Nanoparticles as Drug Delivery Systems: A Review of the Implication of Nanoparticles’ Physicochemical Properties on Responses in Biological Systems
Abstract
1. Nanotechnology: Current State of the Art
2. Industrial Application of Nanotechnology
2.1. Food Industry
2.2. Cosmetic Industry
2.3. Nanomedicine
- Size and Shape: The size and shape of the iron/silica nanoparticles must be carefully controlled to optimize their performance and minimize any potential toxicity.
- Surface functionalization: The surface of the nanoparticles can be functionalized with various moieties, such as polymers, antibodies, or small molecules, to target specific cells or tissues. It is important to consider the stability, specificity, and efficiency of these functionalisation in the design of the nanoplatform.
- Core stability: Some of these nanoparticles such as iron oxide are known to be highly reactive, so it is important to ensure that the iron oxide core of the nanoparticles is stable and does not degrade or aggregate in biological systems.
- Biocompatibility: The nanoplatform must be biocompatible, meaning that it should not elicit an adverse reaction in biological systems, such as inflammation, toxicity, or immune response.
- Release kinetics: For therapeutic applications, it is important to consider the release kinetics of the payload from the nanoplatform. The release rate should be carefully controlled to ensure that the payload is delivered in a manner that is effective and safe.
- Targeting and accumulation: For therapeutic applications, it is also important to consider the targeting and accumulation of the nanoplatform in the desired tissue or organ. The nanoplatform must be able to selectively target and accumulate in the desired location in order to maximize its therapeutic efficacy.
3. Physiochemical Properties of Nanoparticles in Medicine
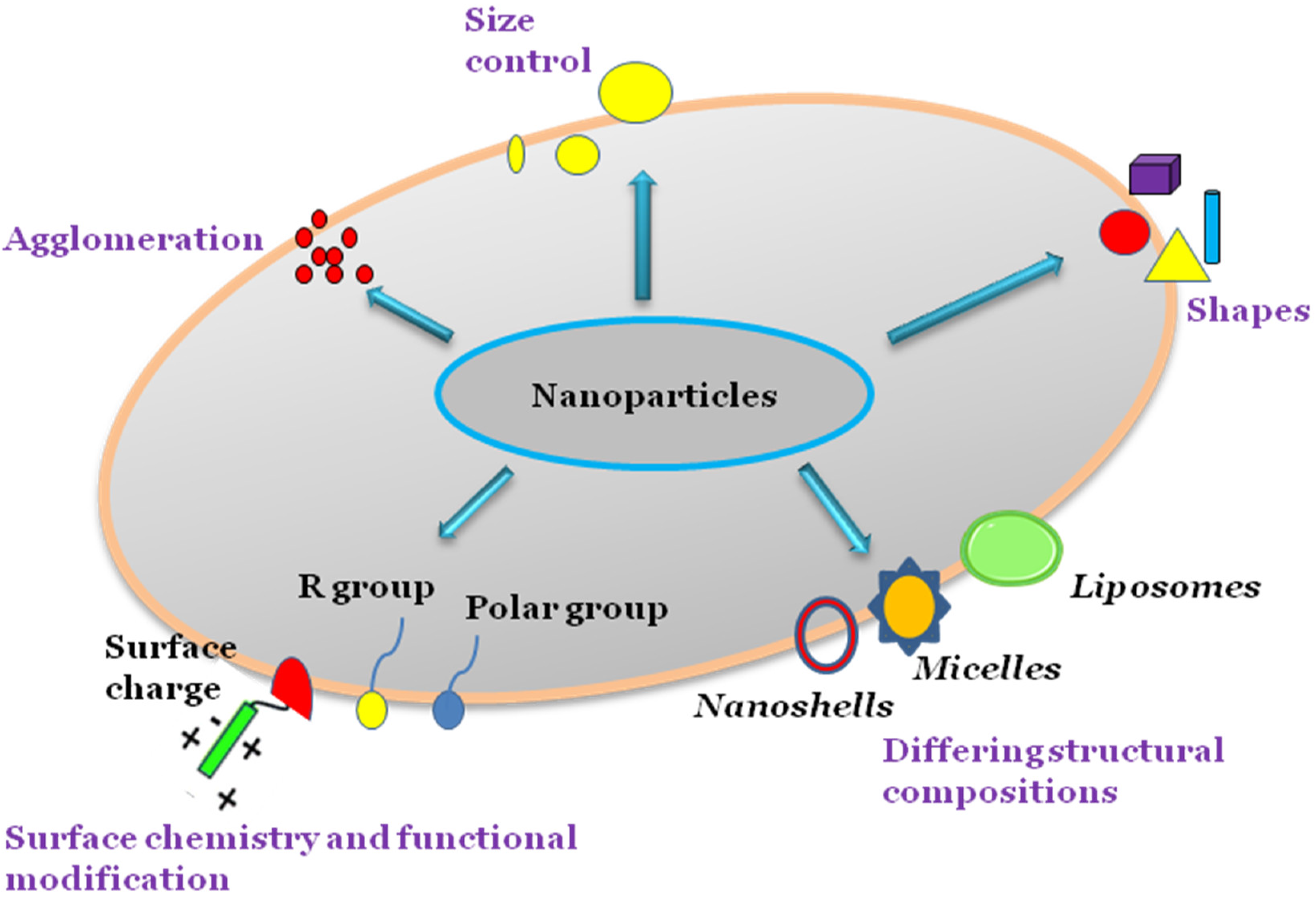
3.1. Size and Surface Area
3.2. Surface Chemistry
3.3. Shape
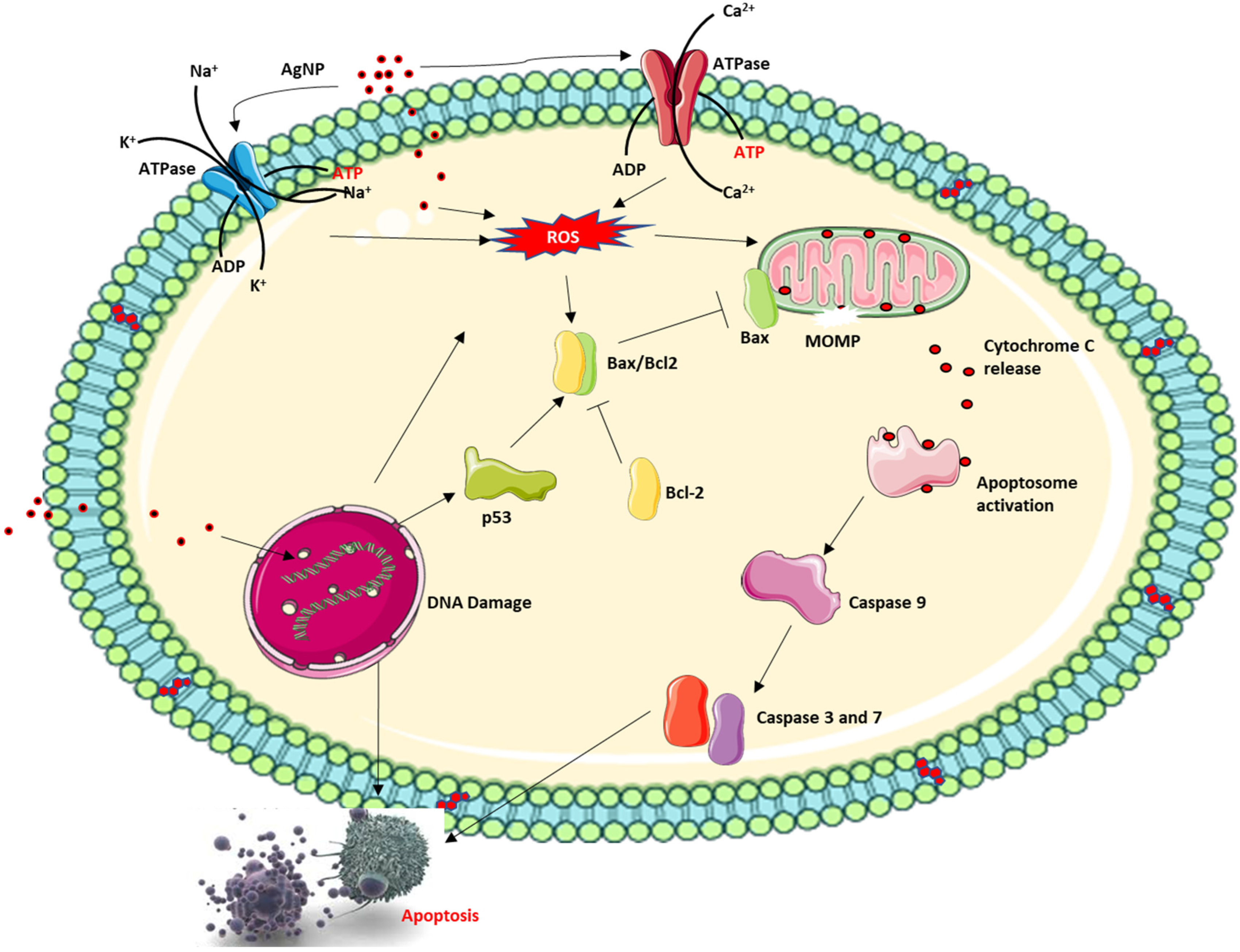
4. Nanoparticle Cytotoxicity
5. Nanoparticle Drug Delivery Systems (DSSs) in Disease Treatment
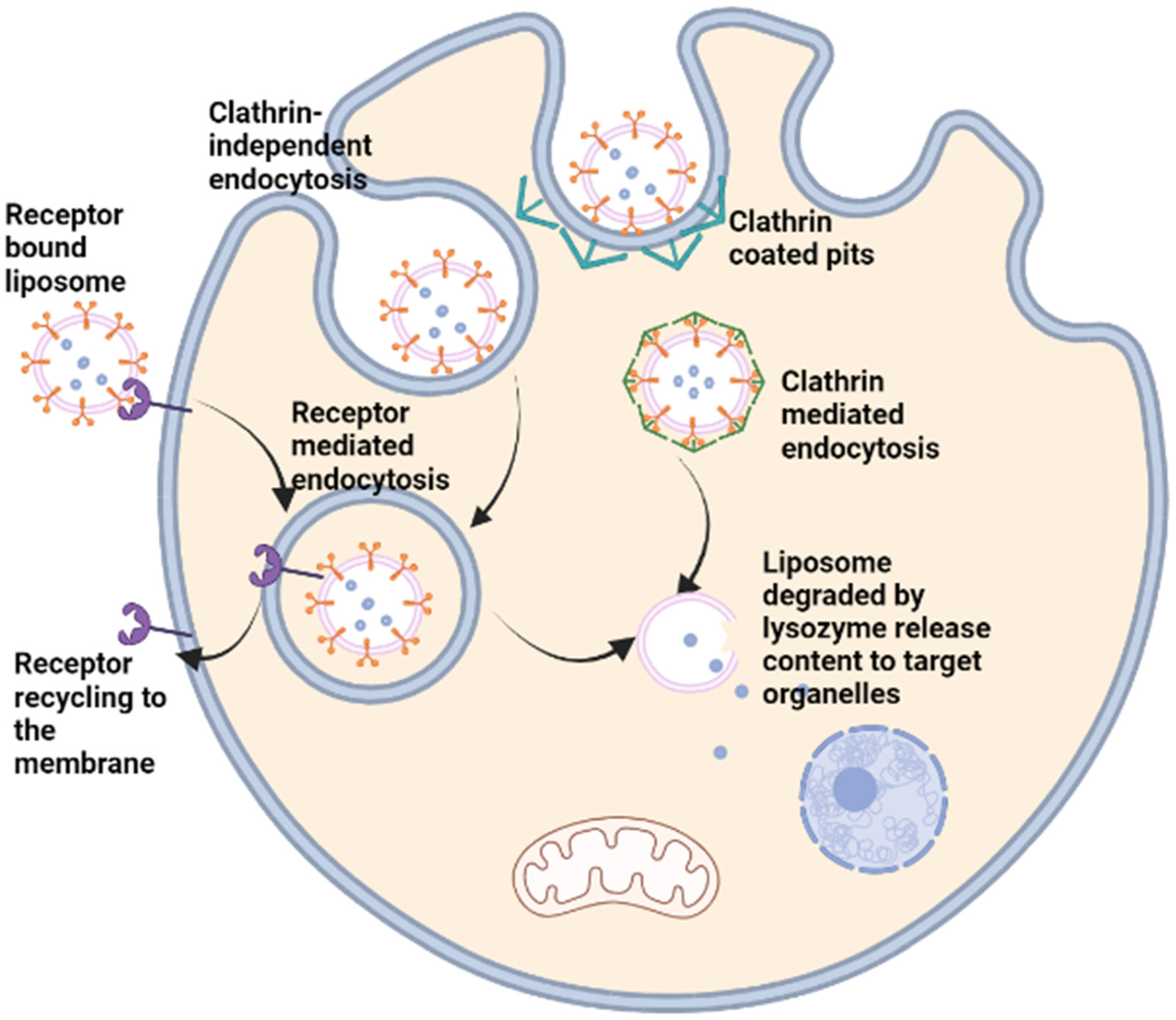
5.1. Lipid-Based DSSs
5.2. Polymeric DSSs
5.3. Peptide Nanoparticle DSSs
5.4. Inorganic Nanoparticle-Based DSSs
5.5. Nanoparticle Delivery Systems and Suppression of Drug-Associated Toxicity
6. Summary and Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nasrollahzadeh, M.; Sajadi, S.M.; Sajjadi, M.; Issaabadi, Z. An introduction to nanotechnology. In Interface Science and Technology; Elsevier: Amsterdam, The Netherlands, 2019; Volume 28, pp. 1–27. [Google Scholar]
- Doran, J.; Ryan, G. Does nanotechnology research generate an innovation premium over other types of research? Evidence from Ireland. Technol. Soc. 2019, 59, 101183. [Google Scholar] [CrossRef]
- Cheng, Y.J.; Wolkenhauer, M.; Bumbu, G.G.; Gutmann, J.S. A Facile Route to Reassemble Titania Nanoparticles into Ordered Chain-like Networks on Substrate. Macromol. Rapid Commun. 2012, 33, 218–224. [Google Scholar] [CrossRef] [PubMed]
- Kango, S.; Kalia, S.; Celli, A.; Njuguna, J.; Habibi, Y.; Kumar, R. Surface modification of inorganic nanoparticles for development of organic–inorganic nanocomposites—A review. Prog. Polym. Sci. 2013, 38, 1232–1261. [Google Scholar] [CrossRef]
- Roco, M.C. Overview: Affirmation of Nanotechnology between 2000 and 2030. In Nanotechnology Commercialization: Manufacturing Processes and Products; Wiley: Hoboken, NJ, USA, 2017; pp. 1–23. [Google Scholar] [CrossRef]
- Huang, Q.; Yu, H.; Ru, Q. Bioavailability and delivery of nutraceuticals using nanotechnology. J. Food Sci. 2010, 75, R50–R57. [Google Scholar] [CrossRef] [PubMed]
- Bajpai, V.K.; Kamle, M.; Shukla, S.; Mahato, D.K.; Chandra, P.; Hwang, S.K.; Kumar, P.; Huh, Y.S.; Han, Y.-K. Prospects of using nanotechnology for food preservation, safety, and security. J. Food Drug Anal. 2018, 26, 1201–1214. [Google Scholar] [CrossRef]
- Carbone, M.; Donia, D.T.; Sabbatella, G.; Antiochia, R. Silver nanoparticles in polymeric matrices for fresh food packaging. J. King Saud Univ. Sci. 2016, 28, 273–279. [Google Scholar] [CrossRef]
- An, J.; Zhang, M.; Wang, S.; Tang, J. Physical, chemical and microbiological changes in stored green asparagus spears as affected by coating of silver nanoparticles-PVP. LWT Food Sci. Technol. 2008, 41, 1100–1107. [Google Scholar] [CrossRef]
- Banach, M.; Tymczyna, L.; Chmielowiec-Korzeniowska, A.; Pulit-Prociak, J. Nanosilver biocidal properties and their application in disinfection of hatchers in poultry processing plants. Bioinorg. Chem. Appl. 2016, 2016, 5214783. [Google Scholar] [CrossRef]
- Emamifar, A.; Kadivar, M.; Shahedi, M.; Soleimanian-Zad, S. Effect of nanocomposite packaging containing Ag and ZnO on inactivation of Lactobacillus plantarum in orange juice. Food Control 2011, 22, 408–413. [Google Scholar] [CrossRef]
- Zhang, C.; Li, W.; Zhu, B.; Chen, H.; Chi, H.; Li, L.; Qin, Y.; Xue, J. The Quality Evaluation of Postharvest Strawberries Stored in Nano-Ag Packages at Refrigeration Temperature. Polymers 2018, 10, 894. [Google Scholar] [CrossRef]
- Venkatasubbu, G.D.; Baskar, R.; Anusuya, T.; Seshan, C.A.; Chelliah, R. Toxicity mechanism of titanium dioxide and zinc oxide nanoparticles against food pathogens. Colloids Surf. B Biointerfaces 2016, 148, 600–606. [Google Scholar] [CrossRef] [PubMed]
- Fathi, M.; Martín, Á.; McClements, D.J. Nanoencapsulation of food ingredients using carbohydrate based delivery systems. Trends Food Sci. Technol. 2014, 39, 18–39. [Google Scholar] [CrossRef]
