Improving Hemocompatibility of Polysulfone Membrane by UV-Assisted Grafting of Sulfonated Chitosan
Abstract
1. Introduction
2. Objects and Methods
2.1. Materials
2.2. Preparation of Sulfonated Dihydroxy Propyl Chitosan (SDHPCS)
2.3. Sulfonated Dihydroxy Propyl Chitosan-Grafted Allyl Glycidyl Ether (AGE-SDHPCS)
2.4. PSf Membrane Grafted with 2,4-Dihydroxybenzophenone (PSf-OH)
2.5. Synthesis of PSf-OH Membrane Grafted with SDHPCS (PSf-SDHPCS)
2.6. Characterization
2.7. Blood Compatibility
2.7.1. Bovine Serum Albumin (BSA) Adhesion
2.7.2. Hemolysis Test
2.7.3. Platelet Adhesion
2.7.4. Plasma Recalcification Time (PRT)
2.7.5. APTT, PT and TT
3. Results and Discussions
3.1. Surface Characterization
3.1.1. Synthesis of Chitosan Derivates
3.1.2. Water Contact Angle Analysis
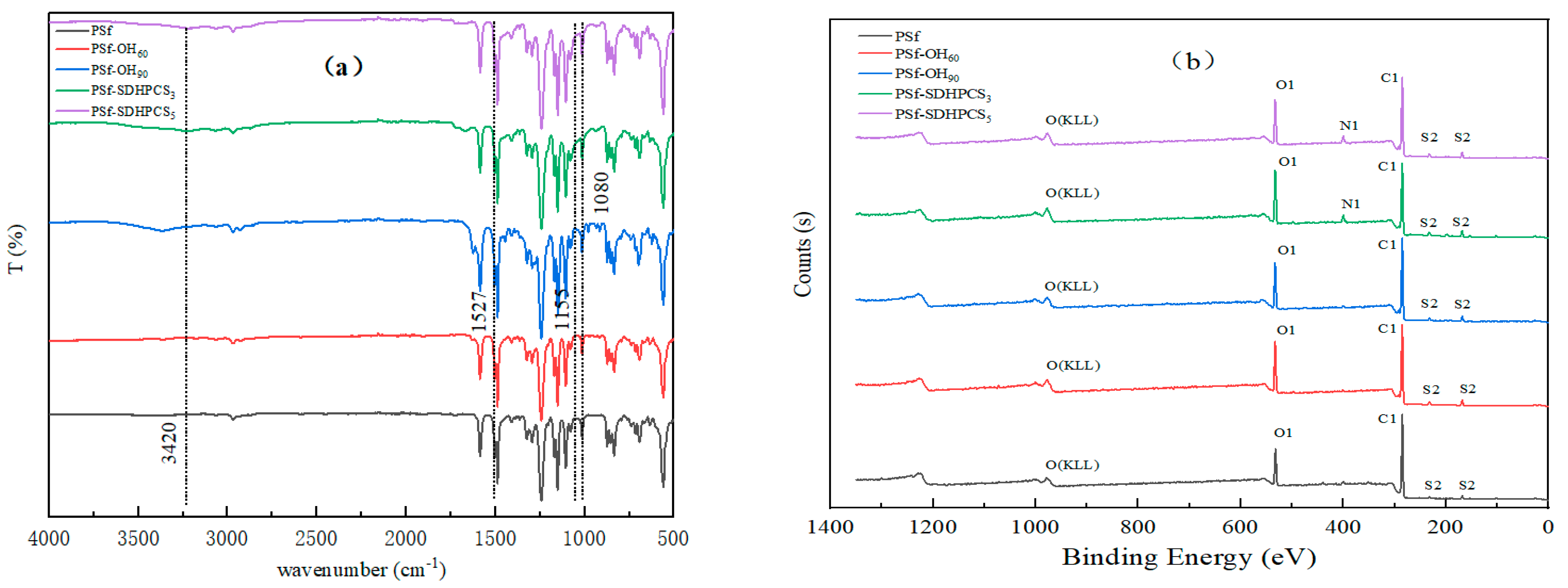
3.1.3. ATR-FTIR Analysis
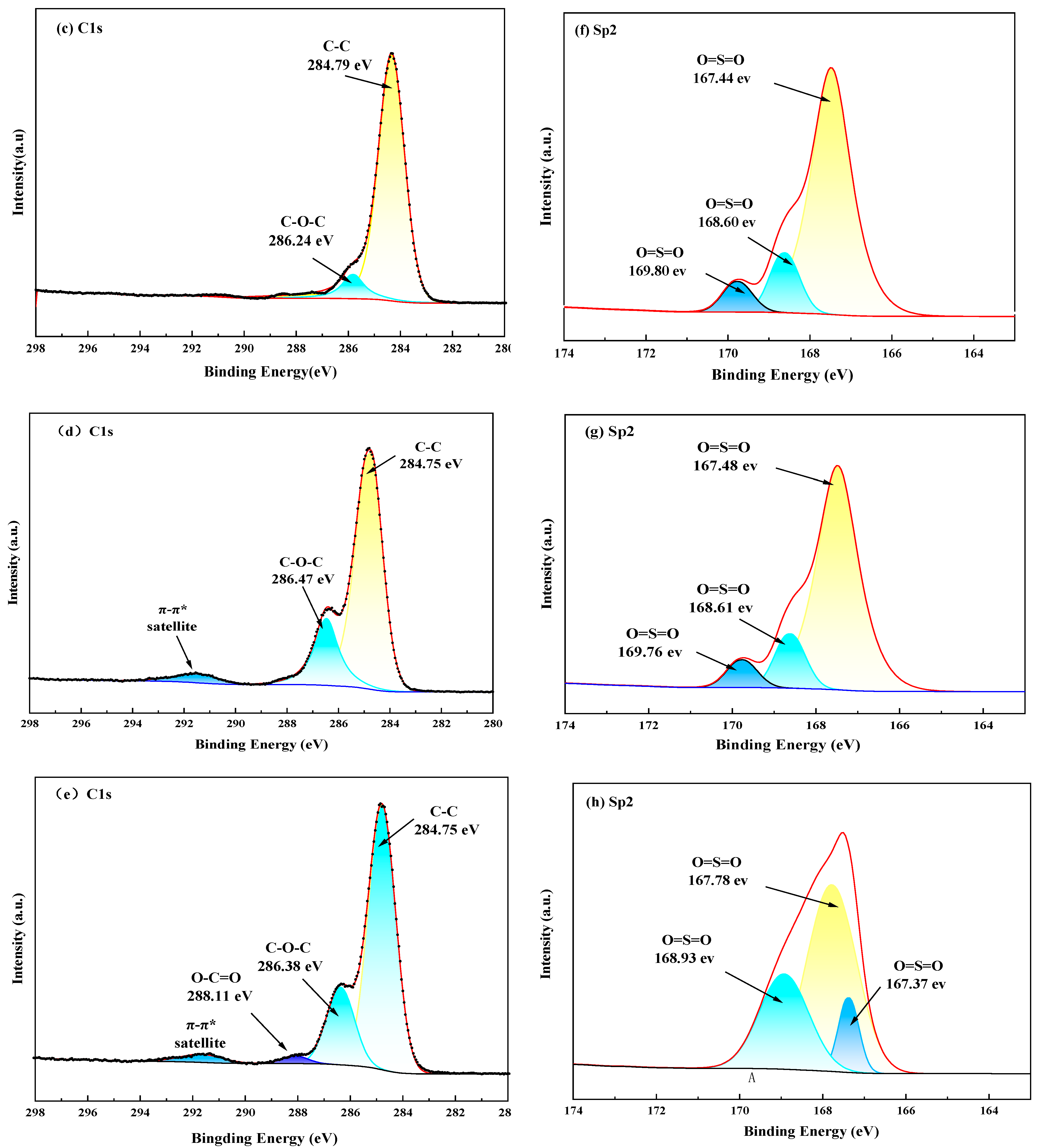
3.1.4. XPS Analysis
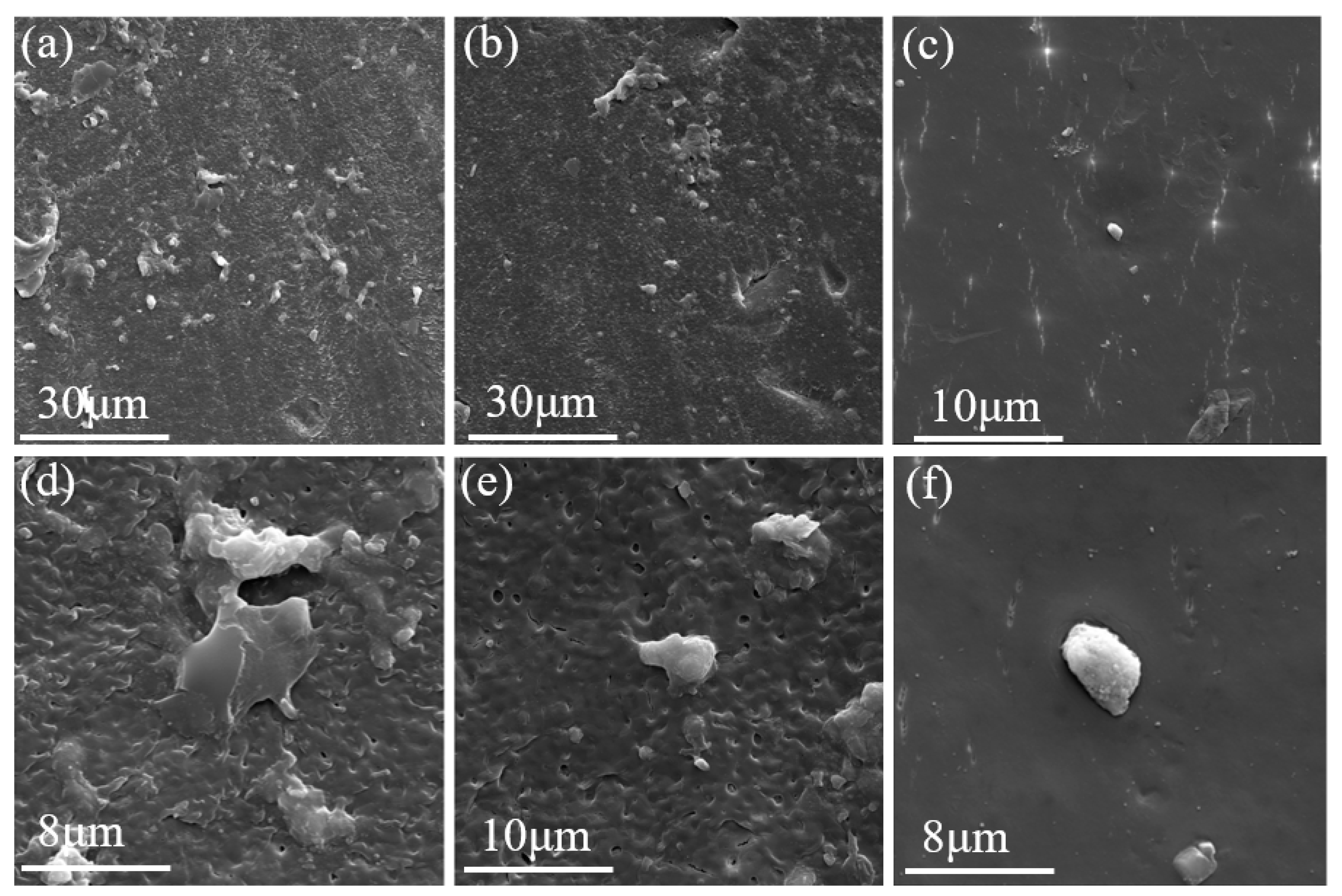
3.1.5. The Across-Section Morphologies of Membranes
3.2. Hemocompatibility Tests
3.2.1. Adsorption of Protein
3.2.2. Platelet Adhesion
3.2.3. Hemolysis Assay
3.2.4. Plasma Recalcification Time (PRT)
3.2.5. APTT, PT and TT
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Lufrano, F.; Squadrito, G.; Patti, A.; Passalacqua, E. Sulfonated Polysulfone as Promising Membranes for Polymer Electrolyte Fuel Cells. J. Appl. Polym. Sci. 2015, 77, 1250–1256. [Google Scholar] [CrossRef]
- Ishihara, K.; Fukumoto, K.; Iwasaki, Y.; Nakabayashi, N. Modification of Polysulfone with Phospholipid Polymer for Improvement of the Blood Compatibility. Part 1. Surface Characterization. Biomaterials 1999, 20, 1545–1551. [Google Scholar] [CrossRef] [PubMed]
