Influence of Air-Barrier and Curing Light Distance on Conversion and Micro-Hardness of Dental Polymeric Materials
Abstract
1. Introduction
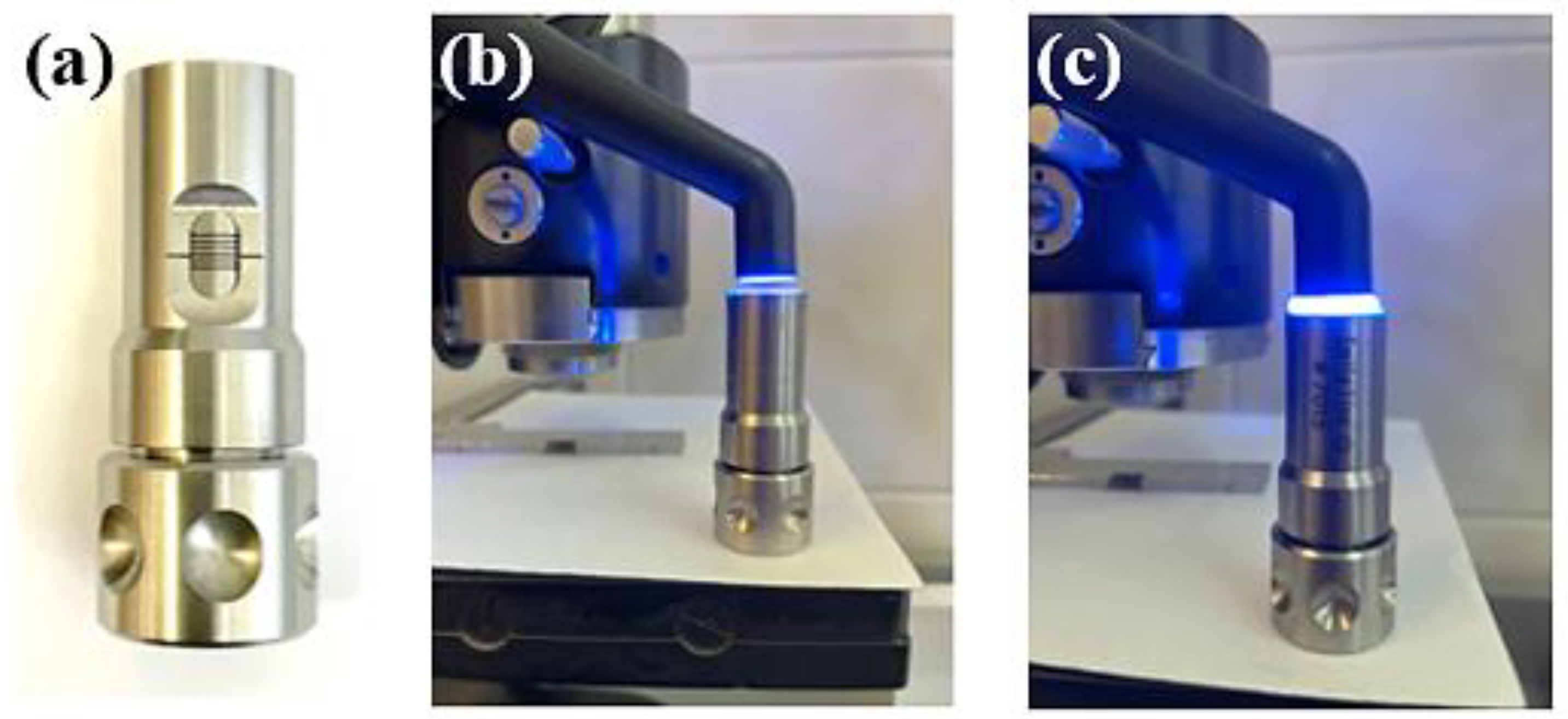
2. Materials and Methods
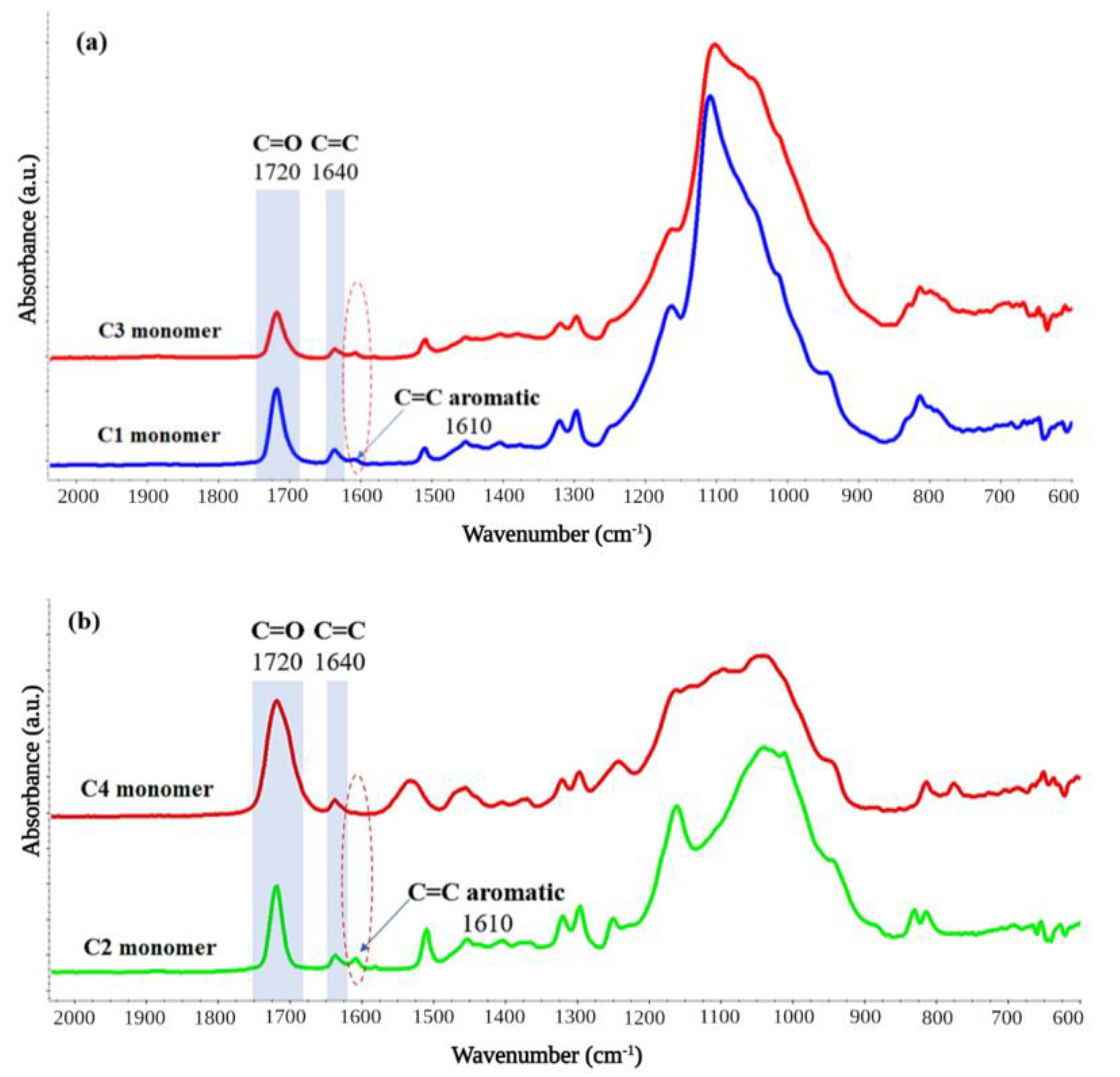
2.1. Fourier Transform Infrared Spectrometry (FT-IR)
2.2. Nano-Indentation Experiments
2.3. Statistical Analysis
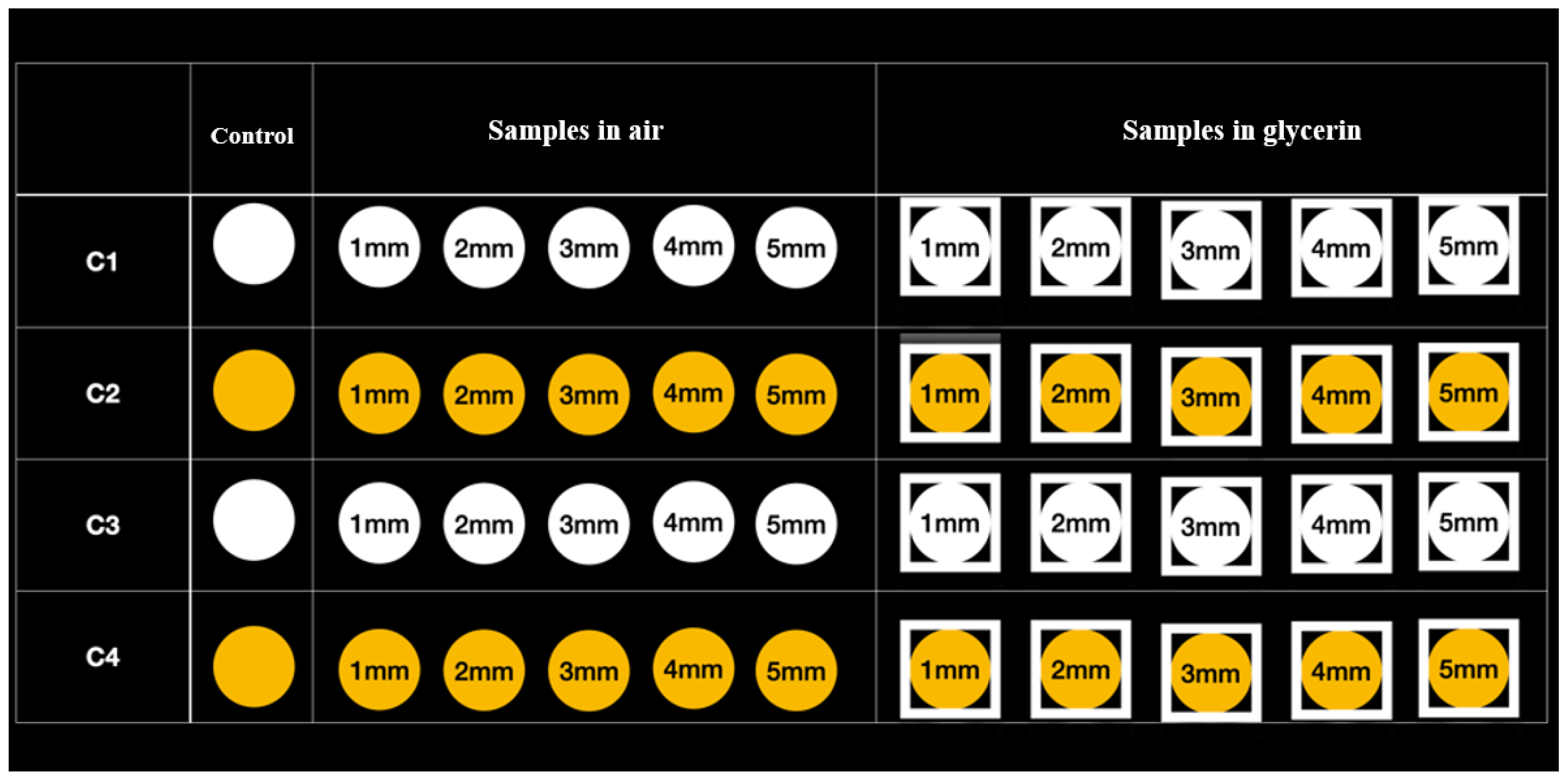
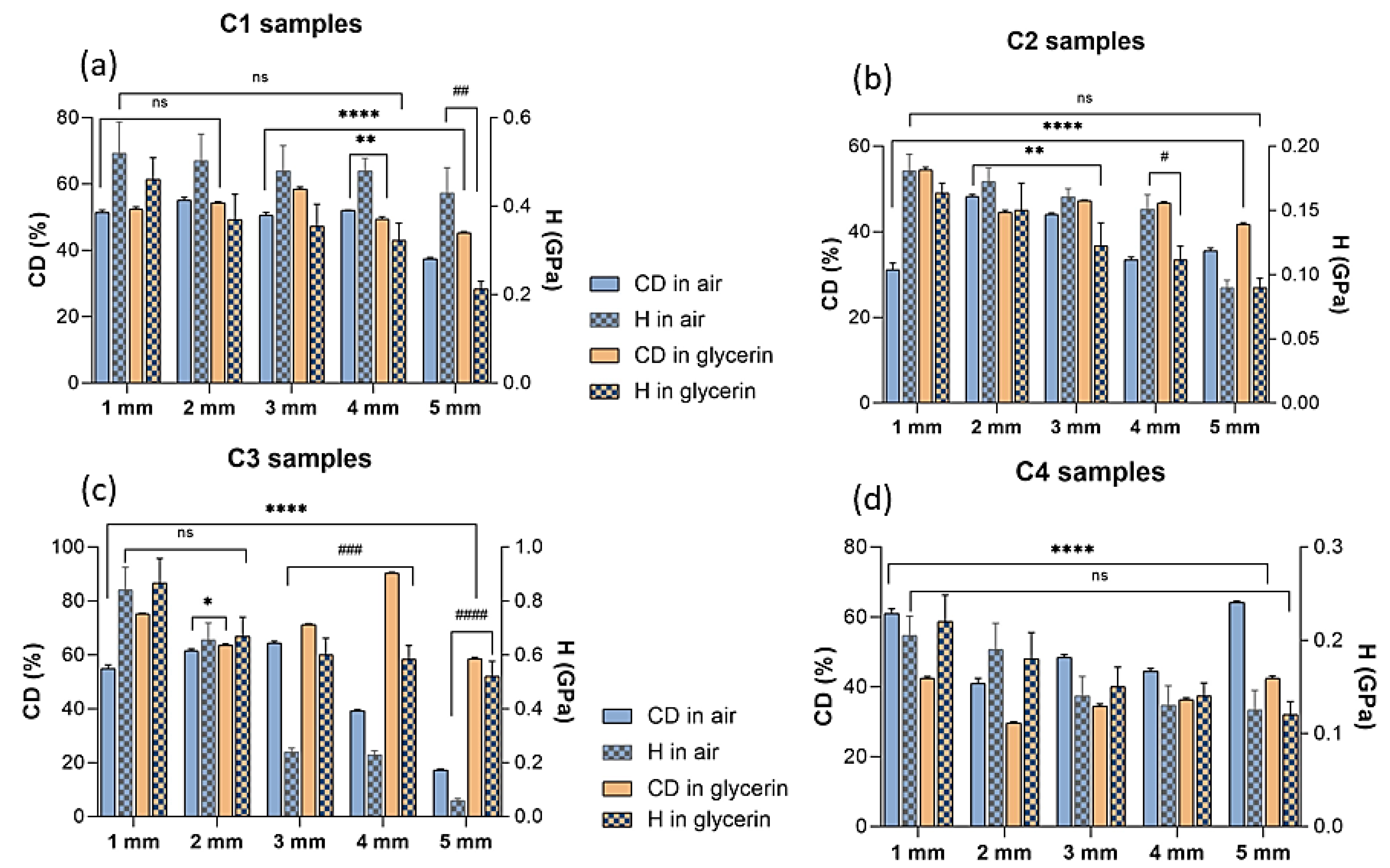
3. Results
3.1. Fourier Transform Infrared Spectrometry (FT-IR)
3.2. Nano-Indentation Experiments
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Khosravani, M.R. Mechanical behavior of restorative dental composites under various loading conditions. J. Mech. Behav. Biomed. Mater. 2019, 93, 151–157. [Google Scholar] [CrossRef] [PubMed]
- Gomes de Carvalho, A.B.; de Andrade, G.S.; Mendes Tribst, J.P.; Grassi, E.D.A.; Ausiello, P.; Saavedra, G.; Bressane, A.; Marques de Melo, R.; Borges, A.L.S. Mechanical Behavior of Different Restorative Materials and Onlay Preparation Designs in Endodontically Treated Molars. Materials 2021, 14, 1923. [Google Scholar] [CrossRef] [PubMed]
- Zabrovsky, A.; Beyth, N.; Pietrokovski, Y.; Ben-Gal, G.; Houri-Haddad, Y. 5—Biocompatibility and functionality of dental restorative materials. In Biocompatibility of Dental Biomaterials; Shelton, R., Ed.; Woodhead Publishing: Cambridge, UK, 2017; pp. 63–75. [Google Scholar]
- Hatton, P.V.; Mulligan, S.; Martin, N. The safety and biocompatibility of direct aesthetic restorative materials. Br. Dent. J. 2022, 232, 611–614. [Google Scholar] [CrossRef]
- Vichi, A.; Margvelashvili, M.; Goracci, C.; Papacchini, F.; Ferrari, M. Bonding and sealing ability of a new self-adhering flowable composite resin in class I restorations. Clin. Oral Investig. 2013, 17, 1497–1506. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, C.; Gavriil, D. Predictable bonding of adhesive indirect restorations: Factors for success. Br. Dent. J. 2021, 231, 287–293. [Google Scholar] [CrossRef] [PubMed]
- Yang, D.-L.; Sun, Q.; Niu, H.; Wang, R.-L.; Wang, D.; Wang, J.-X. The properties of dental resin composites reinforced with silica colloidal nanoparticle clusters: Effects of heat treatment and filler composition. Compos. Part B Eng. 2020, 186, 107791. [Google Scholar] [CrossRef]