- Davis, J.L.; Paris, H.L.; Beals, J.W.; Binns, S.E.; Giordano, G.R.; Scalzo, R.L.; Schweder, M.M.; Blair, E.; Bell, C. Liposomal-encapsulated Ascorbic Acid: Influence on Vitamin C Bioavailability and Capacity to Protect Against Ischemia-Reperfusion Injury. Nutr. Metab. Insights 2016, 9, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Hallan, S.S.; Kaur, V.; Jain, V.; Mishra, N. Development and characterization of polymer lipid hybrid nanoparticles for oral delivery of LMWH. Artif. Cells Nanomed. Biotechnol. 2017, 45, 1631–1639. [Google Scholar] [CrossRef] [PubMed]
- Lu, H.; Zhang, S.; Wang, J.; Chen, Q. A Review on Polymer and Lipid-Based Nanocarriers and Its Application to Nano-Pharmaceutical and Food-Based Systems. Front. Nutr. 2021, 8, 783831. [Google Scholar] [CrossRef]
- Singh, T.; Shukla, S.; Kumar, P.; Wahla, V.; Bajpai, V.K. Application of Nanotechnology in Food Science: Perception and Overview. Front. Microbiol. 2017, 8, 1501. [Google Scholar] [CrossRef]
- Frohlich, E.E.; Frohlich, E. Cytotoxicity of Nanoparticles Contained in Food on Intestinal Cells and the Gut Microbiota. Int. J. Mol. Sci. 2016, 17, 509. [Google Scholar] [CrossRef]
- Kim, Y.S.; Kim, J.S.; Cho, H.S.; Rha, D.S.; Kim, J.M.; Park, J.D.; Choi, B.S.; Lim, R.; Chang, H.K.; Chung, Y.H.; et al. Twenty-eight-day oral toxicity, genotoxicity, and gender-related tissue distribution of silver nanoparticles in Sprague-Dawley rats. Inhal. Toxicol. 2008, 20, 575–583. [Google Scholar] [CrossRef]
- Shahare, B.; Yashpal, M. Toxic effects of repeated oral exposure of silver nanoparticles on small intestine mucosa of mice. Toxicol. Mech. Methods 2013, 23, 161–167. [Google Scholar] [CrossRef]
- Park, E.J.; Bae, E.; Yi, J.; Kim, Y.; Choi, K.; Lee, S.H.; Yoon, J.; Lee, B.C.; Park, K. Repeated-dose toxicity and inflammatory responses in mice by oral administration of silver nanoparticles. Environ. Toxicol. Pharm. 2010, 30, 162–168. [Google Scholar] [CrossRef]
- Morganti, P. Use and potential of nanotechnology in cosmetic dermatology. Clin. Cosmet. Investig. Dermatol. CCID 2010, 3, 5. [Google Scholar] [CrossRef]
- Verma, P.; Pathak, K. Therapeutic and cosmeceutical potential of ethosomes: An overview. J. Adv. Pharm. Technol. Res. 2010, 1, 274–282. [Google Scholar] [CrossRef]
- Abadi, M.F.D.; Mehrabian, S.; Asghari, B.; Namvar, A.E.; Ezzatifar, F.; Lari, A.R. Silver nanoparticles as active ingredient used for alcohol-free mouthwash. GMS Hyg. Infect. Control 2013, 8, Doc05. [Google Scholar] [CrossRef]
- Prabhu, S.; Poulose, E.K. Silver nanoparticles: Mechanism of antimicrobial action, synthesis, medical applications, and toxicity effects. Int. Nano Lett. 2012, 2, 32. [Google Scholar] [CrossRef]
- Feynman, R.P. There’s plenty of room at the bottom. Eng. Sci. 1960, 23, 22–36. [Google Scholar]
- Douglas, S.M.; Bachelet, I.; Church, G.M. A logic-gated nanorobot for targeted transport of molecular payloads. Science 2012, 335, 831–834. [Google Scholar] [CrossRef]
- Trihirun, S.; Achalakul, T.; Kaewkamnerdpong, B. Modeling nanorobot control for blood vessel repair: A non-Newtonian blood model. In Proceedings of the Biomedical Engineering International Conference (BMEiCON), Amphur Muang, Thailand, 23–25 October 2013; pp. 1–5. [Google Scholar]
- Cavalcanti, A.; Rosen, L.; Shirinzadeh, B.; Rosenfeld, M.; Paulo, S.; Aviv, T. Nanorobot for treatment of patients with artery occlusion. In Proceedings of the Proceedings of Virtual Concept, Cancun, Mexico, 26 November–1 December 2006. [Google Scholar]
- Khadka, P.; Ro, J.; Kim, H.; Kim, I.; Kim, J.T.; Kim, H.; Cho, J.M.; Yun, G.; Lee, J. Pharmaceutical particle technologies: An approach to improve drug solubility, dissolution and bioavailability. Asian J. Pharm. Sci. 2014, 9, 304–316. [Google Scholar] [CrossRef]
- Barua, S.; Mitragotri, S. Challenges associated with Penetration of Nanoparticles across Cell and Tissue Barriers: A Review of Current Status and Future Prospects. Nano Today 2014, 9, 223–243. [Google Scholar] [CrossRef]
- Khurana, A.; Tekula, S.; Saifi, M.A.; Venkatesh, P.; Godugu, C. Therapeutic applications of selenium nanoparticles. Biomed. Pharm. 2019, 111, 802–812. [Google Scholar] [CrossRef]
- Sharma, A.R.; Lee, Y.H.; Bat-Ulzii, A.; Bhattacharya, M.; Chakraborty, C.; Lee, S.S. Recent advances of metal-based nanoparticles in nucleic acid delivery for therapeutic applications. J. Nanobiotechnol. 2022, 20, 501. [Google Scholar] [CrossRef]
- Park, J.H.; von Maltzahn, G.; Ruoslahti, E.; Bhatia, S.N.; Sailor, M.J. Micellar hybrid nanoparticles for simultaneous magnetofluorescent imaging and drug delivery. Angew. Chem. Int. Ed. Engl. 2008, 47, 7284–7288. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Cai, X.; Hu, J.; Shao, N.; Wang, F.; Zhang, Q.; Xiao, J.; Cheng, Y. Glutathione-triggered “off–on” release of anticancer drugs from dendrimer-encapsulated gold nanoparticles. J. Am. Chem. Soc. 2013, 135, 9805–9810. [Google Scholar] [CrossRef] [PubMed]
- Sanyakamdhorn, S.; Agudelo, D.; Tajmir-Riahi, H.-A. Encapsulation of antitumor drug doxorubicin and its analogue by chitosan nanoparticles. Biomacromolecules 2013, 14, 557–563. [Google Scholar] [CrossRef] [PubMed]
- Hasan, M.; Belhaj, N.; Benachour, H.; Barberi-Heyob, M.; Kahn, C.; Jabbari, E.; Linder, M.; Arab-Tehrany, E. Liposome encapsulation of curcumin: Physico-chemical characterizations and effects on MCF7 cancer cell proliferation. Int. J. Pharm. 2014, 461, 519–528. [Google Scholar] [CrossRef]
