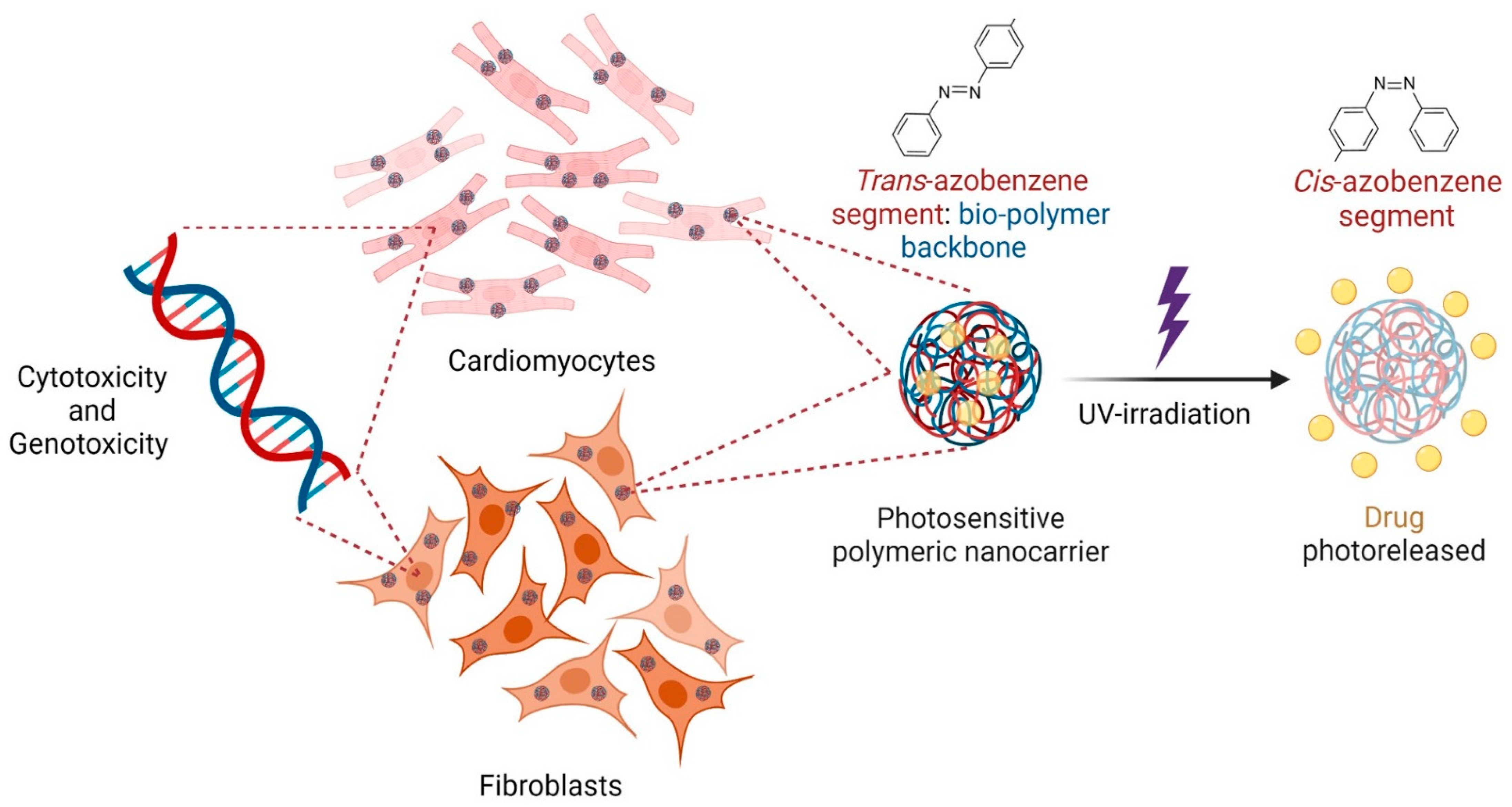
Cytotoxicity and Genotoxicity of Azobenzene-Based Polymeric Nanocarriers for Phototriggered Drug Release and Biomedical Applications
Abstract
:1. Introduction
2. Materials and Methods
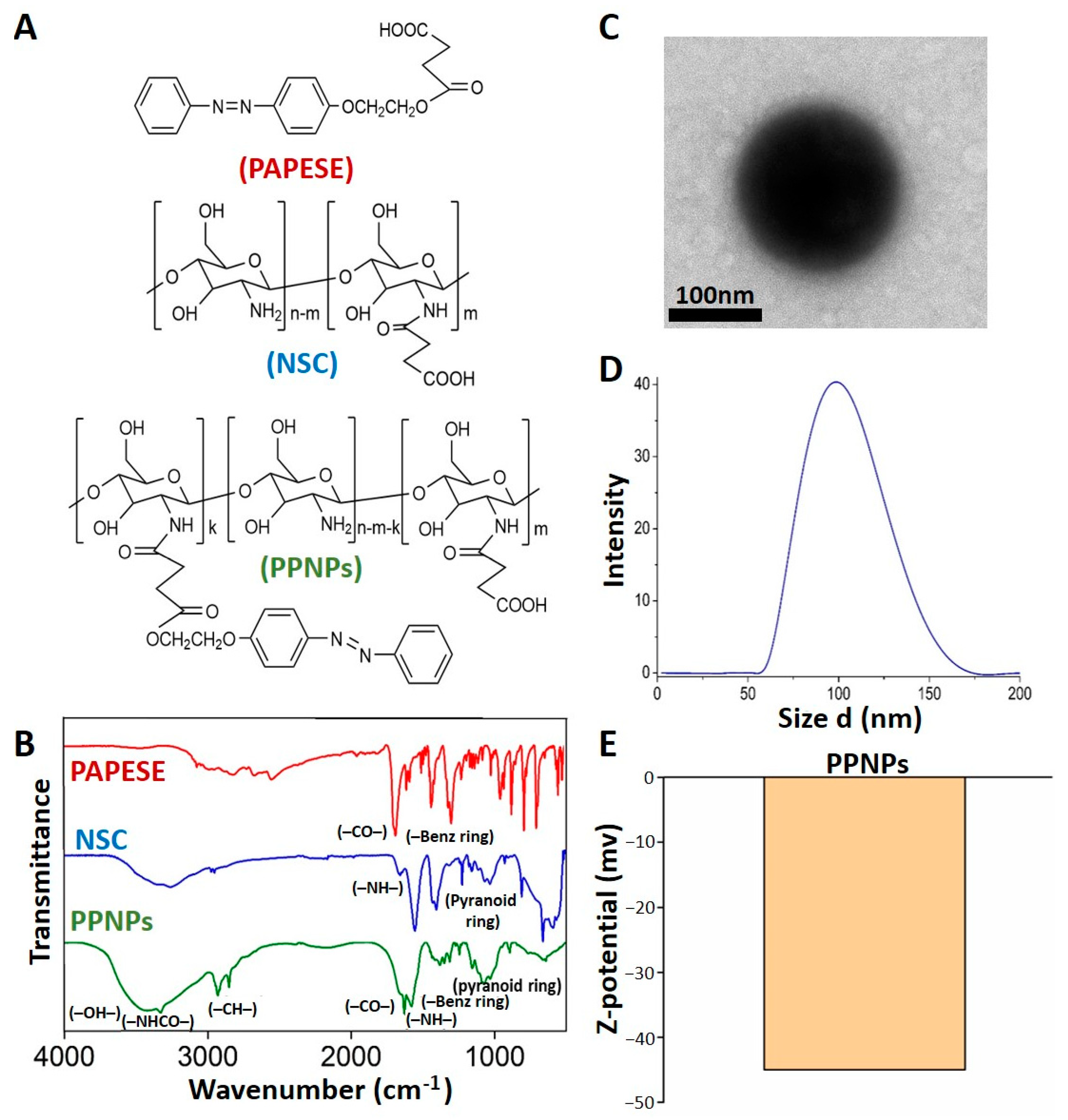
2.1. Synthesis, Self-Assembly, and Characterization of PPNPs
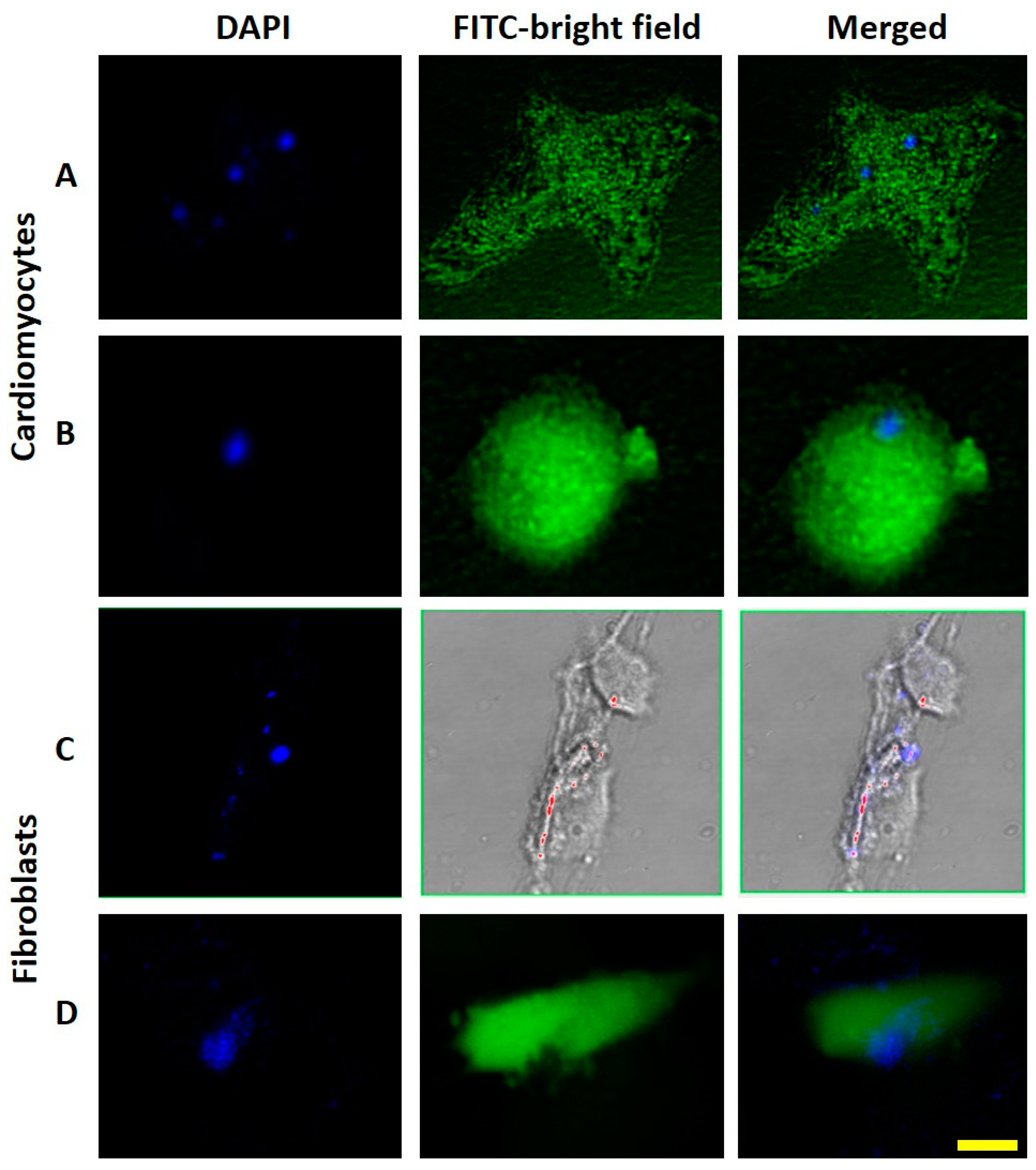
2.2. PPNPs Capture by Cells and Characterization
2.3. Cell Culture
2.4. MTT Assay
2.5. Trypan Blue Exclusion Assay
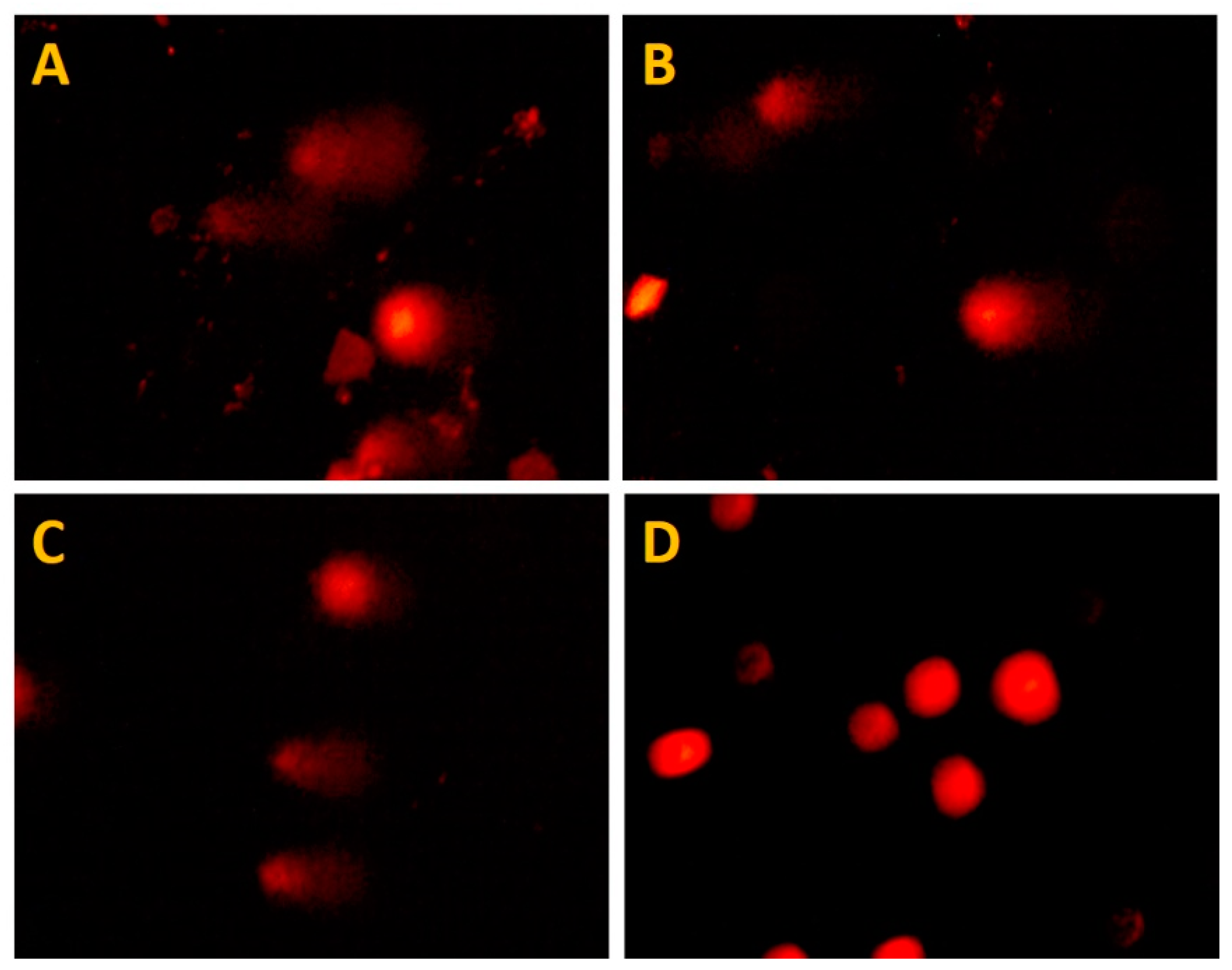
2.6. Comet Assay
2.7. PPNP Photoisomerization, Drug Nanoencapasulation, and Photorelease
3. Results
3.1. Photosensitive Nanoparticle Characterization
3.1.1. FT-IR Detailed Spectral Data of the PPNP Synthesis
3.1.2. Morphologies, Sizes, and Surface Charges of the PPNPs
3.2. Nanoparticle Catchment by Cells
3.3. Evaluation of Mitochondrial Metabolism
3.4. Evaluation of Membrane Stability
3.5. Genotoxicity Test
3.6. PPNP Photoisomerization and Drug Photorealase
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Devarajan, P.V.; Jain, S. Targeted Drug Delivery: Concepts and Design; Springer: Berlin/Heidelberg, Germany, 2015; ISBN 3319113550. [Google Scholar]
- Lewinski, N.; Colvin, V.; Drezek, R. Cytotoxicity of Nanoparticles. Small 2008, 4, 26–49. [Google Scholar] [CrossRef] [PubMed]
- Arora, S.; Rajwade, J.M.; Paknikar, K.M. Nanotoxicology and in Vitro Studies: The Need of the Hour. Toxicol. Appl. Pharmacol. 2012, 258, 151–165. [Google Scholar] [CrossRef] [PubMed]
- Elieh-Ali-Komi, D.; Hamblin, M.R. Chitin and Chitosan: Production and Application of Versatile Biomedical Nanomaterials. Int. J. Adv. Res. 2016, 4, 411–427. [Google Scholar]
