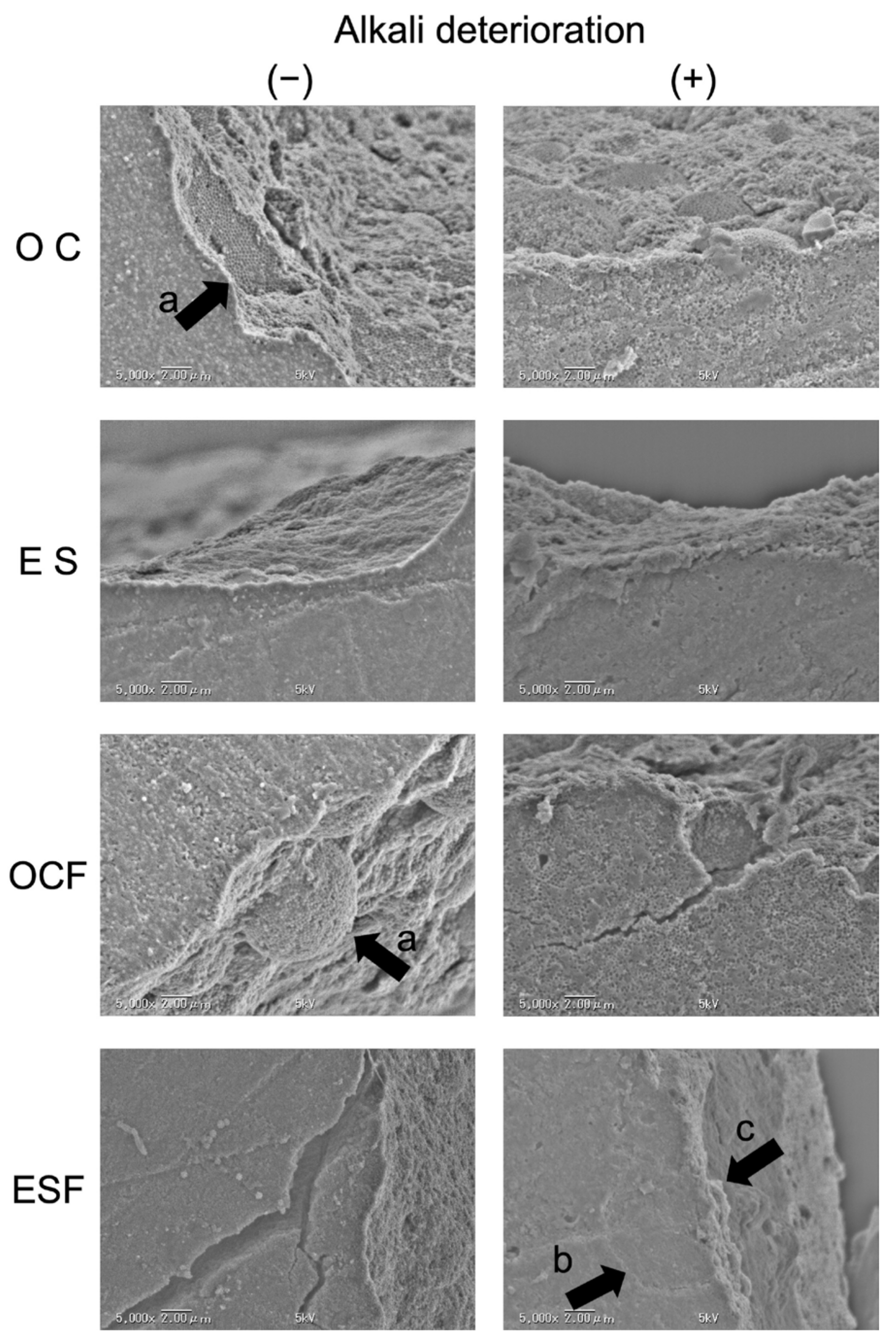
3.2. SEM Observations
3.3. Discussion
4. Conclusions
- For paste-type materials, the biaxial flexural strength of universal shade resin-based composites was higher than that of conventional resin-based composites before alkaline degradation, but after degradation, the two materials showed similar values.
- For flowable materials, the biaxial flexural strength of universal shade resin-based composites was lower than that of conventional resin-based composites.
- Flowable universal shade resin composites should be used with caution in dental restorations.