- Koudelka, S.; Masek, J.; Neuzil, J.; Turanek, J. Lyophilised liposome-based formulations of alpha-tocopheryl succinate: Preparation and physico-chemical characterisation. J. Pharm. Sci. 2010, 99, 2434–2443. [Google Scholar] [CrossRef]
- Barenholz, Y. Doxil(R)—The first FDA-approved nano-drug: Lessons learned. J. Control. Release 2012, 160, 117–134. [Google Scholar] [CrossRef]
- Ventola, C.L. Progress in Nanomedicine: Approved and Investigational Nanodrugs. Pharm. Ther. 2017, 42, 742–755. [Google Scholar]
- Tran, S.; DeGiovanni, P.J.; Piel, B.; Rai, P. Cancer nanomedicine: A review of recent success in drug delivery. Clin. Transl. Med. 2017, 6, 44. [Google Scholar] [CrossRef]
- Patra, J.K.; Das, G.; Fraceto, L.F.; Campos, E.V.R.; Rodriguez-Torres, M.D.P.; Acosta-Torres, L.S.; Diaz-Torres, L.A.; Grillo, R.; Swamy, M.K.; Sharma, S.; et al. Nano based drug delivery systems: Recent developments and future prospects. J. Nanobiotechnol. 2018, 16, 71. [Google Scholar] [CrossRef]
- Meyerhoff, A.U.S. Food and Drug Administration approval of AmBisome (liposomal amphotericin B) for treatment of visceral leishmaniasis. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 1999, 28, 42–48; discussion 49–51. [Google Scholar] [CrossRef]
- Passero, F.C.; Grapsa, D.; Syrigos, K.N.; Saif, M.W. The safety and efficacy of Onivyde (irinotecan liposome injection) for the treatment of metastatic pancreatic cancer following gemcitabine-based therapy. Expert Rev. Anticancer Ther. 2016, 16, 697–703. [Google Scholar] [CrossRef]
- Alfayez, M.; Kantarjian, H.; Kadia, T.; Ravandi-Kashani, F.; Daver, N. CPX-351 (vyxeos) in AML. Leuk. Lymphoma 2020, 61, 288–297. [Google Scholar] [CrossRef]
- Kraft, J.C.; Freeling, J.P.; Wang, Z.; Ho, R.J. Emerging research and clinical development trends of liposome and lipid nanoparticle drug delivery systems. J. Pharm. Sci. 2014, 103, 29–52. [Google Scholar] [CrossRef]
- Liu, L.; Ye, Q.; Lu, M.; Chen, S.-T.; Tseng, H.-W.; Lo, Y.-C.; Ho, C. A New Approach to Deliver Anti-cancer Nanodrugs with Reduced Off-target Toxicities and Improved Efficiency by Temporarily Blunting the Reticuloendothelial System with Intralipid. Sci. Rep. 2017, 7, 16106. [Google Scholar] [CrossRef] [PubMed]
- Angst, M.S.; Drover, D.R. Pharmacology of Drugs Formulated with DepoFoam™. Clin. Pharmacokinet. 2006, 45, 1153–1176. [Google Scholar] [CrossRef] [PubMed]
- Hamblin, M.R. Photodynamic Therapy for Cancer: What’s Past is Prologue. Photochem. Photobiol. 2020, 96, 506–516. [Google Scholar] [CrossRef] [PubMed]
- Harris, J.M.; Chess, R.B. Effect of pegylation on pharmaceuticals. Nat. Rev. Drug Discov. 2003, 2, 214–221. [Google Scholar] [CrossRef]
- Fishburn, C.S. The pharmacology of PEGylation: Balancing PD with PK to generate novel therapeutics. J. Pharm. Sci. 2008, 97, 4167–4183. [Google Scholar] [CrossRef]
- Ohlmann, C.H.; Gross-Langenhoff, M. Efficacy and Tolerability of Leuprorelin Acetate (Eligard®) in Daily Practice in Germany: Pooled Data from 2 Prospective, Non-Interventional Studies with 3- or 6-Month Depot Formulations in Patients with Advanced Prostate Cancer. Urol. Int. 2018, 100, 66–71. [Google Scholar] [CrossRef]
- Goel, N.; Stephens, S. Certolizumab Pegol. MAbs 2010, 2, 137–147. [Google Scholar] [CrossRef]
- Nagpal, M.; Nagpal, K.; Nagpal, P.N. A comparative debate on the various anti-vascular endothelial growth factor drugs: Pegaptanib sodium (Macugen), ranibizumab (Lucentis) and bevacizumab (Avastin). Indian J. Ophthalmol. 2007, 55, 437–439. [Google Scholar] [CrossRef]
- Alphandéry, E.; Grand-Dewyse, P.; Lefèvre, R.; Mandawala, C.; Durand-Dubief, M. Cancer therapy using nanoformulated substances: Scientific, regulatory and financial aspects. Expert Rev. Anticancer Ther. 2015, 15, 1233–1255. [Google Scholar] [CrossRef]
- Wang, Y.-S.; Youngster, S.; Grace, M.; Bausch, J.; Bordens, R.; Wyss, D.F. Structural and biological characterization of pegylated recombinant interferon alpha-2b and its therapeutic implications. Adv. Drug Deliv. Rev. 2002, 54, 547–570. [Google Scholar] [CrossRef]
- Steinman, L.; Zamvil, S.S. How to successfully apply animal studies in experimental allergic encephalomyelitis to research on multiple sclerosis. Ann. Neurol. 2006, 60, 12–21. [Google Scholar] [CrossRef]
- Goodman, A. New Drug Watch: Aprepitant (Emend). Oncol. Times 2003, 25, 58. [Google Scholar] [CrossRef]
- Swanson, J.M.; Lerner, M.; Wigal, T.; Steinhoff, K.; Greenhill, L.; Posner, K.; Freid, J.; Wigal, S. The use of a laboratory school protocol to evaluate concepts about efficacy and side effects of new formulations of stimulant medications. J. Atten. Disord. 2002, 6, 73–88. [Google Scholar] [CrossRef]
- Kverno, K.; Rozenberg, I. Long-Acting Injectable Antipsychotics in the Treatment of Schizophrenia: Practical Considerations. J. Psychosoc. Nurs. Ment. Health Serv. 2021, 59, 7–12. [Google Scholar] [CrossRef]
- Gracies, J.-M.; Nance, P.; Elovic, E.; McGuire, J.; Simpson, D.M. Traditional pharmacological treatments for spasticity part II: General and regional treatments. Muscle Nerve Off. J. Am. Assoc. Electrodiagn. Med. 1997, 20, 92–120. [Google Scholar] [CrossRef]
- Singh, I. Bad Boys, Good Mothers, and the “Miracle” of Ritalin. Sci. Context 2002, 15, 577–603. [Google Scholar] [CrossRef]
- Gordon, D.B. New Opioid Formulations and Delivery Systems. Pain Manag. Nurs. 2007, 8, S6–S13. [Google Scholar] [CrossRef]
- Auerbach, M.; Henry, D.; DeLoughery, T.G. Intravenous ferric derisomaltose for the treatment of iron deficiency anemia. Am. J. Hematol. 2021, 96, 727–734. [Google Scholar] [CrossRef] [PubMed]