- Hata, K.; Ikeda, H.; Nagamatsu, Y.; Masaki, C.; Hosokawa, R.; Shimizu, H. Dental Poly(methyl methacrylate)-Based Resin Containing a Nanoporous Silica Filler. J. Funct. Biomater. 2022, 13, 32. [Google Scholar] [CrossRef]
- Henriks-Eckerman, M.-L.; Suuronen, K.; Jolanki, R.; Alanko, K. Methacrylates in dental restorative materials. Contact Dermatitis 2004, 50, 233–237. [Google Scholar] [CrossRef]
- Rana, M.H.; Shaik, S.; Hameed, M.S.; Al-Saleh, S.; AlHamdan, E.M.; Alshahrani, A.; Alqahtani, A.; Albaqawi, A.H.; Vohra, F.; Abduljabbar, T. Influence of Dental Glass Fibers and Orthopedic Mesh on the Failure Loads of Polymethyl Methacrylate Denture Base Resin. Polymers 2021, 13, 2793. [Google Scholar] [CrossRef]
- Curtis, A.R.; Palin, W.M.; Fleming, G.J.; Shortall, A.C.; Marquis, P.M. The mechanical properties of nanofilled resin-based composites: Characterizing discrete filler particles and agglomerates using a micromanipulation technique. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2009, 25, 180–187. [Google Scholar] [CrossRef]
- Salari, S.; Dadkan, S.; Khakbiz, M.; Atai, M. Effect of nanoparticles on surface characteristics of dental nanocomposite. Med. Devices Sens. 2020, 3, e10081. [Google Scholar] [CrossRef]
- Hegde, M.N.; Hegde, P.; Bhandary, S.; Deepika, K. An evalution of compressive strength of newer nanocomposite: An in vitro study. J. Conserv. Dent. JCD 2011, 14, 36–39. [Google Scholar] [CrossRef] [PubMed]
- Alrobeigy, N. Mechanical properties of contemporary resin composites determined by nanoindentation. Tanta Dent. J. 2017, 14, 129–138. [Google Scholar] [CrossRef]
- Colombo, M.; Poggio, C.; Lasagna, A.; Chiesa, M.; Scribante, A. Vickers Micro-Hardness of New Restorative CAD/CAM Dental Materials: Evaluation and Comparison after Exposure to Acidic Drink. Materials 2019, 12, 1246. [Google Scholar] [CrossRef] [PubMed]
- Pieniak, D.; Walczak, A.; Walczak, M.; Przystupa, K.; Niewczas, A.M. Hardness and Wear Resistance of Dental Biomedical Nanomaterials in a Humid Environment with Non-Stationary Temperatures. Materials 2020, 13, 1255. [Google Scholar] [CrossRef]
