Flexural Strength of Resin Core Build-Up Materials: Correlation to Root Dentin Shear Bond Strength and Pull-Out Force
Abstract
1. Introduction
2. Materials and Methods
2.1. Flexural Strength
2.2. Shear Bond Strength to Root Dentin
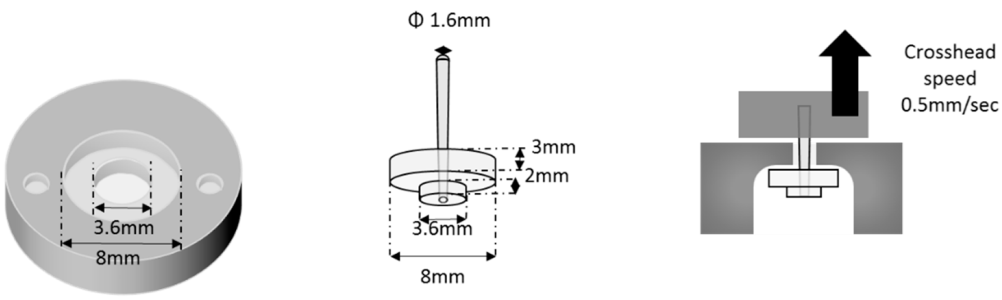
2.3. Pull-Out Force
2.4. Statistical Analysis
3. Results
3.1. Flexural Strength
3.2. Shear Bond Strength to Root Dentin
3.3. Pull-Out Force
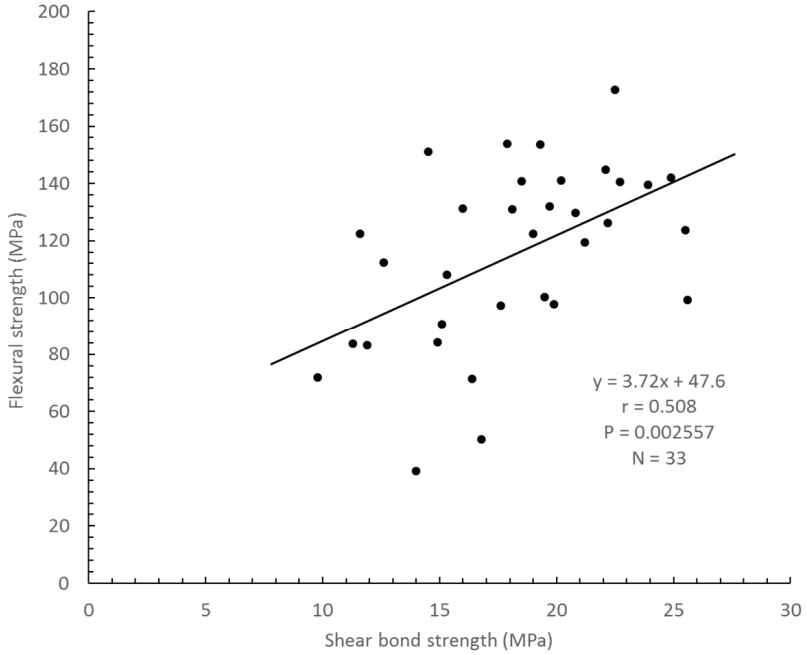
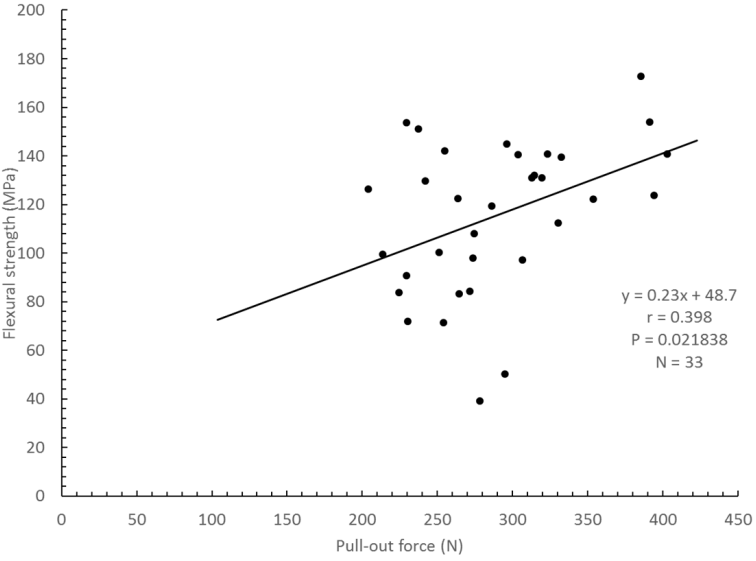
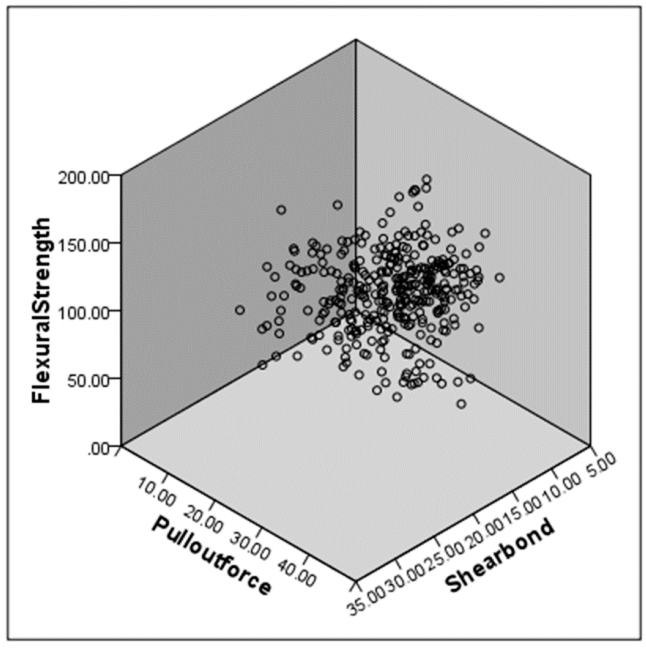
3.4. Correlation
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Sorensen, J.A.; Martinoff, T. Intracoronal reinforcement and coronal coverage: A study of eondodontically treated teeth. J. Prosthet. Dent. 1984, 51, 780–784. [Google Scholar] [CrossRef]
- Sidoli, G.E.; King, P.A.; Setchell, D.J. An in vitro evaluation of a carbon fiber based post and core system. J. Prosthet. Dent. 1997, 78, 5–9. [Google Scholar] [CrossRef]
- Mishra, L.; Khan, A.S.; Velo, M.M.A.C.; Saurav Panda, S.; Zavattini, A.; Rizzante, F.A.P.; Vega, H.I.A.; Sauro, S.; Lukomska-Szymanska, M. Effects of Surface Treatments of Glass Fiber-Reinforced Post on Bond Strength to Root Dentine: A Systematic Review. Materials 2020, 13, 1967. [Google Scholar] [CrossRef] [PubMed]
- Alshali, R.Z.; Salim, N.A.; Satterthwaite, J.D.; Silikas, N. Long-term sorption and solubility of bulk-fill and conventional resin-composites in water and artificial saliva. J. Dent. 2015, 43, 1511–1518. [Google Scholar] [CrossRef] [PubMed]
- Sokolowski, K.; Szczesio-Wlodarczyk, A.; Bociong, K.; Krasowski, M.; Fronczek-Wojciechowska, M.; Domarecka, M.; Sokolowski, J.; Lukomska-Szymanska, M. Contraction and Hydroscopic Expansion Stress of Dental Ion-Releasing Polymeric Materials. Polymers 2018, 10, 1093. [Google Scholar] [CrossRef] [PubMed]
- Pest, L.B.; Cavalli, G.; Bertani, P.; Gagliani, M. Adhesive post-endodontic restorations with fiber posts: Push-out tests and SEM observations. Dent. Mater. 2002, 18, 596–602. [Google Scholar] [CrossRef]
- Gutierrez, M.F.; Malaquias, P.; Matos, T.d.P.; De Souza, L.M.; Reis, A.; Perdigao, J.; Loguercio, A.D. Effect of self-curing activators and curing protocols on adhesive properties of universal adhesives bonded to dual-cured composites. Dent. Mater. 2017, 33, 775–787. [Google Scholar] [CrossRef]
- Combe, E.C.; Shaglouf, A.-M.S.; Watts, D.C.; Wilson, N.H.F. Mechanical properties of direct core build-up materials. Dent. Mater. 1999, 15, 158–165. [Google Scholar] [CrossRef]
