Trueness, Flexural Strength, and Surface Properties of Various Three-Dimensional (3D) Printed Interim Restorative Materials after Accelerated Aging
Abstract
1. Introduction
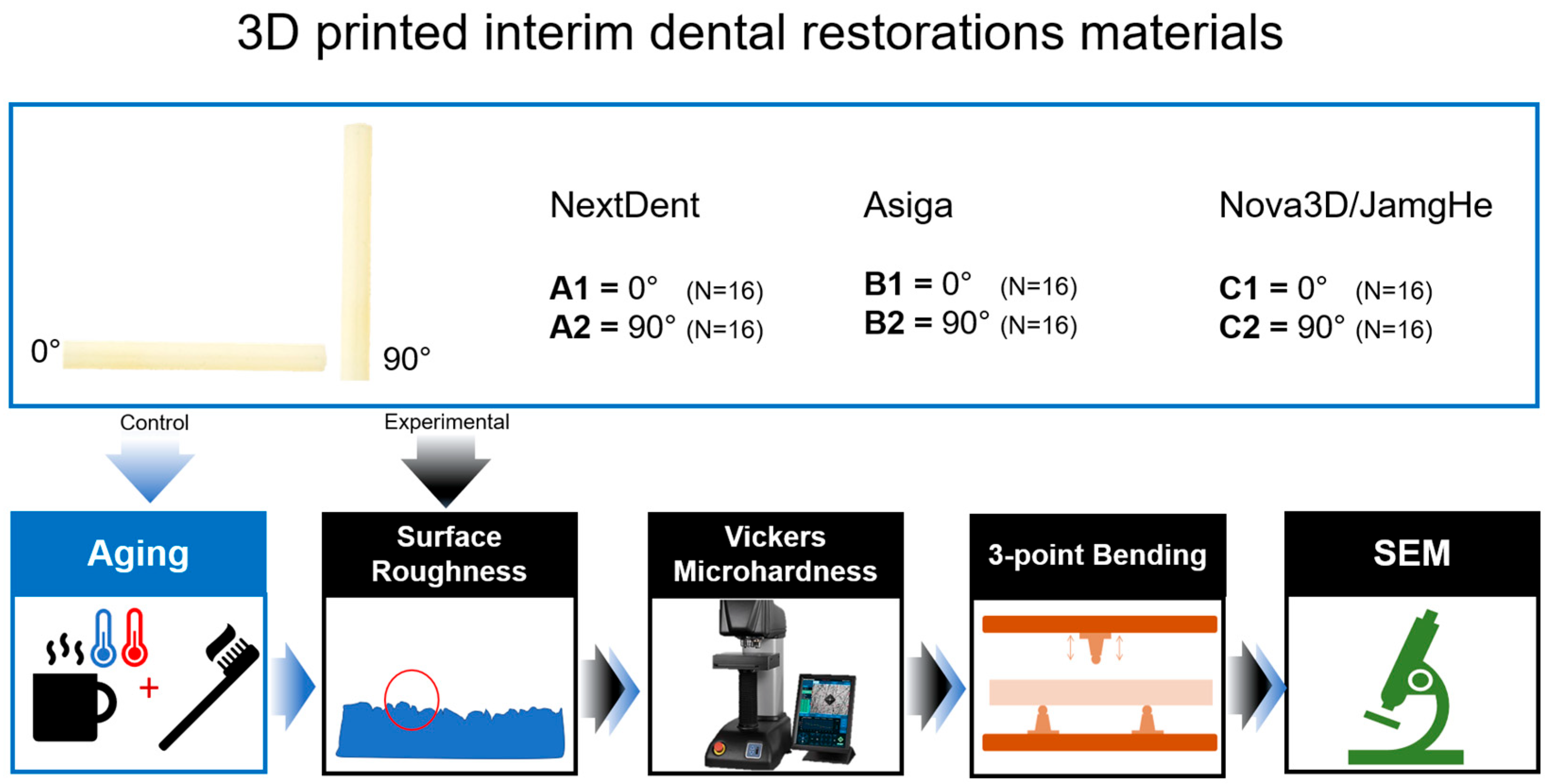
2. Materials and Methods
2.1. Specimen Preparation
2.2. Accelerated Aging Treatment
2.3. Trueness Assessment
2.4. Surface Roughness Assessment
2.5. Microhardness Assessment
2.6. Mechanical Testing
2.7. Statistical Analyses
3. Results
3.1. Trueness
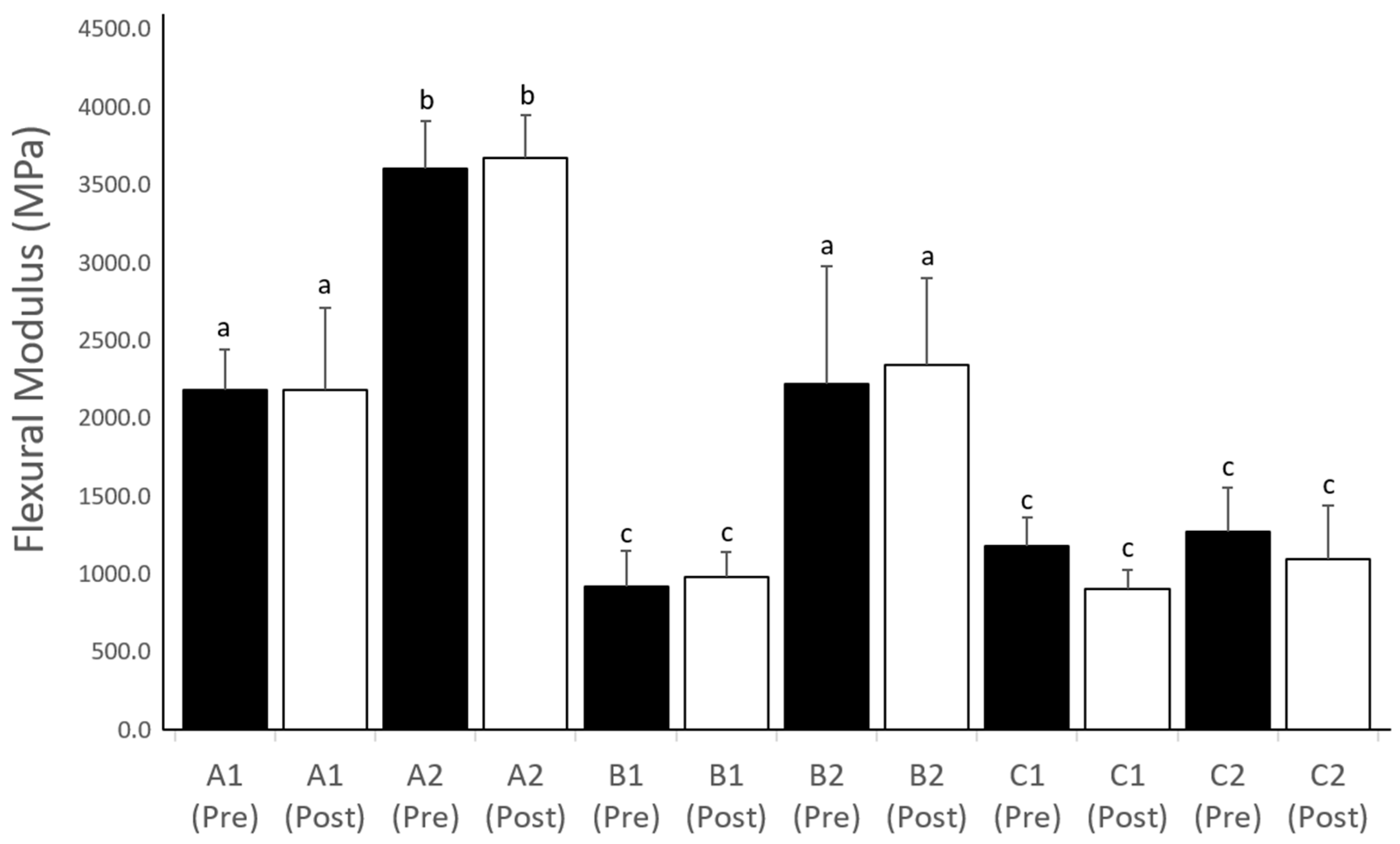
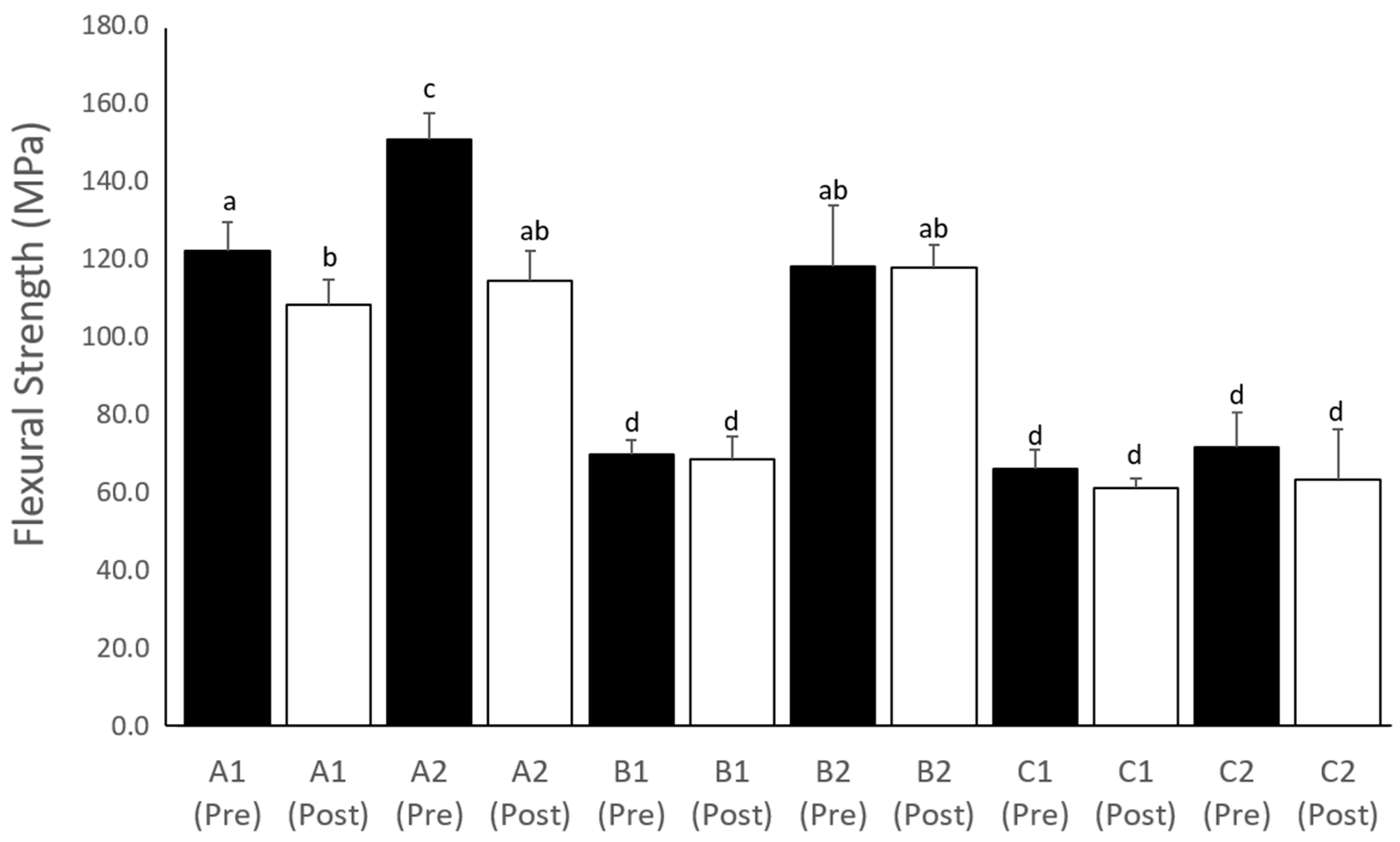
3.2. Mechanical Testing
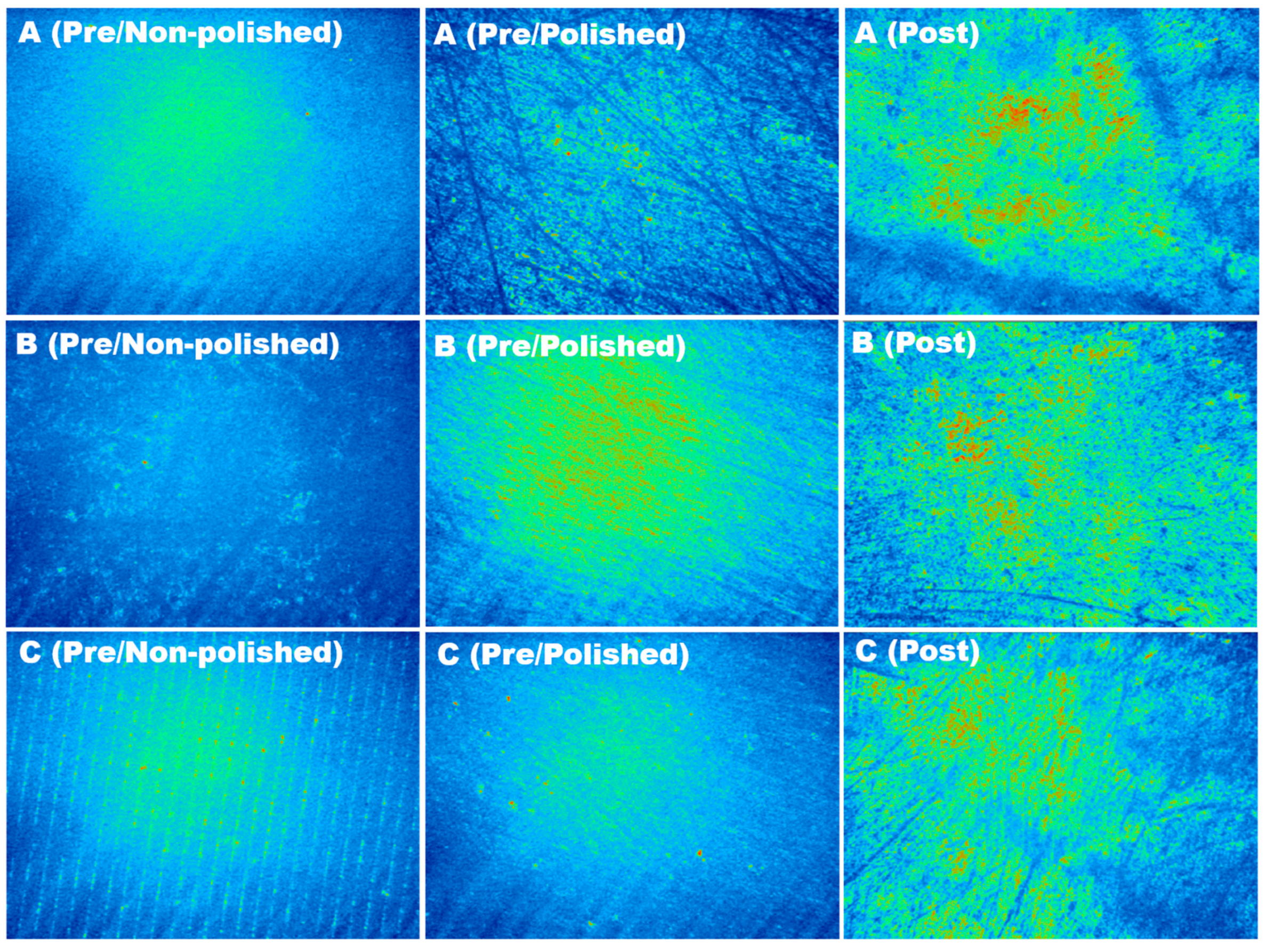
3.3. Surface Roughness
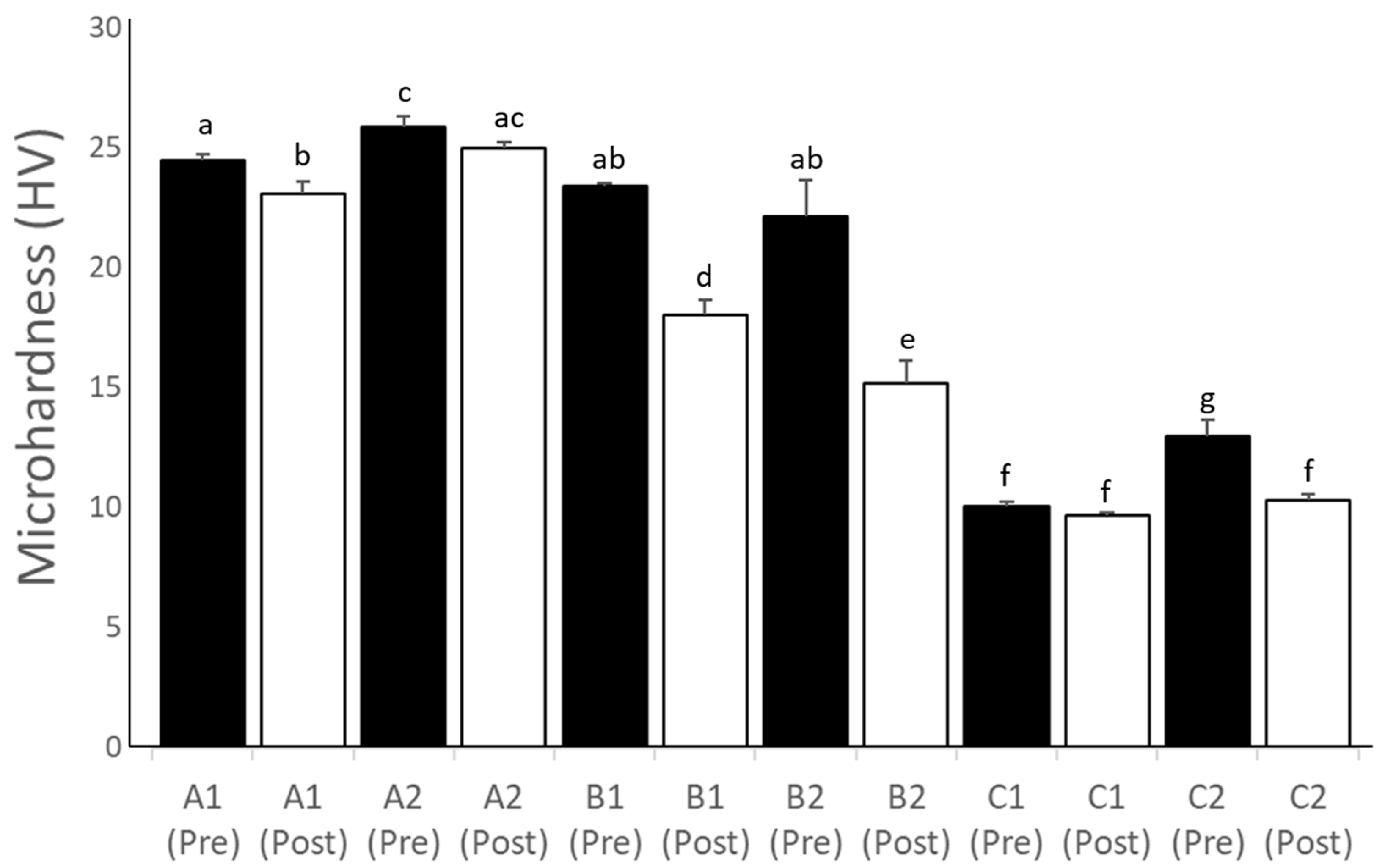
3.4. Microhardness
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Abdullah, A.O.; Pollington, S.; Liu, Y. Comparison between direct chairside and digitally fabricated temporary crowns. Dent. Mater. J. 2018, 37, 957–963. [Google Scholar] [CrossRef] [PubMed]
- Mai, H.-N.; Lee, K.-B.; Lee, D.-H. Fit of interim crowns fabricated using photopolymer-jetting 3D printing. J. Prosthet. Dent. 2017, 118, 208–215. [Google Scholar] [CrossRef] [PubMed]
- Scotti, C.K.; Velo, M.M.D.A.C.; Rizzante, F.A.P.; de Lima Nascimento, T.R.; Mondelli, R.F.L.; Bombonatti, J.F.S. Physical and surface properties of a 3D-printed composite resin for a digital workflow. J. Prosthet. Dent. 2020, 124, 615. [Google Scholar] [CrossRef]
- Regish, K.M.; Sharma, D.; Prithviraj, D.R. Techniques of Fabrication of Provisional Restoration: An Overview. Int. J. Dent. 2011, 2011, 134659. [Google Scholar] [CrossRef]