- Barton, A.J.; Sagers, R.D.; Pitt, W.G. Bacterial Adhesion to Orthopedic Implant Polymers. J. Biomed. Mater. Res. Part B Appl. Biomater. 2015, 30, 403–410. [Google Scholar] [CrossRef]
- Saedi, S.; Madaeni, S.S.; Arabi Shamsabadi, A.; Mottaghi, F. The Effect of Surfactants on the Structure and Performance of PES Membrane for Separation of Carbon Dioxide from Methane. Sep. Purif. Technol. 2012, 99, 104–119. [Google Scholar] [CrossRef]
- Tran, C.; Hallahan, N.; Kosobrodova, E.; Tong, J.; Thorn, P.; Bilek, M. Plasma Surface Engineering to Biofunctionalise Polymers for β-Cell Adhesion. Coatings 2021, 11, 1085. [Google Scholar] [CrossRef]
- Serbanescu, O.S.; Voicu, S.I.; Thakur, V.K. Polysulfone Functionalized Membranes: Properties and Challenges. Mater. Today Chem. 2020, 17, 100302. [Google Scholar] [CrossRef]
- Eken, G.A.; Acar, M.H. Polysulfone-based Amphiphilic Copolymers: Effect of Hydrophilic Content on Morphology and Performance of Ultrafiltration Membranes. J. Appl. Polym. Sci. 2020, 137, 48306. [Google Scholar] [CrossRef]
- Li, S.; Cui, Z.; Zhang, L.; He, B.; Li, J. The Effect of Sulfonated Polysulfone on the Compatibility and Structure of Polyethersulfone-Based Blend Membranes. J. Membr. Ence 2016, 513, 1–11. [Google Scholar] [CrossRef]
- Higuchi, A.; Shirano, K.; Harashima, M.; Yoon, B.O.; Hara, M.; Hattori, M.; Imamura, K. Chemically Modified Polysulfone Hollow Fibers with Vinylpyrrolidone Having Improved Blood Compatibility. Biomaterials 2002, 23, 2659–2666. [Google Scholar] [CrossRef] [PubMed]