- Ferrari, M.; Carvalho, C.A.; Goracci, C.F.; Antoniolli, A.; Mazzoni, G.; Mazzotti, M.C.; Breschi, L. Influence of luting material filler content on post cementation. J. Dent. Res. 2009, 88, 951–956. [Google Scholar] [CrossRef]
- Naumann, M.; Sterzenbach, G.; Rosentritt, M.; Beuer, F.; Meyer-Luckel, H.; Frankenberger, R. Self-adhesive cements as core build-ups for one-stage post-endodontic restorations? Int. Endod. J. 2011, 44, 95–202. [Google Scholar] [CrossRef]
- Pereira, J.R.; Do Valle, A.L.; Ghizoni, J.S.; Lorenzoni, F.C.; Ramos, M.B.; Dos Reis So, M.V. Push-out bond strengths of different dental cements used to cement glass fiber posts. J. Prosthet. Dent. 2013, 110, 134–140. [Google Scholar] [CrossRef]
- Rodrigues, R.V.; Sampaio, C.S.; Pacheco, R.R.; Pascon, F.M.; Puppin-Rontani, R.M.; Giannini, M. Influence of adhesive cementation systems on the bond strength of relined fiber posts to root dentin. J. Prosthet. Dent. 2017, 118, 493–499. [Google Scholar] [CrossRef] [PubMed]
- Goracci, C.; Raffaelli, O.; Monticelli, F.; Balleri, B.; Bertelli, E.; Ferrari, M. The adhesion between prefabricated FRC posts and composite resin cores: Microtensile bond strength with and without post-silanization. Dent. Mater. 2005, 21, 437–444. [Google Scholar] [CrossRef]
- Breschi, L.; Mazzoni, A.; Ruggeri, A.; Cadenaro, M.; Di Lenarda, R.; De Stefano Dorigo, E. Dental Adhesion review: Aging and stability of the bonded interface. Dent. Mater. 2008, 24, 90–101. [Google Scholar] [CrossRef] [PubMed]
- Zicari, F.; De Munck, J.; Scotti, R.; Naert, I.; Van Meerbeek, B. Factors affecting the cement-post interface. Dent. Mater. 2012, 28, 287–297. [Google Scholar] [CrossRef] [PubMed]
- Zicari, F.; Coutinho, E.; Scotti, R.; Van Meerbeek, B.; Naert, I. Mechanical properties and micro-morphology of fiber posts. Dent. Mater. 2013, 29, e45–e52. [Google Scholar] [CrossRef] [PubMed]
- Sadek, F.T.; Goracci, C.; Monticelli, F.; Grandini, S.; Cury, A.H.; Tay, F.; Ferrari, M. Immediate and 24-hours evaluation of the interfacial strengths of fiber posts. J. Endod. 2006, 32, 1174–1177. [Google Scholar] [CrossRef] [PubMed]
- Naumann, M.; Preuss, A.; Frankenberger, R. Reinforcement effect of adhesively luted fiber reinforced composite versus titanium posts. Dent. Mater. 2007, 23, 138–144. [Google Scholar] [CrossRef]
