Fear of the Relapse: Effect of Composite Type on Adhesion Efficacy of Upper and Lower Orthodontic Fixed Retainers: In Vitro Investigation and Randomized Clinical Trial
Abstract
1. Introduction
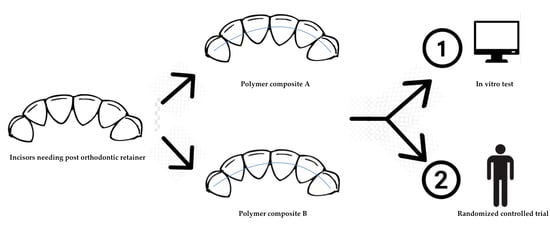
2. Materials and Methods
2.1. In Vitro Study
2.1.1. Specimen Preparation
2.1.2. Shear Bond Strength (SBS) Test
2.1.3. Adhesive Remnant Index (ARI) Score
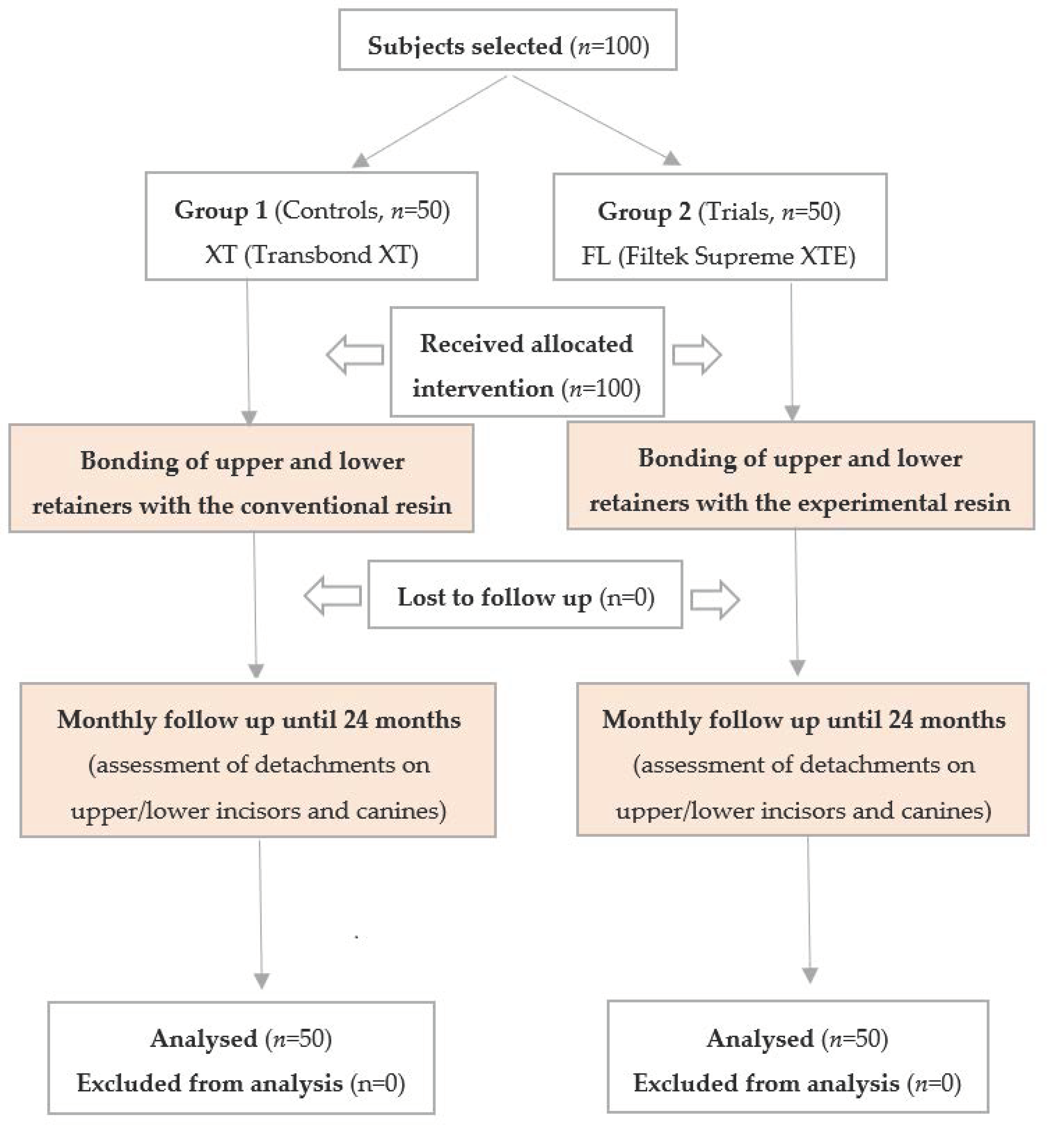
2.2. Randomized Clinical Trial (RCT)
2.2.1. Trial Design
2.2.2. Participants
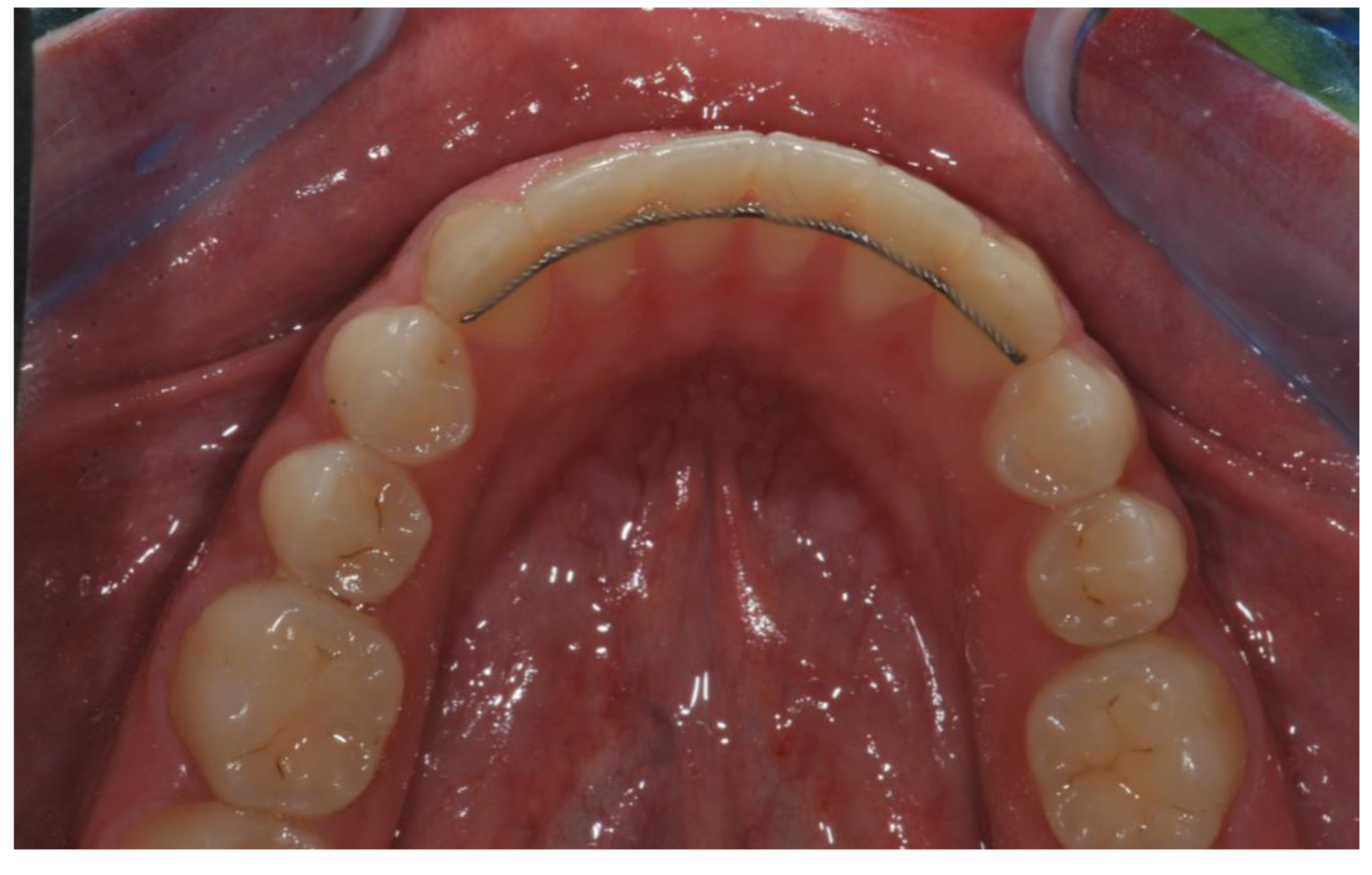
2.2.3. Interventions
2.2.4. Outcomes
2.2.5. Sample Size
2.2.6. Randomization and Blinding
2.3. Statistical Methods
3. Results
3.1. In Vitro Study
3.1.1. Shear Bond Strength (SBS) Test
3.1.2. Adhesive Remnant Index (ARI) Score
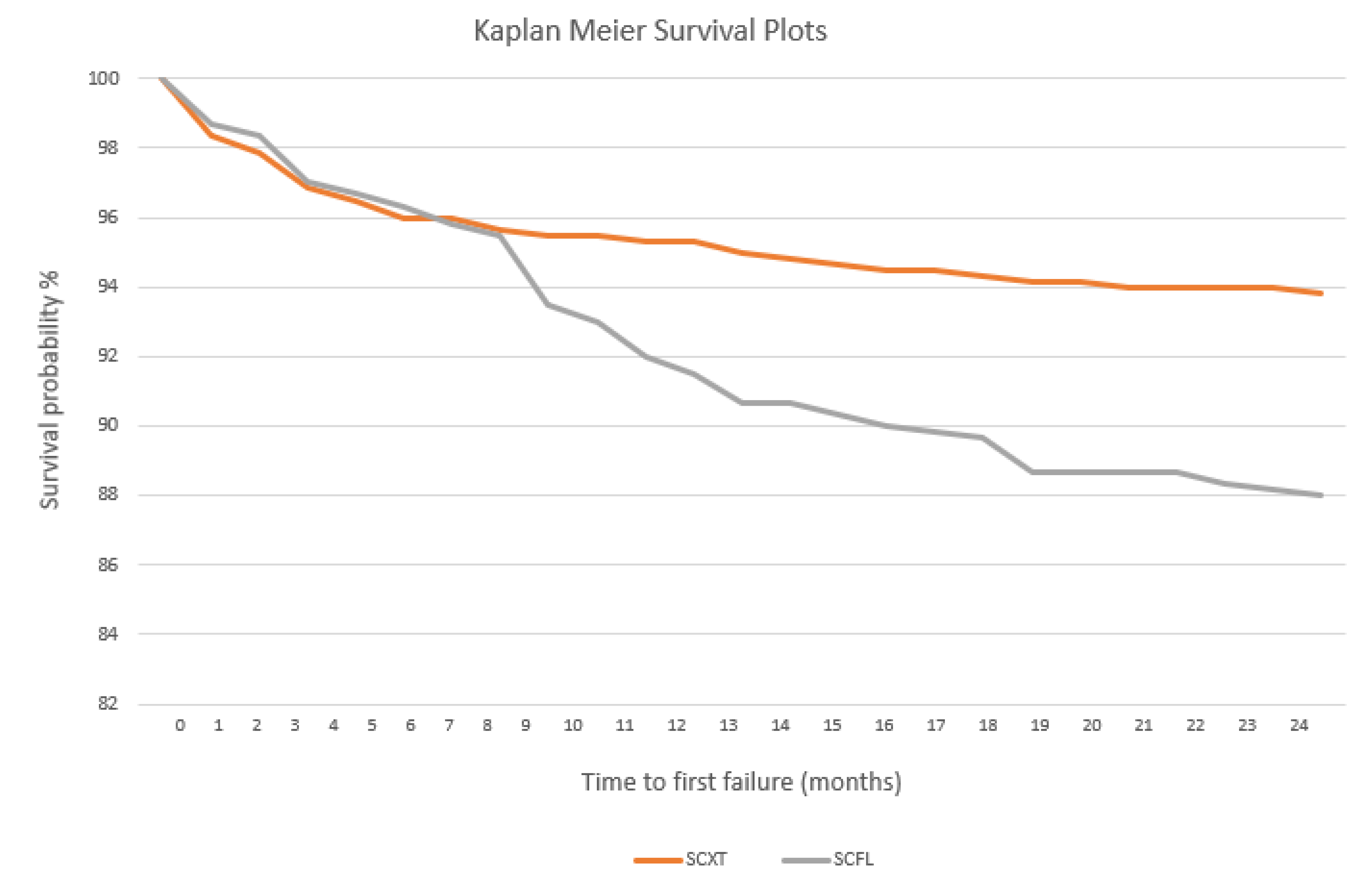
3.2. Randomized Clinical Trial (RCT)
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Littlewood, S.J.; Millett, D.T.; Doubleday, B.; Bearn, D.R.; Worthington, H.V. Retention procedures for stabilising tooth position after treatment with orthodontic braces. Cochrane Database Syst. Rev. 2016, 1, CD002283. [Google Scholar] [CrossRef]
- Gugger, J.; Pandis, N.; Zinelis, S.; Patcas, R.; Eliades, G.; Eliades, T. Retrieval analysis of lingual fixed retainer adhesives. Am. J. Orthod. Dentofac. Orthop. 2016, 150, 575–584. [Google Scholar] [CrossRef]
- Lai, C.S.; Grossen, J.M.; Renkema, A.M.; Bronkhorst, E.; Fudalej, P.S.; Katsaros, C. Orthodontic retention procedures in Switzerland. Swiss Dent. J. 2014, 124, 655–661. [Google Scholar] [PubMed]
- Renkema, A.M.; Sips, E.T.; Bronkhorst, E.; Kuijpers-Jagtman, A.M. A survey on orthodontic retention procedures in the Netherlands. Eur. J. Orthod. 2009, 31, 423–437. [Google Scholar] [CrossRef] [PubMed]