- Ciocan, L.T.; Ghitman, J.; Vasilescu, V.G.; Iovu, H. Mechanical Properties of Polymer-Based Blanks for Machined Dental Restorations. Materials 2021, 14, 7293. [Google Scholar] [CrossRef]
- Waqar, Z.; Khan, A.A.; Siddiqui, A.Z.; Noori, S.; Imtiaz, F. Sorption rate evaluation of flowable composite materials by using different photo-activation methods: A spectroscopic analysis. Pak. Oral Dent. J. 2014, 34, 566–570. [Google Scholar]
- Almeida, R.; Manarte-Monteiro, P.; Domingues, J.; Falcão, C.; Herrero-Climent, M.; Ríos-Carrasco, B.; Lemos, B.F. High-Power LED Units Currently Available for Dental Resin-Based Materials—A Review. Polymers 2021, 13, 2165. [Google Scholar] [CrossRef]
- Consani, R.L.X.; de Paula, A.B.; Fugolin, A.P.P.; Pfeifer, C.S. Effect of the combination of a crosslinking agent and a thiourethane additive on the properties of acrylic denture bases processed with microwave energy. J. Mech. Behav. Biomed. Mater. 2019, 98, 90–95. [Google Scholar] [CrossRef]
- da Silva, E.M.; Poskus, L.T.; Guimarães, J.G.; de Araújo Lima Barcellos, A.; Fellows, C.E. Influence of light polymerization modes on degree of conversion and crosslink density of dental composites. J. Mater. Sci. Mater. Med. 2008, 19, 1027–1032. [Google Scholar] [CrossRef]
- Fan, P.L.; Schumacher, R.M.; Azzolin, K.; Geary, R.; Eichmiller, F.C. Curing-light intensity and depth of cure of resin-based composites tested according to international standards. J. Am. Dent. Assoc. 2002, 133, 429–434; quiz 491–423. [Google Scholar] [CrossRef] [PubMed]
- da Silva, E.M.; Poskus, L.T.; Guimarães, J.G. Influence of light-polymerization modes on the degree of conversion and mechanical properties of resin composites: A comparative analysis between a hybrid and a nanofilled composite. Oper. Dent. 2008, 33, 287–293. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.; Kerr, W.J. Light-curing acrylic resin as an orthodontic baseplate material. Quintessence Int. 1998, 29, 508–512. [Google Scholar] [PubMed]
- Rodriguez, A.; Yaman, P.; Dennison, J.; Garcia, D. Effect of Light-Curing Exposure Time, Shade, and Thickness on the Depth of Cure of Bulk Fill Composites. Oper. Dent. 2017, 42, 505–513. [Google Scholar] [CrossRef]
- Alpöz, A.R.; Ertugrul, F.; Cogulu, D.; Ak, A.T.; Tanoglu, M.; Kaya, E. Effects of light curing method and exposure time on mechanical properties of resin based dental materials. Eur. J. Dent. 2008, 2, 37–42. [Google Scholar] [CrossRef]