- Naumann, M.; Sterzenbach, G.; Rosentritt, M.; Beuer, F.; Frankenberger, R. Is adhesive cementation of endodontic posts necessary? J. Endod. 2008, 34, 1006–1010. [Google Scholar] [CrossRef]
- Akgungor, G.; Sen, D.; Aydin, M. Influence of different surface treatments on the short-term bond strength and durability between a zirconia post and composite resin core material. J. Prosthet. Dent. 2008, 99, 388–399. [Google Scholar] [CrossRef]
- Bitter, K.; Paris, S.; Pfuertner, C.; Neumann, K.; Kielbassa, A.M. Morphological and bond strength evaluation of different resin cements to root dentin. Eur. J. Oral Sci. 2009, 117, 326–333. [Google Scholar] [CrossRef] [PubMed]
- Sunada, N.; Ishii, R.; Shiratsuchi, S.; Shimizu, Y.; Tsubota, K.; Kurokawa, H.; Miyazaki, M. Ultrasonic measurement of the effects of adhesive application and power density on the polymerization behavior of core build-up resins. Acta Odontol. Scand. 2013, 71, 137–143. [Google Scholar] [CrossRef] [PubMed]
- Bitter, K.; Glaser, C.; Neumann, K.; Blunck, U.; Frankenberger, R. Analysis of resin-dentin interface morphology and bond strength evaluation of core materials for one stage post-endodontic restorations. PLoS ONE 2014, 9, e86924. [Google Scholar] [CrossRef] [PubMed]
- Irie, M.; Suzuki, K. Current luting cements: Marginal gap formation of co, mposite inlay and their mechanical properties. Dent. Mater. 2001, 17, 347–353. [Google Scholar] [CrossRef]
- Irie, M.; Suzuki, K.; Watts, D.C. Marginal and flexural integrity of three classes of luting cement, with early finishing and water storage. Dent. Mater. 2004, 20, 3–11. [Google Scholar] [CrossRef]
- Peutzfeldt, A.; Asmussen, E. Determinants of in vitro gap formation of resin composites. J. Dent. 2004, 32, 109–115. [Google Scholar] [CrossRef]
- Irie, M.; Hatanaka, K.; Suzuki, K.; Watts, D.C. Immediate versus water-storage performance of class V flowable composite restoratives. Dent. Mater. 2006, 22, 875–883. [Google Scholar] [CrossRef][Green Version]
- Hosaka, K.; Nakajima, M.; Takahashi, M.; Itoh, S.; Ikeda, M.; Tagami, J.; Pashley, D.H. Relationship between mechanical properties of one-step self-etch adhesives and water sorption. Dent. Mater. 2010, 26, 360–367. [Google Scholar] [CrossRef]
- Asmussen, E.; Peutzfeldt, A. Influence of UEDMA, BisGMA and TEGDMA on selected mechanical properties of experimental resin composites. Dent. Mater. 1998, 14, 51–56. [Google Scholar] [CrossRef]