- Singh, P.; Grammati, S.; Kirschen, R. Orthodontic retention patterns in the United Kingdom. J. Orthod. 2009, 36, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Vandevska-Radunovic, V.; Espeland, L.; Stenvik, A. Retention: Type, duration and need for common guidelines. A survey of Norwegian orthodontists. Orthodontics 2013, 14, e110–e117. [Google Scholar] [CrossRef] [PubMed]
- Valiathan, M.; Hughes, E. Results of a survey-based study to identify common retention practices in the United States. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 170–177. [Google Scholar] [CrossRef]
- Wong, P.M.; Freer, T.J. A comprehensive survey of retention procedures in Australia and New Zealand. Aust. Orthod. J. 2004, 20, 99–106. [Google Scholar]
- Scribante, A.; Gandini, P.; Tessera, P.; Vallittu, P.K.; Lassila, L.; Sfondrini, M.F. Spot-Bonding and Full-Bonding Techniques for Fiber Reinforced Composite (FRC) and Metallic Retainers. Int. J. Mol. Sci. 2017, 18, 2096. [Google Scholar] [CrossRef]
- Batra, C.; Nagpal, R.; Tyagi, S.P.; Singh, U.P.; Manuja, N. In Vitro bonding effectiveness of three different one-step self-etch adhesives with additional enamel etching. J. Investig. Clin. Dent. 2014, 5, 226–236. [Google Scholar] [CrossRef]
- Beltrami, R.; Chiesa, M.; Scribante, A.; Allegretti, J.; Poggio, C. Comparison of shear bond strength of universal adhesives on etched and nonetched enamel. J. Appl. Biomater. Funct. Mater. 2016, 14, 78–83. [Google Scholar] [CrossRef] [PubMed]
- De Goes, M.F.; Shinohara, M.S.; Freitasc, M.S. Performance of a New One-step Multi-mode Adhesive on Etched vs Non-etched Enamel on Bond Strength and Interfacial Morphology. J. Adhes. Dent. 2014, 16, 243–250. [Google Scholar] [PubMed]
- Erickson, R.L.; Barkmeier, W.W.; Latta, M.A. The role of etching in bonding to enamel: A comparison of self-etching and etch-and-rinse adhesive systems. Dent. Mater. 2009, 25, 1459–1467. [Google Scholar] [CrossRef]
- Khosravi, K.; Ataei, E.; Mousavi, M.; Khodaeian, N. Enamel Margins on the Microleakage of a Simplified All-in-One and a Self-etch Adhesive System. Oper. Dent. 2009, 34, 531–536. [Google Scholar] [CrossRef]