- Gatin, E.; Iordache, S.-M.; Matei, E.; Luculescu, C.-R.; Iordache, A.-M.; Grigorescu, C.E.A.; Ilici, R.R. Raman Spectroscopy as Spectral Tool for Assessing the Degree of Conversion after Curing of Two Resin-Based Materials Used in Restorative Dentistry. Diagnostics 2022, 12, 1993. [Google Scholar] [CrossRef]
- Domarecka, M.; Szczesio-Wlodarczyk, A.; Krasowski, M.; Fronczek, M.; Gozdek, T.; Sokolowski, J.; Bociong, K. A Comparative Study of the Mechanical Properties of Selected Dental Composites with a Dual-Curing System with Light-Curing Composites. Coatings 2021, 11, 1255. [Google Scholar] [CrossRef]
- Bayrak, G.D.; Yaman-Dosdogru, E.; Selvi-Kuvvetli, S. The Effect of Two Different Light-Curing Units and Curing Times on Bulk-Fill Restorative Materials. Polymers 2022, 14, 1885. [Google Scholar] [CrossRef]
- Thomé, T.; Steagall, W., Jr.; Tachibana, A.; Braga, S.R.; Turbino, M.L. Influence of the distance of the curing light source and composite shade on hardness of two composites. J. Appl. Oral Sci. Rev. FOB 2007, 15, 486–491. [Google Scholar] [CrossRef]
- Borges, M.G.; Silva, G.R.; Neves, F.T.; Soares, C.J.; Faria, E.S.A.L.; Carvalho, R.F.; Menezes, M.S. Oxygen Inhibition of Surface Composites and Its Correlation with Degree of Conversion and Color Stability. Braz. Dent. J. 2021, 32, 91–97. [Google Scholar] [CrossRef]
- Gaviria-Martinez, A.; Castro-Ramirez, L.; Ladera-Castañeda, M.; Cervantes-Ganoza, L.; Cachay-Criado, H.; Alvino-Vales, M.; Garcia-Luna, G.; López-Gurreonero, C.; Cornejo-Pinto, A.; Cayo-Rojas, C.F. Surface roughness and oxygen inhibited layer control in bulk-fill and conventional nanohybrid resin composites with and without polishing: In vitro study. BMC Oral Health 2022, 22, 258. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.smileline.ch/en/products/porcelain-sampler (accessed on 18 August 2022).
- Kwaśny, M.; Polkowski, J.; Bombalska, A. A Study on the Photopolymerization Kinetics of Selected Dental Resins Using Fourier Infrared Spectroscopy (FTIR). Materials 2022, 15, 5850. [Google Scholar] [CrossRef] [PubMed]