- Irie, M.; Maruo, Y.; Nishigawa, G.; Suzuki, K.; Watts, D.C. Physical properties of dual-cured luting-agents correlated to early no interfacial-gap incidence with composite inlay restorations. Dent. Mater. 2010, 26, 608–615. [Google Scholar] [CrossRef]
- Takahashi, H.; Finger, W.J.; Utterodt, A.; Komatsu, M.; Woestmann, B.; Balkenhol, M. Factors influencing marginal cavity adaptation of nanofiller containing resin composite restorations. Dent. Mater. 2010, 26, 1166–1175. [Google Scholar] [CrossRef] [PubMed]
- Irie, M.; Maruo, Y.; Nishigawa, G. Performance of Class I composite restorations when polished immediately or after one-day water storage. PLoS ONE 2017, 12, e0183381. [Google Scholar] [CrossRef] [PubMed]
- Irie, M. Shear bond strength to human tooth and flexural strength of current resin cements. J. Jpn. Assoc. Dent. Traumatol. 2007, 3, 9–14. [Google Scholar]
- Al Sunbul, H.; Silikas, N.; Watts, D.C. Polymerization shrinkage kinetics and shrinkage-stress in dental resin-composites. Dent. Mater. 2016, 32, 998–1006. [Google Scholar] [CrossRef] [PubMed]
- Feilzer, A.J.; De Gee, A.J.; Davidson, C.L. Relaxation of polymerization contraction shear stress by hygroscopic expansion. J. Dent. Res. 1990, 69, 36–39. [Google Scholar] [CrossRef] [PubMed]
- Hatanaka, K.; Irie, M.; Tjandrawinata, R.; Suzuki, K. Effect of thermocycling on interfacial gap-formation in Class V cavities and mechanical properties of spherical silica filler addition to resin-modified glass ionomer restorations. Dent. Mater. J. 2006, 25, 655–663. [Google Scholar] [CrossRef][Green Version]
- Kumar, N.; Zafar, M.S.; Waheed, D.M.; Dahri, W.M.; Khan, M.A.; Khurshid, Z.; Shariq Najeeb, S. Effects of deformation rate variation on biaxial flexural properties of dental resin composites. J. Taibah Univ. Med. Sci. 2020, 15, 319–326. [Google Scholar] [CrossRef]
- Kumar, N.; Fareed, M.A.; Zafar, M.S.; Ghani, F.; Khurshid, Z. Influence of various specimen storage strategies on dental resin-based composite properties. Mater. Technol. 2020. [Google Scholar] [CrossRef]
- 3M-US. Permanent Dental Cements: Luting, Resin, Veneer. RelyX Self-Adhesive Resins for Oral Care. Available online: https://www.3m.com/3M/en_US/company-us/all-3m-products/~/All-3M-Products/Health-Care/Oral-Care/Dental-Products/Dental-Cements/RelyX/Permanent-Dental-Cements/Self-Adhesive-Resins/?N=5002385+8707795+8707799+8710731+8711017+8711728+8713393+8740260+8740284+3294857497&rt=r3 (accessed on 6 November 2020).