- Park, J.Y.; Acar, M.H.; Akthakul, A.; Kuhlman, W.; Mayes, A.M. Polysulfone-Graft-Poly(Ethylene Glycol) Graft Copolymers for Surface Modification of Polysulfone Membranes. Biomaterials 2006, 27, 856–865. [Google Scholar] [CrossRef]
- Tu, M.M.; Xu, J.-J.; Qiu, Y.R. Surface Hemocompatible Modification of Polysulfone Membrane via Covalently Grafting Acrylic Acid and Sulfonated Hydroxypropyl Chitosan. RSC Adv. 2019, 9, 6254–6266. [Google Scholar] [CrossRef] [PubMed]
- Pandele, A.M.; Serbanescu, O.S.; Voicu, S.I. Polysulfone Composite Membranes with Carbonaceous Structure. Synthesis and Applications. Coatings 2020, 10, 609. [Google Scholar] [CrossRef]
- Yang, H.C.; Luo, J.; Lv, Y.; Shen, P.; Xu, Z.K. Surface Engineering of Polymer Membranes via Mussel-Inspired Chemistry. J. Membr. Sci. 2015, 483, 42–59. [Google Scholar] [CrossRef]
- Wang, J.; Yang, X.; Zheng, D.; Yao, A.; Zhan, G. Fabrication of Bioinspired Gallic Acid-Grafted Chitosan/Polysulfone Composite Membranes for Dye Removal via Nanofiltration. ACS Omega 2020, 5, 13077–13086. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.; Ma, B.R.; Dong, Z.; Zhu, L.J.; Xue, L.X. Positively Charged Loose Nanofiltration Membrane Grafted by Diallyl Dimethyl Ammonium Chloride (DADMAC) via UV for Salt and Dye Removal. React. Funct. Polym. 2014, 86, 191–198. [Google Scholar] [CrossRef]
- Deng, H.; Xu, Y.; Chen, Q.; Wei, X.; Zhu, B. High Flux Positively Charged Nanofiltration Membranes Prepared by UV-Initiated Graft Polymerization of Methacrylatoethyl Trimethyl Ammonium Chloride (DMC) onto Polysulfone Membranes. J. Membr. Sci. 2011, 366, 363–372. [Google Scholar] [CrossRef]