- Lührs, A.K.; Guhr, S.; Schilke, R.; Borchers, L.; Geurtsen, W.; Günay, H. Shear Bond Strength of Self-etch Adhesives to Enamel with Additional Phosphoric Acid Etching. Oper. Dent. 2008, 33, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Manuja, N.; Nagpal, R.; Pandit, I.K. Dental Adhesion: Mechanism, Techniques and Durability. J. Clin. Pediatr. Dent. 2012, 36, 223–234. [Google Scholar] [CrossRef] [PubMed]
- Miguez, P.A.; Castrob, P.S.; Nunesb, M.F.; Waltera, R.; Pereirac, P.N.R. Effect of Acid etching on the Enamel Bond of Two Self-etching Systems. Adhes. Dent. 2003, 5, 107–112. [Google Scholar]
- Suzuki, T.; Takamizawa, T.; Barkmeier, W.W.; Tsujimoto, A.; Endo, H.; Erickson, R.L.; Latta, M.A.; Miyazaki, M. Influence of Etching Mode on Enamel Bond Durability of Universal Adhesive Systems. Oper. Dent. 2016, 41, 520–530. [Google Scholar] [CrossRef]
- Van Landuyt, K.L.; Kanumilli, P.; De Munck, J.; Peumans, M.; Lambrechts, P.; Van Meerbeek, B. Bond strength of a mild self-etch adhesive with and without prior acid-etching. J. Dent. 2006, 34, 77–85. [Google Scholar] [CrossRef]
- Van Meerbeek, B.; Kanumilli, P.; De Munck, J.; Van Landuyt, K.; Lambrechts, P.; Peumans, M. A randomized controlled study evaluating the effectiveness of a two-step self-etch adhesive with and without selective phosphoric-acid etching of enamel. Dent. Mater. 2005, 21, 375–383. [Google Scholar] [CrossRef]
- Cooke, M.E.; Sherriff, M. Debonding force and deformation of two multi-stranded lingual retainer wires bonded to incisor enamel: An in Vitro study. Eur. J. Orthod. 2010, 32, 741–746. [Google Scholar] [CrossRef] [PubMed]
- Milheiro, A.; de Jager, N.; Feilzer, A.J.; Kleverlaan, C.J. In Vitro debonding of orthodontic retainers analyzed with finite element analysis. Eur. J. Orthod. 2015, 37, 491–496. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Oesterle, L.J.; Shellhart, C.; Henderson, S. Enhancing wire-composite bond strength of bonded retainers with wire surface treatment. Am. J. Orthod. Dentofac. Orthop. 2001, 119, 625–631. [Google Scholar] [CrossRef] [PubMed]
