Fracture Resistance Comparative Analysis of Milled-Derived vs. 3D-Printed CAD/CAM Materials for Single-Unit Restorations
Abstract
:1. Introduction
1.1. PMMA
1.2. 3DPPa
1.3. 3DPPb
2. Materials and Methods
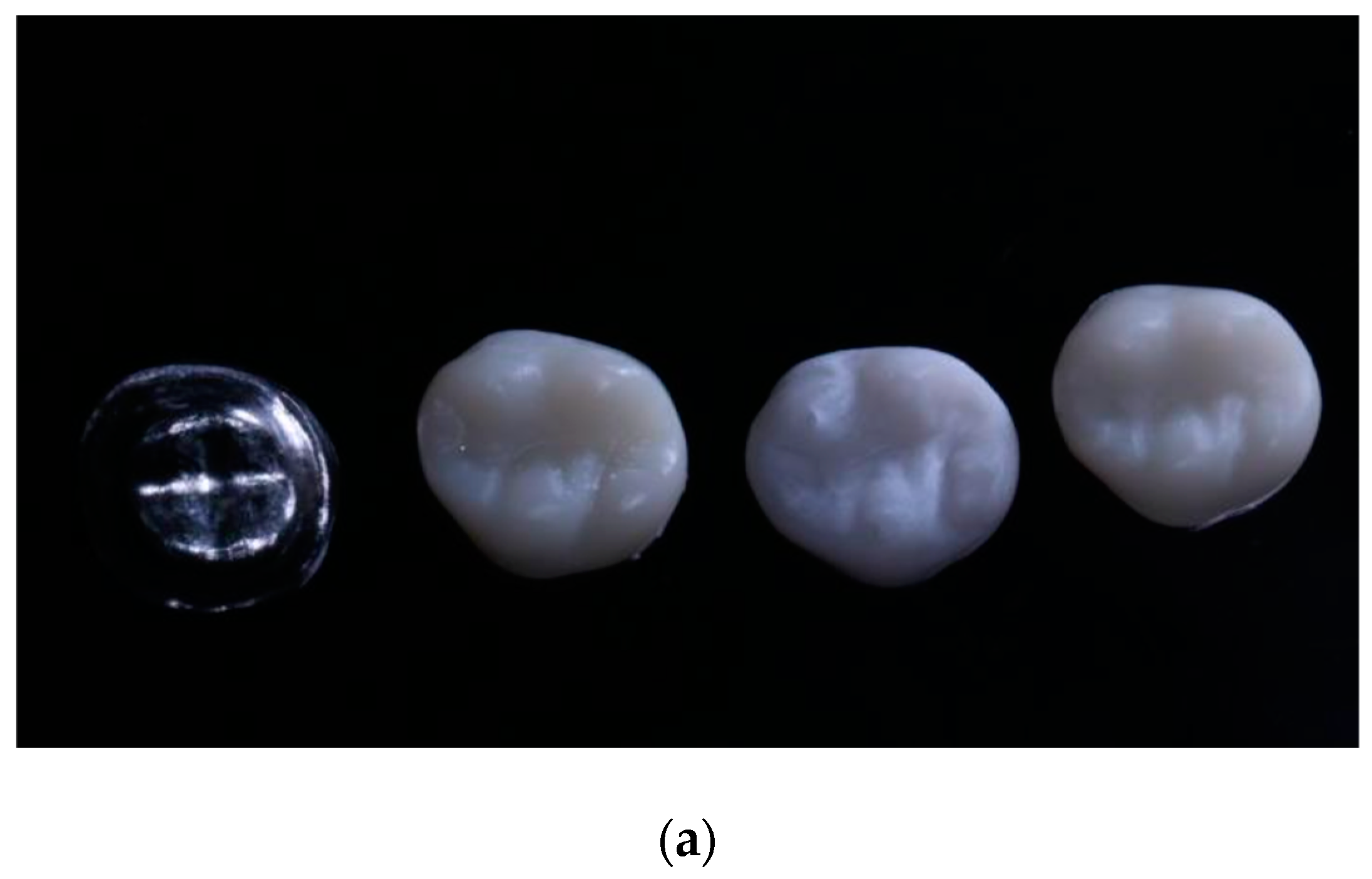
2.1. Sample Preparation
2.2. PMMA Samples
2.3. 3D-Printed Crowns
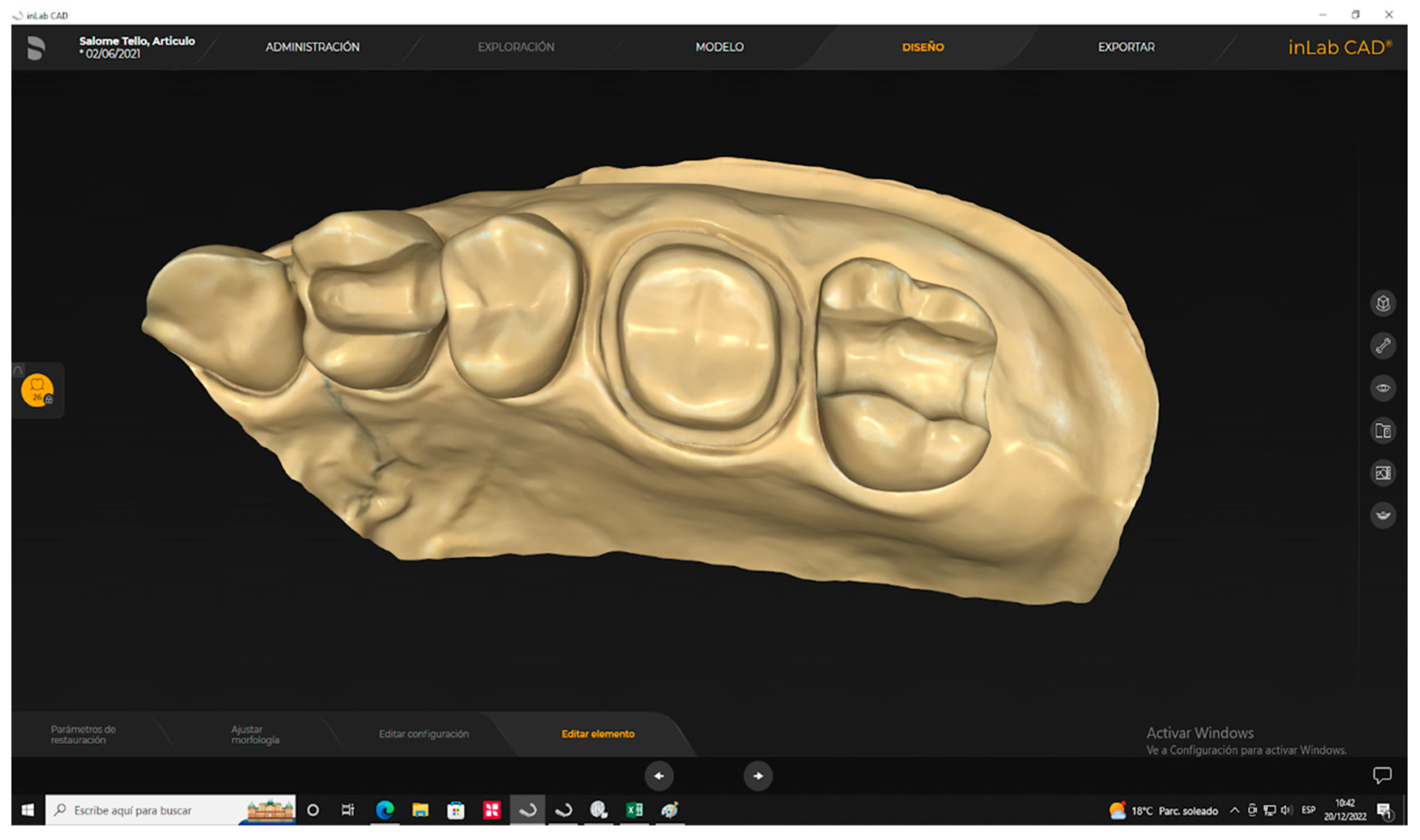
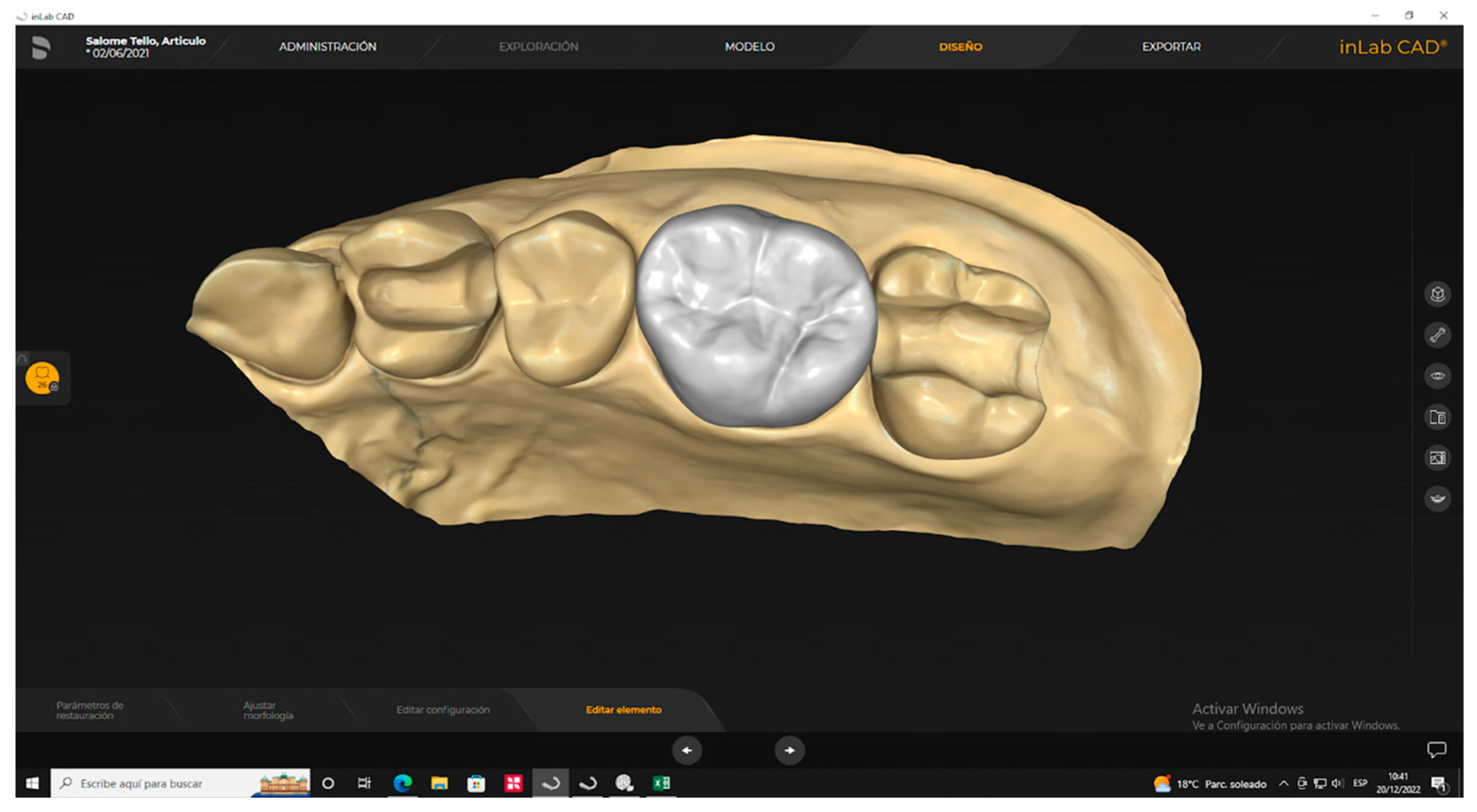
2.3.1. Digitalization Scanning and Design of Samples
2.3.2. 3D-Printed Materialization
2.3.3. Postproduction
2.4. Thermocycling of Samples
