3D Printable Electrically Conductive Hydrogel Scaffolds for Biomedical Applications: A Review
Abstract
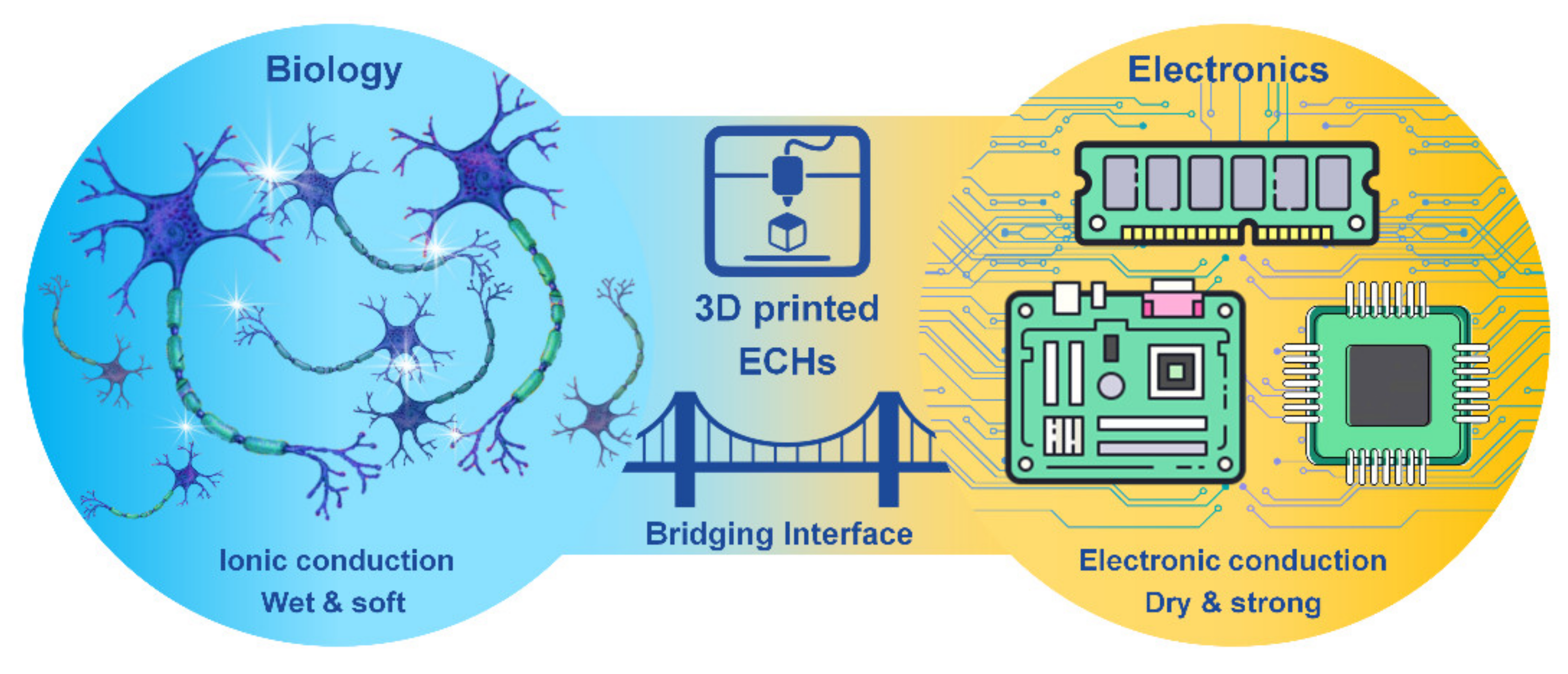
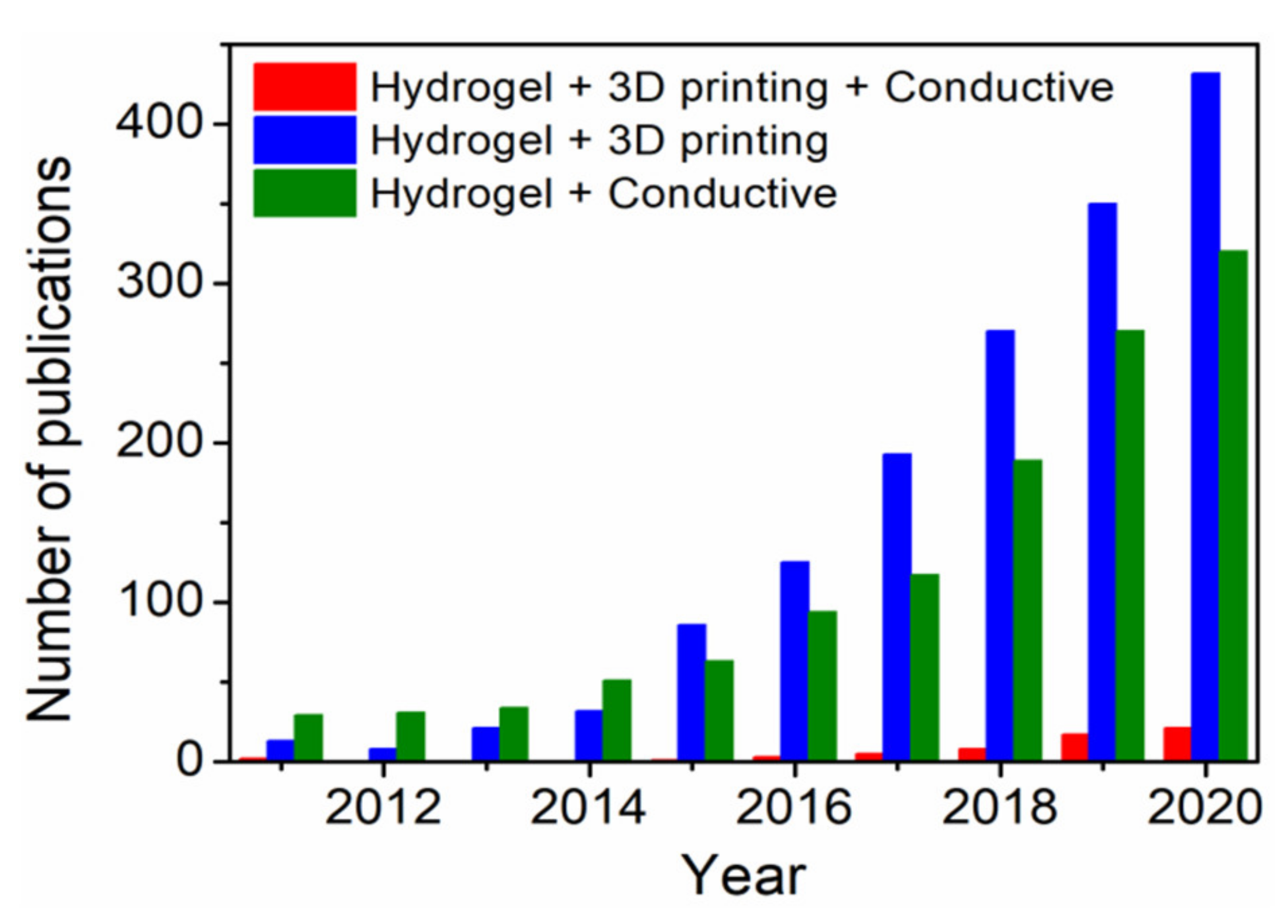
1. Introduction
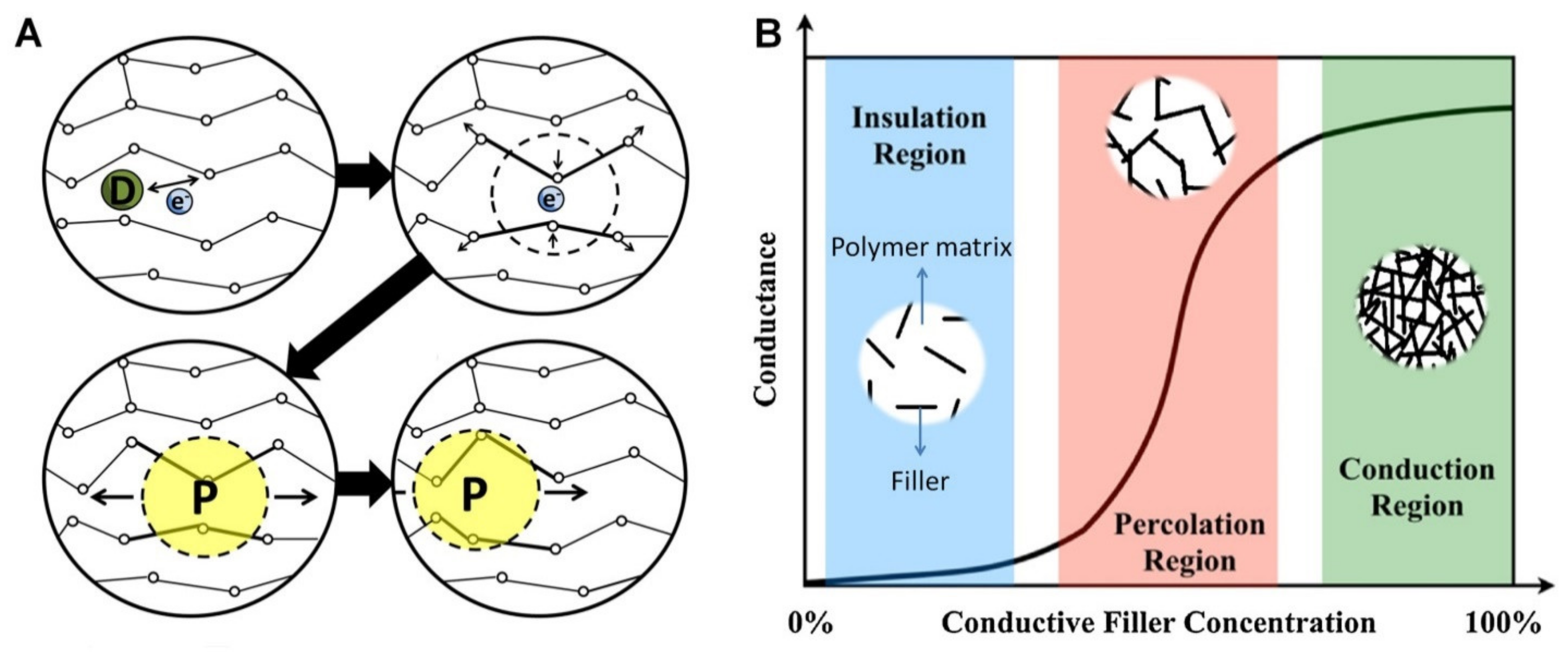
2. Mechanism of Electrical Conductivity in ECHs
3. 3D Printing of ECHs
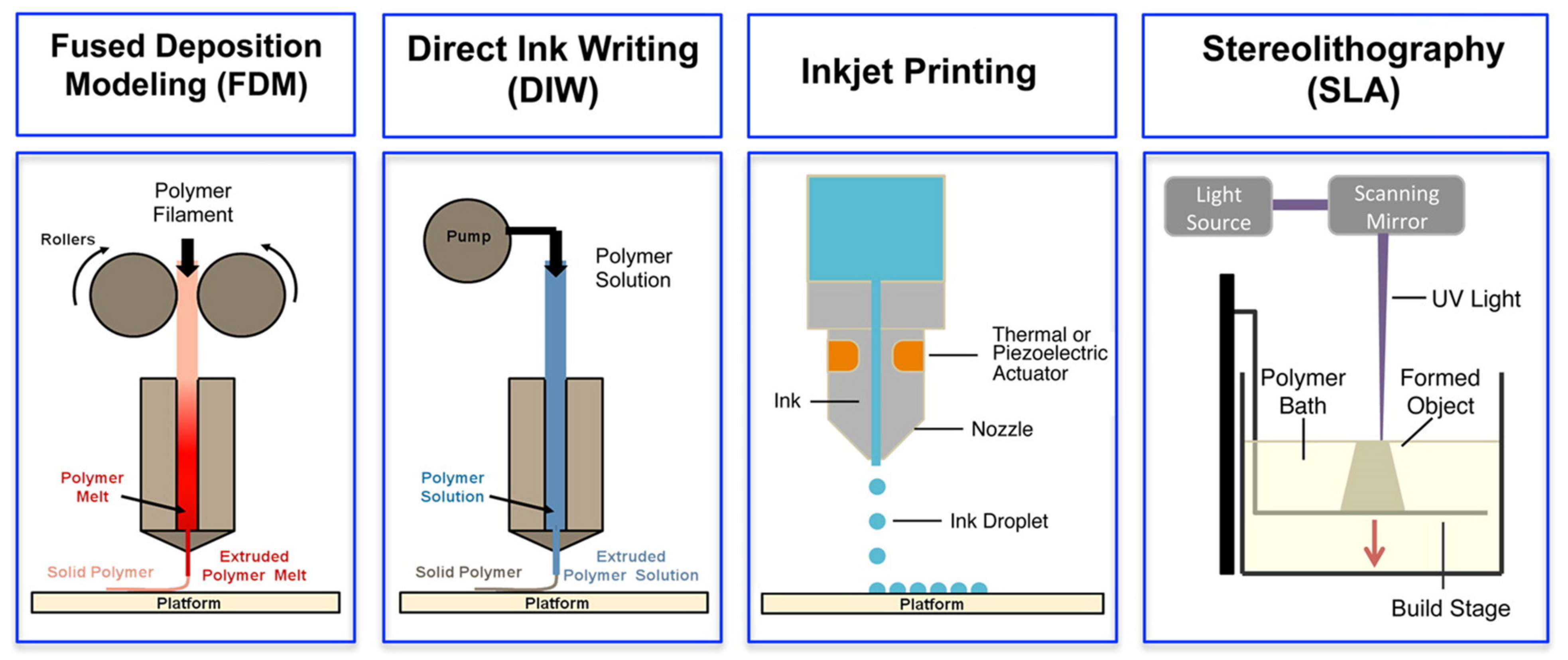
3.1. Fused Deposition Modelling (FDM)
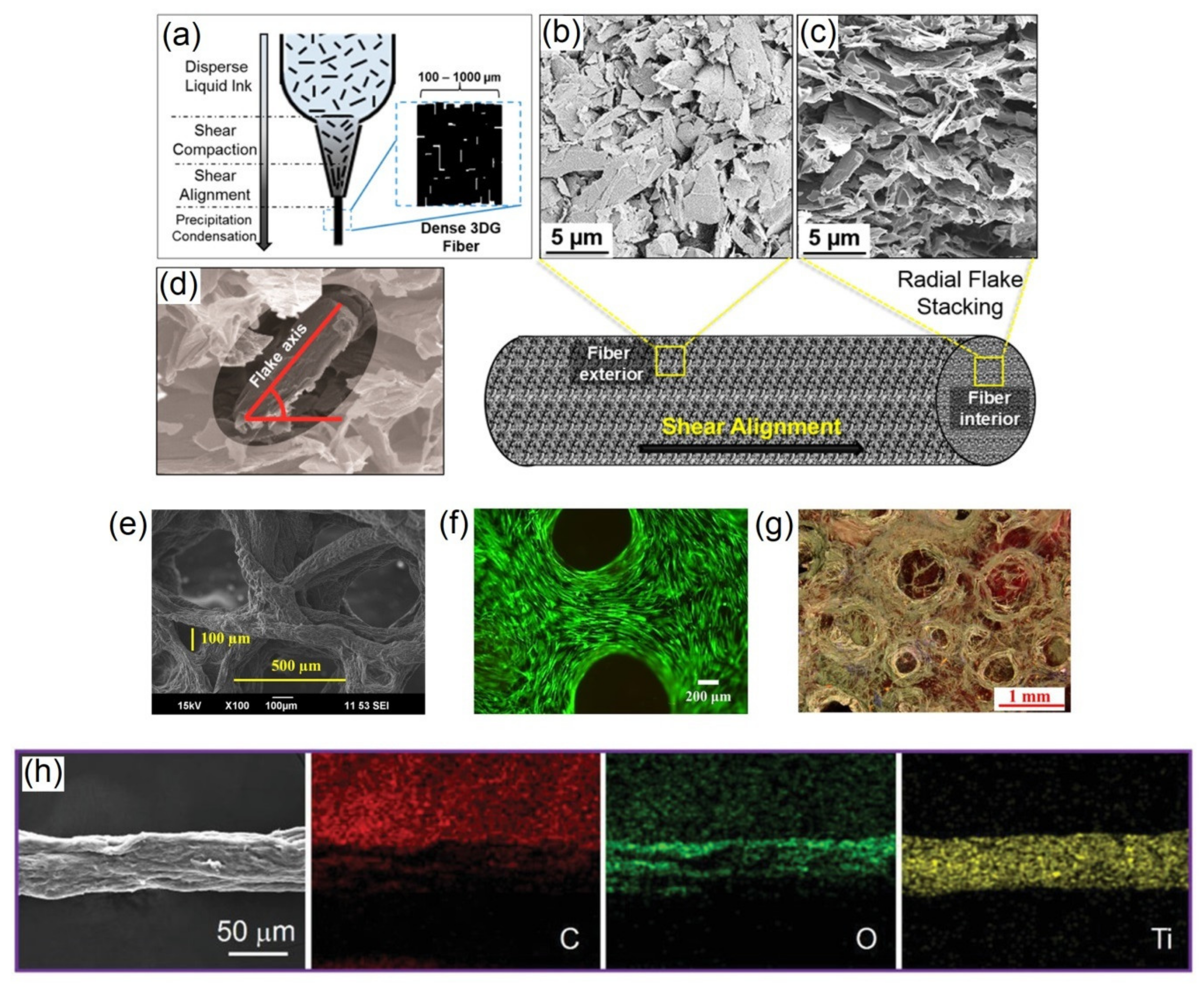
3.2. Direct Ink Writing (DIW)
3.3. Inkjet Printing
3.4. Stereolithography (SLA)
4. State-of-the-Art 3D Printed ECHs: Fabrication, Properties and Biomedical Applications
4.1. Conducting Polymer-Based Gel
| Hydrogel Composition | Bioink | Printing Methods and Parameters | Crosslinking/Post-Treatment | Electrical Properties | Mechanical Properties | Biocompatibility | Biomedical Applications | Reference |
|---|---|---|---|---|---|---|---|---|
| PEDOT:PSS | No | DIW: Nozzle diameter—30, 50, 100 and 200 µm. | Air-drying, annealing | Conductivity—28.0 S cm−1 (wet), and 155.0 S cm−1 (dry). | Compressive modulus—1.1 MPa (wet), and 1.5 GPa (dry). | Mouse dorsal hippocampus | Neural tissue engineering | [20] |
| PEGDA/PEDOT:PSS | No | SLA: Laser spot diameter—200 µm; print speed—8 mm/s; UV wavelength—355 nm. | Photocrosslinking | Resistance—0.7 to 2.8 kΩ/sq. | Compression stiffness—26.3 to 35.4 MPa. | Dorsal root ganglion neuronal cell differentiation under electrical stimulation | Neural tissue engineering | [29] |
| p(HEMA-co-EGMA)/PEDOT:PSS | No | SLA; EB: Nozzle diameter—200 µm; print speed—2.5 to 8.0 mm/s | UV curing | Resistance—100 to 125 kΩ. | Compressive modulus—82 kPa. | Neural progenitor cells | Neural tissue engineering | [30] |
| GelMA/PEDOT:PSS | Yes | DIW: Nozzle diameter—160 µm; print speed—5 to 10 mm/s; pressure—70 to 90 kPa. | Printing in CaCl2 support bath, photocrosslinking, isotherm | Resistance—261.0 to 281.2 kΩ. | Tensile modulus—40.9 to 141.7 kPa. | Mouse myoblast cells, subcutaneous implant in rats | Tissue engineering | [22] |
| MC/kCA/PEDOT:PSS | Yes | DIW: Nozzle diameter—210 µm; print speed—1, 2, 4, 6 and 8 mm/s; pressure—10, 15 and 20 psi. | Immersion in 5 wt% KCl solution | Conductivity—1.2 to 2.9 mS cm−1. | Compressive modulus—8.0 to 28.5 kPa. | Human embryonic kidney cells | Tissue engineering | [31] |
| Nafion/PEDOT | No | FDM: Substrate printing | Interfacial polymerization of EDOT monomers into post-printed Nafion matrix | Conductivity—1 to 5 S cm−1 (dry) | Tensile modulus—620 MPa (dry). | - | Wearable sensors | [33] |
| PAA/PPy-Chi | No | DIW: Nozzle diameter—300 µm; print speed—2 mm/s; pressure—40 psi. | Washing with 5 wt% ammonium persulfate solution | Conductivity—13.0 to 30.0 S cm−1. | Compressive modulus—0.6 to 0.8 MPa; stretchability—1500%. | - | Wearable sensors | [34] |
| PEGDA/PPy | No | SLA: Substrate printing | Interfacial polymerization of pyrrole monomers into post-printed PEGDA matrix | Resistance—0.013 to 3.5 MΩ.cm. | Compressive modulus—0.6 to 1.4 MPa. | - | Bioelectronics | [35] |
| PLLA/PPy | No | DIW: Nozzle diameter—260 µm; print speed—140 mm/min; pressure—5 kPa. | Printing with receiving condenser at -7 °C, freeze-drying | Conductivity—170 to 750 mS cm−1. | Compressive strength—18 to 32 MPa. | Mouse fibroblast cells | Tissue engineering | [36] |
| Alg/PPy | No | DIW: Nozzle diameter—100 µm; print speed—140 mm/min; pressure—5 kPa. | Printing in 15% ethanol coagulation bath with 5% CaCl2 | Conductivity—4.1 to 6.3 mS cm−1. | - | Neuronal cells | Neural tissue engineering | [37] |