- Scribante, A.; Dermenaki Farahani, M.R.; Marino, G.; Matera, C.; Rodriguez Y Baena, R.; Lanteri, V.; Butera, A. Biomimetic Effect of Nano-Hydroxyapatite in Demineralized Enamel before Orthodontic Bonding of Brackets and Attachments: Visual, Adhesion Strength, and Hardness in In Vitro Tests. Biomed. Res. Int. 2020, 2020, 6747498. [Google Scholar] [CrossRef]
- Scribante, A.; Sfondrini, M.F.; Fraticelli, D.; Daina, P.; Tamagnone, A.; Gandini, P. The influence of no-primer adhesives and anchor pylons bracket bases on shear bond strength of orthodontic brackets. Biomed. Res. Int. 2013, 2013, 315023. [Google Scholar] [CrossRef]
- Colombo, M.; Gallo, S.; Padovan, S.; Chiesa, M.; Poggio, C.; Scribante, A. Influence of Different Surface Pretreatments on Shear Bond Strength of an Adhesive Resin Cement to Various Zirconia Ceramics. Materials (Basel) 2020, 13, 652. [Google Scholar] [CrossRef] [PubMed]
- Poggio, C.; Scribante, A.; Della Zoppa, F.; Colombo, M.; Beltrami, R.; Chiesa, M. Shear bond strength of one-step self-etch adhesives to enamel: Effect of acid pretreatment. Dent. Traumatol. 2014, 30, 43–48. [Google Scholar] [CrossRef] [PubMed]
- Artun, J.; Bergland, S. Clinical trials with crystal growth conditioning as an alternative to acid-etch enamel pretreatment. Am. J. Orthod. 1984, 85, 333–340. [Google Scholar] [CrossRef]
- Scribante, A.; Cacciafesta, V.; Sfondrini, M.F. Effect of various adhesive systems on the shear bond strength of fiber-reinforced composite. Am. J. Orthod. Dentofac. Orthop. 2006, 130, 224–227. [Google Scholar] [CrossRef]
- R Development Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2008. [Google Scholar]