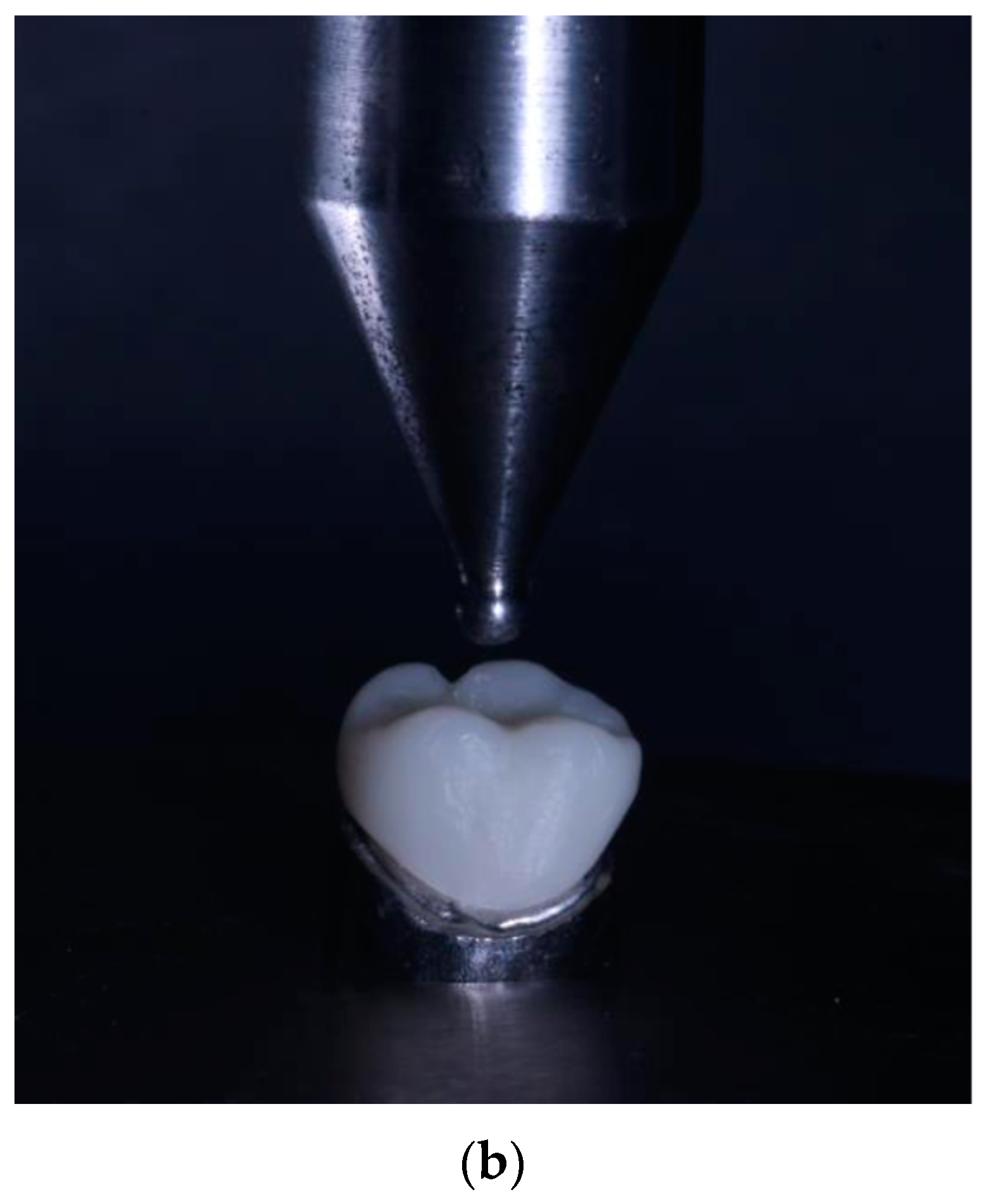
2.5. Fracture Resistance Test
2.6. Data Processing and Analysis
3. Results
Descriptive Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Lambert, H.; Durand, J.-C.; Jacquot, B.; Fages, M. Dental biomaterials for chairside CAD/CAM: State of the art. J. Adv. Prosthodont. 2017, 9, 486–495. [Google Scholar] [CrossRef]
- Alp, G.; Murat, S.; Yilmaz, B. Comparison of Flexural Strength of Different CAD/CAM PMMA-Based Polymers. J. Prosthodont. 2018, 28, e491–e495. [Google Scholar] [CrossRef]
