Prevention of Encrustation on Ureteral Stents: Which Surface Parameters Provide Guidance for the Development of Novel Stent Materials?
Abstract
1. Introduction
2. Materials and Methods
2.1. Polymer Materials
2.2. Surface Characteristics
2.2.1. Contact Angle
2.2.2. Surface Charge
2.3. Encrustation
2.3.1. Scanning Electron Microscopy
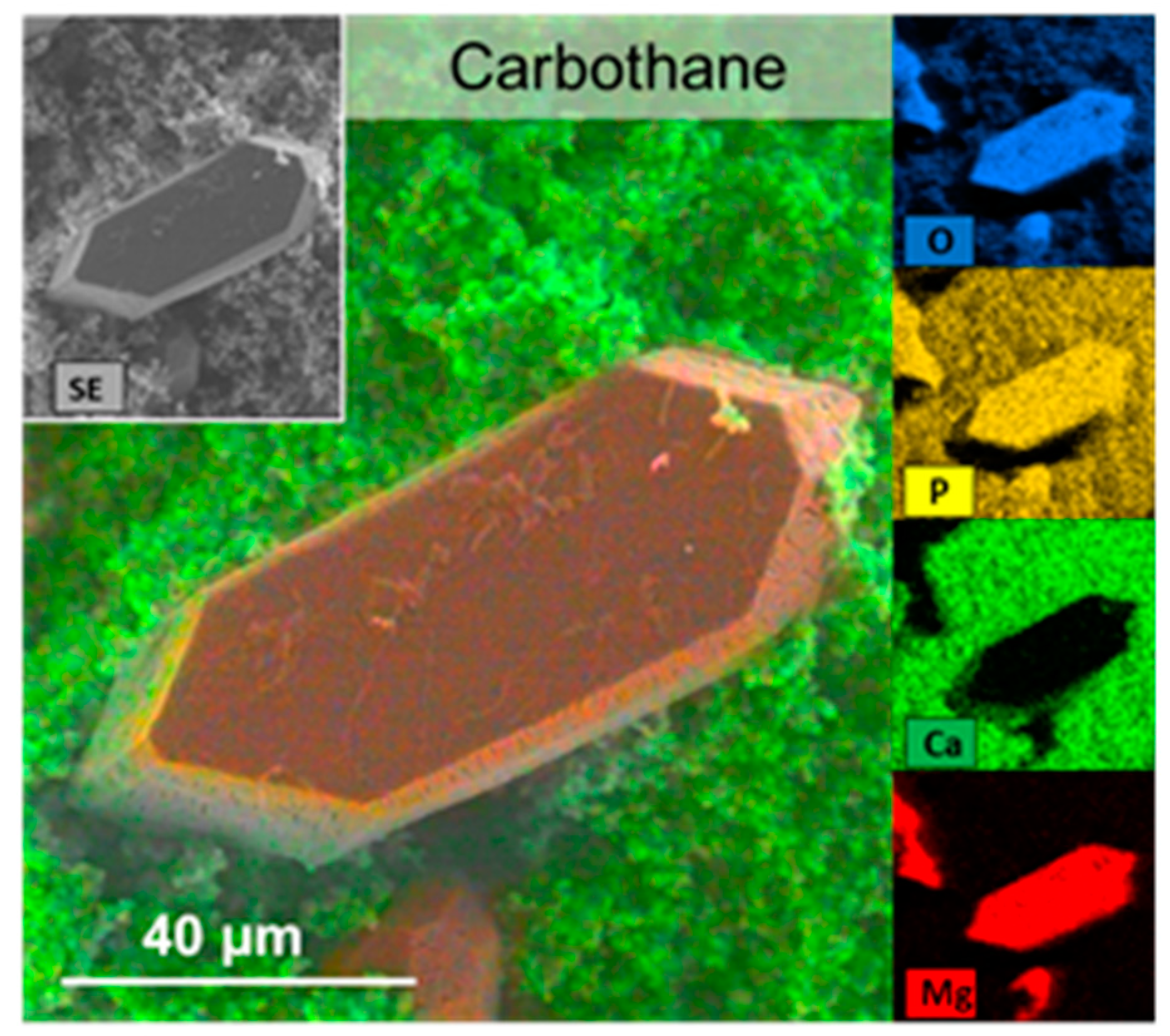
2.3.2. Energy Dispersive X-ray Spectroscopy
2.3.3. Fourier Transform Infrared Spectroscopy
2.4. Cell Culture
2.4.1. Cells
2.4.2. Biocompatibility Assay
2.5. Statistics
3. Results and Discussion
3.1. Use of Synthetic Urine to Ensure Reproducibility in Comparative Studies
3.2. Surface Characteristics can be Correlated to Encrustation Mass
- Group 1: hydrophobic (above 90°) and slightly negatively charged (Carbothane, Pelletane, Tecoflex, Tecophilic, Tecothane)
- Group 2: moderately hydrophilic (around 85°) and a strong negative surface charge (Elastollan, Styroflex, and Greenflex).
