Solvent-Free Processing of Drug-Loaded Poly(ε-Caprolactone) Scaffolds with Tunable Macroporosity by Combination of Supercritical Foaming and Thermal Porogen Leaching †
Abstract
1. Introduction
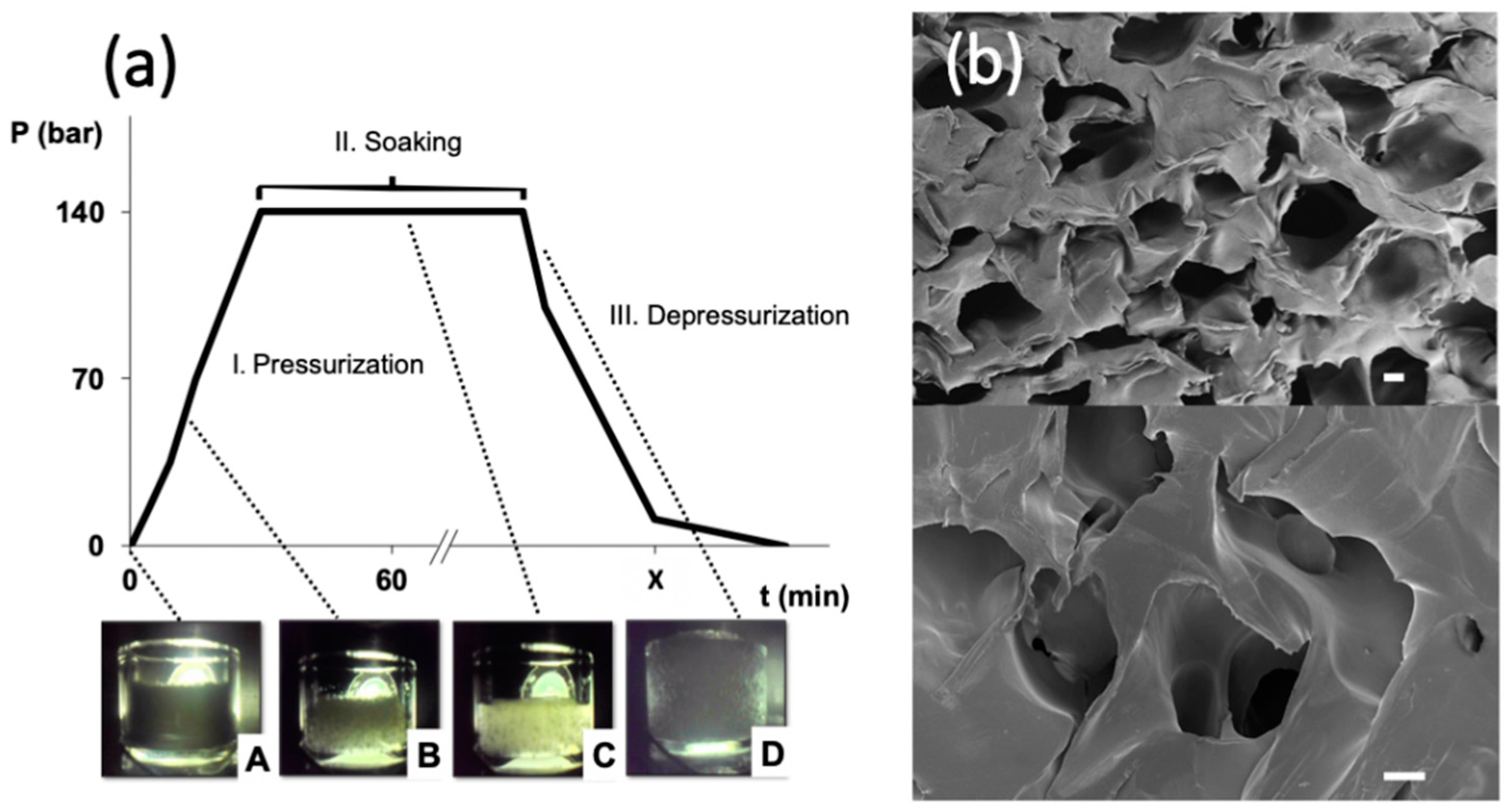
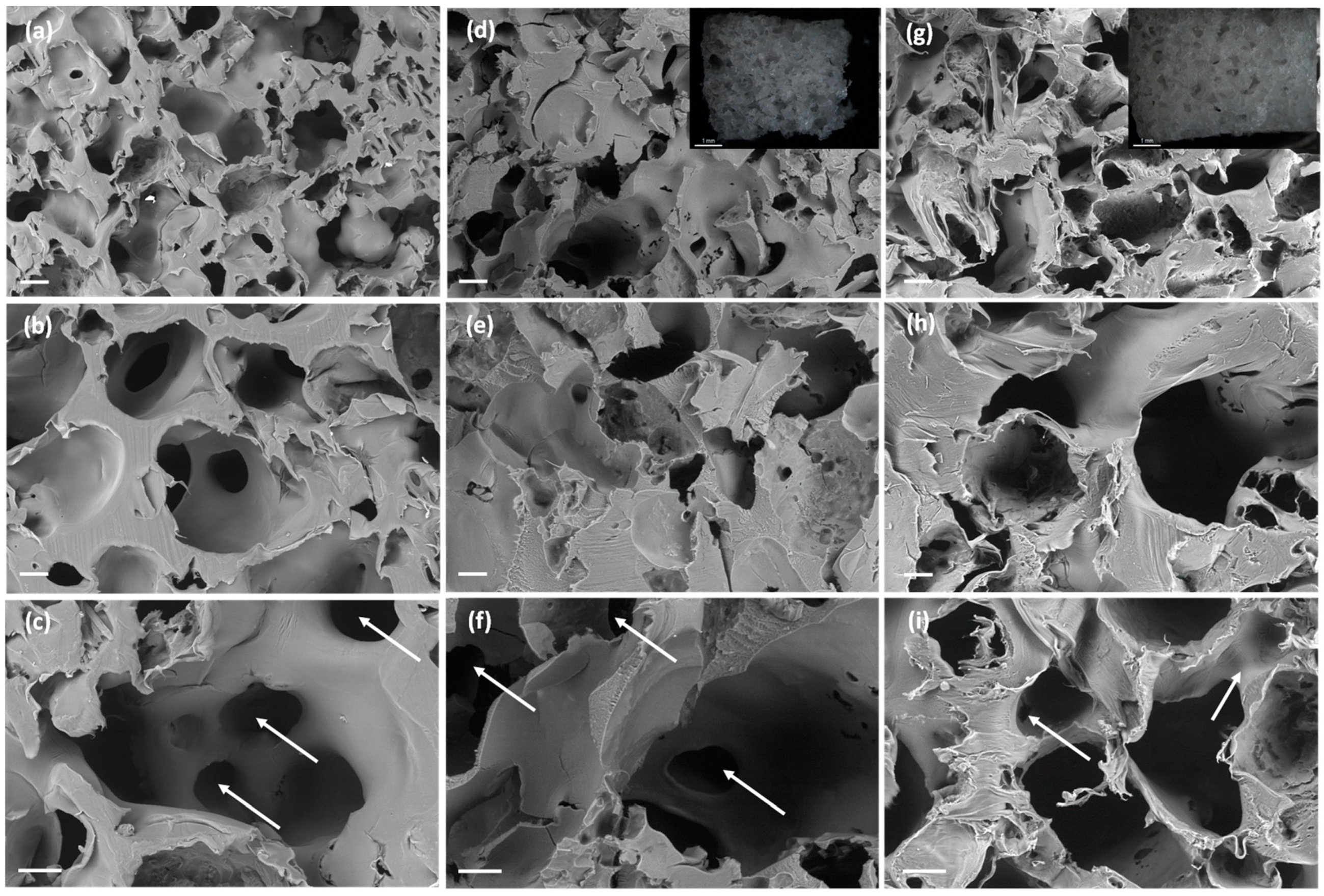
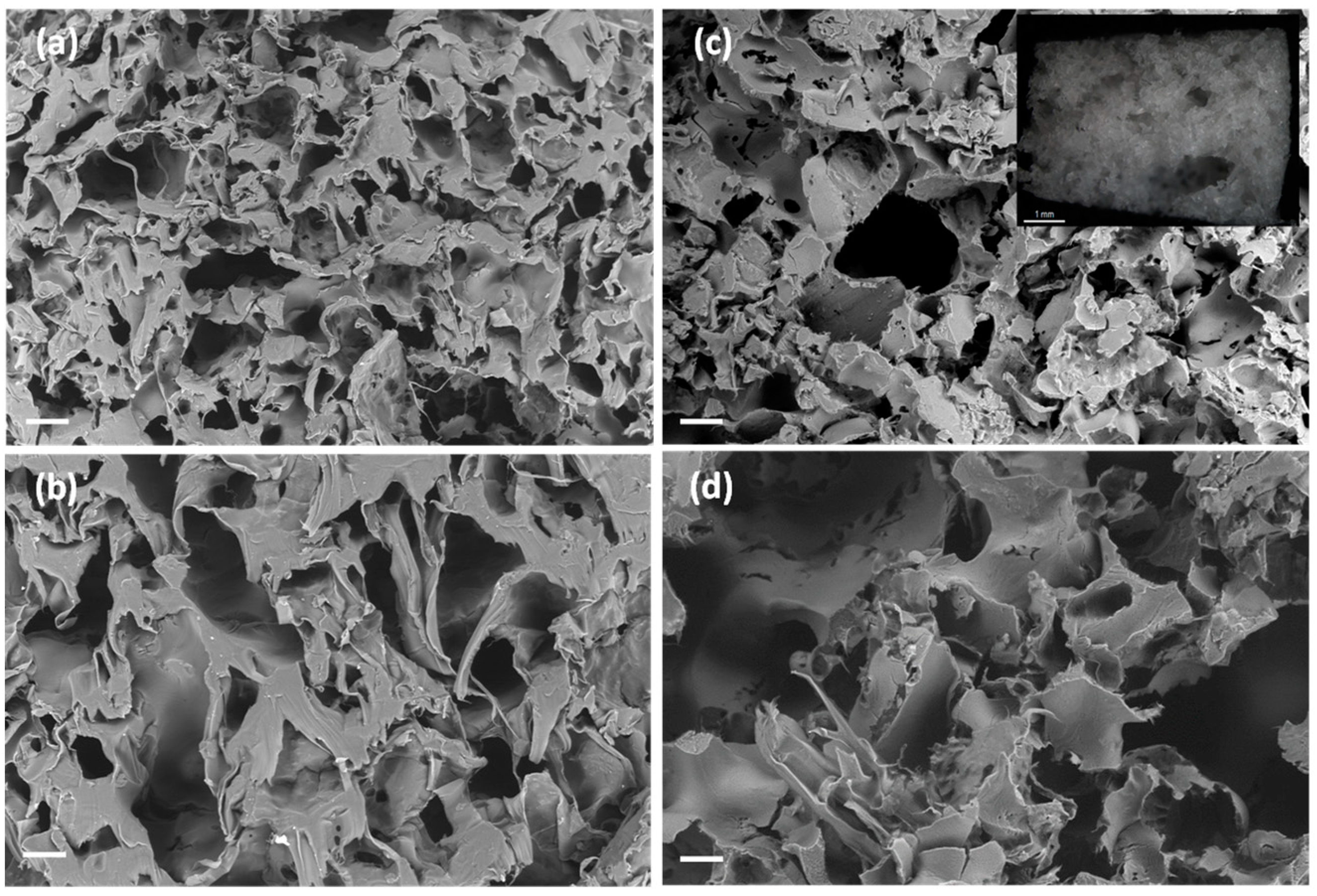
2. Results and Discussion
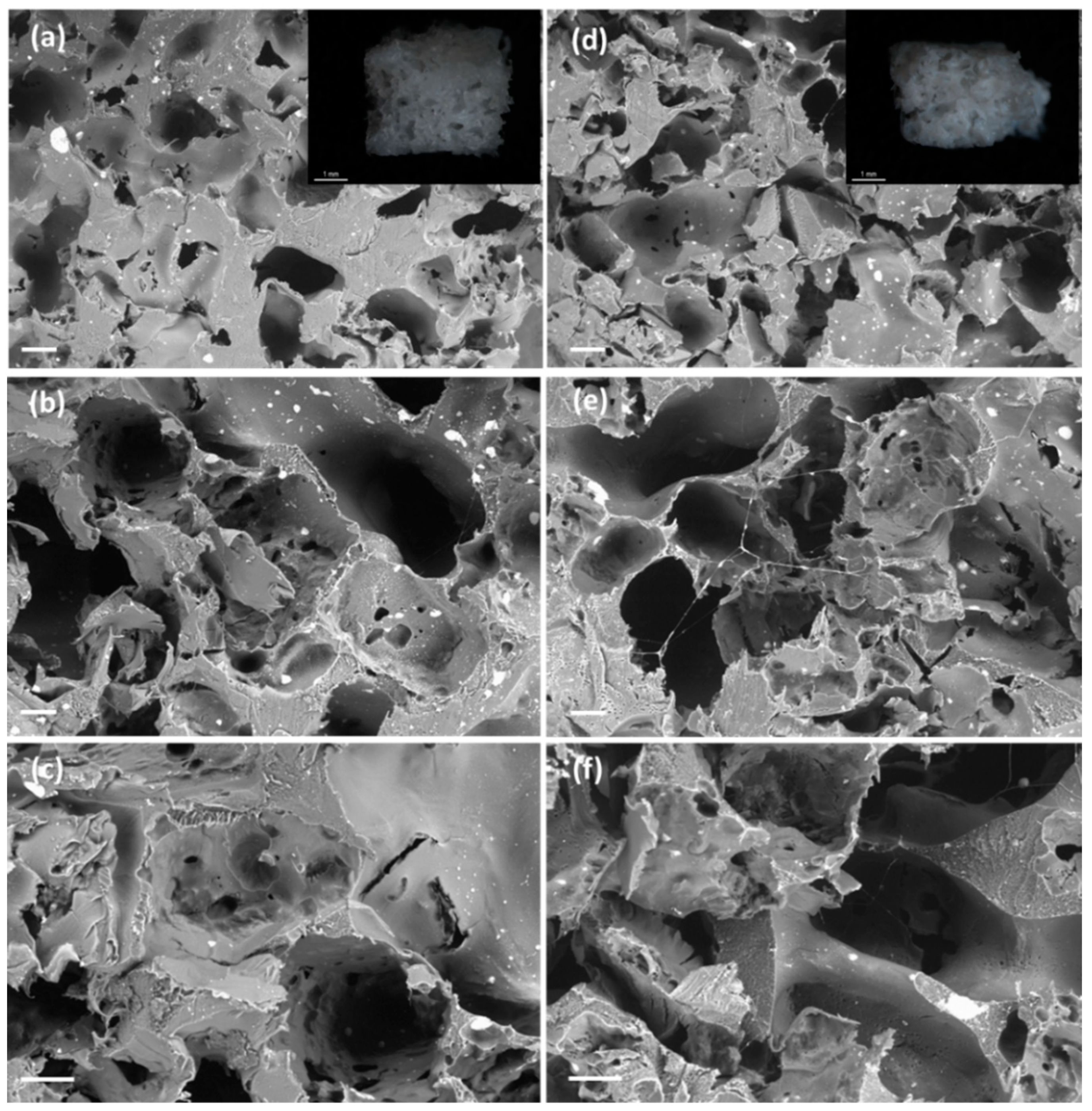
2.1. Scaffolds Development and Morphological Characterization
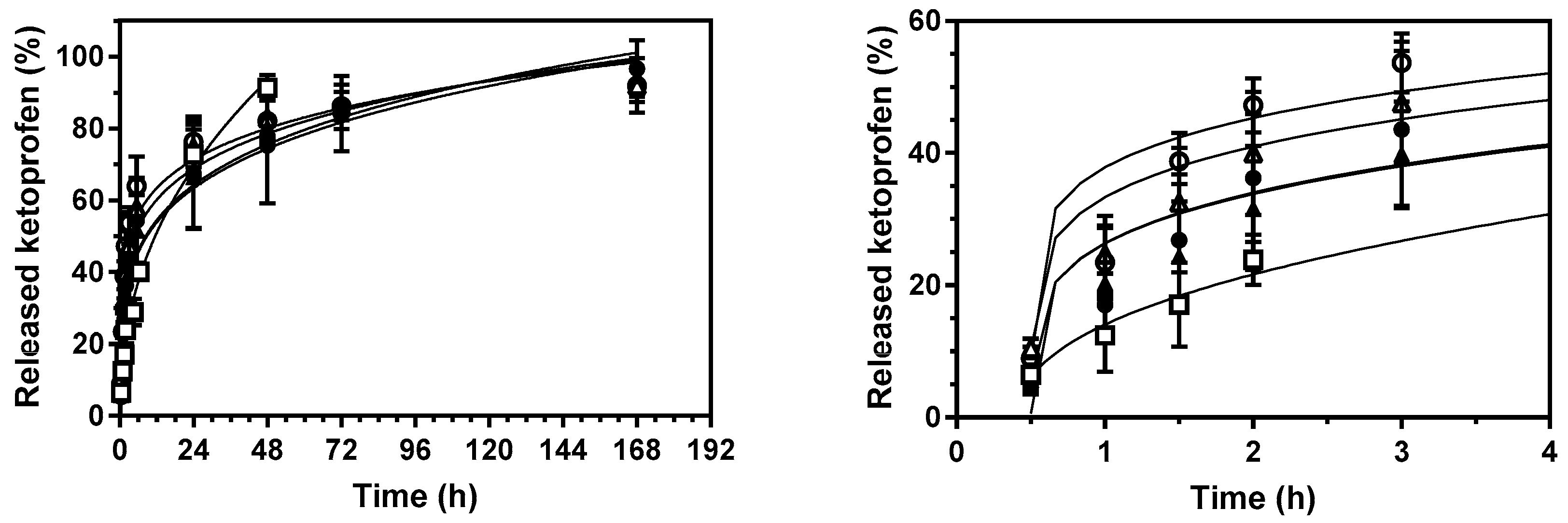