| PANI | No | Inkjet: Microdot arrays—18 to 21.5 µm diameter; Nozzle diameter—9 to 40 µm. | In situ polymerization of aniline monomer | Conductivity—0.1 S cm−1. | - | - | Bioelectronics | [24] |
| GelMA/PANI | No | SLA: Substrate printing | Interfacial polymerization of aniline monomers into post-printed acidic GelMA matrix | Resistance—165.6 Ω. | Compressive modulus—13.7 to 15.2 kPa. | Murine mesenchymal progenitor cells | Bioelectronic interfaces | [25] |
| PSU/PANI | No | DIW: Nozzle diameter—600 µm; print speed—6.8 mm/s; pressure—93.6 psi. | - | Resistance—4.8 Ω.m (dry). | - | - | Implantable biodevices | [39] |
| PCL/PANI | No | FDM: Nozzle diameter—330 µm; print speed—20 mm/s; pressure—6 bar. | - | Conductivity—0.25 to 0.28 mS cm−1 (dry). | Compressive modulus—68.4 to 82.6 MPa (dry). | Human adipose-derived stem cells | Implantable biodevices | [40] |
4.2. Conductive Filler-Based Gel
| Hydrogel Composition | Bioink | Printing Methods and Parameters | Crosslinking/Post-Treatment | Electrical Properties | Mechanical Properties | Biocompatibility | Biomedical Applications | Reference |
|---|---|---|---|---|---|---|---|---|
| Chitosan/rGO | No | DIW: Nozzle diameter—200 µm; print speed—150 mm/min. | Printing in isopropyl alcohol precipitating bath | Conductivity—0.015 to 15 µS m−1 (dry). | Tensile strength—272 to 372 kPa. | Mouse fibroblast cells | Tissue engineering | [42] |
| ChiMA/rGO | No | DIW: Nozzle diameter—200 µm; print speed—150 mm/min. | Printing in isopropyl alcohol precipitating bath | Conductivity—20 to 250 µS m−1 (dry). | - | Mouse fibroblast cells | Tissue engineering | [44] |
| PEGDA/rGO | No | SLA: 50 µm projector resolution, print time—1.5 to 2 s/layer. | UV curing, thermal reduction of GO | Conductivity—95.8 to 109.5 n S cm−1. | Compressive modulus—6.8 to 8.7 MPa (dry). | - | Bioelectronics | [46] |
| PCL/rGO | No | FDM: Nozzle diameter—0.9 mm; print speed—0.3 mm/s; temperature 220 °C; pressure—6 bar. | Air-drying | Conductivity—0.68 µS m−1 (dry). | Human bone marrow-derived mesenchymal stem cells | Tissue engineering, anti-bacterial | [48] | |
| PAA/rGO | No | DIW: Nozzle diameter—600 µm. | Humidity curing, hydroiodic acid vapor induced reduction of GO | Resistance—230 to 855 kΩ. | - | - | Wearable | [51] |
| Alg/rGO | No | DIW: Substrate printing | Printing Alg/Gel, immersion in CaCl2 bath, Gel dissolution by thermal treatment, GO coating/incorporation, ascorbic acid induced reduction of GO | Resistance—1.5 kΩ/sq | Compressive modulus—195 kPa. | Human adipose stem cells | Tissue engineering | [52] |
| PLG/GNPs | No | DIW: Nozzle diameter—410 µm; print speed—10 to 45 mm/s; pressure—0.5 to 5.0 bar. | - | Conductivity—875 S m−1 (dry). | Compressive modulus—3.0 MPa (dry). | Human mesenchymal stem cells, subcutaneous implant in mouse | Nerve guide conduits | [21] |
| PLG/Hap/GNPs | No | DIW: Nozzle diameter: 100, 200 400 and 1000 µm, print speed: 10 to 75 mm/s; pressure—0.5 to 5.0 bar. | - | Conductivity—127 S cm−1 (dry). | Compressive modulus—3.0 MPa (dry). | Human mesenchymal stem cells | Tissue engineering | [43] |
| PEG/PEI/GNPs | No | DIW: Nozzle diameter—400 µm. | Spark plasma sintering, burning-out | Conductivity—5.6 to 533.5 S cm−1 (dry). | Compressive modulus—0.35 to 0.58 MPa (dry). | - | Bioelectronics | [45] |
| PLA/GNPs | No | FDM: Nozzle diameter—0.4 mm; temperature 210 °C. | Air-drying | Resistance –102 Ω.cm (dry). | Tensile modulus—2.4 GPa (dry). | - | Bioelectronics | [47] |