- Wang, X.L.; Wei, J.F.; Yang, Y.M.; Zhang, H.; Shi, G.Y. Preparation and Characterization of Negatively Charged Polysulfone Hollow Fiber Membrane by UV-Photografting Polymerization of AMPS. Adv. Mater. Res. 2010, 129–131, 295–300. [Google Scholar] [CrossRef]
- Chen, D.; Chang, C.C.; Cooper, B.; Silvers, A.; Emrick, T.; Hayward, R.C. Photopatternable Biodegradable Aliphatic Polyester with Pendent Benzophenone Groups. Biomacromolecules 2015, 16, 3329–3335. [Google Scholar] [CrossRef] [PubMed]
- Dimida, S.; Barca, A.; Cancelli, N.; Benedictis, V.D.; Demitri, C. Effects of Genipin Concentration on Cross-Linked Chitosan Scaffolds for Bone Tissue Engineering: Structural Characterization and Evidence of Biocompatibility Features. Int. J. Polym. Sci. 2017, 2017, 8410750. [Google Scholar] [CrossRef]
- Zhang, C.; Qu, G.; Sun, Y.; Wu, X.; Yao, Z.; Guo, Q.; Ding, Q.; Yuan, S.; Shen, Z.; Ping, Q. Pharmacokinetics, Biodistribution, Efficacy and Safety of N-Octyl-O-Sulfate Chitosan Micelles Loaded with Paclitaxel. Biomaterials 2008, 29, 1233–1241. [Google Scholar] [CrossRef] [PubMed]
- Xiong, W.; Yi, Y.; Liu, H.; Wang, H.; Liu, J.; Ying, G. Selective Carboxypropionylation of Chitosan: Synthesis, Characterization, Blood Compatibility, and Degradation. Carbohydr. Res. 2011, 346, 1217–1223. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; He, C.; Feng, Y.; Yang, Y.; Zhao, C.S. A Chitosan Modified Asymmetric Small-Diameter Vascular Graft with Anti-Thrombotic and Anti-Bacterial Functions for Vascular Tissue Engineering. J. Mater. Chem. B 2019, 8, 568–577. [Google Scholar] [CrossRef] [PubMed]