- Abbas, A. Chitosan for Biomedical Applications; University of Iowa: Iowa City, IA, USA, 2010. [Google Scholar]
- Aiping, Z.; Tian, C.; Lanhua, Y.; Hao, W.; Ping, L. Synthesis and Characterization of N-Succinyl-Chitosan and Its Self-Assembly of Nanospheres. Carbohydr. Polym. 2006, 66, 274–279. [Google Scholar] [CrossRef]
- Giraldo, P.M.; Buitrago, S.P.; Pinal, R.; Palacio, L.H. Síntesis de N-Succinil-Quitosano y Formación de Nanomicelas Para Transporte de Fármacos Hidrófobos. Investig. Appl. 2015, 9, 125–131. [Google Scholar]
- Yang, S.; Zhu, W.; Zhu, Q.; Chen, W.; Ren, Z.; Li, F.; Yuan, Z.; Li, J.; Liu, Y.; Zhou, X. Binary-copolymer System Base on Low-density Lipoprotein-coupled N-succinyl Chitosan Lipoic Acid Micelles for Co-delivery MDR1 SiRNA and Paclitaxel, Enhances Antitumor Effects via Reducing Drug. J. Biomed. Mater. Res. Part B Appl. Biomater. 2017, 105, 1114–1125. [Google Scholar] [CrossRef]
- Duan, H.; Lü, S.; Qin, H.; Gao, C.; Bai, X.; Wei, Y.; Wu, X.; Liu, M.; Zhang, X.; Liu, Z. Co-Delivery of Zinc and 5-Aminosalicylic Acid from Alginate/N-Succinyl-Chitosan Blend Microspheres for Synergistic Therapy of Colitis. Int. J. Pharm. 2017, 516, 214–224. [Google Scholar] [CrossRef]
- Arjmand, F.; Salami-Kalajahi, M.; Roghani-Mamaqani, H. Preparation of Photolabile Nanoparticles by Coumarin-Based Crosslinker for Drug Delivery under Light Irradiation. J. Phys. Chem. Solids 2021, 154, 110102. [Google Scholar] [CrossRef]
- Park, S.M.; Kim, M.S.; Park, S.-J.; Park, E.S.; Choi, K.-S.; Kim, Y.-S.; Kim, H.R. Novel Temperature-Triggered Liposome with High Stability: Formulation, in Vitro Evaluation, and in Vivo Study Combined with High-Intensity Focused Ultrasound (HIFU). J. Control. Release 2013, 170, 373–379. [Google Scholar] [CrossRef]