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Ferracane, J.L. Resin composite--state of the art. Dent. Mater. 2011, 27, 29–38. [Google Scholar] [CrossRef]
- Frencken, J.E.; Peters, M.C.; Manton, D.J.; Leal, S.C.; Gordan, V.V.; Eden, E. Minimal intervention dentistry for managing dental caries - a review: Report of a FDI task group. Int. Dent. J. 2012, 62, 223–243. [Google Scholar] [CrossRef]
- Ilie, N.; Hickel, R. Resin composite restorative materials. Aust. Dent. J. 2011, 56, 59–66. [Google Scholar] [CrossRef]
- Tsujimoto, A.; Barkmeier, W.W.; Teixeira, E.C.; Takamizawa, T.; Miyazaki, M.; Latta, M.A. Fatigue bond strength of dental adhesive systems: Historical background of test methodology, clinical considerations and future perspectives. Jpn. Dent. Sci. Rev. 2022, 58, 193–207. [Google Scholar] [CrossRef]
- de Abreu, J.L.B.; Sampaio, C.S.; Benalcázar Jalkh, E.B.; Hirata, R. Analysis of the color matching of universal resin composites in anterior restorations. J. Esthet. Restor. Dent. 2021, 33, 269–276. [Google Scholar] [CrossRef]
- Joiner, A. Tooth colour: A review of the literature. J. Dent. 2004, 32, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Villarroel, M.; Fahl, N.; De Sousa, A.M.; De Oliveira, O.B., Jr. Direct esthetic restorations based on translucency and opacity of composite resins. J. Esthet. Restor. Dent. 2011, 23, 73–87. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, A.; Nakajima, M.; Seki, N.; Foxton, R.M.; Tagami, J. The effect of tooth age on colour adjustment potential of resin composite restorations. J. Dent. 2015, 43, 253–260. [Google Scholar] [CrossRef]
- Maia, R.R.; Oliveira, D.; D’Antonio, T.; Qian, F.; Skiff, F. Comparison of light-transmittance in dental tissues and dental composite restorations using incremental layering build-up with varying enamel resin layer thickness. Restor. Dent. Endod. 2018, 43, e22. [Google Scholar] [CrossRef] [PubMed]
- La Rosa, G.R.M.; Pasquale, S.; Pedullà, E.; Palermo, F.; Rapisarda, E.; Gueli, A.M. Colorimetric study about the stratification’s effect on colour perception of resin composites. Odontology. 2020, 108, 479–485. [Google Scholar] [CrossRef]
- Joiner, A.; Luo, W. Tooth colour and whiteness: A review. J. Dent. 2017, 67S, S3–S10. [Google Scholar] [CrossRef] [PubMed]
- Mourouzis, P.; Koulaouzidou, E.A.; Palaghias, G.; Helvatjoglu-Antoniades, M. Color match of resin composites to intact tooth structure. J. Appl. Biomater. Funct. Mater. 2015, 13, e259–e265. [Google Scholar] [CrossRef] [PubMed]
- Swift, E.J., Jr.; Hammel, S.A.; Lund, P.S. Colorimetric evaluation of vita shade resin composites. Int. J. Prosthodont. 1994, 7, 356–361. [Google Scholar] [PubMed]
- Trifkovic, B.; Powers, J.M.; Paravina, R.D. Color adjustment potential of resin composites. Clin. Oral Investig. 2018, 22, 1601–1607. [Google Scholar] [CrossRef]
- Paravina, R.D.; Westland, S.; Johnston, W.M.; Powers, J.M. Color adjustment potential of resin composites. J. Dent. Res. 2008, 87, 499–503. [Google Scholar] [CrossRef]
- Hatayama, T.; Kano, Y.; Aida, A.; Chiba, A.; Sato, K.; Seki, N.; Hosaka, K.; Foxton, R.M.; Tagami, J.; Nakajima, M. The combined effect of light-illuminating direction and enamel rod orientation on color adjustment at the enamel borders of composite restorations. Clin. Oral. Investig. 2020, 24, 2305–2313. [Google Scholar] [CrossRef]
- Maesako, M.; Matsui, N.; Fujitani, M.; Garcia-Godoy, F.; Tsujimoto, A. Comparison of surface properties of universal shade and conventional resin-based composites after degradation and repolishing. Am. J. Dent. 2024, 37, 147–153. [Google Scholar]