2.2. Ketoprofen Release Studies
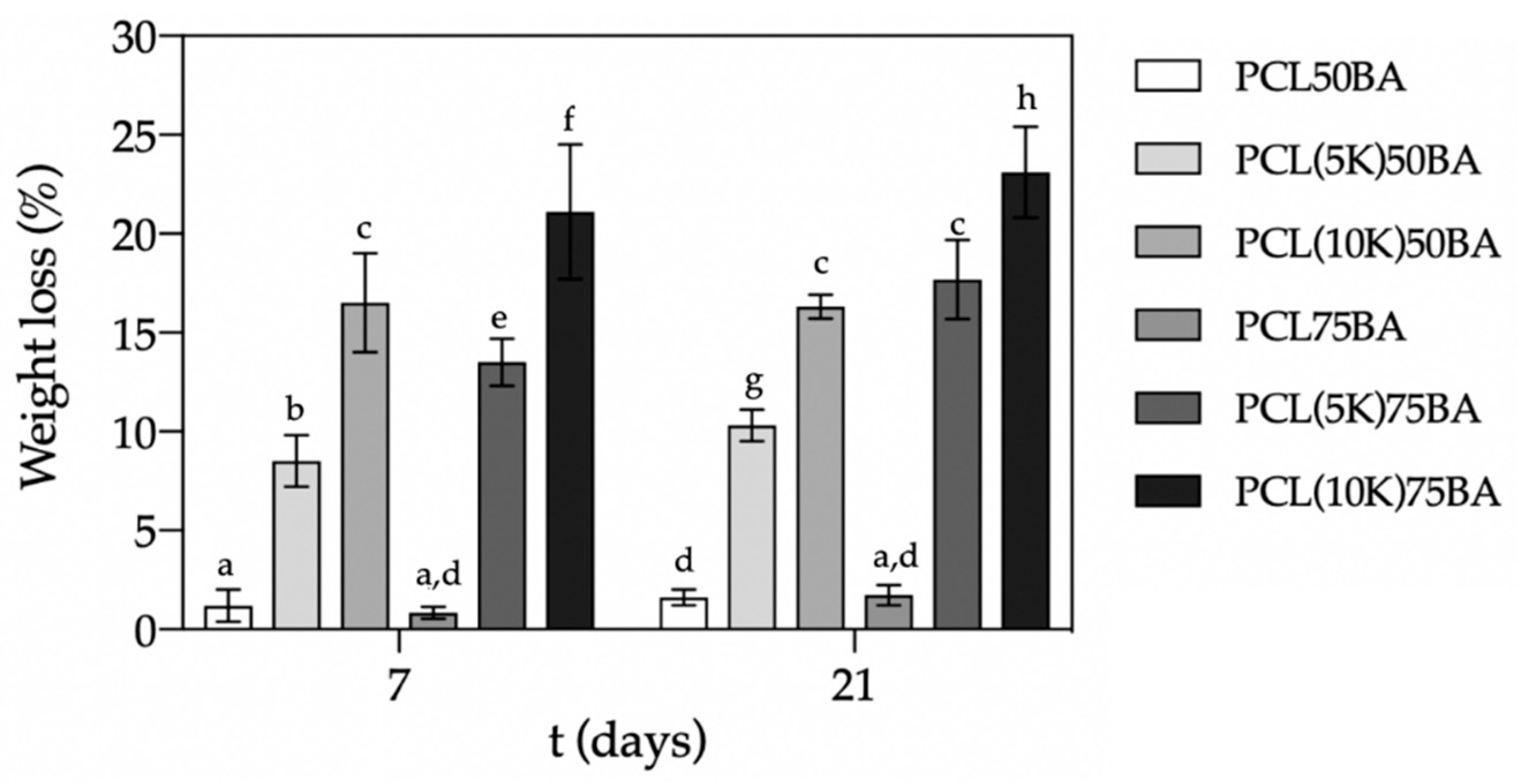
2.3. PCL-Scaffold Degradation Studies
2.4. Cytotoxicity Tests
3. Materials and Methods
3.1. Materials
3.2. Macroporous PCL-Ketoprofen Composite Scaffold Preparation
3.3. In Situ Visual Follow-Up of the Supercritical Foaming of Scaffolds
3.4. Structural and Physicochemical Characterization of the Scaffolds
3.5. Ketoprofen Release Studies
3.6. Cytotoxicity Tests
3.7. Statistical Analysis