- Peng, C.C.; Chung, K.H.; Yau, H.T. Assessment of the internal fit and marginal integrity of interim crowns made by different manufacturing methods. J. Prosthet. Dent. 2020, 123, 515–522. [Google Scholar] [CrossRef]
- Alageel, O.; Alsadon, O.; Almansour, H.; Alshehri, A.; Alhabbad, F.; Alsarani, M. Assessment of effect of accelerated aging on interim fixed dental materials using digital technologies. J. Adv. Prosthodont. 2022, 15, 360–368. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.-W.; Ye, S.-Y.; Chien, C.-H.; Chen, C.-J.; Papaspyridakos, P.; Ko, C.-C. Randomized clinical trial of a conventional and a digital workflow for the fabrication of interim crowns: An evaluation of treatment efficiency, fit, and the effect of clinician experience. J. Prosthet. Dent. 2021, 125, 73–81. [Google Scholar] [CrossRef]
- Alageel, O. Three-dimensional printing technologies for dental prosthesis: A review. Rapid Prototyp. J. 2022, 28, 1764–1778. [Google Scholar] [CrossRef]
- Park, S.-M.; Park, J.-M.; Kim, S.-K.; Heo, S.-J.; Koak, J.-Y. Comparison of flexural strength of three-dimensional printed three-unit provisional fixed dental prostheses according to build directions. J. Korean Dent. Sci. 2019, 12, 13–19. [Google Scholar]
- Jain, S.; Sayed, M.E.; Shetty, M.; Alqahtani, S.M.; Al Wadei, M.H.D.; Gupta, S.G.; Othman, A.A.A.; Alshehri, A.H.; Alqarni, H.; Mobarki, A.H.; et al. Physical and Mechanical Properties of 3D-Printed Provisional Crowns and Fixed Dental Prosthesis Resins Compared to CAD/CAM Milled and Conventional Provisional Resins: A Systematic Review and Meta-Analysis. Polymers 2022, 15, 2691. [Google Scholar] [CrossRef]