- Sfondrini, M.F.; Fraticelli, D.; Castellazzi, L.; Scribante, A.; Gandini, P. Clinical evaluation of bond failures and survival between mandibular canine-to-canine retainers made of flexible spiral wire and fiber-reinforced composite. J. Clin. Exp. Dent. 2014, 6, e145–e149. [Google Scholar] [CrossRef]
- Dahl, E.H.; Zachrisson, B.U. Long-term experience with direct-bonded lingual retainers. J. Clin. Orthod. 1991, 25, 619–630. [Google Scholar] [PubMed]
- Stormann, I.; Ehmer, U. A prospective randomized study of different retainer types. J. Orofac. Orthop. 2002, 63, 42–50. [Google Scholar] [CrossRef]
- Scribante, A.; Vallittu, P.K.; Özcan, M. Fiber-Reinforced Composites for Dental Applications. Biomed. Res. Int 2018, 2018, 4734986. [Google Scholar] [CrossRef]
- Freilich, M.A.; Karmaker, A.C.; Burstone, C.J.; Goldberg, A.J. Development and clinical applications of a light-polymerized fiber-reinforced composite. J. Prosthet. Dent. 1998, 80, 311–318. [Google Scholar] [CrossRef]
- Vallittu, P.K.; Lassila, V.P. Reinforcement of acrylic resin denture base material with metal or fibre strengtheners. J. Oral Rehabil. 1992, 19, 225–230. [Google Scholar] [CrossRef] [PubMed]
- Sfondrini, M.F.; Vallittu, P.K.; Lassila, L.V.J.; Viola, A.; Gandini, P.; Scribante, A. Glass Fiber Reinforced Composite Orthodontic Retainer: In Vitro Effect of Tooth Brushing on the Surface Wear and Mechanical Properties. Materials (Basel) 2020, 13, 1028. [Google Scholar] [CrossRef]
- Tacken, M.P.E.; Cosyn, J.; De Wilde, P.; Aerts, J.; Govaerts, E.; Vannet, B.V. Glass fiber reinforced versus multistranded bonded orthodontic retainers: A 2 year prospective multi-centre study. Eur. J. Orthod. 2010, 32, 117–123. [Google Scholar] [CrossRef]
- Karaman, A.I.; Polat, Ö.; Büyükyilmaz, T. A practical method of fabricating a lingual retainer. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 327–330. [Google Scholar] [CrossRef]
- Aldrees, A.M.; Al-Mutairi, T.K.; Hakami, Z.W.; Al-Malki, M.M. Bonded orthodontic retainers: A comparison of initial bond strength of different wire-and-composite combinations. J. Orofac. Orthop. 2010, 71, 290–299. [Google Scholar] [CrossRef]