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
| 1st Heating Cycle | 2nd Heating Cycle | |||||
|---|---|---|---|---|---|---|
| Scaffold | Tm (°C) | ΔH (J/g) | Crystallinity (%) | Tm (°C) | ΔH (J/g) | Crystallinity (%) |
| PCL(0K)0BA | 63.70 | 84.5 | 59.5 | 55.80 | 60.3 | 42.5 |
| PCL(5K)50BA | 61.74 | 97.6 | 72.4 | 53.02 | 76.2 | 56.5 |
| PCL(10K)50BA | 61.29 | 96.1 | 75.2 | 52.76 | 70.4 | 55.1 |
| PCL(5K)75BA | 62.67 | 100.9 | 74.8 | 54.65 | 75.1 | 55.7 |
| PCL(10K)75BA | 61.74 | 91.4 | 71.5 | 54.72 | 79.7 | 62.3 |
References
- European Commission. Directorate-General for Economic and Financial Affairs. In The 2018 Ageing Report Economic & Budgetary Projections for the 28 EU Member States (2016–2070); European Commission: Brussels, Belgium, 2018. [Google Scholar]
- Office of the Surgeon General (US). Bone Health and Osteoporosis: A Report of the Surgeon General; Reports of the Surgeon General; Office of the Surgeon General (US): Rockville, MD, USA, 2004.