- Lerner, H.; Nagy, K.; Pranno, N.; Zarone, F.; Admakin, O.; Mangano, F. Trueness and precision of 3D-printed versus milled-derived monolithic zirconia crowns: An in vitro study. J. Dent. 2021, 113, 103792. [Google Scholar]
- Aneeza, H. Additive vs. Subtractive Manufacturing in Dental Laboratory Technology. CUNY Acad. Works 2021, 1, 1–2. [Google Scholar]
- Beuer, F.; Schweiger, J.; Edelhoff, D. Digital dentistry: An overview of recent developments for CAD/CAM generated restorations. Br. Dent. J. 2008, 204, 505–511. [Google Scholar] [CrossRef] [PubMed]
- Kessler, A.; Hickel, R.; Reymus, M. 3D-Printing in Dentistry-State of the Art. Oper Dent. 2020, 45, 30–40. [Google Scholar]
- Sabane, A.; Manaswita, Y.; Rohit, T.; Ravikiran, A. Impresion Makin in Fixed Partial Denture: Tradicional or Go Digital? IIOABJ 2017, 8, 38–43. [Google Scholar]
- Formlabs. Comparación de tecnologías de impresión 3D: FDM, SLA o SLS. 2023. Available online: https://formlabs.com/latam/blog/fdm-sla-sls-como-elegir-tecnologia-impresion-3d-adecuada/ (accessed on 15 April 2023).