- Al-Odayni, A.-B.; Alfotawi, R.; Khan, R.; Sharaf Saeed, W.; Al-Kahtani, A.; Aouak, T.; Alrahlah, A. Synthesis of chemically modified BisGMA analog with low viscosity and potential physical and biological properties for dental resin composite. Dent. Mater. 2019, 35, 1532–1544. [Google Scholar] [CrossRef] [PubMed]
- Frauscher, K.E.; Ilie, N. Degree of conversion of nano-hybrid resin-based composites with novel and conventional matrix formulation. Clin. Oral Investig. 2013, 17, 635–642. [Google Scholar] [CrossRef]
- Prejmerean, C.; Prodan, D.; Vlassa, M.; Streza, M.; Buruiana, T.; Colceriu, L.; Prejmerean, V.; Cuc, S.; Moldovan, M. ATR technique, an appropriate method for determining the degree of conversion in dental giomers. Meas. Sci. Technol. 2016, 27, 124008. [Google Scholar] [CrossRef]
- Amirouche-Korichi, A.; Mouzali, M.; Watts, D.C. Effects of monomer ratios and highly radiopaque fillers on degree of conversion and shrinkage-strain of dental resin composites. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2009, 25, 1411–1418. [Google Scholar] [CrossRef]
- Yoshinaga, K.; Yoshihara, K.; Yoshida, Y. Development of new diacrylate monomers as substitutes for Bis-GMA and UDMA. Dent. Mater. 2021, 37, e391–e398. [Google Scholar] [CrossRef]
- Gonçalves, F.; Kawano, Y.; Pfeifer, C.; Stansbury, J.W.; Braga, R.R. Influence of BisGMA, TEGDMA, and BisEMA contents on viscosity, conversion, and flexural strength of experimental resins and composites. Eur. J. Oral Sci. 2009, 117, 442–446. [Google Scholar] [CrossRef]
- Srivastava, R.; Liu, J.; He, C.; Sun, Y. BisGMA analogues as monomers and diluents for dental restorative composite materials. Mater. Sci. Eng. C 2018, 88, 25–31. [Google Scholar] [CrossRef]
- Cramer, N.B.; Stansbury, J.W.; Bowman, C.N. Recent advances and developments in composite dental restorative materials. J. Dent. Res. 2011, 90, 402–416. [Google Scholar] [CrossRef]
- Pereira-Cenci, T.; Cenci, M.S.; Fedorowicz, Z.; Marchesan, M.A. Antibacterial agents in composite restorations for the prevention of dental caries. Cochrane Database Syst. Rev. 2009, 12, CD007819. [Google Scholar] [CrossRef]
- Lohbauer, U.; Frankenberger, R.; Krämer, N.; Petschelt, A. Strength and fatigue performance versus filler fraction of different types of direct dental restoratives. J. Biomed. Mater. Res. B Appl. Biomater. 2006, 76, 114–120. [Google Scholar] [CrossRef] [PubMed]