- García-González, C.A.; Concheiro, A.; Alvarez-Lorenzo, C. Processing of Materials for Regenerative Medicine Using Supercritical Fluid Technology. Bioconjug. Chem. 2015, 26, 1159–1171. [Google Scholar] [CrossRef] [PubMed]
- Sohn, H.-S.; Oh, J.-K. Review of bone graft and bone substitutes with an emphasis on fracture surgeries. Biomater. Res. 2019, 23, 9. [Google Scholar] [CrossRef] [PubMed]
- Jones, J.R. Scaffolds for tissue engineering. In Biomaterials, Artificial Organs and Tissue Engineering; Elsevier: Amsterdam, The Netherlands, 2005; pp. 201–214. ISBN 978-1-85573-737-2. [Google Scholar]
- Yin, S.; Zhang, W.; Zhang, Z.; Jiang, X. Recent Advances in Scaffold Design and Material for Vascularized Tissue-Engineered Bone Regeneration. Adv. Healthc. Mater. 2019, 8, 1801433. [Google Scholar] [CrossRef] [PubMed]
- Johnson, C.T.; García, A.J. Scaffold-based Anti-infection Strategies in Bone Repair. Ann. Biomed. Eng. 2015, 43, 515–528. [Google Scholar] [CrossRef] [PubMed]
- Aoki, K.; Saito, N. Biodegradable Polymers as Drug Delivery Systems for Bone Regeneration. Pharmaceutics 2020, 12, 95. [Google Scholar] [CrossRef]
- García-González, C.A.; Barros, J.; Rey-Rico, A.; Redondo, P.; Gómez-Amoza, J.L.; Concheiro, A.; Alvarez-Lorenzo, C.; Monteiro, F.J. Antimicrobial Properties and Osteogenicity of Vancomycin-Loaded Synthetic Scaffolds Obtained by Supercritical Foaming. ACS Appl. Mater. Interfaces 2018, 10, 3349–3360. [Google Scholar] [CrossRef]
- Goimil, L.; Santos-Rosales, V.; Delgado, A.; Évora, C.; Reyes, R.; Lozano-Pérez, A.A.; Aznar-Cervantes, S.D.; Cenis, J.L.; Gómez-Amoza, J.L.; Concheiro, A.; et al. scCO2-foamed silk fibroin aerogel/poly(ε-caprolactone) scaffolds containing dexamethasone for bone regeneration. J. CO2 Util. 2019, 31, 51–64. [Google Scholar] [CrossRef]
- Jiang, K.; Weaver, J.D.; Li, Y.; Chen, X.; Liang, J.; Stabler, C.L. Local release of dexamethasone from macroporous scaffolds accelerates islet transplant engraftment by promotion of anti-inflammatory M2 macrophages. Biomaterials 2017, 114, 71–81. [Google Scholar] [CrossRef]
- Santos-Rosales, V.; Iglesias-Mejuto, A.; García-González, C.A. Solvent-Free Approaches for the Processing of Scaffolds in Regenerative Medicine. Polymers 2020, 12, 533. [Google Scholar] [CrossRef]
- Di Maio, E.; Kiran, E. Foaming of polymers with supercritical fluids and perspectives on the current knowledge gaps and challenges. J. Supercrit. Fluids 2018, 134, 157–166. [Google Scholar] [CrossRef]
- Diaz-Gomez, L.; Concheiro, A.; Alvarez-Lorenzo, C.; García-González, C.A. Growth factors delivery from hybrid PCL-starch scaffolds processed using supercritical fluid technology. Carbohydr. Polym. 2016, 142, 282–292. [Google Scholar] [CrossRef] [PubMed]
- Liao, X.; Zhang, H.; He, T. Preparation of Porous Biodegradable Polymer and Its Nanocomposites by Supercritical CO2 Foaming for Tissue Engineering. J. Nanomater. 2012, 2012, 836394. [Google Scholar] [CrossRef]
- Chen, C.-X.; Liu, Q.-Q.; Xin, X.; Guan, Y.-X.; Yao, S.-J. Pore formation of poly(ε-caprolactone) scaffolds with melting point reduction in supercritical CO2 foaming. J. Supercrit. Fluids 2016, 117, 279–288. [Google Scholar] [CrossRef]
- Santos-Rosales, V.; Gallo, M.; Jaeger, P.; Alvarez-Lorenzo, C.; Gómez-Amoza, J.L.; García-González, C.A. New insights in the morphological characterization and modelling of poly(ε-caprolactone) bone scaffolds obtained by supercritical CO2 foaming. J. Supercrit. Fluids 2020, 166, 105012. [Google Scholar] [CrossRef]
- Chen, C.-X.; Peng, H.-H.; Guan, Y.-X.; Yao, S.-J. Morphological study on the pore growth profile of poly(ε-caprolactone) bi-modal porous foams using a modified supercritical CO2 foaming process. J. Supercrit. Fluids 2019, 143, 72–81. [Google Scholar] [CrossRef]