- Yang, Y.; Xie, X.; Yang, Y.; Li, Z.; Yu, F.; Gong, W.; Li, Y.; Zhang, H.; Wang, Z.; Mei, X. Polymer Nanoparticles Modified with Photo-and PH-Dual-Responsive Polypeptides for Enhanced and Targeted Cancer Therapy. Mol. Pharm. 2016, 13, 1508–1519. [Google Scholar] [CrossRef]
- Cao, J.; Huang, S.; Chen, Y.; Li, S.; Li, X.; Deng, D.; Qian, Z.; Tang, L.; Gu, Y. Near-Infrared Light-Triggered Micelles for Fast Controlled Drug Release in Deep Tissue. Biomaterials 2013, 34, 6272–6283. [Google Scholar] [CrossRef] [PubMed]
- Razavi, B.; Abdollahi, A.; Roghani-Mamaqani, H.; Salami-Kalajahi, M. Light-and Temperature-Responsive Micellar Carriers Prepared by Spiropyran-Initiated Atom Transfer Polymerization: Investigation of Photochromism Kinetics, Responsivities, and Controlled Release of Doxorubicin. Polymer 2020, 187, 122046. [Google Scholar] [CrossRef]
- Pérez-Buitrago, S.; Mena-Giraldo, P.; Pinal, R.; Hoyos-Palacio, L. Azopolymer Based Nanoparticles for Phototriggered Drug Delivery. In Proceedings of the 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Berlin, Germany, 23–27 July 2019; pp. 1089–1092. [Google Scholar]
- Jhaveri, A.; Deshpande, P.; Torchilin, V. Stimuli-Sensitive Nanopreparations for Combination Cancer Therapy. J. Control. Release 2014, 190, 352–370. [Google Scholar] [CrossRef] [PubMed]
- Motornov, M.; Roiter, Y.; Tokarev, I.; Minko, S. Stimuli-Responsive Nanoparticles, Nanogels and Capsules for Integrated Multifunctional Intelligent Systems. Prog. Polym. Sci. 2010, 35, 174–211. [Google Scholar] [CrossRef]
- Mena-Giraldo, P.; Orozco, J. Polymeric Micro/Nanocarriers and Motors for Cargo Transport and Phototriggered Delivery. Polymers 2021, 13, 3920. [Google Scholar] [CrossRef]