- Kim, D.; Shim, J.S.; Lee, D.; Shin, S.H.; Nam, N.E.; Park, K.H.; Shim, J.S.; Kim, J.E. Effects of post-curing time on the mechanical and color properties of three-dimensional printed crown and bridge materials. Polymers 2020, 12, 2762. [Google Scholar] [CrossRef]
- Mihaela, P.; Ciocoiu, R.C.; Greabu, M.; Totan, A.R.; Imre, M.; Cristina, A.M.; Sfeatcu, R.; Spînu, T.C.; Ilinca, R.; Petre, A.E. Compressive and flexural strength of 3D-printed and conventional resins designated for interim fixed dental prostheses: An in vitro comparison. Materials 2022, 15, 3075. [Google Scholar]
- Dikova, T.D.; Dzhendov, D.A.; Ivanov, D.; Bliznakova, K. Dimensional accuracy and surface roughness of polymeric dental bridges produced by different 3D printing processes. Arch. Mater. Sci. Eng. 2018, 94, 65–75. [Google Scholar] [CrossRef]
- Derban, P.; Negrea, R.; Rominu, M.; Marsavina, L. Influence of the printing angle and load direction on flexure strength in 3D printed materials for provisional dental restorations. Materials 2021, 15, 3376. [Google Scholar] [CrossRef]
- Moon, W.; Kim, S.; Lim, B.-S.; Park, Y.-S.; Kim, R.J.-Y.; Chung, S.H. Dimensional accuracy evaluation of temporary dental restorations with different 3D printing systems. Materials 2021, 15, 1487. [Google Scholar] [CrossRef]