- Sadid-Zadeh, R.; Zirkel, C.; Makwoka, S.; Li, R. Fracture Strength of Interim CAD/CAM and Conventional Partial Fixed Dental Prostheses. J. Prosthodont. 2021, 30, 720–724. [Google Scholar] [CrossRef] [PubMed]
- Ayatollahi, M.R.; Ghouli, S.; Bahrami, B. Experimental and theoretical fracture analyses for three biomaterials with dental applications. J. Mech. Behav. Biomed. Mater. 2020, 103, 103612. [Google Scholar] [CrossRef]
- Srinivasan, M.; Gjengedal, H.; Cattani-Lorente, M.; Moussa, M.; Durual, S.; Schimmel, M.; Müller, F. CAD/CAM milled-derived complete removable dental prostheses: An in vitro evaluation of biocompatibility, mechanical properties, and surface roughness. Dent. Mater. J. 2018, 37, 526–533. [Google Scholar]
- Al-Dwairi, Z.N.; Tahboub, K.Y.; Baba, N.Z.; Goodacre, C.J.; Özcan, M. A Comparison of the Surface Properties of CAD/CAM and Conventional Polymethylmethacrylate (PMMA). J. Prosthodont. 2019, 28, 452–457. [Google Scholar] [CrossRef]
- Karaman, T.; Eser, B.; Altintas, E.; Atala, M.H. Evaluation of the effects of finish line type and width on the fracture strength of provisional crowns. Odontology 2021, 109, 76–81. [Google Scholar] [CrossRef]
- Çakmak, G.; Yilmaz, H.; Aydoğ, Ö.; Yilmaz, B. Flexural strength of CAD-CAM and conventional interim resin materials with a surface sealant. J. Prosthet. Dent. 2020, 124, 800.e1–800.e7. [Google Scholar] [CrossRef] [PubMed]
- Abad-Coronel, C.; Carrera, E.; Mena, N.; Fajardo, J.; Aliaga, P. Comparative Analysis of Fracture Resistance between CAD/CAM Materials for Interim Fixed Prosthesis (Basel). Materials 2021, 14, 77–91. [Google Scholar]
- SprintRay. 3D-Printing Material Library by SprintRay. Resins Designed for Dental 3D-Printing. 2023. Available online: https://10.1016/j.prosdent.2021.11.005.sprintray.com/dental-3d-printing-materials/ (accessed on 12 May 2023).
- Raszewski, Z. Dynamics of different ion release from denture-base acrylic resins and their mechanical properties after the addition of bioactive materials. Saudi Dent. J. 2021, 33, 1071–1077. [Google Scholar] [CrossRef]
- Martín-Ortega, N.; Sallorenzo, A.; Casajús, J.; Cervera, A.; Revilla-León, M.; Gómez-Polo, M. Fracture resistance of additive manufactured and milled-derived implant-supported interim crowns. J. Prosthet. Dent. 2022, 127, 267–274. [Google Scholar]
- Reeponmaha, T.; Angwaravong, O.; Angwarawong, T. Comparison of fracture strength after thermo-mechanical aging between provisional crowns made with CAD/CAM and conventional method. J. Adv. Prosthodont. 2020, 12, 218–224. [Google Scholar]
- SprintRay, 3D-Printed Ceramic Crown Scientific Studies Summary. Fracture Load with 10-Year Chewing Simulation, Comparison of Milled-Derived and 3D-Printed Materials. 2023, p. 4. Available online: https://info.sprintray.com/hubfs/Ceramic_Crown_Study20230531B.pdf (accessed on 27 July 2023).