- Díaz-Moscoso, A.; Arroyave, F.A.; Ballester, P. Moving Systems of Polar Dimeric Capsules out of Thermal Equilibrium by Light Irradiation. Chem. Commun. 2016, 52, 3046–3049. [Google Scholar] [CrossRef]
- Moleavin, I.; Ibanescu, C.; Hodorog-Rusu, A.; Peptu, E.; Doroftei, F.; Hurduc, N. Amphiphilic Azopolymers Capable to Generate Photo-Sensitive Micelles. Cent. Eur. J. Chem. 2011, 9, 1117–1125. [Google Scholar] [CrossRef]
- Molla, M.R.; Rangadurai, P.; Antony, L.; Swaminathan, S.; de Pablo, J.J.; Thayumanavan, S. Dynamic Actuation of Glassy Polymersomes through Isomerization of a Single Azobenzene Unit at the Block Copolymer Interface. Nat. Chem. 2018, 10, 659–666. [Google Scholar] [CrossRef]
- Abid, J.-P.; Frigoli, M.; Pansu, R.; Szeftel, J.; Zyss, J.; Larpent, C.; Brasselet, S. Light-Driven Directed Motion of Azobenzene-Coated Polymer Nanoparticles in an Aqueous Medium. Langmuir 2011, 27, 7967–7971. [Google Scholar] [CrossRef]
- Zhao, T.; Wang, P.; Li, Q.; Al-Khalaf, A.A.; Hozzein, W.N.; Zhang, F.; Li, X.; Zhao, D. Near-Infrared Triggered Decomposition of Nanocapsules with High Tumor Accumulation and Stimuli Responsive Fast Elimination. Angew. Chem. 2018, 130, 2641–2645. [Google Scholar] [CrossRef]
- Mena-Giraldo, P.; Orozco, J. Photosensitive Polymeric Janus Micromotor for Enzymatic Activity Protection and Enhanced Substrate Degradation. ACS Appl. Mater. Interfaces 2022, 14, 4. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Deng, Y.; He, Y.; Tong, X.; Wang, X. Amphiphilic Azo Polymer Spheres, Colloidal Monolayers, and Photoinduced Chromophore Orientation. Langmuir 2005, 21, 6567–6571. [Google Scholar] [CrossRef] [PubMed]