- Al-Qahtani, A.S.; Tulbah, H.I.; Binhasan, M.; Abbasi, M.S.; Ahmed, N.; Shabib, S.; Farooq, I.; Aldahian, N.; Nisar, S.S.; Tanveer, S.A.; et al. Surface Properties of Polymer Resins Fabricated with Subtractive and Additive Manufacturing Techniques. Polymers 2021, 13, 4077. [Google Scholar] [CrossRef]
- Alharbi, N.; Osman, R.; Wismeijer, D. Effects of build direction on the mechanical properties of 3D-printed complete coverage interim dental restorations. J. Prosthet. Dent. 2016, 115, 760–767. [Google Scholar] [CrossRef] [PubMed]
- Tahayeri, A.; Morgan, M.; Fugolin, A.P.; Bompolaki, D.; Athirasala, A.; Pfeifer, C.S.; Ferracane, J.L.; Bertassoni, L.E. 3D printed versus conventionally cured provisional crown and bridge dental materials. Dent. Mater. J. 2018, 34, 192–200. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Cheng, D.-H.; Huang, S.-C.; Lin, Y.-M. Comparison of flexural properties and cytotoxicity of interim materials printed from mono-LCD and DLP 3D printers. J. Prosthet. Dent. 2020, 126, 703–708. [Google Scholar] [CrossRef]
- Taşın, S.; Ismatullaev, A. Comparative evaluation of the effect of thermocycling on the mechanical properties of conventionally polymerized, CAD-CAM milled, and 3D-printed interim materials. J. Prosthet. Dent. 2022, 127, 173. [Google Scholar] [CrossRef]
- Nam, N.-E.; Shin, S.-H.; Lim, J.-H.; Shim, J.-S.; Kim, J.-E. Effects of artificial tooth brushing and hydrothermal aging on the mechanical properties and color stability of dental 3D printed and CAD/CAM materials. Materials 2021, 15, 6207. [Google Scholar] [CrossRef]