- Chertow, G.M.; Mason, P.D.; Vaage-Nilsen, O.; Ahlmén, J. Update on adverse drug events associated with parenteral iron. Nephrol. Dial. Transplant. 2005, 21, 378–382. [Google Scholar] [CrossRef] [PubMed]
- Rüger, J.; Ioannou, S.; Castanotto, D.; Stein, C.A. Oligonucleotides to the (Gene) Rescue: FDA Approvals 2017–2019. Trends Pharmacol. Sci. 2020, 41, 27–41. [Google Scholar] [CrossRef] [PubMed]
- Doolittle, N.D.; Dosa, E.; Neuwelt, E.A. Iron-Oxide Nanoparticles as Magnetic Resonance Contrast Agents: Expanding Their Potential Beyond Iron Replacement Therapy. Blood 2009, 114, 1998. [Google Scholar] [CrossRef]
- Nam, J.; Won, N.; Bang, J.; Jin, H.; Park, J.; Jung, S.; Park, Y.; Kim, S. Surface engineering of inorganic nanoparticles for imaging and therapy. Adv. Drug Deliv. Rev. 2013, 65, 622–648. [Google Scholar] [CrossRef]
- Lee, N.; Yoo, D.; Ling, D.; Cho, M.H.; Hyeon, T.; Cheon, J. Iron Oxide Based Nanoparticles for Multimodal Imaging and Magnetoresponsive Therapy. Chem. Rev. 2015, 115, 10637–10689. [Google Scholar] [CrossRef]
- Kim, J.S.; Rieter, W.J.; Taylor, K.M.; An, H.; Lin, W. Self-assembled hybrid nanoparticles for cancer-specific multimodal imaging. J. Am. Chem. Soc. 2007, 129, 8962–8963. [Google Scholar] [CrossRef]
- Louie, A. Multimodality imaging probes: Design and challenges. Chem. Rev. 2010, 110, 3146–3195. [Google Scholar] [CrossRef]
- Shirshahi, V.; Soltani, M. Solid silica nanoparticles: Applications in molecular imaging. Contrast Media Mol. Imaging 2015, 10, 1–17. [Google Scholar] [CrossRef]
- Chaloupka, K.; Malam, Y.; Seifalian, A.M. Nanosilver as a new generation of nanoproduct in biomedical applications. Trends Biotechnol. 2010, 28, 580–588. [Google Scholar] [CrossRef]
- Nel, A.; Xia, T.; Mädler, L.; Li, N. Toxic potential of materials at the nanolevel. Science 2006, 311, 622–627. [Google Scholar] [CrossRef]
- Powers, K.W.; Palazuelos, M.; Moudgil, B.M.; Roberts, S.M. Characterization of the size, shape, and state of dispersion of nanoparticles for toxicological studies. Nanotoxicology 2007, 1, 42–51. [Google Scholar] [CrossRef]
- Tsai, C.Y.; Lu, S.L.; Hu, C.W.; Yeh, C.S.; Lee, G.B.; Lei, H.Y. Size-dependent attenuation of TLR9 signaling by gold nanoparticles in macrophages. J. Immunol. 2012, 188, 68–76. [Google Scholar] [CrossRef]
- Jiang, W.; Kim, B.Y.; Rutka, J.T.; Chan, W.C. Nanoparticle-mediated cellular response is size-dependent. Nat. Nanotechnol. 2008, 3, 145–150. [Google Scholar] [CrossRef]
- Rejman, J.; Oberle, V.; Zuhorn, I.S.; Hoekstra, D. Size-dependent internalization of particles via the pathways of clathrin- and caveolae-mediated endocytosis. Biochem. J. 2004, 377, 159–169. [Google Scholar] [CrossRef]
- Chithrani, D.B.; Dunne, M.; Stewart, J.; Allen, C.; Jaffray, D.A. Cellular uptake and transport of gold nanoparticles incorporated in a liposomal carrier. Nanomedicine 2010, 6, 161–169. [Google Scholar] [CrossRef]
- Gosangari, S.L.; Watkin, K.L. Effect of preparation techniques on the properties of curcumin liposomes: Characterization of size, release and cytotoxicity on a squamous oral carcinoma cell line. Pharm. Dev. Technol. 2012, 17, 103–109. [Google Scholar] [CrossRef]
- Oh, E.; Delehanty, J.B.; Sapsford, K.E.; Susumu, K.; Goswami, R.; Blanco-Canosa, J.B.; Dawson, P.E.; Granek, J.; Shoff, M.; Zhang, Q. Cellular uptake and fate of PEGylated gold nanoparticles is dependent on both cell-penetration peptides and particle size. Acs Nano 2011, 5, 6434–6448. [Google Scholar] [CrossRef]
- Saucier-Sawyer, J.K.; Deng, Y.; Seo, Y.-E.; Cheng, C.J.; Zhang, J.; Quijano, E.; Saltzman, W.M. Systemic delivery of blood–brain barrier-targeted polymeric nanoparticles enhances delivery to brain tissue. J. Drug Target. 2015, 23, 736–749. [Google Scholar] [CrossRef]
- Suk, J.S.; Xu, Q.; Kim, N.; Hanes, J.; Ensign, L.M. PEGylation as a strategy for improving nanoparticle-based drug and gene delivery. Adv. Drug Deliv. Rev. 2016, 99, 28–51. [Google Scholar] [CrossRef]
- Fillion, P.; Desjardins, A.; Sayasith, K.; Lagace, J. Encapsulation of DNA in negatively charged liposomes and inhibition of bacterial gene expression with fluid liposome-encapsulated antisense oligonucleotides. Biochim. Biophys. Acta 2001, 1515, 44–54. [Google Scholar] [CrossRef] [PubMed]
- Dichello, G.A.; Fukuda, T.; Maekawa, T.; Whitby, R.L.D.; Mikhalovsky, S.V.; Alavijeh, M.; Pannala, A.S.; Sarker, D.K. Preparation of liposomes containing small gold nanoparticles using electrostatic interactions. Eur. J. Pharm. Sci. 2017, 105, 55–63. [Google Scholar] [CrossRef] [PubMed]
- Ewert, K.K.; Kotamraju, V.R.; Majzoub, R.N.; Steffes, V.M.; Wonder, E.A.; Teesalu, T.; Ruoslahti, E.; Safinya, C.R. Synthesis of linear and cyclic peptide-PEG-lipids for stabilization and targeting of cationic liposome-DNA complexes. Bioorg. Med. Chem. Lett. 2016, 26, 1618–1623. [Google Scholar] [CrossRef] [PubMed]
- Pan, G.-H.; Barras, A.; Boussekey, L.; Addad, A.; Boukherroub, R. Alkyl passivation and SiO2 encapsulation of silicon nanoparticles: Preparation, surface modification and luminescence properties. J. Mater. Chem. C 2013, 1, 5261–5271. [Google Scholar] [CrossRef]
- Yin, H.; Casey, P.S.; McCall, M.J. Surface modifications of ZnO nanoparticles and their cytotoxicity. J. Nanosci. Nanotechnol. 2010, 10, 7565–7570. [Google Scholar] [CrossRef]
- Bozzuto, G.; Molinari, A. Liposomes as nanomedical devices. Int. J. Nanomed. 2015, 10, 975. [Google Scholar] [CrossRef]