- Graf, N.; Ilie, N. Long-term mechanical stability and light transmission characteristics of one shade resin-based composites. J. Dent. 2022, 116, 103915. [Google Scholar] [CrossRef]
- Piccoli, Y.B.; Lima, V.P.; Basso, G.R.; Salgado, V.E.; Lima, G.S.; Moraes, R.R. Optical stability of high-translucency resin-based composites. Oper. Dent. 2019, 44, 536–544. [Google Scholar] [CrossRef]
- Oliveira, H.L.Q.; Ribeiro, M.T.H.; Oliveira, G.; Peres, T.S.; Bragança, G.F.; Silva, G.R.; Soares, C.J. Mechanical and optical characterization of single-shade resin. Oper. Dent. 2024, 49, 210–221. [Google Scholar] [CrossRef]
- Durand, L.B.; Ruiz-López, J.; Perez, B.G.; Ionescu, A.; Carrillo-Perez, F.; Ghinea, R.; Pérez, M.M. Color, lightness, chroma, hue, and translucency adjustment potential of resin composites using CIEDE2000 color difference formula. J. Esthet. Restor. Dent. 2021, 33, 836–843. [Google Scholar] [CrossRef] [PubMed]
- Yamashita, A.; Kobayashi, S.; Furusawa, K.; Tichy, A.; Oguro, R.; Hosaka, K.; Shimada, Y.; Nakajima, M. Does the thickness of universal-shade composites affect the ability to reflect the color of background dentin? Dent. Mater. J. 2023, 42, 255–265. [Google Scholar] [CrossRef] [PubMed]
- Tsujimoto, A.; Barkmeier, W.W.; Takamizawa, T.; Latta, M.A.; Miyazaki, M. Depth of cure, flexural properties and volumetric shrinkage of low and high viscosity bulk-fill giomers and resin composites. Dent. Mater. J. 2017, 36, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Ilie, N. Universal chromatic resin-based composites: Aging behavior quantified by quasi-static and viscoelastic behavior analysis. Bioengineering 2022, 9, 270. [Google Scholar] [CrossRef]
- Katada, H.; Inokoshi, M.; Kamijo, S.; Liu, H.; Xu, K.; Kawashita, M.; Yokoi, T.; Shimabukuro, M.; Minakuchi, S. Effects of multiple firings on the translucency, crystalline phase, and mechanical strength of highly translucent zirconia. Dent. Mater. J. 2024, 43, 294–302. [Google Scholar] [CrossRef] [PubMed]
- Al-Johani, H.; Haider, J.; Silikas, N.; Satterthwaite, J. Effect of repeated firing on the topographical, optical, and mechanical properties of fully crystallized lithium silicate-based ceramics. J. Prosthet. Dent. 2024, 131, 741.e1–741.e11. [Google Scholar] [CrossRef]
- Frankel, N.; Pearson, G.J.; Labella, R. Long-term strength of aesthetic restoratives. J. Oral. Rehabil. 1998, 25, 89–93. [Google Scholar] [CrossRef] [PubMed]
- ISO 6872:2015; Dental Ceramics. International Organization for Standardization: Geneva, Switzerland, 2015.
- Ban, S.; Hasegawa, J.; Anusavice, K.J. Effect of loading conditions on bi-axial flexure strength of dental cements. Dent. Mater. 1992, 8, 100–104. [Google Scholar] [CrossRef] [PubMed]
- Tsujimoto, A.; Irie, M.; Teixeira, E.C.N.; Jurado, C.A.; Maruo, Y.; Nishigawa, G.; Matsumoto, T.; Garcia-Godoy, F. Relationships between flexural and bonding properties, marginal adaptation, and polymerization shrinkage in flowable composite restorations for dental application. Polymers 2021, 13, 2613. [Google Scholar] [CrossRef]
- Chai, H.; Russ, J.; Vardhaman, S.; Lim, C.H.; Zhang, Y. A bilayer method for measuring the toughness and strength of dental ceramics. J. Dent. Res. 2024, 103, 419–426. [Google Scholar] [CrossRef]
- Chung, S.M.; Yap, A.U.; Chandra, S.P.; Lim, C.T. Flexural strength of dental composite restoratives: Comparison of biaxial and three-point bending test. J. Biomed. Mater. Res. B Appl. Biomater. 2004, 71, 278–283. [Google Scholar] [CrossRef] [PubMed]
- Maesako, M.; Kishimoto, T.; Horie, T.; Suzuki, M.; Inoue, K.; Mizuno, A.; Tomoda, S.; Fujitani, M. Microstructural properties and surface properties of a new resin composite employing structural color technology. J. Hard Tissue Biol. 2021, 30, 7–12. [Google Scholar] [CrossRef]