| PVB/GNPs | No | DIW: Nozzle diameter—300, 400 and 500 µm; print speed—5 to 15 mm/s; pressure—0.1 to 0.6 MPa. | Air-drying | Conductivity—130 to 230 S m−1 (dry). | Compressive modulus—0.57 to 4.37 MPa (dry). | - | Bioelectronics | [49] |
| HPC/Fe3O4-GNPs | No | DIW: Nozzle diameter—200 µm; print speed—1 mm/s; pressure—140 psi. | Annealing at different temperatures | Conductivity—85 to 580 S m−1 (dry). | - | - | Biosensors | [50] |
| TOCNF/Ti3C2-MXene | No | DIW: Nozzle diameter—600 µm; print speed—4.2 mm/s. | Immersion in ethanol coagulation bath | Conductivity—4.8 to 211.0 S m−1 (dry). | Tensile modulus—4.7 to 9.3 GPa (dry). | - | Wearable sensors | [53] |
| HA/Alg/Ti3C2-MXene | Yes | DIW: Nozzle diameter—210 µm; print speed—6 mm/s; pressure—5 and 15 psi. | Immersion in CaCl2 bath | Conductivity—1.2 to 7.2 mS cm−1 (ink). | Compressive modulus—2.8 to 5.5 kPa. | Human embryonic kidney cells | Tissue engineering | [55] |
| Alg/EGaIn-LM | No | Inkjet | Mechanical sintering | Conductivity—0.4 MS m−1 (dry). | - | - | Bioelectronics | [57] |
| TA/EGaIn-LM | No | DIW: Writing speed—2.5 mm/s. | Air-drying | Conductivity—0.29 to 1.6 MS m−1 (dry). | - | - | Bioelectronics | [58] |
4.3. Hybrid Methods for Fabrication of Multiscale 3D Printed ECH Structures
5. Conclusions and Outlook
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| Alg | Alginate |
| Chi | Chitosan |
| ChiMA | Chitosan methacrylate |
| TOCNF | Tempo oxidised cellulose nanofibers |
| DIW | Direct ink writing |
| EHD | Electrohydrodynamic |
| FDM | Fused deposition modelling |
| GO | Graphene oxide |
| Gel | Gelatin |
| GelMA | Gelatin methacrylate |
| GNPs | Graphene nanoplatelets |
| HA | Hyaluronic acid |
| Hap | Hydroxyapatite |
| HPC | Hydroxypropyl cellulose |
| kCA | Kappa-carrageenan |
| MC | Methylcellulose |
| PAA | Poly(acrylic acid) |
| PCL | Polycaprolactone |
| PEDOT | Poly(3,4-ethylenedioxythiophene) |
| PEG | Poly(ethylene glycol) |
| PEGDA | Poly(ethylene glycol) diacrylate |
| PEI | Polyethylenimine |
| PEGMA | Poly(ethylene glycol methacrylate) |
| PEO | Poly(ethylene oxide) |
| PHEMA | Poly(2-hydroxyethyl methacrylate) |
| PLA | Poly(lactic acid) |
| PLCL | Poly(l-lactic acid-co-caprolactone) |
| PLG | Poly(lactide-co-glycolide) |
| PLLA | Poly(l-lactide) |
| PPy | Polypyrrole |
| PSS | Polystyrene sulfonate |
| PSU | Polysulfone |
| PU | Polyurethane |
| PVA | Poly(vinyl alcohol) |
| PVB | Poly(vinyl butyral) |
| rGO | Reduced graphene oxide |
| SLA | Stereolithography |
| TA | Tannic acid |
References
- Sikorski, P. Electroconductive scaffolds for tissue engineering applications. Biomater. Sci. 2020, 8, 5583–5588. [Google Scholar] [CrossRef]
- Lu, H.; Zhang, N.; Ma, M. Electroconductive hydrogels for biomedical applications. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2019, 11, e1568. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Feng, P.; Chen, J.; Sun, Z.; Zhao, B. Electrically conductive hydrogels for flexible energy storage systems. Prog. Polym. Sci. 2019, 88, 220–240. [Google Scholar] [CrossRef]
- Vo, R.; Hsu, H.-H.; Jiang, X. Hydrogel facilitated bioelectronic integration. Biomater. Sci. 2021, 9, 23–37. [Google Scholar] [CrossRef] [PubMed]
- Min, J.H.; Patel, M.; Koh, W.G. Incorporation of conductive materials into hydrogels for tissue engineering applications. Polymers 2018, 10, 1078. [Google Scholar] [CrossRef] [PubMed]