- Harris, L.D.; Kim, B.-S.; Mooney, D.J. Open pore biodegradable matrices formed with gas foaming. J. Biomed. Mater. Res. 1998, 42, 396–402. [Google Scholar] [CrossRef]
- Nam, Y.S.; Yoon, J.J.; Park, T.G. A novel fabrication method of macroporous biodegradable polymer scaffolds using gas foaming salt as a porogen additive. J. Biomed. Mater. Res. 2000, 53, 1–7. [Google Scholar] [CrossRef]
- Jing, X.; Mi, H.-Y.; Cordie, T.; Salick, M.; Peng, X.-F.; Turng, L.-S. Fabrication of Porous Poly(ε-caprolactone) Scaffolds Containing Chitosan Nanofibers by Combining Extrusion Foaming, Leaching, and Freeze-Drying Methods. Ind. Eng. Chem. Res. 2014, 53, 17909–17918. [Google Scholar] [CrossRef]
- Ribeiro Rodrigues, L.; de Sousa Laranjeira, M.; Fernandes, M.H.; Monteiro, F.J.; de Carvallho Zavaglia, C.A. HA/TCP scaffolds obtained by sucrose crystal leaching method: Preliminary in vitro Evaluation. Mater. Res. 2014, 17, 811–816. [Google Scholar] [CrossRef][Green Version]
- Wang, X.; Salick, M.R.; Gao, Y.; Jiang, J.; Li, X.; Liu, F.; Cordie, T.; Li, Q.; Turng, L.-S. Interconnected porous poly(ɛ-caprolactone) tissue engineering scaffolds fabricated by microcellular injection molding. J. Cell. Plast. 2018, 54, 379–397. [Google Scholar] [CrossRef]
- Zhang, K.; Wang, Y.; Jiang, J.; Wang, X.; Hou, J.; Sun, S.; Li, Q. Fabrication of highly interconnected porous poly(ɛ-caprolactone) scaffolds with supercritical CO2 foaming and polymer leaching. J. Mater. Sci. 2019, 54, 5112–5126. [Google Scholar] [CrossRef]
- Santos-Rosales, V.; Ardao, I.; Alvarez-Lorenzo, C.; Ribeiro, N.; Oliveira, A.; García-González, C. Sterile and Dual-Porous Aerogels Scaffolds Obtained through a Multistep Supercritical CO2-Based Approach. Molecules 2019, 24, 871. [Google Scholar] [CrossRef] [PubMed]
- Kwon, D.Y.; Park, J.Y.; Lee, B.Y.; Kim, M.S. Comparison of Scaffolds Fabricated via 3D Printing and Salt Leaching: In Vivo Imaging, Biodegradation, and Inflammation. Polymers 2020, 12, 2210. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Ye, J.; Liao, X.; Li, S.; Xiao, W.; Yang, Q.; Li, G. Organic solvent free preparation of porous scaffolds based on the phase morphology control using supercritical CO2. J. Supercrit. Fluids 2019, 149, 88–96. [Google Scholar] [CrossRef]
- Xin, X.; Liu, Q.-Q.; Chen, C.-X.; Guan, Y.-X.; Yao, S.-J. Fabrication of bimodal porous PLGA scaffolds by supercritical CO2 foaming/particle leaching technique. J. Appl. Polym. Sci. 2016, 133. [Google Scholar] [CrossRef]
- Deng, A.; Chen, A.; Wang, S.; Li, Y.; Liu, Y.; Cheng, X.; Zhao, Z.; Lin, D. Porous nanostructured poly-L-lactide scaffolds prepared by phase inversion using supercritical CO2 as a nonsolvent in the presence of ammonium bicarbonate particles. J. Supercrit. Fluids 2013, 77, 110–116. [Google Scholar] [CrossRef]
- Murphy, W.L.; Peters, M.C.; Kohn, D.H.; Mooney, D.J. Sustained release of vascular endothelial growth factor from mineralized poly(lactide-co-glycolide) scaffolds for tissue engineering. Biomaterials 2000, 21, 2521–2527. [Google Scholar] [CrossRef]
- Zhang, L.; Yang, D.; Chen, H.; Sun, R.; Xu, L.; Xiong, Z.; Govender, T.; Xiong, C. An ionically crosslinked hydrogel containing vancomycin coating on a porous scaffold for drug delivery and cell culture. Int. J. Pharm. 2008, 353, 74–87. [Google Scholar] [CrossRef]
- Song, H.-F.; Chen, A.-Z.; Wang, S.-B.; Kang, Y.-Q.; Ye, S.-F.; Liu, Y.-G.; Wu, W.-G. Preparation of Chitosan-Based Hemostatic Sponges by Supercritical Fluid Technology. Materials 2014, 7, 2459–2473. [Google Scholar] [CrossRef]
- Bigler, T.; Weidman-Evans, E.; Flowers, D. Relationship Between Nonsteroidal Anti-Inflammatory Drugs and Bone-Healing After Fracture or Orthopaedic Surgery. JBJS J. Orthop. Physician Assist. 2018, 6, e14. [Google Scholar] [CrossRef]
- Mazières, B. Topical Ketoprofen Patch. Drugs R&D 2005, 6, 337–344. [Google Scholar]