- Reicheneder, C.; Hofrichter, B.; Faltermeier, A.; Proff, P.; Lippold, C.; Kirschneck, C. Shear bond strength of different retainer wires and bonding adhesives in consideration of the pretreatment process. Head Face Med. 2014, 10, 51. [Google Scholar] [CrossRef]
- Radlanski, R.J.; Zain, N.D. Stability of the Bonded Lingual Wire Retainer—A Study of the Initial Bond Strength. J. Orofac. Orthop. 2004, 65, 321. [Google Scholar] [CrossRef] [PubMed]
- Tabrizi, S.; Salemis, E.; Usumez, S. Flowable Composites for Bonding Orthodontic Retainers. Angle Orthod. 2010, 80, 195–200. [Google Scholar] [CrossRef] [PubMed]
- Scribante, A.; Contreras-Bulnes, R.; Montasser, M.A.; Vallittu, P.K. Orthodontics: Bracket Materials, Adhesives Systems, and Their Bond Strength. Biomed. Res. Int. 2016, 2016, 1329814. [Google Scholar] [CrossRef] [PubMed]
- Soares, F.M.Z.; Follak, A.; da Rosa, L.S.; Montagner, A.S.; Lenzi, T.L.; Rocha, R.O. Bovine tooth is a substitute for human tooth on bond strength studies: A systematic review and meta-analysis of in vitro studies. Dent. Mater. 2016, 32, 1385–1393. [Google Scholar] [CrossRef]
- Salehi, P.; Zarif Najafi, H.; Roeinpeikar, S.M. Comparison of survival time between two types of orthodontic fixed retainer: A prospective randomized clinical trial. Prog. Orthod. 2013, 14, 25. [Google Scholar] [CrossRef]
- Kocher, K.E.; Gebistorf, M.C.; Pandis, N.; Fudalej, P.S.; Katsaros, C. Survival of maxillary and mandibular bonded retainers 10 to 15 years after orthodontic treatment: A retrospective observational study. Prog. Orthod. 2019, 20, 28. [Google Scholar] [CrossRef]
- Scribante, A.; Sfondrini, M.F.; Broggini, S.; D’Allocco, M.; Gandini, P. Efficacy of Esthetic Retainers: Clinical Comparison between Multistranded Wires and Direct-Bond Glass Fiber-Reinforced Composite Splints. Int. J. Dent. 2011, 2011, 548356. [Google Scholar] [CrossRef]