- Corbani, K.; Hardan, L.; Eid, R.; Skienhe, H.; Alharbi, N.; Ozcan, M.; Salameh, Z. Fracture Resistance of Three-unit Fixed Dental Prostheses Fabricated with Milled-Derived and 3D-Printed Composite-based Materials. J. Contemp. Dent. Pract. 2021, 22, 985–990. [Google Scholar] [PubMed]
- Freitas, R.F.C.P.; Duarte, S.; Feitosa, S.; Dutra, V.; Lin, W.S.; Panariello, B.H.D.; Carreiro, A.D.F.P. Physical, Mechanical, and Anti-Biofilm Formation Properties of CAD-CAM-Milled-Derived or 3D-Printed Denture Base Resins: In Vitro Analysis. J. Prosthodont. 2023, 32, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Farina, A.P.; Cecchin, D.; Soares, R.G.; Botelho, A.L.; Takahashi, J.M.F.K.; Mazzetto, M.O.; Mesquita, M.F. Evaluation of Vickers hardness of different types of acrylic denture base resins with and without glass fibre reinforcement. Gerodontology 2010, 29, e155–e160. [Google Scholar] [CrossRef]
- Al-Dwairi, Z.N.; Ebrahim, A.A.A.H.; Baba, N.Z. A Comparison of the Surface and Mechanical Properties of 3D Printable Denture-Base Resin Material and Conventional Polymethylmethacrylate (PMMA). J. Prosthodont. 2022, 32, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Raszewski, Z. Acrylic resins in the CAD/CAM technology: A systematic literature review. Dent. Med. Probl. 2020, 57, 449–454. [Google Scholar] [CrossRef]
- De Oliveira, E.; Zancanaro, E.; Spohr, A.M.; Lima, M. Properties of Acrylic Resin For CAD/CAM: A Systematic Review and Meta-Analysis of In Vitro Studies. J. Prosthodont. 2021, 30, 656–664. [Google Scholar] [PubMed]
- Pantea, M.; Ciocoiu, R.C.; Greabu, M.; Totan, A.R.; Imre, M.; Țâncu, A.M.C.; Sfeatcu, R.; Spînu, T.C.; Ilinca, R.; Petre, A.E. Compressive and Flexural Strength of 3D-Printed and Conventional Resins Designated for Interim Fixed Dental Prostheses: An In Vitro Comparison. Materials 2022, 15, 3075. [Google Scholar] [CrossRef]
- Fasbinder, D.J. Digital dentistry: Innovation for restorative treatment. Compend. Contin. Educ. Dent. 2010, 4, 2–12. [Google Scholar]
- Corbani, K.; Hardan, L.; Skienhe, H.; Özcan, M.; Alharbi, N.; Salameh, Z. Effect of material thickness on the fracture resistance and failure pattern of 3D-printed composite crowns. Int. J. Comput. Dent. 2020, 23, 225–233. [Google Scholar] [PubMed]
- Jockin, S.; Thanos, K.; Kurtzman, G. Using a Printed, Ceramic-Based Resin for Anterior and Posterior Final Crowns. 2023. Available online: https://www.dentistrytoday.com/using-a-printed-ceramic-based-resin-for-anterior-and-posterior-final-crowns/ (accessed on 12 May 2023).
- Jerman, E.; Eichberger, M.; Schönhoff, L.; Reymus, M.; Stawarczyk, B. Department of Prosthetic Dentistry: University Hospital. Munich, Germany. 2020. Breaking Load and Abrasion Resistance 10-Year Chewing Simulation Based on the Scientific Study Fracture Load and Two-Body Wear of 3D-Printed and Conventionally Fabricated Crowns: Artificial Aging of 10 In-Vivo Years. Available online: https://docplayer.net/201931907-Varseosmile-crown-plus.html (accessed on 14 March 2021).