- Murphy, C.M.; Haugh, M.G.; O’Brien, F.J. The effect of mean pore size on cell attachment, proliferation and migration in collagen–glycosaminoglycan scaffolds for bone tissue engineering. Biomaterials 2010, 31, 461–466. [Google Scholar] [CrossRef] [PubMed]
- Gualandi, C.; White, L.J.; Chen, L.; Gross, R.A.; Shakesheff, K.M.; Howdle, S.M.; Scandola, M. Scaffold for tissue engineering fabricated by non-isothermal supercritical carbon dioxide foaming of a highly crystalline polyester. Acta Biomater. 2010, 6, 130–136. [Google Scholar] [CrossRef] [PubMed]
- White, L.J.; Hutter, V.; Tai, H.; Howdle, S.M.; Shakesheff, K.M. The effect of processing variables on morphological and mechanical properties of supercritical CO2 foamed scaffolds for tissue engineering. Acta Biomater. 2012, 8, 61–71. [Google Scholar] [CrossRef] [PubMed]
- Karimi, M.; Heuchel, M.; Weigel, T.; Schossig, M.; Hofmann, D.; Lendlein, A. Formation and size distribution of pores in poly(ɛ-caprolactone) foams prepared by pressure quenching using supercritical CO2. J. Supercrit. Fluids 2012, 61, 175–190. [Google Scholar] [CrossRef]
- Marcinkowski, Ł.; Kloskowski, A.; Spietelun, A.; Namieśnik, J. Evaluation of polycaprolactone as a new sorbent coating for determination of polar organic compounds in water samples using membrane–SPME. Anal. Bioanal. Chem. 2015, 407, 1205–1215. [Google Scholar] [CrossRef][Green Version]
- Li, Z.-H.; Wang, L.; Dai, H.-L.; Wang, X.-Y.; Li, J.-S.; Zhao, Z. Fabrication, characterization, and in vitro evaluation of biomimetic silk fibroin porous scaffolds via supercritical CO2 technology. J. Supercrit. Fluids 2019, 150, 86–93. [Google Scholar] [CrossRef]
- O’Brien, F.J.; Harley, B.A.; Yannas, I.V.; Gibson, L.J. The effect of pore size on cell adhesion in collagen-GAG scaffolds. Biomaterials 2005, 26, 433–441. [Google Scholar] [CrossRef]
- Goimil, L.; Braga, M.E.M.; Dias, A.M.A.; Gómez-Amoza, J.L.; Concheiro, A.; Alvarez-Lorenzo, C.; de Sousa, H.C.; García-González, C.A. Supercritical processing of starch aerogels and aerogel-loaded poly(ε-caprolactone) scaffolds for sustained release of ketoprofen for bone regeneration. J. CO2 Util. 2017, 18, 237–249. [Google Scholar] [CrossRef]
- Athanasiou, K.A.; Zhu, C.-F.; Lanctot, D.R.; Agrawal, C.M.; Wang, X. Fundamentals of Biomechanics in Tissue Engineering of Bone. Tissue Eng. 2000, 6, 361–381. [Google Scholar] [CrossRef]
- Rege, A.; Hillgärtner, M.; Itskov, M. Mechanics of biopolymer aerogels based on microstructures generated from 2-d Voronoi tessellations. J. Supercrit. Fluids 2019, 151, 24–29. [Google Scholar] [CrossRef]
- Santos-Rosales, V.; Alvarez-Rivera, G.; Hillgärtner, M.; Cifuentes, A.; Itskov, M.; García-González, C.A.; Rege, A. Stability Studies of Starch Aerogel Formulations for Biomedical Applications. Biomacromolecules 2020, 21, 5336–5344. [Google Scholar] [CrossRef] [PubMed]
- Gibson, L.J.; Ashby, M.F. Cellular Solids: Structure and Properties, 2nd ed.; Cambridge Solid State Science Series; Cambridge University Press: Cambridge, UK, 2001; ISBN 978-0-521-49911-8. [Google Scholar]
- Raafat, A.I.; Abd-Allah, W.M. In vitro apatite forming ability and ketoprofen release of radiation synthesized (gelatin-polyvinyl alcohol)/bioglass composite scaffolds for bone tissue regeneration. Polym. Compos. 2018, 39, 606–615. [Google Scholar] [CrossRef]
- Tezcaner, A.; Keskin, D. Bioactive Agent Delivery in Bone Tissue Regeneration. In Active Implants and Scaffolds for Tissue Regeneration; Zilberman, M., Ed.; Studies in Mechanobiology, Tissue Engineering and Biomaterials; Springer: Berlin/Heidelberg, Germany, 2010; Volume 8, pp. 193–223. ISBN 978-3-642-18064-4. [Google Scholar]
- Peppas, N.A. Analysis of Fickian and non-Fickian drug release from polymers. Pharm. Acta Helv. 1985, 60, 110–111. [Google Scholar] [PubMed]