- Maesako, M.; Kishimoto, T.; Tomoda, S.; Horie, T.; Yamada, M.; Iwawaki, R.; Odagiri, Y.; Sakuma, K.; Inoue, K.; Takeguchi, A.; et al. Evaluation of the repolished surface properties of a resin composite employing structural coloration technology. Materials 2021, 14, 7280. [Google Scholar] [CrossRef] [PubMed]
- Sarkar, N.K. Internal corrosion in dental composite wear. J. Biomed. Mater. Res. 2000, 53, 371–380. [Google Scholar] [CrossRef] [PubMed]
- Bagheri, R.; Tyas, M.J.; Burrow, M.F. Subsurface degradation of resin-based composites. Dent. Mater. 2007, 23, 944–951. [Google Scholar] [CrossRef] [PubMed]
- Sathyanarayana, H.P.; Premkumar, S.; Manjula, W.S. Assessment of maximum voluntary bite force in adults with normal occlusion and different types of malocclusions. J. Contemp. Dent. Pract. 2012, 13, 534–538. [Google Scholar] [CrossRef]
- Padma, S.; Umesh, S.; Asokan, S.; Srinivas, T. Bite force measurement based on fiber Bragg grating sensor. J. Biomed. Opt. 2017, 22, 107002. [Google Scholar] [CrossRef]
| Brand Name | Omnichroma | Omnichroma Flow (Medium) | Estelite Σ Quick | Estelite Universal Flow |
|---|---|---|---|---|
| Code | OC | OCF | ES | ESF |
| Manufacturer | Tokuyama | Tokuyama | Tokuyama | Tokuyama |
| Dental | Dental | Dental | Dental | |
| Lot No. | 573 | 48,032 | 219,089 | 94,040 |
| Filler size | φ260 nm | φ260 nm | φ200 nm | φ200 nm |
| Filler contents | 79 wt% (68 vol/%) | 71 wt% (57 vol/%) | 82 wt% (71 vol/%) | 71 wt% (57 vol/%) |
| Matrix resin | UDMA | UDMA | Bis-GMA | Bis-GMA UDMA Bis-MPEPP |
| Source | SS | df | Mean Squares | F-Ratio | p-Value |
|---|---|---|---|---|---|
| Material | 140,487.357 | 3 | 46,829.119 | 190.593 | 0.006 |
| Condition | 20,302.466 | 1 | 20,302.466 | 82.63 | <0.001 |
| Material × Condition | 1470.167 | 3 | 490.056 | 1.99 | 0.083 |
| Condition | Material | |
|---|---|---|
| OC | ES | |
| Alkaline-deterioration (−) | 156.2 (28.6) Aa | 131.2 (9.9) Ab |
| Alkaline-deterioration (+) | 109.7 (5.2) Ba | 103.7 (7.9) Ba |
| Source | SS | df | Mean Squares | F-Ratio | p-Value |
|---|---|---|---|---|---|
| Material | 61,679.818 | 1 | 61,679.818 | 290.642 | <0.001 |
| Condition | 7139.851 | 1 | 7139.818 | 33.644 | <0.001 |
| Material × Condition | 55.909 | 1 | 55.909 | 0.263 | 0.611 |
| Condition | Material | |
|---|---|---|
| OCF | ESF | |
| Alkaline-deterioration (−) | 160.0 (10.6) Aa | 240.8 (8.7) Ab |
| Alkaline-deterioration (+) | 135.6 (12.4) Ba | 211.72 (20.5) Bb |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sakuma, K.; Horie, T.; Kishimoto, T.; Maesako, M.; Tomoda, S.; Fujitani, M.; Tsujimoto, A. Investigation on the Biaxial Flexural Strength of Universal Shade Resin-Based Composites. Polymers 2024, 16, 1853. https://doi.org/10.3390/polym16131853
Sakuma K, Horie T, Kishimoto T, Maesako M, Tomoda S, Fujitani M, Tsujimoto A. Investigation on the Biaxial Flexural Strength of Universal Shade Resin-Based Composites. Polymers. 2024; 16(13):1853. https://doi.org/10.3390/polym16131853
Chicago/Turabian StyleSakuma, Keiko, Taku Horie, Takafumi Kishimoto, Mayumi Maesako, Shigetaka Tomoda, Morioki Fujitani, and Akimasa Tsujimoto. 2024. "Investigation on the Biaxial Flexural Strength of Universal Shade Resin-Based Composites" Polymers 16, no. 13: 1853. https://doi.org/10.3390/polym16131853
APA StyleSakuma, K., Horie, T., Kishimoto, T., Maesako, M., Tomoda, S., Fujitani, M., & Tsujimoto, A. (2024). Investigation on the Biaxial Flexural Strength of Universal Shade Resin-Based Composites. Polymers, 16(13), 1853. https://doi.org/10.3390/polym16131853