- Drummond, J.L. Degradation, fatigue, and failure of resin dental composite materials. J. Dent. Res. 2008, 87, 710–719. [Google Scholar] [CrossRef]


| Material | Type | Composition | pH | Application Protocol |
|---|---|---|---|---|
| Scotchbond Universal | Universal adhesive | 10-MDP, HEMA, silane, dimethacrylate resins, VitrebondTM copolymer, filler, ethanol, water, initiators, catalysts | 2.7 | According to the total-etch modality: 1. Tooth isolation 2. Etching 3. Rinsing and air-drying 4. Adhesive application 5. Air-drying 6. Light curing for 20” |
| Transbond XT | Orthodontic light curing composite resin | Silane treated quartz (70%-80%), Bis-GMA (10%-20%), Bisphenol A Bis(2-hydroxyethyl ether) dimethacrylate (5%-10%), Silane treated silica (<2%), DPIHFP (<0.2%) | - | 1. Apply around lingual retainer 2. Light curing for 20” |
| Filtek Supreme XTE | Flowable light curing nanocomposite | bis-GMA, UDMA, TEGDMA, bis-EMA(6) | - | 1. Apply around lingual retainer 2. Light curing for 20” |
| Group | Resin | Mean | SD | Minimum | Median | Maximum | Significance |
|---|---|---|---|---|---|---|---|
| 1 (XT) | Conventional | 13.31 | 2.87 | 8.95 | 12.85 | 21.64 | |
| 2 (FL) | Flowable | 8.28 | 1.45 | 5.54 | 8.22 | 11.80 | P < 0.05 |
| Score | Group 1 (XT) | Group 2 (FL) |
|---|---|---|
| ARI = 0 | 0 | 0 |
| ARI = 1 | 35 | 45 |
| ARI = 2 | 60 | 45 |
| ARI = 3 | 5 | 10 |
| Group | Composite | Splint Zone | Teeth Bonded | Failures | Percentage (%) | Significance |
|---|---|---|---|---|---|---|
| Group 1 | Conventional | Overall | 600 | 37 | 6.17 | |
| Group 2 | Flowable | Overall | 600 | 72 | 12.00 | P < 0.05 |
| Group 1 | Conventional | Upper | 300 | 16 | 5.33 | |
| Group 2 | Flowable | Upper | 300 | 32 | 10.67 | P < 0.05 |
| Group 1 | Conventional | Lower | 300 | 21 | 7.00 | |
| Group 2 | Flowable | Lower | 300 | 40 | 13.33 | P < 0.05 |
| Group | Composite | Splint Zone | Tooth | Teeth Bonded | Failures | Percentage (%) | Significance |