- Jasiūnaitė, A.; Verenis, A.M.; Ivanauskienė, E.; Žilinskas, J. A comparison of mechanic properties regarding complete removable dentures, which were made from polymethylmethacrilate (PMMA) during conventional and CAD/CAM processes. Systemic literature review. Stomatologija 2022, 24, 3–12. [Google Scholar] [PubMed]
- Valenti, C.; Federici, I.; Masciotti, F.; Marinucci, L.; Xhimitiku, I.; Cianetti, S.; Pagano, S. Mechanical properties of 3D-printed prosthetic materials compared with milled-derived and conventional processing: A systematic review and meta-analysis of in vitro studies. J. Prosthet. Dent. 2022, 22, 41–52. [Google Scholar]
- Abualsaud, R.; Gad, M.M. Flexural strength of CAD/CAM denture base materials: Systematic review and meta-analysis of in-vitro studies. J. Int. Soc. Prev. Community Dent. 2022, 12, 160–170. [Google Scholar] [CrossRef]
- Arslan, M.; Murat, S.; Alp, G.; Zaimoglu, A. Evaluation of flexural strength and surface properties of prepolymerized CAD/CAM PMMA-based polymers used for digital 3D complete dentures. Int. J. Comput. Dent. 2018, 21, 31–40. [Google Scholar]
- Jovanović, M.; Živić, M.; Milosavljević, M. A Potential Application of Materials Based on a Polymer and CAD/CAM Composite Resins in Prosthetic Dentistry. J. Prosthodont. Res. 2021, 65, 137–147. [Google Scholar] [CrossRef] [PubMed]
- Paradowska-Stolarz, A.; Malysa, A.; Mikulewicz, M. Comparison of the Compression and Tensile Modulus of Two Chosen Resins Used in Dentistry for 3D Printing. Materials 2022, 15, 8956. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.C.; Li, R.; Zhou, Y.S.; Wang, Y. Application and outlook of three-dimensional printing in prosthetic dentistry. Zhonghua Kou Qiang Yi Xue Za Zhi 2017, 52, 381–385. [Google Scholar] [PubMed]


| Product Name | Manufacturer’s Brand | Lot | Material |
|---|---|---|---|
| 3DPPa | SprintRay (Los Angeles, CA, USA) | 600,663 | Hybrid material for dental 3D-crown printing |
| PMMA | Ivoclar Vivadent (Lichtenstein) | 48,820 | Thermoplastic polymer |
| 3DPPb | SprintRay | 0202021 | Nano ceramic hybrid, 3D-printing |
| Material | n | Mean (x) | Standard Deviation (sd) | Coefficient of Variation (cv) | Minimum | Maximum | Ci 95% for the Mean |
|---|---|---|---|---|---|---|---|
| PMMA | 20 | 1427.9 | 36.9 | 3.2% | 1368.8 | 1486.8 | (1410.6; 1445.2) |
| 3DPPa | 20 | 1231.0 | 380.1 | 30.9% | 622.8 | 1848.4 | (1053.1; 1408.9) |
| 3DPPb | 20 | 1029.9 | 166.4 | 16.2% | 786.1 | 1282.2 | (952.0; 1107.8) |
| Sample 1—Sample 2 | Test Statistic | Deviation from Test Statistic | p-Value |
|---|---|---|---|
| 3DPPb—3DPPa | 14.150 | 2.562 | 0.010 |
| 3DPPb—PMMA | −26.500 | −4.798 | 0.000 |
| 3DPPa—PMMA | −12.350 | −2.236 | 0.025 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abad-Coronel, C.; Bravo, M.; Tello, S.; Cornejo, E.; Paredes, Y.; Paltan, C.A.; Fajardo, J.I. Fracture Resistance Comparative Analysis of Milled-Derived vs. 3D-Printed CAD/CAM Materials for Single-Unit Restorations. Polymers 2023, 15, 3773. https://doi.org/10.3390/polym15183773
Abad-Coronel C, Bravo M, Tello S, Cornejo E, Paredes Y, Paltan CA, Fajardo JI. Fracture Resistance Comparative Analysis of Milled-Derived vs. 3D-Printed CAD/CAM Materials for Single-Unit Restorations. Polymers. 2023; 15(18):3773. https://doi.org/10.3390/polym15183773
Chicago/Turabian StyleAbad-Coronel, Cristian, Manuel Bravo, Salomé Tello, Emilia Cornejo, Yirelly Paredes, Cesar A. Paltan, and Jorge I. Fajardo. 2023. "Fracture Resistance Comparative Analysis of Milled-Derived vs. 3D-Printed CAD/CAM Materials for Single-Unit Restorations" Polymers 15, no. 18: 3773. https://doi.org/10.3390/polym15183773
APA StyleAbad-Coronel, C., Bravo, M., Tello, S., Cornejo, E., Paredes, Y., Paltan, C. A., & Fajardo, J. I. (2023). Fracture Resistance Comparative Analysis of Milled-Derived vs. 3D-Printed CAD/CAM Materials for Single-Unit Restorations. Polymers, 15(18), 3773. https://doi.org/10.3390/polym15183773