- Fu, F.; Wang, J.; Zeng, H.; Yu, J. Functional conductive hydrogels for bioelectronics. ACS Mater. Lett. 2020, 2, 1287–1301. [Google Scholar] [CrossRef]
- Guo, B.; Ma, P.X. Conducting polymers for tissue engineering. Biomacromolecules 2018, 19, 1764–1782. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Sun, Y.; Ding, H.; Zhao, X.; Zhang, L.; Bai, J.; Liu, K. Bioelectronics-related 2D materials beyond graphene: Fundamentals, properties, and applications. Adv. Funct. Mater. 2020, 30, 2003732. [Google Scholar] [CrossRef]
- Shin, S.R.; Li, Y.-C.; Jang, H.L.; Khoshakhlagh, P.; Akbari, M.; Nasajpour, A.; Zhang, Y.S.; Tamayol, A.; Khademhosseini, A. Graphene-based materials for tissue engineering. Adv. Drug Deliv. Rev. 2016, 105, 255–274. [Google Scholar] [CrossRef]
- Yan, J.; Lu, Y.; Chen, G.; Yang, M.; Gu, Z. Advances in liquid metals for biomedical applications. Chem. Soc. Rev. 2018, 47, 2518–2533. [Google Scholar] [CrossRef]
- Zhang, Y.-Z.; El-Demellawi, J.K.; Jiang, Q.; Ge, G.; Liang, H.; Lee, K.; Dong, X.; Alshareef, H.N. Mxene hydrogels: Fundamentals and applications. Chem. Soc. Rev. 2020, 49, 7229–7251. [Google Scholar] [CrossRef] [PubMed]
- Zhao, P.; Gu, H.; Mi, H.; Rao, C.; Fu, J.; Turng, L.-s. Fabrication of scaffolds in tissue engineering: A review. Front. Mech. Eng. 2018, 13, 107–119. [Google Scholar] [CrossRef]
- Li, J.; Wu, C.; Chu, P.K.; Gelinsky, M. 3D printing of hydrogels: Rational design strategies and emerging biomedical applications. Mater. Sci. Eng. R Rep. 2020, 140, 100543. [Google Scholar] [CrossRef]
- Unagolla, J.M.; Jayasuriya, A.C. Hydrogel-based 3D bioprinting: A comprehensive review on cell-laden hydrogels, bioink formulations, and future perspectives. Appl. Mater. Today 2020, 18, 100479. [Google Scholar] [CrossRef] [PubMed]
- Distler, T.; Boccaccini, A.R. 3D printing of electrically conductive hydrogels for tissue engineering and biosensors—A review. Acta Biomater. 2020, 101, 1–13. [Google Scholar] [CrossRef]
- Balint, R.; Cassidy, N.J.; Cartmell, S.H. Conductive polymers: Towards a smart biomaterial for tissue engineering. Acta Biomater. 2014, 10, 2341–2353. [Google Scholar] [CrossRef]
- Bredas, J.L.; Street, G.B. Polarons, bipolarons, and solitons in conducting polymers. Acc. Chem. Res. 1985, 18, 309–315. [Google Scholar] [CrossRef]
- Blinova, N.V.; Stejskal, J.; Trchová, M.; Prokeš, J. Control of polyaniline conductivity and contact angles by partial protonation. Polym. Int. 2008, 57, 66–69. [Google Scholar] [CrossRef]
- Guvendiren, M.; Molde, J.; Soares, R.M.D.; Kohn, J. Designing biomaterials for 3D printing. ACS Biomater. Sci. Eng. 2016, 2, 1679–1693. [Google Scholar] [CrossRef]
- Yuk, H.; Lu, B.; Lin, S.; Qu, K.; Xu, J.; Luo, J.; Zhao, X. 3D printing of conducting polymers. Nat. Commun. 2020, 11, 1604. [Google Scholar] [CrossRef]
- Jakus, A.E.; Secor, E.B.; Rutz, A.L.; Jordan, S.W.; Hersam, M.C.; Shah, R.N. Three-dimensional printing of high-content graphene scaffolds for electronic and biomedical applications. ACS Nano 2015, 9, 4636–4648. [Google Scholar] [CrossRef] [PubMed]
- Spencer, A.R.; Shirzaei Sani, E.; Soucy, J.R.; Corbet, C.C.; Primbetova, A.; Koppes, R.A.; Annabi, N. Bioprinting of a cell-laden conductive hydrogel composite. ACS Appl. Mater. Interfaces 2019, 11, 30518–30533. [Google Scholar] [CrossRef] [PubMed]
- Tran, T.S.; Dutta, N.K.; Choudhury, N.R. Poly(ionic liquid)-stabilized graphene nanoinks for scalable 3D printing of graphene aerogels. ACS Appl. Nano Mater. 2020, 3, 11608–11619. [Google Scholar] [CrossRef]