- Qian, M.; Zou, B.; Chen, Z.; Huang, W.; Wang, X.; Tang, B.; Liu, Q.; Zhu, Y. The Influence of Filler Size and Crosslinking Degree of Polymers on Mullins Effect in Filled NR/BR Composites. Polymers 2021, 13, 2284. [Google Scholar] [CrossRef] [PubMed]
- Barszczewska-Rybarek, I.M. A Guide through the Dental Dimethacrylate Polymer Network Structural Characterization and Interpretation of Physico-Mechanical Properties. Materials 2019, 12, 4057. [Google Scholar] [CrossRef] [PubMed]
- Leprince, J.G.; Palin, W.M.; Hadis, M.A.; Devaux, J.; Leloup, G. Progress in dimethacrylate-based dental composite technology and curing efficiency. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2013, 29, 139–156. [Google Scholar] [CrossRef]
- Maximov, J.; Dikova, T.; Duncheva, G.; Georgiev, G. Influence of Factors in the Photopolymerization Process on Dental Composites Microhardness. Materials 2022, 15, 6459. [Google Scholar] [CrossRef]
- Lempel, E.; Czibulya, Z.; Kovács, B.; Szalma, J.; Tóth, Á.; Kunsági-Máté, S.; Varga, Z.; Böddi, K. Degree of Conversion and BisGMA, TEGDMA, UDMA Elution from Flowable Bulk Fill Composites. Int. J. Mol. Sci. 2016, 17, 732. [Google Scholar] [CrossRef]
- Ciccone-Nogueira, J.C.; Borsatto, M.C.; de Souza-Zaron, W.C.; Ramos, R.P.; Palma-Dibb, R.G. Microhardness of composite resins at different depths varying the post-irradiation time. J. Appl. Oral Sci. 2007, 15, 305–309. [Google Scholar] [CrossRef]
- Khan, A.A.; Al-Kheraif, A.A.; Al-Shehri, A.M.; Säilynoja, E.; Vallittu, P.K. Polymer matrix of fiber-reinforced composites: Changes in the semi-interpenetrating polymer network during the shelf life. J. Mech. Behav. Biomed. Mater. 2018, 78, 414–419. [Google Scholar] [CrossRef]
- Mousavinasab, S.M.; Meyers, I. Comparison of Depth of Cure, Hardness and Heat Generation of LED and High Intensity QTH Light Sources. Eur. J. Dent. 2011, 5, 299–304. [Google Scholar] [CrossRef]
- Galvão, M.R.; Caldas, S.G.; Bagnato, V.S.; de Souza Rastelli, A.N.; de Andrade, M.F. Evaluation of degree of conversion and hardness of dental composites photo-activated with different light guide tips. Eur. J. Dent. 2013, 7, 86–93. [Google Scholar] [PubMed]