- Badr, I.H.A.; Gouda, M.; Abdel-Sattar, R.; Sayour, H.E.M. Reduction of Thrombogenicity of PVC-Based Sodium Selective Membrane Electrodes Using Heparin-Modified Chitosan. Carbohydr. Polym. 2014, 99, 783–790. [Google Scholar] [CrossRef]
- Nie, C.; Ma, L.; Cheng, C.; Deng, J.; Zhao, C. Nanofibrous Heparin and Heparin-Mimicking Multilayers as Highly Effective Endothelialization and Antithrombogenic Coatings. Biomacromolecules 2015, 16, 992–1001. [Google Scholar] [CrossRef] [PubMed]
- Song, W.; Zeng, Q.; Yin, X.; Zhu, L.; Gong, T.; Pan, C. Changjiang Preparation and Anticoagulant Properties of Heparin-like Electrospun Membranes from Carboxymethyl Chitosan and Bacterial Cellulose Sulfate. Int. J. Biol. Macromol. 2018, 120, 1396–1405. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.M.; Xu, J.J.; Qiu, Y.R. A Novel Kind of Polysulfone Material with Excellent Biocompatibility Modified by the Sulfonated Hydroxypropyl Chitosan. Mater. Sci. Eng. C Mater. Biol. Appl. 2017, 79, 570. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.M.; Xu, J.J.; Qiu, Y.R. The Effect of Upstream Platelet–Fibrinogen Interactions on Downstream Adhesion and Activation. Biomaterials 2012, 33, 1255–1260. [Google Scholar]
- Tokarska-Schlattner, M.; Epand, R.F.; Meiler, F.; Zandomeneghi, G.; Neumann, D.; Widmer, H.R.; Meier, B.H.; Epand, R.M.; Saks, V.; Wallimann, T. Phosphocreatine Interacts with Phospholipids, Affects Membrane Properties and Exerts Membrane-Protective Effects. PLoS ONE 2012, 7, e43178. [Google Scholar] [CrossRef] [PubMed]