- Yao, Q.; Morton, D.; Eckert, G.J.; Lin, W.-S. The effect of surface treatments on the color stability of CAD-CAM interim fixed dental prostheses. The effect of surface treatments on the color stability of CAD-CAM interim fixed dental prostheses. J. Prosthet. Dent. 2021, 126, 248–253. [Google Scholar] [CrossRef]
- Atalay, S.; Çakmak, G.; Fonseca, M.; Schimmel, M.; Yilmaz, B. Effect of thermocycling on the surface properties of CAD-CAM denture base materials after different surface treatments. J. Mech. Behav. Biomed. Mater. 2021, 121, 104646. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.-S.; Lee, D.-H.; Lee, K.-B. Evaluation of internal fit of interim crown fabricated with CAD/CAM milling and 3D printing system. J. Adv. Prosthodont. 2017, 9, 265–270. [Google Scholar] [CrossRef] [PubMed]
- Bangalore, D.; Alshehri, A.M.; Alsadon, O.; Alaqeel, S.M.; Alageel, O.; Alsarani, M.M.; Almansour, H.; AlShahrani, O. Coffee Staining and Simulated Brushing Induced Color Changes and Surface Roughness of 3D-Printed Orthodontic Retainer Material. Polymers 2023, 15, 2164. [Google Scholar] [CrossRef]
- Rubayo, D.D.; Phasuk, K.; Vickery, J.M.; Morton, D.; Lin, W.-S. Influences of build angle on the accuracy, printing time, and material consumption of additively manufactured surgical templates. J. Prosthet. Dent. 2021, 126, 658–663. [Google Scholar] [CrossRef] [PubMed]