|---|---|---|---|---|---|---|---|
| Group 1 | Conventional | Upper | Canines | 100 | 2 | 2.00 | |
| Group 1 | Conventional | Upper | Incisors | 200 | 14 | 7.00 | ns |
| Group 1 | Conventional | Lower | Canines | 100 | 4 | 4.00 | |
| Group 1 | Conventional | Lower | Incisors | 200 | 17 | 8.50 | ns |
| Group 2 | Flowable | Upper | Canines | 100 | 7 | 7.00 | |
| Group 2 | Flowable | Upper | Incisors | 200 | 25 | 12.50 | ns |
| Group 2 | Flowable | Lower | Canines | 100 | 9 | 9.00 | |
| Group 2 | Flowable | Lower | Incisors | 200 | 31 | 15.50 | ns |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scribante, A.; Gallo, S.; Turcato, B.; Trovati, F.; Gandini, P.; Sfondrini, M.F. Fear of the Relapse: Effect of Composite Type on Adhesion Efficacy of Upper and Lower Orthodontic Fixed Retainers: In Vitro Investigation and Randomized Clinical Trial. Polymers 2020, 12, 963. https://doi.org/10.3390/polym12040963
Scribante A, Gallo S, Turcato B, Trovati F, Gandini P, Sfondrini MF. Fear of the Relapse: Effect of Composite Type on Adhesion Efficacy of Upper and Lower Orthodontic Fixed Retainers: In Vitro Investigation and Randomized Clinical Trial. Polymers. 2020; 12(4):963. https://doi.org/10.3390/polym12040963
Chicago/Turabian StyleScribante, Andrea, Simone Gallo, Benedetta Turcato, Federico Trovati, Paola Gandini, and Maria Francesca Sfondrini. 2020. "Fear of the Relapse: Effect of Composite Type on Adhesion Efficacy of Upper and Lower Orthodontic Fixed Retainers: In Vitro Investigation and Randomized Clinical Trial" Polymers 12, no. 4: 963. https://doi.org/10.3390/polym12040963
APA StyleScribante, A., Gallo, S., Turcato, B., Trovati, F., Gandini, P., & Sfondrini, M. F. (2020). Fear of the Relapse: Effect of Composite Type on Adhesion Efficacy of Upper and Lower Orthodontic Fixed Retainers: In Vitro Investigation and Randomized Clinical Trial. Polymers, 12(4), 963. https://doi.org/10.3390/polym12040963