- Gorbet, M.B.; Sefton, M. V Biomaterial-Associated Thrombosis: Roles of Coagulation Factors, Complement, Platelets and Leukocytes. Biomaterials 2004, 25, 5681–5703. [Google Scholar] [CrossRef] [PubMed]
- Yan, S.; Tu, M.-M.; Qiu, Y.-R. The Hemocompatibility of the Modified Polysulfone Membrane with 4-(Chloromethyl)Benzoic Acid and Sulfonated Hydroxypropyl Chitosan. Colloids Surf. B Biointerfaces 2020, 188, 110769. [Google Scholar] [CrossRef] [PubMed]
- ISO 10993; Biological Evaluation of Medical Devices. Food and Drug Administration: White Oak, MD, USA, 2016.






| Samples | Elemental (at%) | |||
|---|---|---|---|---|
| O% | N% | C% | S% | |
| PSf | 22.70 | 0.18 | 74.11 | 2.62 |
| PSf-OH60 | 21.93 | 0.14 | 75.72 | 2.20 |
| PSf-OH90 | 20.62 | 0.21 | 76.46 | 2.66 |
| PSf-SDHPCS3 | 30.24 | 2.88 | 62.99 | 3.94 |
| PSf-SDHPCS5 | 33.41 | 3.31 | 59.17 | 4.11 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yan, S.; Qiu, Y. Improving Hemocompatibility of Polysulfone Membrane by UV-Assisted Grafting of Sulfonated Chitosan. Polymers 2024, 16, 1555. https://doi.org/10.3390/polym16111555
Yan S, Qiu Y. Improving Hemocompatibility of Polysulfone Membrane by UV-Assisted Grafting of Sulfonated Chitosan. Polymers. 2024; 16(11):1555. https://doi.org/10.3390/polym16111555
Chicago/Turabian StyleYan, Sheng, and Yunren Qiu. 2024. "Improving Hemocompatibility of Polysulfone Membrane by UV-Assisted Grafting of Sulfonated Chitosan" Polymers 16, no. 11: 1555. https://doi.org/10.3390/polym16111555
APA StyleYan, S., & Qiu, Y. (2024). Improving Hemocompatibility of Polysulfone Membrane by UV-Assisted Grafting of Sulfonated Chitosan. Polymers, 16(11), 1555. https://doi.org/10.3390/polym16111555