- Chen, X.; Han, W.; Zhao, X.; Tang, W.; Wang, F. Epirubicin-loaded marine carrageenan oligosaccharide capped gold nanoparticle system for pH-triggered anticancer drug release. Sci. Rep. 2019, 9, 6754. [Google Scholar] [CrossRef]
- Wang, J.; Li, J.; Guo, G.; Wang, Q.; Tang, J.; Zhao, Y.; Qin, H.; Wahafu, T.; Shen, H.; Liu, X.; et al. Silver-nanoparticles-modified biomaterial surface resistant to staphylococcus: New insight into the antimicrobial action of silver. Sci. Rep. 2016, 6, 32699. [Google Scholar] [CrossRef]
- Milla, P.; Dosio, F.; Cattel, L. PEGylation of proteins and liposomes: A powerful and flexible strategy to improve the drug delivery. Curr. Drug Metab. 2012, 13, 105–119. [Google Scholar] [CrossRef]
- Marchetti, C.; Palaia, I.; Giorgini, M.; De Medici, C.; Iadarola, R.; Vertechy, L.; Domenici, L.; Di Donato, V.; Tomao, F.; Muzii, L.; et al. Targeted drug delivery via folate receptors in recurrent ovarian cancer: A review. Onco Targets Ther. 2014, 7, 1223–1236. [Google Scholar] [CrossRef]
- Carron, P.M.; Crowley, A.; O’Shea, D.; McCann, M.; Howe, O.; Hunt, M.; Devereux, M. Targeting the Folate Receptor: Improving Efficacy in Inorganic Medicinal Chemistry. Curr. Med. Chem. 2018, 25, 2675–2708. [Google Scholar] [CrossRef]
- Steichen, S.D.; Caldorera-Moore, M.; Peppas, N.A. A review of current nanoparticle and targeting moieties for the delivery of cancer therapeutics. Eur. J. Pharm. Sci. 2013, 48, 416–427. [Google Scholar] [CrossRef]
- Champion, J.A.; Mitragotri, S. Role of target geometry in phagocytosis. Proc. Natl. Acad. Sci. USA 2006, 103, 4930–4934. [Google Scholar] [CrossRef]
- Zhao, Y.; Wang, Y.; Ran, F.; Cui, Y.; Liu, C.; Zhao, Q.; Gao, Y.; Wang, D.; Wang, S. A comparison between sphere and rod nanoparticles regarding their in vivo biological behavior and pharmacokinetics. Sci. Rep. 2017, 7, 4131. [Google Scholar] [CrossRef]
- Wozniak, A.; Malankowska, A.; Nowaczyk, G.; Grzeskowiak, B.F.; Tusnio, K.; Slomski, R.; Zaleska-Medynska, A.; Jurga, S. Size and shape-dependent cytotoxicity profile of gold nanoparticles for biomedical applications. J. Mater. Sci. Mater. Med. 2017, 28, 92. [Google Scholar] [CrossRef]
- Wang, Y.; Gou, K.; Guo, X.; Ke, J.; Li, S.; Li, H. Advances in regulating physicochemical properties of mesoporous silica nanocarriers to overcome biological barriers. Acta Biomater. 2021, 123, 72–92. [Google Scholar] [CrossRef]
- Hadji, H.; Bouchemal, K. Effect of micro- and nanoparticle shape on biological processes. J. Control. Release 2022, 342, 93–110. [Google Scholar] [CrossRef]
- Gatoo, M.A.; Naseem, S.; Arfat, M.Y.; Dar, A.M.; Qasim, K.; Zubair, S. Physicochemical properties of nanomaterials: Implication in associated toxic manifestations. BioMed Res. Int. 2014, 2014, 498420. [Google Scholar] [CrossRef]
- Kerfahi, D.; Tripathi, B.M.; Singh, D.; Kim, H.; Lee, S.; Lee, J.; Adams, J.M. Effects of functionalized and raw multi-walled carbon nanotubes on soil bacterial community composition. PLoS ONE 2015, 10, e0123042. [Google Scholar] [CrossRef]
- Sohn, E.K.; Chung, Y.S.; Johari, S.A.; Kim, T.G.; Kim, J.K.; Lee, J.H.; Lee, Y.H.; Kang, S.W.; Yu, I.J. Acute toxicity comparison of single-walled carbon nanotubes in various freshwater organisms. BioMed Res. Int. 2015, 2015, 323090. [Google Scholar] [CrossRef]
- Choi, S.J.; Oh, J.M.; Choy, J.H. Toxicological effects of inorganic nanoparticles on human lung cancer A549 cells. J. Inorg. Biochem. 2009, 103, 463–471. [Google Scholar] [CrossRef] [PubMed]
- Fu, P.P.; Xia, Q.; Hwang, H.M.; Ray, P.C.; Yu, H. Mechanisms of nanotoxicity: Generation of reactive oxygen species. J. Food Drug Anal. 2014, 22, 64–75. [Google Scholar] [CrossRef] [PubMed]
- Schaeublin, N.M.; Braydich-Stolle, L.K.; Schrand, A.M.; Miller, J.M.; Hutchison, J.; Schlager, J.J.; Hussain, S.M. Surface charge of gold nanoparticles mediates mechanism of toxicity. Nanoscale 2011, 3, 410–420. [Google Scholar] [CrossRef] [PubMed]
- Tomita, Y.; Rikimaru-Kaneko, A.; Hashiguchi, K.; Shirotake, S. Effect of anionic and cationic n-butylcyanoacrylate nanoparticles on NO and cytokine production in Raw264.7 cells. Immunopharmacol. Immunotoxicol. 2011, 33, 730–737. [Google Scholar] [CrossRef] [PubMed]
- Hanot, C.C.; Choi, Y.S.; Anani, T.B.; Soundarrajan, D.; David, A.E. Effects of Iron-Oxide Nanoparticle Surface Chemistry on Uptake Kinetics and Cytotoxicity in CHO-K1 Cells. Int. J. Mol. Sci. 2015, 17, 54. [Google Scholar] [CrossRef]
- Shukla, S.; Eber, F.J.; Nagarajan, A.S.; DiFranco, N.A.; Schmidt, N.; Wen, A.M.; Eiben, S.; Twyman, R.M.; Wege, C.; Steinmetz, N.F. The Impact of Aspect Ratio on the Biodistribution and Tumor Homing of Rigid Soft-Matter Nanorods. Adv. Health Mater. 2015, 4, 874–882. [Google Scholar] [CrossRef]
- Fubini, B.; Fenoglio, I.; Tomatis, M.; Turci, F. Effect of chemical composition and state of the surface on the toxic response to high aspect ratio nanomaterials. Nanomedicine 2011, 6, 899–920. [Google Scholar] [CrossRef]
- Gunay, M.S.; Ozer, A.Y.; Chalon, S. Drug Delivery Systems for Imaging and Therapy of Parkinson’s Disease. Curr. Neuropharmacol. 2016, 14, 376–391. [Google Scholar] [CrossRef]
- Iwamoto, T. Clinical application of drug delivery systems in cancer chemotherapy: Review of the efficacy and side effects of approved drugs. Biol. Pharm. Bull. 2013, 36, 715–718. [Google Scholar] [CrossRef]