- Mena-Giraldo, P.; Pérez-Buitrago, S.; Londoño-Berrío, M.; Ortiz-Trujillo, I.C.; Hoyos-Palacio, L.M.; Orozco, J. Photosensitive Nanocarriers for Specific Delivery of Cargo into Cells. Sci. Rep. 2020, 10, 2110. [Google Scholar] [CrossRef] [Green Version]
- Kobashigawa, L.C.; Xu, Y.C.; Padbury, J.F.; Tseng, Y.T.; Yano, N. Metformin Protects Cardiomyocyte from Doxorubicin Induced Cytotoxicity through an AMP-Activated Protein Kinase Dependent Signaling Pathway: An in Vitro Study. PLoS ONE 2014, 9, e104888. [Google Scholar] [CrossRef] [Green Version]
- Maayah, Z.H.; Abdelhamid, G.; El-Kadi, A.O.S. Development of Cellular Hypertrophy by 8-Hydroxyeicosatetraenoic Acid in the Human Ventricular Cardiomyocyte, RL-14 Cell Line, Is Implicated by MAPK and NF-ΚB. Cell Biol. Toxicol. 2015, 31, 241–259. [Google Scholar] [CrossRef] [PubMed]
- Sahu, S.C.; Casciano, D.A. Nanotoxicity: From In Vivo and In Vitro Models to Health Risks; John Wiley & Sons: Hoboken, NJ, USA, 2009; ISBN 047074779X. [Google Scholar]
- Mosmann, T. Rapid Colorimetric Assay for Cellular Growth and Survival: Application to Proliferation and Cytotoxicity Assays. J. Immunol. Methods 1983, 65, 55–63. [Google Scholar] [CrossRef]
- Fotakis, G.; Timbrell, J.A. In Vitro Cytotoxicity Assays: Comparison of LDH, Neutral Red, MTT and Protein Assay in Hepatoma Cell Lines Following Exposure to Cadmium Chloride. Toxicol. Lett. 2006, 160, 171–177. [Google Scholar] [CrossRef]
- Bilmin, K.; Kopczynska, B.; Grieb, P. Influence of Serum and Albumin on the in Vitro Anandamide Cytotoxicity toward C6 Glioma Cells Assessed by the MTT Cell Viability Assay: Implications for the Methodology of the MTT Tests. Folia Neuropathol. 2013, 51, 44–50. [Google Scholar] [CrossRef]
- Strober, W. Trypan Blue Exclusion Test of Cell Viability. Curr. Protoc. Immunol. 2015, 111, A3-B. [Google Scholar] [CrossRef]