- Pan, L.; Yu, G.; Zhai, D.; Lee, H.R.; Zhao, W.; Liu, N.; Wang, H.; Tee, B.C.-K.; Shi, Y.; Cui, Y.; et al. Hierarchical nanostructured conducting polymer hydrogel with high electrochemical activity. Proc. Natl. Acad. Sci. USA 2012, 109, 9287–9292. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Chen, Y.X.; Yan, J.; Quinn, D.; Dong, P.; Sawyer, S.W.; Soman, P. Fabrication of conductive gelatin methacrylate–polyaniline hydrogels. Acta Biomater. 2016, 33, 122–130. [Google Scholar] [CrossRef] [PubMed]
- Yuk, H.; Lu, B.; Zhao, X. Hydrogel bioelectronics. Chem. Soc. Rev. 2019, 48, 1642–1667. [Google Scholar] [CrossRef]
- Baoyang, L.; Qi, Z.; Jingkun, X.; Yu, G. Conductive Polymer 3D Printing Ink and Preparation Method Thereof. CN Patent CN110922810A, 27 March 2020. [Google Scholar]
- Vasile, C.; Pamfil, D.; Stoleru, E.; Baican, M. New developments in medical applications of hybrid hydrogels containing natural polymers. Molecules 2020, 25, 1539. [Google Scholar] [CrossRef]
- Heo, D.N.; Lee, S.-J.; Timsina, R.; Qiu, X.; Castro, N.J.; Zhang, L.G. Development of 3D printable conductive hydrogel with crystallized pedot:Pss for neural tissue engineering. Mater. Sci. Eng. C 2019, 99, 582–590. [Google Scholar] [CrossRef]
- Aggas, J.R.; Abasi, S.; Phipps, J.F.; Podstawczyk, D.A.; Guiseppi-Elie, A. Microfabricated and 3-D printed electroconductive hydrogels of pedot:Pss and their application in bioelectronics. Biosens. Bioelectron. 2020, 168, 112568. [Google Scholar] [CrossRef]
- Rastin, H.; Zhang, B.; Bi, J.; Hassan, K.; Tung, T.T.; Losic, D. 3D printing of cell-laden electroconductive bioinks for tissue engineering applications. J. Mater. Chem. B 2020, 8, 5862–5876. [Google Scholar] [CrossRef]
- Kim, G.; Kim, H.; Kim, I.J.; Kim, J.R.; Lee, J.I.; Ree, M. Bacterial adhesion, cell adhesion and biocompatibility of nafion films. J. Biomater. Sci. Polym. Ed. 2009, 20, 1687–1707. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, A.I.; Östergren, I.; Kim, Y.; Fauth, S.; Craighero, M.; Yoon, M.-H.; Lund, A.; Müller, C. All-polymer conducting fibers and 3D prints via melt processing and templated polymerization. ACS Appl. Mater. Interfaces 2020, 12, 8713–8721. [Google Scholar] [CrossRef] [PubMed]
- Darabi, M.A.; Khosrozadeh, A.; Mbeleck, R.; Liu, Y.; Chang, Q.; Jiang, J.; Cai, J.; Wang, Q.; Luo, G.; Xing, M. Skin-inspired multifunctional autonomic-intrinsic conductive self-healing hydrogels with pressure sensitivity, stretchability, and 3D printability. Adv. Mater. 2017, 29, 1700533. [Google Scholar] [CrossRef] [PubMed]
- Fantino, E.; Roppolo, I.; Zhang, D.; Xiao, J.; Chiappone, A.; Castellino, M.; Guo, Q.; Pirri, C.F.; Yang, J. 3D printing/interfacial polymerization coupling for the fabrication of conductive hydrogel. Macromol. Mater. Eng. 2018, 303, 1700356. [Google Scholar] [CrossRef]
- Ma, C.; Jiang, L.; Wang, Y.; Gang, F.; Xu, N.; Li, T.; Liu, Z.; Chi, Y.; Wang, X.; Zhao, L.; et al. 3D printing of conductive tissue engineering scaffolds containing polypyrrole nanoparticles with different morphologies and concentrations. Materials 2019, 12, 2491. [Google Scholar] [CrossRef]
- Wright, C.J.; Molino, B.Z.; Chung, J.H.Y.; Pannell, J.T.; Kuester, M.; Molino, P.J.; Hanks, T.W. Synthesis and 3D printing of conducting alginate–polypyrrole ionomers. Gels 2020, 6, 13. [Google Scholar] [CrossRef]
- Dufresne, M.; Bacchin, P.; Cerino, G.; Remigy, J.C.; Adrianus, G.N.; Aimar, P.; Legallais, C. Human hepatic cell behavior on polysulfone membrane with double porosity level. J. Membr. Sci. 2013, 428, 454–461. [Google Scholar] [CrossRef][Green Version]