- Wang, J.; Mongayt, D.; Torchilin, V.P. Polymeric micelles for delivery of poorly soluble drugs: Preparation and anticancer activity in vitro of paclitaxel incorporated into mixed micelles based on poly(ethylene glycol)-lipid conjugate and positively charged lipids. J. Drug Target 2005, 13, 73–80. [Google Scholar] [CrossRef]
- Rau, K.-M.; Lin, Y.-C.; Chen, Y.-Y.; Chen, J.-S.; Lee, K.-D.; Wang, C.-H.; Chang, H.-K. Pegylated liposomal doxorubicin (Lipo-Dox®) combined with cyclophosphamide and 5-fluorouracil is effective and safe as salvage chemotherapy in taxane-treated metastatic breast cancer: An open-label, multi-center, non-comparative phase II study. BMC Cancer 2015, 15, 423. [Google Scholar] [CrossRef]
- Casagrande, N.; Celegato, M.; Borghese, C.; Mongiat, M.; Colombatti, A.; Aldinucci, D. Preclinical activity of the liposomal cisplatin lipoplatin in ovarian cancer. Clin. Cancer Res. 2014, 20, 5496–5506. [Google Scholar] [CrossRef]
- Guo, S.; Huang, L. Nanoparticles containing insoluble drug for cancer therapy. Biotechnol. Adv. 2014, 32, 778–788. [Google Scholar] [CrossRef]
- Deshpande, P.P.; Biswas, S.; Torchilin, V.P. Current trends in the use of liposomes for tumor targeting. Nanomedicine 2013, 8, 1509–1528. [Google Scholar] [CrossRef]
- Marques-Gallego, P.; de Kroon, A.I. Ligation strategies for targeting liposomal nanocarriers. BioMed Res. Int. 2014, 2014, 129458. [Google Scholar] [CrossRef]
- Gai, M.; Simon, J.; Lieberwirth, I.; Mailänder, V.; Morsbach, S.; Landfester, K. A bio-orthogonal functionalization strategy for site-specific coupling of antibodies on vesicle surfaces after self-assembly. Polym. Chem. 2020, 11, 527–540. [Google Scholar] [CrossRef]
- O’Brien, M.E.; Wigler, N.; Inbar, M.; Rosso, R.; Grischke, E.; Santoro, A.; Catane, R.; Kieback, D.G.; Tomczak, P.; Ackland, S.P.; et al. Reduced cardiotoxicity and comparable efficacy in a phase III trial of pegylated liposomal doxorubicin HCl (CAELYX/Doxil) versus conventional doxorubicin for first-line treatment of metastatic breast cancer. Ann. Oncol. 2004, 15, 440–449. [Google Scholar] [CrossRef]
- Udhrain, A.; Skubitz, K.M.; Northfelt, D.W. Pegylated liposomal doxorubicin in the treatment of AIDS-related Kaposi’s sarcoma. Int. J. Nanomed. 2007, 2, 345–352. [Google Scholar]
- Mishra, P.; Nayak, B.; Dey, R. PEGylation in anti-cancer therapy: An overview. Asian J. Pharm. Sci. 2016, 11, 337–348. [Google Scholar] [CrossRef]
- Accardo, A.; Salsano, G.; Morisco, A.; Aurilio, M.; Parisi, A.; Maione, F.; Cicala, C.; Tesauro, D.; Aloj, L.; De Rosa, G.; et al. Peptide-modified liposomes for selective targeting of bombesin receptors overexpressed by cancer cells: A potential theranostic agent. Int. J. Nanomed. 2012, 7, 2007–2017. [Google Scholar] [CrossRef]
- Nicolas, J.; Mura, S.; Brambilla, D.; Mackiewicz, N.; Couvreur, P. Design, functionalization strategies and biomedical applications of targeted biodegradable/biocompatible polymer-based nanocarriers for drug delivery. Chem. Soc. Rev. 2013, 42, 1147–1235. [Google Scholar] [CrossRef]
- Liu, J.; Huang, Y.; Kumar, A.; Tan, A.; Jin, S.; Mozhi, A.; Liang, X.J. pH-sensitive nano-systems for drug delivery in cancer therapy. Biotechnol. Adv. 2014, 32, 693–710. [Google Scholar] [CrossRef] [PubMed]
- Cheung, R.C.; Ng, T.B.; Wong, J.H.; Chan, W.Y. Chitosan: An Update on Potential Biomedical and Pharmaceutical Applications. Mar. Drugs 2015, 13, 5156–5186. [Google Scholar] [CrossRef] [PubMed]
- Bouissou, C.; Rouse, J.J.; Price, R.; van der Walle, C.F. The influence of surfactant on PLGA microsphere glass transition and water sorption: Remodeling the surface morphology to attenuate the burst release. Pharm. Res. 2006, 23, 1295–1305. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.S.; Gao, Z.; Kim, D.; Park, K.; Kwon, I.C.; Bae, Y.H. Super pH-sensitive multifunctional polymeric micelle for tumor pH(e) specific TAT exposure and multidrug resistance. J. Control. Release 2008, 129, 228–236. [Google Scholar] [CrossRef]
- Lee, E.S.; Na, K.; Bae, Y.H. Doxorubicin loaded pH-sensitive polymeric micelles for reversal of resistant MCF-7 tumor. J. Control. Release 2005, 103, 405–418. [Google Scholar] [CrossRef]
- Broaders, K.E.; Grandhe, S.; Frechet, J.M. A biocompatible oxidation-triggered carrier polymer with potential in therapeutics. J. Am. Chem. Soc. 2011, 133, 756–758. [Google Scholar] [CrossRef]
- Kim, S.K.; Huang, L. Nanoparticle delivery of a peptide targeting EGFR signaling. J. Control. Release 2012, 157, 279–286. [Google Scholar] [CrossRef]
- Sun, L.C.; Coy, D.H. Somatostatin receptor-targeted anti-cancer therapy. Curr. Drug Deliv. 2011, 8, 2–10. [Google Scholar] [CrossRef]
- Kang, M.H.; Park, M.J.; Yoo, H.J.; Hyuk, K.Y.; Lee, S.G.; Kim, S.R.; Yeom, D.W.; Kang, M.J.; Choi, Y.W. RIPL peptide (IPLVVPLRRRRRRRRC)-conjugated liposomes for enhanced intracellular drug delivery to hepsin-expressing cancer cells. Eur. J. Pharm. Biopharm. 2014, 87, 489–499. [Google Scholar] [CrossRef]
- Wang, T.; Rong, F.; Tang, Y.; Li, M.; Feng, T.; Zhou, Q.; Li, P.; Huang, W. Targeted polymer-based antibiotic delivery system: A promising option for treating bacterial infections via macromolecular approaches. Prog. Polym. Sci. 2021, 116, 101389. [Google Scholar] [CrossRef]
- Carvalho, M.R.; Reis, R.L.; Oliveira, J.M. Dendrimer nanoparticles for colorectal cancer applications. J. Mater. Chem. B 2020, 8, 1128–1138. [Google Scholar] [CrossRef]
- Song, C.; Shen, M.; Rodrigues, J.; Mignani, S.; Majoral, J.-P.; Shi, X. Superstructured poly(amidoamine) dendrimer-based nanoconstructs as platforms for cancer nanomedicine: A concise review. Coord. Chem. Rev. 2020, 421, 213463. [Google Scholar] [CrossRef]