- Ferreiro, G.R.; Badıas, L.C.; Lopez-Nigro, M.; Palermo, A.; Mudry, M.; Elio, P.G.; Carballo, M.A. DNA Single Strand Breaks in Peripheral Blood Lymphocytes Induced by Three Nitroimidazole Derivatives. Toxicol. Lett. 2002, 132, 109–115. [Google Scholar] [CrossRef]
- Rodrigues, S.; Dionísio, M.; López, C.R.; Grenha, A. Biocompatibility of Chitosan Carriers with Application in Drug Delivery. J. Funct. Biomater. 2012, 3, 615–641. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Malatesta, M.; Galimberti, V.; Cisterna, B.; Costanzo, M.; Biggiogera, M.; Zancanaro, C. Chitosan Nanoparticles Are Efficient Carriers for Delivering Biodegradable Drugs to Neuronal Cells. Histochem. Cell Biol. 2014, 141, 551–558. [Google Scholar] [CrossRef] [PubMed]
- Malatesta, M.; Grecchi, S.; Chiesa, E.; Cisterna, B.; Costanzo, M.; Zancanaro, C. Internalized Chitosan Nanoparticles Persist for Long Time in Cultured Cells. Eur. J. Histochem. 2015, 59, 2492. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jena, P.; Mohanty, S.; Mallick, R.; Jacob, B.; Sonawane, A. Toxicity and Antibacterial Assessment of Chitosancoated Silver Nanoparticles on Human Pathogens and Macrophage Cells. Int. J. Nanomed. 2012, 7, 1805. [Google Scholar]
- Mori, H.; Mori, Y.; Sugie, S.; Yoshimi, N.; Takahashi, M.; Ni-i, H.; Yamazaki, H.; Toyoshi, K.; Williams, G.M. Genotoxicity of a Variety of Azobenzene and Aminoazobenzene Compounds in the Hepatocyte/DNA Repair Test and the Salmonella/Mutagenicity Test. Cancer Res. 1986, 46, 1654–1658. [Google Scholar]
- Shang, L.; Nienhaus, K.; Nienhaus, G.U. Engineered Nanoparticles Interacting with Cells: Size Matters. J. Nanobiotechnol. 2014, 12, 5. [Google Scholar] [CrossRef] [Green Version]