- Miao, Z.; Seo, J.; Hickner, M.A. Solvent-cast 3D printing of polysulfone and polyaniline composites. Polymer 2018, 152, 18–24. [Google Scholar] [CrossRef]
- Wibowo, A.; Vyas, C.; Cooper, G.; Qulub, F.; Suratman, R.; Mahyuddin, A.I.; Dirgantara, T.; Bartolo, P. 3D printing of polycaprolactone–polyaniline electroactive scaffolds for bone tissue engineering. Materials 2020, 13, 512. [Google Scholar] [CrossRef]
- Lu, H.; Zhang, S.; Guo, L.; Li, W. Applications of graphene-based composite hydrogels: A review. RSC Adv. 2017, 7, 51008–51020. [Google Scholar] [CrossRef]
- Sayyar, S.; Murray, E.; Thompson, B.C.; Chung, J.; Officer, D.L.; Gambhir, S.; Spinks, G.M.; Wallace, G.G. Processable conducting graphene/chitosan hydrogels for tissue engineering. J. Mater. Chem. B 2015, 3, 481–490. [Google Scholar] [CrossRef] [PubMed]
- Jakus, A.E.; Shah, R.N. Multi and mixed 3D-printing of graphene-hydroxyapatite hybrid materials for complex tissue engineering. J. Biomed. Mater. Res. Part A 2017, 105, 274–283. [Google Scholar] [CrossRef] [PubMed]
- Sayyar, S.; Gambhir, S.; Chung, J.; Officer, D.L.; Wallace, G.G. 3D printable conducting hydrogels containing chemically converted graphene. Nanoscale 2017, 9, 2038–2050. [Google Scholar] [CrossRef] [PubMed]
- De la Osa, G.; Pérez-Coll, D.; Miranzo, P.; Osendi, M.I.; Belmonte, M. Printing of graphene nanoplatelets into highly electrically conductive three-dimensional porous macrostructures. Chem. Mater. 2016, 28, 6321–6328. [Google Scholar] [CrossRef]
- Chiappone, A.; Roppolo, I.; Naretto, E.; Fantino, E.; Calignano, F.; Sangermano, M.; Pirri, F. Study of graphene oxide-based 3D printable composites: Effect of the in situ reduction. Compos. B Eng. 2017, 124, 9–15. [Google Scholar] [CrossRef]
- Prashantha, K.; Roger, F. Multifunctional properties of 3D printed poly(lactic acid)/graphene nanocomposites by fused deposition modeling. J. Macromol. Sci. Part A Pure Appl. Chem. 2017, 54, 24–29. [Google Scholar] [CrossRef]
- Angulo-Pineda, C.; Srirussamee, K.; Palma, P.; Fuenzalida, V.M.; Cartmell, S.H.; Palza, H. Electroactive 3D printed scaffolds based on percolated composites of polycaprolactone with thermally reduced graphene oxide for antibacterial and tissue engineering applications. Nanomaterials 2020, 10, 428. [Google Scholar] [CrossRef]
- Huang, K.; Yang, J.; Dong, S.; Feng, Q.; Zhang, X.; Ding, Y.; Hu, J. Anisotropy of graphene scaffolds assembled by three-dimensional printing. Carbon 2018, 130, 1–10. [Google Scholar] [CrossRef]
- Wajahat, M.; Kim, J.H.; Ahn, J.; Lee, S.; Bae, J.; Pyo, J.; Seol, S.K. 3D printing of Fe3O4 functionalized graphene-polymer (fgp) composite microarchitectures. Carbon 2020, 167, 278–284. [Google Scholar] [CrossRef]
- Wang, Y.; Chang, Q.; Zhan, R.; Xu, K.; Wang, Y.; Zhang, X.; Li, B.; Luo, G.; Xing, M.; Zhong, W. Tough but self-healing and 3D printable hydrogels for e-skin, e-noses and laser controlled actuators. J. Mater. Chem. A 2019, 7, 24814–24829. [Google Scholar] [CrossRef]
- Li, J.; Liu, X.; Crook, J.M.; Wallace, G.G. 3D printing of cytocompatible graphene/alginate scaffolds for mimetic tissue constructs. Front. Bioeng. Biotechnol. 2020, 8, 824. [Google Scholar] [CrossRef] [PubMed]
- Cao, W.-T.; Ma, C.; Mao, D.-S.; Zhang, J.; Ma, M.-G.; Chen, F. Mxene-reinforced cellulose nanofibril inks for 3D-printed smart fibres and textiles. Adv. Funct. Mater. 2019, 29, 1905898. [Google Scholar] [CrossRef]