3.3. Characterization of Encrustations: Deposits Resemble In Vivo Infection Situation
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Data Availability
References
- Stickler, D.J. Clinical complications of urinary catheters caused by crystalline biofilms: Something needs to be done. J. Int. Med. 2014, 276, 120–129. [Google Scholar] [CrossRef] [PubMed]
- Burke, J.P.; Zavasky, D.M. Nosocomial urinary tract infection. In Hospital Epidemiology and Infection Control; Glen Mayhall, C., Ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 1999; pp. 173–185. [Google Scholar]
- Foxman, B. Epidemiology of urinary tract infections: Incidence, morbidity, and economic costs. Am. J. Med. 2002, 113, 5–13. [Google Scholar] [CrossRef]
- Li, J.K.M.; Teoh, J.Y.C.; Ng, C.F. Updates in endourological management of urolithiasis. Int. J. Urol. 2019, 26, 172–183. [Google Scholar] [CrossRef]
- Kram, W.; Buchholz, N.; Hakenberg, O.W. Ureteral stent encrustation. Pathophysiology. Arch. Esp. Urol. 2016, 69, 485–493. [Google Scholar] [PubMed]
- Knoll, T.; Schubert, A.B.; Fahlenkamp, D.; Leusmann, D.B.; Wendt-Nordahl, G.; Schubert, G. Urolithiasis through the ages: Data on more than 200,000 urinary stone analyses. J. Urol. 2011, 185, 1304–1311. [Google Scholar] [CrossRef]
- Grases, F.; Söhnel, O.; Costa-Bauza, A.; Ramis, M.; Wang, Z. Study on concretions developed around urinary catheters and mechanisms of renal calculi development. Nephron 2001, 88, 320–328. [Google Scholar] [CrossRef] [PubMed]
- Griffith, D.P.; Musher, D.M.; Itin, C. Urease. The primary cause of infection-induced urinary stones. Invest. Urol 1976, 13, 346–350. [Google Scholar]
- Bichler, K.H.; Eipper, E.; Naber, K.; Braun, V.; Zimmermann, R.; Lahme, S. Urinary infection stones. Int. J. Antimicrob. Agents 2002, 19, 488–498. [Google Scholar] [CrossRef]
- Kleinen, L.; Syring, I.; Laube, N. Reduction of biofilm formation on a-C:H coated implants: Investigation of biofilm-surface interactions by variation of thin film properties. Plasma Process. Polym. 2009, 6, 41–45. [Google Scholar] [CrossRef]
- Laube, N.; Desai, C.; Bernsmann, F. Hydrophobic forces as a key factor in crystalline biofilm formation on ureteral stents. Biomed. Eng. Biomed. Tech. 2016, 61, 483–490. [Google Scholar] [CrossRef]
- Mulhall, A.B.; Chapman, R.G.; Crow, R.A. Bacteriuria during indwelling urethral catheterization. J. Hosp. Infect. 1988, 11, 253–262. [Google Scholar] [CrossRef]
- Jahn, P.; Preuss, M.; Kernig, A.; Langer, G.; Seifert-Huehmer, A. Types of indwelling urinary catheters for long-term bladder drainage in adults. Cochrane Database Syst. Rev. 2007, 18, CD004997. [Google Scholar]
- Cortese, Y.J.; Wagner, V.E.; Tierney, M.; Devine, D.; Fogarty, A. Review of catheter-associated urinary tract infections and in vitro urinary tract models. J. Healthc. Eng. 2018, 2018, 2986742. [Google Scholar] [CrossRef] [PubMed]