- Ventola, C.L. The Nanomedicine Revolution: Part 1: Emerging Concepts. Pharm. Ther. 2012, 37, 512–525. [Google Scholar]
- Murthy, S.K. Nanoparticles in modern medicine: State of the art and future challenges. Int. J. Nanomed. 2007, 2, 129–141. [Google Scholar]
- Bao, G.; Mitragotri, S.; Tong, S. Multifunctional nanoparticles for drug delivery and molecular imaging. Annu. Rev. Biomed Eng. 2013, 15, 253–282. [Google Scholar] [CrossRef]
- Vance, M.E.; Kuiken, T.; Vejerano, E.P.; McGinnis, S.P.; Hochella, M.F., Jr.; Rejeski, D.; Hull, M.S. Nanotechnology in the real world: Redeveloping the nanomaterial consumer products inventory. Beilstein J. Nanotechnol. 2015, 6, 1769–1780. [Google Scholar] [CrossRef]
- Liu, C.; Miyajima, T.; Melangath, G.; Miyai, T.; Vasanth, S.; Deshpande, N.; Kumar, V.; Ong Tone, S.; Gupta, R.; Zhu, S.; et al. Ultraviolet A light induces DNA damage and estrogen-DNA adducts in Fuchs endothelial corneal dystrophy causing females to be more affected. Proc. Natl. Acad. Sci. USA 2020, 117, 573–583. [Google Scholar] [CrossRef]
- Tang, J.; Lu, X.; Chen, B.; Cai, E.; Liu, W.; Jiang, J.; Chen, F.; Shan, X.; Zhang, H. Mechanisms of silver nanoparticles-induced cytotoxicity and apoptosis in rat tracheal epithelial cells. J. Toxicol. Sci. 2019, 44, 155–165. [Google Scholar] [CrossRef]
- Salehi, F.; Behboudi, H.; Kavoosi, G.; Ardestani, S.K. Oxidative DNA damage induced by ROS-modulating agents with the ability to target DNA: A comparison of the biological characteristics of citrus pectin and apple pectin. Sci. Rep. 2018, 8, 13902. [Google Scholar] [CrossRef]
- León-Silva, S.; Fernández-Luqueño, F.; López-Valdez, F. Silver Nanoparticles (AgNP) in the environment: A review of potential risks on human and environmental health. Water Air Soil Pollut. 2016, 227, 306. [Google Scholar] [CrossRef]
- Yusuf, A.; Brophy, A.; Gorey, B.; Casey, A. Liposomal encapsulation of silver nanoparticles enhances cytotoxicity and causes induction of reactive oxygen species-independent apoptosis. J. Appl. Toxicol. 2018, 38, 616–627. [Google Scholar] [CrossRef] [PubMed]
- Yusuf, A.; Casey, A. Liposomal encapsulation of silver nanoparticles (AgNP) improved nanoparticle uptake and induced redox imbalance to activate caspase-dependent apoptosis. Apoptosis 2020, 25, 120–134. [Google Scholar] [CrossRef] [PubMed]
- Yusuf, A.; Casey, A. Surface modification of silver nanoparticle (AgNP) by liposomal encapsulation mitigates AgNP-induced inflammation. Toxicol. Vitr. 2019, 61, 104641. [Google Scholar] [CrossRef] [PubMed]
- Khan, I.; Saeed, K.; Khan, I. Nanoparticles: Properties, applications and toxicities. Arab. J. Chem. 2019, 12, 908–931. [Google Scholar] [CrossRef]

| Trade Name (Manufacturer) | Component | Delivery Method | Indication(s) | Approval Year | References | |
|---|---|---|---|---|---|---|
| Liposomal nanoparticle | AmBIsome (Gilead Sciences, Foster City, CA, USA) | Amphotericin B in liposome | Intravenous infusion | Fungal/protozoal infections | 1991 | [44] |
| Onivyde (Ipsen Biopharmaceuticals, Paris France) | Irinotecan in liposome | Intravenous injection | Metastatic adenocarcinoma of the pancreas | 2015 | [45] | |
| Vyxeos (Jazz Pharmaceuticals, Dublin Ireland) | Daunorubicin and cytarabine in liposome | intramuscular, intrathecal, or subcutaneous injection | AML, AML due to previous cancer therapy, AML with myelodysplasia related changes | 2017 | [46] | |
| Doxil (Janssen, Beerse Belgium) | Doxorubicin-HCl in liposome | Intravenous infusion | Multiple myeloma Kaposi’s sarcoma and Ovarian cancer | 1995 | [47] | |
| Marqibo (Spectrum Pharmaceuticals, Boston, MA, USA) | Vincristine in liposome | Intravenous injection | ALL | 2012 | [48] | |
| DepoDur (Pacira Pharmaceuticals, San Diego, CA, USA) | Orphine sulphate in liposome | Epidural administration | Postoperative pain | 2011 | [49] | |
| Visudyne (Bausch and Lomb, Vaughan, ON, Canada) | Verteporfin in liposome | Intravenous injection | subfoveal choroidal neovascularization due to AMD, myopia | 2000 | [50] | |
| Polymer NPs | Adagen (Leadiant Biosciences, Gaithersburg, MD, USA) | Pegademase bovine | intramuscular injection | SCID | 1990 | [51] |
| Plegridy (Biogen, Cambridge, MA, USA) | Pegylated IFN-β-1a | Subcutaneous injection | Multiple sclerosis | 2014 | [41] | |
| Somavert (Pfizer, New York, NY, USA) | Pegvisomant | Subcutaneous injection | Acromegaly | 2007 | [52] | |
| Eligard (Tolmar, Chicago, IL, USA) | Leuprolide acetate and polymer | Subcutaneous injection | Prostate cancer | 2003 | [53] | |
| Cimzia (UCB, Brussels, Belgium) | Certolizumab pegol | Pills or intravenous injection | Rheumatoid arthritis, Crohn’s disease, psoriatic arthritis, ankylosing spondylitis | 2009 | [54] | |
| Macugen (Bausch and Lomb, Vaughan, ON, Canada) | Pegaptinib | Intravitreal injections | Neovascular AMD | 2004 | [55] | |
| Neulasta (Amgen, C Thousand Oaks, CA, USA) | Pegfilgrastim | On-body injection | Chemotherapy-induced neutropenia | 2002 | [56] | |
| Pegasys (Genentech, Souht San Francisco, CA, USA) | Pegylated IFN alpha-2a | Subcutaneous injection | Hepatitis B, hepatitis C | 2002 | [51] | |
| PegIntron (Merck, Kenilworth, NY, USA) | Pegylated IFN alpha-2b | Subcutaneous injection | Hepatitis C | 2001 | [57] | |
| Copaxone (Teva, Tel Aviv Israel) | Glatimer acetate | Subcutaneous injection | Multiple sclerosis | 1996 | [58] | |
| Rebinyn (Novo Nordisk, Bagsværd, Denmark) | Coagulation factor IX (recombinant), glycopegylated | Intravenous injection | Haemophilia B | 2008 | [41] | |