- Asmussen, E. Factors affecting the quantity of remaining double bonds in restorative resin polymers. Eur. J. Oral Sci. 1982, 90, 490–496. [Google Scholar] [CrossRef] [PubMed]
- Knobloch, L.; Kerby, R.E.; Clelland, N.; Lee, J. Hardness and degree of conversion of posterior packable composites. Oper. Dent. 2004, 29, 642–649. [Google Scholar] [PubMed]
- Masouras, K.; Akhtar, R.; Watts, D.C.; Silikas, N. Effect of filler size and shape on local nanoindentation modulus of resin-composites. J. Mater. Sci. Mater. Med. 2008, 19, 3561–3566. [Google Scholar] [CrossRef]
- Shinkai, K.; Taira, Y.; Suzuki, S.; Kawashima, S.; Suzuki, M. Effect of filler size and filler loading on wear of experimental flowable resin composites. J. Appl. Oral Sci. 2018, 26, e20160652. [Google Scholar] [CrossRef]
- Mirică, I.C.; Furtos, G.; Bâldea, B.; Lucaciu, O.; Ilea, A.; Moldovan, M.; Câmpian, R.S. Influence of Filler Loading on the Mechanical Properties of Flowable Resin Composites. Materials 2020, 13, 1477. [Google Scholar] [CrossRef]

| Sample Name | C1 | C2 | C3 | C4 |
|---|---|---|---|---|
| Commercial name/ Country | GrandioSO Heavy Flow (Voco, Cuxhaven, Germany) | GrandioSO Universal nano-hybrid (Voco, Cuxhaven, Germany) | G-aenial Universal Injectable (GC, Tokyo, Japan) | G-aenial restorative composite (GC, Tokyo, Japan) |
| Viscosity Type | Flowable Universal Restorative Composite | Conventional Universal Restorative Composite | Flowable Universal Injectable Composite | Conventional Anterior Composite |
| Curing Type | Light-Curing | Light-Curing | Light-Curing | Light-Curing |
| Resin components | Methacrylate matrix (Bis-GMA, TEGDMA, Bis-EMA) | Methacrylate matri (Bis-GMA, TEGDMA) | Methacrylate matrix (Bis-EMA, UDMA) | UDMA, Dimethacrylate co-monomers |
| Inorganic filler type | Nano-hybrid Functionalized SiO2 nanoparticles Glass ceramics particles | Nano-hybrid Functionalized SiO2 nanoparticles | Ultra-fine 150 nm homogeneously dispersed barium-glass fillers Full-Coverage Silane Coating (FSC) technology | MFR Hybrid composite Fluoro-aluminosilicates Pre-polymerised fillers |
| Filler loading (% by weight) | 83% w/w | 89% w/w | 69% w/w | 84% w/w |
| Filler particle size range (µm) | 20–40 nm | 20–40 nm | 150 nm | 16–850 nm |