- Pérez-Buitrago, S.; Ugarte, J.P.; Tobón, C. Atrial Rotor Modulation by Localized Dofetilide Application: An in silico Study. In Proceedings of the 2018 Computing in Cardiology Conference (CinC), Maastricht, The Netherlands, 23–26 September 2018; Volume 45, pp. 1–4. [Google Scholar]



| Damage Level | Damage Category | Tail Length (µm) |
|---|---|---|
| 0 | No damage | 0–11.34 |
| 1 | Low damage | 11.34–17.34 |
| 2 | Medium damage | 17.34–23.34 |
| 3 | Total damage | 23.34–34.68 |
| Assay | NSC (mg/mL) | PAPESE (mg/mL) | PPNPs (mg/mL) |
|---|---|---|---|
| PPNPs synthesis | 1.00 | 0.30 | |
| LC50 of RL14 Cardiomyocytes | 2.09 | 1.28 | 3.80 |
| LC50 of NiH3T3 Fibroblasts | 1.28 | 1.72 | 3.41 |
| Treatment | Concentration (mg/mL) | Comet Tail Length (µm) | ||
|---|---|---|---|---|
| Median | 25th Percentile | 95th Percentile | ||
| DMEM | 0 | 9 | 8.0 | 13 |
| NSC | 0.5 | 10 | 8.0 | 13 |
| 1.0 | 10 | 8.0 | 13 | |
| 2.0 | 10 | 8.0 | 13 | |
| PAPESE | 0.5 | 11 | 9.0 | 17 |
| 1.0 | 11 | 9.0 | 16 | |
| 2.0 | 11 | 8.0 | 16 | |
| PPNPs | 0.0 | 11 | 10.0 | 20 |
| 1.0 | 11 | 9.5 | 19 | |
| 2.0 | 11 | 10.0 | 20 | |
| Treatment | Concentration (mg/mL) | Damage Level (% of Cells) | WDI | |||
|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | |||
| DMEM | 0 | 99.1 | 0.89 | 0 | 0 | 9 |
| NSC | 2.0 | 100.0 | 0 | 0 | 0 | 0 |
| 1.0 | 100.0 | 0 | 0 | 0 | 0 | |
| 0.5 | 100.0 | 0 | 0 | 0 | 0 | |
| PAPESE | 2.0 | 89.3 | 10.6 | 0 | 0 | 32 |
| 1.0 | 92.3 | 7.6 | 0 | 0 | 23 | |
| 0.5 | 89.3 | 10.6 | 0 | 0 | 32 | |
| PPNPs | 2.0 | 74.6 | 25.3 | 0 | 0 | 76 |
| 1.0 | 69.0 | 31.0 | 0 | 0 | 93 | |
| 0.5 | 65.6 | 34.3 | 0 | 0 | 103 | |
| Drug | PPNPs (mg/mL) | Drug Encapsulated (μM) | Drug Photoreleased (%) |