- Laube, N.; Kleinen, L.; Avrutin, V.; Böde, U.; Meißner, A.; Fisang, C. The distribution of crystalline material in obstructed stents-In need for intra-luminal surface modification? J. Biomed. Mater. Res. Part B Appl. Biomater. 2008, 87, 590–597. [Google Scholar] [CrossRef]
- Choong, S.K.S.; Wood, S.; Whitfield, H.N. A model to quantify encrustation on ureteric stents, urethral catheters and polymers intended for urological use. BJU Int. 2000, 86, 414–421. [Google Scholar] [CrossRef]
- Atmani, F.; Khan, S.R. Quantification of proteins extracted from calcium oxalate and calcium phosphate crystals induced in vitro in the urine of healthy controls and stone-forming patients. Urol. Int. 2002, 68, 54–59. [Google Scholar] [CrossRef]
- Gomes, D.J.C.; de Souza, N.C.; Silva, J.R. Using a monocular optical microscope to assemble a wetting contact angle analyser. Measurement 2013, 46, 3623–3627. [Google Scholar] [CrossRef]
- Prywer, J.; Sadowski, R.R.; Torzewska, A. Aggregation of struvite, carbonate apatite, and proteus mirabilis as a key factor of infectious urinary stone formation. Cryst. Growth Des. 2015, 15, 1446–1451. [Google Scholar] [CrossRef]
- Le Corre, K.S.; Valsami-Jones, E.; Hobbs, P.; Jefferson, B.; Parsons, S.A. Agglomeration of struvite crystals. Water Res. 2007, 41, 419–425. [Google Scholar] [CrossRef]
- Yuan, H.; Xue, J.; Qian, B.; Chen, H.; Zhu, Y.; Lan, M. Preparation and antifouling property of polyurethane film modified by chondroitin sulfate. Appl. Surf. Sci. 2017, 394, 403–413. [Google Scholar] [CrossRef]
- Riedl, C.R.; Witkowski, M.; Plas, E.; Pflueger, H. Heparin coating reduces encrustation of ureteral stents: A preliminary report. Int. J. Antimicrob. Agents 2002, 19, 507–510. [Google Scholar] [CrossRef]
- Chew, B.H.; Denstedt, J.D. Technology insight: Novel ureteral stent materials and designs. Nat. Clin. Pr. Urol. 2004, 1, 44–48. [Google Scholar] [CrossRef] [PubMed]
- Bonner, M.C.; Tunney, M.M.; Jones, D.S.; Gorman, S.P. Factors affecting in vitro adherence of ureteral stent biofilm isolates to polyurethane. Int. J. Pharma. 1997, 151, 201–207. [Google Scholar] [CrossRef]
- Cox, A.J.; Hukins, D.W.L. Morphology of mineral deposits on encrusted urinary catheters investigated by scanning electron microscopy. J. Urol. 1989, 142, 1347–1350. [Google Scholar] [CrossRef]
- Kumar, P.; Das, S. To study the biochemical analysis of kidney stone by using FTIR spectroscopy in the patients with renal calculosis. Res. Rev. J. Pharm. Anal. 2013, 2, 27–32. [Google Scholar]
- Tunney, M.M.; Keane, P.F.; Jones, D.S.; Gonnan, S.P. Comparative assessment of ureteral stent biomaterial encrustation. Biomaterials 1996, 17, 1541–1546. [Google Scholar] [CrossRef]
- Lagier, R.; Baud, C.A. Magnesium whitlockite, a calcium phosphate crystal of special interest in pathology. Pathol. Res. Pr. 2003, 199, 329–335. [Google Scholar] [CrossRef]