- Zhang, C.; McKeon, L.; Kremer, M.P.; Park, S.-H.; Ronan, O.; Seral-Ascaso, A.; Barwich, S.; Coileáin, C.Ó.; McEvoy, N.; Nerl, H.C.; et al. Additive-free mxene inks and direct printing of micro-supercapacitors. Nat. Commun. 2019, 10, 1795. [Google Scholar] [CrossRef] [PubMed]
- Rastin, H.; Zhang, B.; Mazinani, A.; Hassan, K.; Bi, J.; Tung, T.T.; Losic, D. 3D bioprinting of cell-laden electroconductive mxene nanocomposite bioinks. Nanoscale 2020, 12, 16069–16080. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.; Liu, F.; Zhang, R.; Liu, J. Suspension 3D printing of fluid metal into self-healing hydrogel. Adv. Mater. Technol. 2017, 2, 1700173. [Google Scholar] [CrossRef]
- Li, X.; Li, M.; Zong, L.; Wu, X.; You, J.; Du, P.; Li, C. Liquid metal droplets wrapped with polysaccharide microgel as biocompatible aqueous ink for flexible conductive devices. Adv. Funct. Mater. 2018, 28, 1804197. [Google Scholar] [CrossRef]
- Rahim, M.A.; Centurion, F.; Han, J.; Abbasi, R.; Mayyas, M.; Sun, J.; Christoe, M.J.; Esrafilzadeh, D.; Allioux, F.-M.; Ghasemian, M.B.; et al. Polyphenol-induced adhesive liquid metal inks for substrate-independent direct pen writing. Adv. Funct. Mater. 2020, 2007336. [Google Scholar] [CrossRef]
- Lee, S.J.; Heo, D.N.; Park, J.S.; Kwon, S.K.; Lee, J.H.; Lee, J.H.; Kim, W.D.; Kwon, I.K.; Park, S.A. Characterization and preparation of bio-tubular scaffolds for fabricating artificial vascular grafts by combining electrospinning and a 3D printing system. Phys. Chem. Chem. Phys. 2015, 17, 2996–2999. [Google Scholar] [CrossRef]
- Chen, X.; Liu, X.; Childs, P.; Brandon, N.; Wu, B. A low cost desktop electrochemical metal 3D printer. Adv. Mater. Technol. 2017, 2, 1700148. [Google Scholar] [CrossRef]
- Xue, J.; Wu, T.; Dai, Y.; Xia, Y. Electrospinning and electrospun nanofibers: Methods, materials, and applications. Chem. Rev. 2019, 119, 5298–5415. [Google Scholar] [CrossRef]
- Maurmann, N.; Pereira, D.P.; Burguez, D.; de S Pereira, F.D.A.; Inforçatti Neto, P.; Rezende, R.A.; Gamba, D.; da Silva, J.V.L.; Pranke, P. Mesenchymal stem cells cultivated on scaffolds formed by 3D printed pcl matrices, coated with plga electrospun nanofibers for use in tissue engineering. Biomed. Phys. Eng. Express 2017, 3, 045005. [Google Scholar] [CrossRef]
- Yu, Y.; Hua, S.; Yang, M.; Fu, Z.; Teng, S.; Niu, K.; Zhao, Q.; Yi, C. Fabrication and characterization of electrospinning/3D printing bone tissue engineering scaffold. RSC Adv. 2016, 6, 110557–110565. [Google Scholar] [CrossRef]
- Rampichová, M.; Košt’áková Kuželová, E.; Filová, E.; Chvojka, J.; Šafka, J.; Pelcl, M.; Daňková, J.; Prosecká, E.; Buzgo, M.; Plencner, M.; et al. Composite 3D printed scaffold with structured electrospun nanofibers promotes chondrocyte adhesion and infiltration. Cell Adhes. Migr. 2018, 12, 271–285. [Google Scholar] [CrossRef] [PubMed]
- Vyas, C.; Ates, G.; Aslan, E.; Hart, J.; Huang, B.; Bartolo, P. Three-dimensional printing and electrospinning dual-scale polycaprolactone scaffolds with low-density and oriented fibers to promote cell alignment. 3D Print. Addit. Manuf. 2020, 7, 105–113. [Google Scholar] [CrossRef]
- Chang, J.; He, J.; Lei, Q.; Li, D. Electrohydrodynamic printing of microscale pedot:Pss-peo features with tunable conductive/thermal properties. ACS Appl. Mater. Interfaces 2018, 10, 19116–19122. [Google Scholar] [CrossRef]