| Shade of composites | A2 | A2 | A2 | A2 |
| Sample Name and Analysis Medium | Mean and Standard Deviation of Crosslinking Degree (%) for All the Dental Restorative Composites According to FT-IR Results | |||||||
|---|---|---|---|---|---|---|---|---|
| C1 | C2 | C3 | C4 | C1 | C2 | C3 | C4 | |
| in Air | in Glycerin | |||||||
| 1 mm | 51.5 ± 0.6364 | 31.1 ± 1.5556 | 55 ± 1.3435 | 61.1 ± 1.3435 | 52.5 ± 0.6363 | 54.5 ± 0.6367 | 75.3 ± 0.3536 | 42.4 ± 0.5657 |
| 2 mm | 55.1 ± 0.8485 | 48.3 ± 0.4242 | 61.6 ± 0.6362 | 41 ± 1.4142 | 54.4 ± 0.3536 | 44.6 ± 0.4950 | 63.6 ± 0.5657 | 29.6 ± 0.4243 |
| 3 mm | 50.6 ± 0.8485 | 44.1 ± 0.2828 | 64.5 ± 0.6364 | 48.5 ± 0.7071 | 58.5 ± 0.6367 | 47.2 ± 0.2828 | 71.3 ± 0.4243 | 34.5 ± 0.6361 |
| 4 mm | 52.1 ± 0.0707 | 33.5 ± 0.6363 | 39.3 ± 0.3536 | 44.5 ± 0.7069 | 49.5 ± 0.6359 | 46.7 ± 0.2836 | 90.3 ± 0.3536 | 36.4 ± 0.4950 |
| 5 mm | 37.35 ± 0.4950 | 35.6 ± 0.6363 | 17.3 ± 0.4243 | 64.3 ± 0.3536 | 45.2 ± 0.4243 | 41.8 ± 0.3536 | 58.6 ± 0.5657 | 42.5 ± 0.6365 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ciocan, L.T.; Biru, E.I.; Vasilescu, V.G.; Ghitman, J.; Stefan, A.-R.; Iovu, H.; Ilici, R. Influence of Air-Barrier and Curing Light Distance on Conversion and Micro-Hardness of Dental Polymeric Materials. Polymers 2022, 14, 5346. https://doi.org/10.3390/polym14245346
Ciocan LT, Biru EI, Vasilescu VG, Ghitman J, Stefan A-R, Iovu H, Ilici R. Influence of Air-Barrier and Curing Light Distance on Conversion and Micro-Hardness of Dental Polymeric Materials. Polymers. 2022; 14(24):5346. https://doi.org/10.3390/polym14245346
Chicago/Turabian StyleCiocan, Lucian Toma, Elena Iuliana Biru, Vlad Gabriel Vasilescu, Jana Ghitman, Ana-Roxana Stefan, Horia Iovu, and Roxana Ilici. 2022. "Influence of Air-Barrier and Curing Light Distance on Conversion and Micro-Hardness of Dental Polymeric Materials" Polymers 14, no. 24: 5346. https://doi.org/10.3390/polym14245346
APA StyleCiocan, L. T., Biru, E. I., Vasilescu, V. G., Ghitman, J., Stefan, A.-R., Iovu, H., & Ilici, R. (2022). Influence of Air-Barrier and Curing Light Distance on Conversion and Micro-Hardness of Dental Polymeric Materials. Polymers, 14(24), 5346. https://doi.org/10.3390/polym14245346