- Evan, A.P. Physiopathology and etiology of stone formation in the kidney and the urinary tract. Pediatr. Nephrol. 2010, 25, 831–841. [Google Scholar] [CrossRef]
- Griffith, D.P. Struvite stones. Kidney Int. 1978, 13, 372–382. [Google Scholar] [CrossRef]






| Polymer Type | Trade Name | Processing Temperature (°C) | Drying Temperature (°C) | Drying Process (h) |
|---|---|---|---|---|
| Thermoplastic Urethanes | Elastollan 1185A 10 FC | 188 | 100–111 | 2–4 |
| Carbothane PC 3585A | 193 | 65 (57) | 4-overnight | |
| Pelletane 2363 80A | 198 | 80–95 | 2–4 | |
| Tecoflex EG 60D | 193 | 65.5 (54.5) | 2-overnight | |
| Tecophilic HP 93A 100 | 182 | 65.5 (54.5) | 2-overnight | |
| Tecothane TT 1095 | 205 | 95 (80) | 2-overnight | |
| Styrene-Butadiene Copolymer | Styroflex 2G 66 | 235 | 90 | 2–4 |
| Ethylen-Vinylacetat | Greenflex FL 65 | 103 | 70 | 3 |
| Material | Contact Angle (°) at pH 6.5 | Surface Charge (mV) at pH 6.5 | Encrustation (%) | |||
|---|---|---|---|---|---|---|
| Elastollan | 85 | ±13 | −56.5 | ±2.8 | 2.4 | ±1.2 |
| Carbothane | 92 | ±2 | −41.2 | ±1.9 | 4.5 | ±3.3 |
| Pelletane | 105 | ±5 | −38.2 | ±2.3 | 4 | ±2.8 |
| Tecoflex | 111 | ±2 | −41.8 | ±2.8 | 2.9 | ±2.3 |
| Tecophilic | 104 | ±6 | −29.6 | ±2.8 | 6.0 | ±4.4 |
| Tecothane | 104 | ±4 | −47.9 | ±1.2 | 2.9 | ±1.6 |
| Styroflex | 85 | ±5 | −66.6 | ±3.6 | 2.1 | ±1.8 |
| Greenflex | 86 | ±1 | −56.4 | ±2.7 | 2.8 | ±1.2 |
| n = 3–10 independent replicates | n ≥ 3 independent replicates | n = 3 independent replicates | ||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rebl, H.; Renner, J.; Kram, W.; Springer, A.; Fritsch, N.; Hansmann, H.; Hakenberg, O.W.; Nebe, J.B. Prevention of Encrustation on Ureteral Stents: Which Surface Parameters Provide Guidance for the Development of Novel Stent Materials? Polymers 2020, 12, 558. https://doi.org/10.3390/polym12030558
Rebl H, Renner J, Kram W, Springer A, Fritsch N, Hansmann H, Hakenberg OW, Nebe JB. Prevention of Encrustation on Ureteral Stents: Which Surface Parameters Provide Guidance for the Development of Novel Stent Materials? Polymers. 2020; 12(3):558. https://doi.org/10.3390/polym12030558
Chicago/Turabian StyleRebl, Henrike, Jürgen Renner, Wolfgang Kram, Armin Springer, Nele Fritsch, Harald Hansmann, Oliver W. Hakenberg, and J. Barbara Nebe. 2020. "Prevention of Encrustation on Ureteral Stents: Which Surface Parameters Provide Guidance for the Development of Novel Stent Materials?" Polymers 12, no. 3: 558. https://doi.org/10.3390/polym12030558
APA StyleRebl, H., Renner, J., Kram, W., Springer, A., Fritsch, N., Hansmann, H., Hakenberg, O. W., & Nebe, J. B. (2020). Prevention of Encrustation on Ureteral Stents: Which Surface Parameters Provide Guidance for the Development of Novel Stent Materials? Polymers, 12(3), 558. https://doi.org/10.3390/polym12030558