- Lam, C.X.F.; Hutmacher, D.W.; Schantz, J.-T.; Woodruff, M.A.; Teoh, S.H. Evaluation of polycaprolactone scaffold degradation for 6 months in vitro and in vivo. J. Biomed. Mater. Res. Part A 2009, 90A, 906–919. [Google Scholar] [CrossRef]
- Diaz-Gomez, L.; Yang, F.; Jansen, J.A.; Concheiro, A.; Alvarez-Lorenzo, C.; García-González, C.A. Low viscosity-PLGA scaffolds by compressed CO 2 foaming for growth factor delivery. RSC Adv. 2016, 6, 70510–70519. [Google Scholar] [CrossRef]
- Diaz-Gomez, L.; García-González, C.A.; Wang, J.; Yang, F.; Aznar-Cervantes, S.; Cenis, J.L.; Reyes, R.; Delgado, A.; Évora, C.; Concheiro, A.; et al. Biodegradable PCL/fibroin/hydroxyapatite porous scaffolds prepared by supercritical foaming for bone regeneration. Int. J. Pharm. 2017, 527, 115–125. [Google Scholar] [CrossRef]
- Schneider, M. The importance of ammonia in mammalian cell culture. J. Biotechnol. 1996, 46, 161–185. [Google Scholar] [CrossRef]
- Mukae, K.; Bae, Y.H.; Okano, T.; Kim, S.W. A Thermo-Sensitive Hydrogel: Poly(ethylene oxide-dimethyl siloxane-ethylene oxide)/Poly(N-isopropyl acrylamide) Interpenetrating Polymer Networks II. On-Off Regulation of Solute Release from Thermo-Sensitive Hydrogel. Polym. J. 1990, 22, 250–265. [Google Scholar] [CrossRef]



| Initial Formulation Composition | Textural Properties | |||||
|---|---|---|---|---|---|---|
| Scaffold | PCL (wt.%) | K (wt.%) | BA (wt.%) | ρbulk (g/cm3) | ρskel (g/cm3) | ε (%) |
| PCL(0K)0BA | 100 | - | - | 0.41 ± 0.01 | 1.126 ± 0.015 | 63.6 ± 1.0 |
| PCL(5K)0BA | 95.0 | 5.0 | - | 0.51 ± 0.08 | 1.098 ± 0.004 | 53.6 ± 7.3 |
| PCL(0K)50BA | 50.0 | - | 50.0 | 0.24 ± 0.01 | 1.110 ± 0.011 | 78.4 ± 0.5 |
| PCL(5K)50BA | 47.4 | 2.6 | 50.0 | 0.29 ± 0.04 | 1.032 ± 0.006 | 71.9 ± 3.4 |
| PCL(10K)50BA | 47.4 | 5.3 | 50.0 | 0.28 ± 0.07 | 1.023 ± 0.009 | 72.6 ± 4.4 |
| PCL(0K)75BA | 25.0 | - | 75.0 | 0.20 ± 0.01 | 1.086 ± 0.006 | 81.6 ± 0.6 |
| PCL(5K)75BA | 23.7 | 1.3 | 75.0 | 0.18 ± 0.05 | 1.047 ± 0.005 | 82.8 ± 3.6 |
| PCL(10K)75BA | 22.4 | 2.6 | 75.0 | 0.18 ± 0.07 | 1.034 ± 0.007 | 82.6 ± 4.1 |
| Scaffold | k (hn) | tlag (h) | n | R2 |
|---|---|---|---|---|
| PCL(5K)0BA | 0.196 ± 0.012 | 0.454 ± 0.057 | 0.404 ± 0.019 | 0.978 |
| PCL(5K)50BA | 0.310 ± 0.020 | 0.499 ± 0.002 | 0.231 ± 0.017 | 0.930 |
| PCL(10K)50BA | 0.380 ± 0.022 | 0.499 ± 0.002 | 0.188 ± 0.015 | 0.914 |
| PCL(5K)75BA | 0.322 ± 0.026 | 0.500 ± 0.002 | 0.222 ± 0.021 | 0.886 |
| PCL(10K)75BA | 0.424 ± 0.021 | 0.500 ± 0.001 | 0.165 ± 0.013 | 0.921 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Santos-Rosales, V.; Ardao, I.; Goimil, L.; Gomez-Amoza, J.L.; García-González, C.A. Solvent-Free Processing of Drug-Loaded Poly(ε-Caprolactone) Scaffolds with Tunable Macroporosity by Combination of Supercritical Foaming and Thermal Porogen Leaching. Polymers 2021, 13, 159. https://doi.org/10.3390/polym13010159
Santos-Rosales V, Ardao I, Goimil L, Gomez-Amoza JL, García-González CA. Solvent-Free Processing of Drug-Loaded Poly(ε-Caprolactone) Scaffolds with Tunable Macroporosity by Combination of Supercritical Foaming and Thermal Porogen Leaching. Polymers. 2021; 13(1):159. https://doi.org/10.3390/polym13010159
Chicago/Turabian StyleSantos-Rosales, Víctor, Inés Ardao, Leticia Goimil, Jose Luis Gomez-Amoza, and Carlos A. García-González. 2021. "Solvent-Free Processing of Drug-Loaded Poly(ε-Caprolactone) Scaffolds with Tunable Macroporosity by Combination of Supercritical Foaming and Thermal Porogen Leaching" Polymers 13, no. 1: 159. https://doi.org/10.3390/polym13010159
APA StyleSantos-Rosales, V., Ardao, I., Goimil, L., Gomez-Amoza, J. L., & García-González, C. A. (2021). Solvent-Free Processing of Drug-Loaded Poly(ε-Caprolactone) Scaffolds with Tunable Macroporosity by Combination of Supercritical Foaming and Thermal Porogen Leaching. Polymers, 13(1), 159. https://doi.org/10.3390/polym13010159