| Zilretta (Flexion Therapeutics, Woburn, MA, USA) | Triamcinolone acetonide | Intra-articular injection | Osteoarthritis knee pain | 2017 | [41] | |
| Micellar NPs | Abraxane (Celgene, Summit, NJ, USA) | Micellar containing paclitaxel | Intravenous | breast cancer, non-small cell lung cancer, pancreatic cancer, and ovarian cancer | 2005 | [41] |
| Nanocrystal nanoparticles | Rapamune (Wyeth Pharmaceuticals, Madison, WI, USA) | Sirolimus | Oral administration | Immunosuppressant | 1999 | [41] |
| Emend (Merck, Kenilworth, NJ, USA) | Aprepitant | Oral administration | Antiemetic | 2003 | [59] | |
| Focalin (Novartis, Cambridge, MA, USA) | Dexamethylphenidate HCl | Intravenous injection | Psychostimulant | 2002 | [60] | |
| Invega Sustenna (Janssen, Beerse Belgium) | Paliperidone palmitate | Intramuscular injection | Schizophrenia, schizoaffective disorder | 2009 | [61] | |
| Zanaflex (Acorda, Ardsley, NY, USA) | Tizanidine HCl | Oral administration | Muscle relaxant | 1997 | [62] | |
| Ritalin (Novartis, Cambridge, MA, USA) | Methylphenidate HCl | Oral administration | Attention deficit hyperactivity disorder and narcolepsy | 1955 | [63] | |
| Avinza (Pfizer, New York City, NY, USA) | Morphine sulfate | Oral administration | Severe pain | 2002 | [64] | |
| Tricor (AbbVie, Chicago, IL, USA) | Fenofibrate | Oral administration | Hyper-lipidemia | 1998 | [41] | |
| Inorganic nanoparticles | Dexferrum (American Regent, Shirley, NY, USA) | Iron dextran | Intravenous injection | Iron deficiency | 2009 | [65] |
| Venofer (Vifor Pharma, Zurich Switzerland) | Iron sucrose | Intravenous injection | Iron deficiency in CKD, IBD | 2000 | [66] | |
| Ferrlecit (Sanofi-Aventis, Paris France) | Sodium ferric gluconate complex in sucrose | Intravenous infusion | Iron deficiency in CKD | 1999 | [66] | |
| Onpattro (Alnylam Pharmaceuticals, Cambridge, MA, USA) | Antisense mRNA to the transthyretin (TTR) gene | subcutaneous injection | caused by hereditary transthyretin-mediated amyloidosis (hATTR) | 2018 | [67] | |
| Feraheme (AMAG Pharmaceuticals, Cambridge, MA, USA) | Ferumoxytol | Intravenous infusion | Iron deficiency in CKD | 2009 | [68] |
| Nanoparticle type | Characteristics | Benefits | Applications |
|---|---|---|---|
| Liposomes | Spherical structures made of a lipid bilayer that encapsulates drugs and protects them from degradation. They are biocompatible and can be easily functionalized with targeting moieties for a specific delivery. | Can encapsulate hydrophilic and hydrophobic drugs, biodegradable and biocompatible; can target specific tissues | Drug delivery, gene therapy, vaccine delivery |
| Dendrimers | Highly branched, monodisperse nanoscale polymers that can be used as drug carriers. They are highly customizable, with a range of sizes, surface functionalities, and drug-loading capacities. | Can be designed to have specific sizes and shapes, high drug loading capacity; can target specific tissues | Drug delivery, gene therapy, imaging |
| Polymeric nanoparticles | Made from biodegradable polymers that can encapsulate drugs and protect them from degradation. They are often used for the sustained release of drugs over a period of time. | Can encapsulate hydrophilic and hydrophobic drugs; can be functionalized with targeting ligands or imaging agents, biocompatible | Drug delivery, gene therapy, imaging |
| Metal nanoparticles | Including gold nanoparticles (AuNP) and AgNP, have unique optical, electronic, and thermal properties that make them attractive for use in drug delivery. They can be functionalized with targeting moieties for a specific delivery. | Unique optical and magnetic properties; can be functionalized with targeting ligands or imaging agents; biocompatible | Imaging, cancer therapy, biosensors |
| Solid lipid nanoparticles: | Made of solid lipids and are used to encapsulate hydrophobic drugs. They offer a number of advantages over other types of nanoparticles, including stability, biocompatibility, and improved bioavailability. | Can encapsulate hydrophilic and hydrophobic drugs, biocompatible; can be functionalized with targeting ligands or imaging agents | Drug delivery, cosmetic, and personal care products |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yusuf, A.; Almotairy, A.R.Z.; Henidi, H.; Alshehri, O.Y.; Aldughaim, M.S. Nanoparticles as Drug Delivery Systems: A Review of the Implication of Nanoparticles’ Physicochemical Properties on Responses in Biological Systems. Polymers 2023, 15, 1596. https://doi.org/10.3390/polym15071596
Yusuf A, Almotairy ARZ, Henidi H, Alshehri OY, Aldughaim MS. Nanoparticles as Drug Delivery Systems: A Review of the Implication of Nanoparticles’ Physicochemical Properties on Responses in Biological Systems. Polymers. 2023; 15(7):1596. https://doi.org/10.3390/polym15071596
Chicago/Turabian StyleYusuf, Azeez, Awatif Rashed Z. Almotairy, Hanan Henidi, Ohoud Y. Alshehri, and Mohammed S. Aldughaim. 2023. "Nanoparticles as Drug Delivery Systems: A Review of the Implication of Nanoparticles’ Physicochemical Properties on Responses in Biological Systems" Polymers 15, no. 7: 1596. https://doi.org/10.3390/polym15071596
APA StyleYusuf, A., Almotairy, A. R. Z., Henidi, H., Alshehri, O. Y., & Aldughaim, M. S. (2023). Nanoparticles as Drug Delivery Systems: A Review of the Implication of Nanoparticles’ Physicochemical Properties on Responses in Biological Systems. Polymers, 15(7), 1596. https://doi.org/10.3390/polym15071596