- Alharbi, N.; van de Veen, A.J.; Wismeijer, D.; Osman, R.B. Build angle and its influence on the flexure strength of stereolithography printed hybrid resin material. An in vitro study and a fractographic analysis. Mater. Technol. 2019, 34, 12–17. [Google Scholar] [CrossRef]
- Alshamrani, A.A.; Raju, R.; Ellakwa, A. Effect of printing layer thickness and postprinting conditions on the flexural strength and hardness of a 3D-printed resin. Biomed. Res. Int. 2022, 2022, 8353137. [Google Scholar] [CrossRef]
- Bhambhu, S.; Sahni, S.; Padiyar, N.; Kaurani, P. Comparison of Fracture Resistance of Three-unit Provisional Fixed Dental Prostheses Fabricated Using Conventional and Digital Methods. Int. J. Prosthodont. Restor. Dent. 2023, 12, 59–63. [Google Scholar]
- Revilla-León, M.; Morillo, J.A.; Att, W.; Özcan, M. Chemical composition, Knoop hardness, surface roughness, and adhesion aspects of additively manufactured dental interim materials. J. Prosthet. Dent. 2021, 30, 698–705. [Google Scholar] [CrossRef]
- Zamalloa-Quintana, M.; López-Gurreonero, C.; Santander-Rengifo, F.M.; Ladera-Castañeda, M.; Castro-Pérez Vargas, A.; Cornejo-Pinto, A.; Cervantes-Ganoza, L.; Cayo-Rojas, C. Effect of Additional Dry Heat Curing on Microflexural Strength in Three Types of Resin Composite: An In Vitro Study. Crystals 2022, 12, 1045. [Google Scholar] [CrossRef]

| Group | Resin | Chemical Composition | Printing System |
|---|---|---|---|
| A1 and A2 | Crown & Bridge NextDent ®; Nextdent, Soesterburg, the Netherlands | Methacrylic oligomers, methacrylate monomer, phosphine oxides, pigment | NextDent 5100; Nextdent, Soesterburg, the Netherlands |