|---|---|---|---|
| Nile red | 0.1623 ± 0.0003 | 19.38 + 0.07 | 98.71 |
| Dofetilide | 0.1614 ± 0.0002 | 57.52 ± 0.09 | 97.12 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Londoño-Berrío, M.; Pérez-Buitrago, S.; Ortiz-Trujillo, I.C.; Hoyos-Palacio, L.M.; Orozco, L.Y.; López, L.; Zárate-Triviño, D.G.; Capobianco, J.A.; Mena-Giraldo, P. Cytotoxicity and Genotoxicity of Azobenzene-Based Polymeric Nanocarriers for Phototriggered Drug Release and Biomedical Applications. Polymers 2022, 14, 3119. https://doi.org/10.3390/polym14153119
Londoño-Berrío M, Pérez-Buitrago S, Ortiz-Trujillo IC, Hoyos-Palacio LM, Orozco LY, López L, Zárate-Triviño DG, Capobianco JA, Mena-Giraldo P. Cytotoxicity and Genotoxicity of Azobenzene-Based Polymeric Nanocarriers for Phototriggered Drug Release and Biomedical Applications. Polymers. 2022; 14(15):3119. https://doi.org/10.3390/polym14153119
Chicago/Turabian StyleLondoño-Berrío, Maritza, Sandra Pérez-Buitrago, Isabel Cristina Ortiz-Trujillo, Lina M. Hoyos-Palacio, Luz Yaneth Orozco, Lucelly López, Diana G. Zárate-Triviño, John A. Capobianco, and Pedro Mena-Giraldo. 2022. "Cytotoxicity and Genotoxicity of Azobenzene-Based Polymeric Nanocarriers for Phototriggered Drug Release and Biomedical Applications" Polymers 14, no. 15: 3119. https://doi.org/10.3390/polym14153119
APA StyleLondoño-Berrío, M., Pérez-Buitrago, S., Ortiz-Trujillo, I. C., Hoyos-Palacio, L. M., Orozco, L. Y., López, L., Zárate-Triviño, D. G., Capobianco, J. A., & Mena-Giraldo, P. (2022). Cytotoxicity and Genotoxicity of Azobenzene-Based Polymeric Nanocarriers for Phototriggered Drug Release and Biomedical Applications. Polymers, 14(15), 3119. https://doi.org/10.3390/polym14153119