- Kozior, T.; Mamun, A.; Trabelsi, M.; Wortmann, M.; Lilia, S.; Ehrmann, A. Electrospinning on 3D printed polymers for mechanically stabilized filter composites. Polymers 2019, 11, 2034. [Google Scholar] [CrossRef]
- Jordahl, J.H.; Solorio, L.; Sun, H.; Ramcharan, S.; Teeple, C.B.; Haley, H.R.; Lee, K.J.; Eyster, T.W.; Luker, G.D.; Krebsbach, P.H.; et al. 3D jet writing: Functional microtissues based on tessellated scaffold architectures. Adv. Mater. 2018, 30, 1707196. [Google Scholar] [CrossRef]
- Vijayavenkataraman, S.; Kannan, S.; Cao, T.; Fuh, J.Y.H.; Sriram, G.; Lu, W.F. 3D-printed pcl/ppy conductive scaffolds as three-dimensional porous nerve guide conduits (ngcs) for peripheral nerve injury repair. Front. Bioeng. Biotechnol. 2019, 7, 266. [Google Scholar] [CrossRef]
- Wang, J.; Wang, H.; Mo, X.; Wang, H. Reduced graphene oxide-encapsulated microfiber patterns enable controllable formation of neuronal-like networks. Adv. Mater. 2020, 32, 2004555. [Google Scholar] [CrossRef]
- Ambrosi, A.; Webster, R.D.; Pumera, M. Electrochemically driven multi-material 3D-printing. Appl. Mater. Today 2020, 18, 100530. [Google Scholar] [CrossRef]
- Wang, E.; Desai, M.S.; Lee, S.-W. Light-controlled graphene-elastin composite hydrogel actuators. Nano Lett. 2013, 13, 2826–2830. [Google Scholar] [CrossRef] [PubMed]
- Nadgorny, M.; Xiao, Z.; Chen, C.; Connal, L.A. Three-dimensional printing of ph-responsive and functional polymers on an affordable desktop printer. ACS Appl. Mater. Interfaces 2016, 8, 28946–28954. [Google Scholar] [CrossRef] [PubMed]
- Han, D.; Lu, Z.; Chester, S.A.; Lee, H. Micro 3D printing of a temperature-responsive hydrogel using projection micro-stereolithography. Sci. Rep. 2018, 8, 1963. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Z.; Kuang, X.; Yuan, C.; Qi, H.J.; Fang, D. Hydrophilic/hydrophobic composite shape-shifting structures. ACS Appl. Mater. Interfaces 2018, 10, 19932–19939. [Google Scholar] [CrossRef]
- Han, D.; Farino, C.; Yang, C.; Scott, T.; Browe, D.; Choi, W.; Freeman, J.W.; Lee, H. Soft robotic manipulation and locomotion with a 3D printed electroactive hydrogel. ACS Appl. Mater. Interfaces 2018, 10, 17512–17518. [Google Scholar] [CrossRef]
- Champeau, M.; Heinze, D.A.; Viana, T.N.; de Souza, E.R.; Chinellato, A.C.; Titotto, S. 4d printing of hydrogels: A review. Adv. Funct. Mater. 2020, 30, 1910606. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Athukorala, S.S.; Tran, T.S.; Balu, R.; Truong, V.K.; Chapman, J.; Dutta, N.K.; Roy Choudhury, N. 3D Printable Electrically Conductive Hydrogel Scaffolds for Biomedical Applications: A Review. Polymers 2021, 13, 474. https://doi.org/10.3390/polym13030474
Athukorala SS, Tran TS, Balu R, Truong VK, Chapman J, Dutta NK, Roy Choudhury N. 3D Printable Electrically Conductive Hydrogel Scaffolds for Biomedical Applications: A Review. Polymers. 2021; 13(3):474. https://doi.org/10.3390/polym13030474
Chicago/Turabian StyleAthukorala, Sandya Shiranthi, Tuan Sang Tran, Rajkamal Balu, Vi Khanh Truong, James Chapman, Naba Kumar Dutta, and Namita Roy Choudhury. 2021. "3D Printable Electrically Conductive Hydrogel Scaffolds for Biomedical Applications: A Review" Polymers 13, no. 3: 474. https://doi.org/10.3390/polym13030474
APA StyleAthukorala, S. S., Tran, T. S., Balu, R., Truong, V. K., Chapman, J., Dutta, N. K., & Roy Choudhury, N. (2021). 3D Printable Electrically Conductive Hydrogel Scaffolds for Biomedical Applications: A Review. Polymers, 13(3), 474. https://doi.org/10.3390/polym13030474