| B1 and B2 | DentaTooth; Asiga, Alexandria, NSW, Australia | Trimethyl-4,13-dioxo3,15-dioxa-5,12-diazahexadecane-1,16-diyl bismethacrylate, tetrahydrofurfuryl methacrylate, and diphenyl phosphine oxide | Asiga MAX; Asiga, Alexandria, Australia |
| C1 and C2 | JamgHe temporary resin; JamgHe, Shenzhen, China | NP | Nova 3D Master; Nova3D, Shenzhen, China |
| Pre-Aging (Mean Error in µm ± SD) | Post-Aging (Mean Error in µm ± SD) | |||||
|---|---|---|---|---|---|---|
| Group | Length (L) | Width (W) | Height (H) | Length (L) | Width (W) | Height (H) |
| A1 | 190 (40) A,a | 40 (20) A,b | −10 (10) A,c | 220 (50) A,a | 30 (20) A,b | −10 (2) A,c |
| A2 | 220 (40) A,a | 70 (40) A,b | 50 (10) B,b | 220 (40) A,a | 70 (30) A,b | 50 (10) B,b |
| B1 | 70 (30) B,a | 100 (20) B,b | −70 (20) C,c | 90 (40) B,a | 40 (10) A,d | −50 (20) C,c |
| B2 | −130 (30) C,a | 50 (10) AC,b | 60 (20) B,b | −70 (30) C,d | 40 (10) A,b | 50 (10) B,b |
| C1 | −30 (20) D,a | −70 (40) D,a | −30 (30) AD,a | 10 (30) D,b | −90 (20) B,a | −10 (10) A,a |
| C2 | 30 (20) BE,a | −70 (40) D,b | −60 (40) CE,b | 50 (30) BE,a | −60 (20) C,b | −90 (20) D,b |
| Group | Pre-Aging (Non-Polished) | Pre-Aging (Polished) | Post-Aging (Polished) |
|---|---|---|---|
| A1 | 0.226 (0.002) A,a | 0.224 (0.003) A,a | 0.213 (0.001) A,b |
| A2 | 0.227 (0.002) A,a | 0.213 (0.022) B,b | 0.208 (0.011) A,b |
| B1 | 0.234 (0.012) B,a | 0.219 (0.006) C,b | 0.220 (0.006) B,b |
| B2 | 0.252 (0.048) B,a | 0.217 (0.002) C,b | 0.234 (0.003) C,c |
| C1 | 0.211 (0.003) A,a | 0.225 (0.004) A,b | 0.229 (0.002) D,b |
| C2 | 0.224 (0.003) A,a | 0.190 (0.004) D,b | 0.226 (0.001) D,a |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alageel, O.; Alhijji, S.; Alsadon, O.; Alsarani, M.; Gomawi, A.A.; Alhotan, A. Trueness, Flexural Strength, and Surface Properties of Various Three-Dimensional (3D) Printed Interim Restorative Materials after Accelerated Aging. Polymers 2023, 15, 3040. https://doi.org/10.3390/polym15143040
Alageel O, Alhijji S, Alsadon O, Alsarani M, Gomawi AA, Alhotan A. Trueness, Flexural Strength, and Surface Properties of Various Three-Dimensional (3D) Printed Interim Restorative Materials after Accelerated Aging. Polymers. 2023; 15(14):3040. https://doi.org/10.3390/polym15143040
Chicago/Turabian StyleAlageel, Omar, Saleh Alhijji, Omar Alsadon, Majed Alsarani, Abdurabu Abdullah Gomawi, and Abdulaziz Alhotan. 2023. "Trueness, Flexural Strength, and Surface Properties of Various Three-Dimensional (3D) Printed Interim Restorative Materials after Accelerated Aging" Polymers 15, no. 14: 3040. https://doi.org/10.3390/polym15143040
APA StyleAlageel, O., Alhijji, S., Alsadon, O., Alsarani, M., Gomawi, A. A., & Alhotan, A. (2023). Trueness, Flexural Strength, and Surface Properties of Various Three-Dimensional (3D) Printed Interim Restorative Materials after Accelerated Aging. Polymers, 15(14), 3040. https://doi.org/10.3390/polym15143040