- Hu, M.; Weiger, R.; Fischer, J. Comparison of two test designs for evaluating the shear bond strength of resin composite cements. Dent. Mater. 2016, 32, 223–232. [Google Scholar] [CrossRef]
| Product | Composition | Manufacturer | Batch No. |
|---|---|---|---|
| FluoroCore 2+ | Barium fluoro alumino borosilicate glass (Silanated), Sialne treated silica, Aluminum Oxide, Bis-GMA, Urethane Dimetacrylate, Polymerizable dimetacrylate, Benzoyl Peroxide, Filler content: 69.1 wt.%, 46 vol.%. The particle size ranges from 0.04 to 25 µm. | Dentsply/Caulk, Milford, DE, USA | 160415 |
| RelyX Ultimate | Surface treated Glass Powder Filler, Phosphate ester monomer, TEGDMA, 1,12-Dodecane Dimethaycrylate, silica Filler, Initiator, Calcium Hydroxide, Titanium Dioxide, Filler content: About 70 wt.% | 3M, Seefeld, Germany | 642680 |
| RelyX Unicem 2 Automix | Surface treated Glass Powder Filler, Phosphate ester monomer, TEGDMA, 1,12-Dodecane Dimethaycrylate, Silica Filler, Initiator, Calcium Hydroxide, Sodium p-Toluensulfinatet, Methacrylated Amine, Titanium Dioxide, Filler content: About 70 wt.% | 3M, Seefeld, Germany | 646984 |
| Filtek Bulkfill Flowable Restorative | Silane Treated Ceramic, UDMA, Bis EMA, Bis-GMA, TEGDMA, Other Dimethacrylate, Ytterbium Fluoride, Filler content: 64.5 wt.%, 42.5 vol.% | 3M, St. Paul, USA | N815551 |
| NX3 | Barium Aluminoborosilicate glass, Ytterbium trifluoride, Fumed Silica, TEGDMA, UDMA, EBPADMA, Initiator, Stabilizer, Filler content: 67.5 wt.%, 43.3 vol.% | Kerr, Orange, CA, USA | 6021181 |
| MultiCore Flow | Ytterbium trifluoride, Bis-GMA, UDMA, TEGDMA, Dibenzoyl peroxide, Filler content: 70 wt.%, 46 vol.%, The particle size ranges from 0.04 to 25 µm. | Ivoclar Vivadent AG, Schaan, Liechtenstein | W02582 |
| UniFil Core EM | UDMA, Dimethacrylate, Fluoroaluminosilicate glass, Iron oxide, Dibenzoyl peroxide, Butylated hydroxytoluene, Filler content: 75 wt.% | GC, Tokyo, Japan | 1604251 |
| Beauti Core Flow Paste | Glass Powder Filler (S-PRG Filler), Bis-GMA, TEGDMA, Silica, Initiator, Others, Filler content: 60–70 wt.% | Shofu, Kyoro, Japan | 61610 |
| i-TFC system Post Resin | Dimethacrylates, Silica, Barium glass filler, Photoinitiators, Stabilizer, Others Filler content: 67 wt.% | Sun Medical, Moriyama, Shiga, Japan | MX13 |
| ESTECORE | Bis-GMA, TEGDMA, Bis-MPEPP, Silica-Zirconia Filler, Camphorquinone, Peroxide, Radial amplifier, Others, Filler content: 75 wt.% | Tokuyama Dental, Tokyo, Japan | 112006 |
| Clearfil DC Core Automix ONE | Bis-GMA, TEGDMA, Hydrophilic aliphatic dimethacrylate, Hydrophobic aromatic dimethacrylate, Silanated barium glass filler, Silanated colloidal silica, Colloidal silica, dl-Camphor Quinone, Aluminum oxide filler, Initiators, Accelerators, Pigments. Filler content: 74 wt.%, 52 vol.% | Kuraray Noritake Dental, Tainai, Niigata, Japan | B30218 |
| Adhesive | Batch No. | Composition | Manufacturer | Surface Treatment of Root Dentin | Surface Treatment of Fiber Post |
|---|---|---|---|---|---|
| Prime & Bond XP | 14000254 | PENTA, TCB resin, UDMA, TEGDMA, HEMA, Nanofiller, Camphorquinone, Butylated benzenediol, Ethyl-4 (dimethylamino) benzoate, Camphorquinone, Functionalised amorphous silica | Dentsply/Caulk Milford, DE, USA | Prime & Bond XP + Self Cure Activator (150306, 20 s) − air (5 s) − FluoroCore 2 ± light (20 s) | To fiber post: Prime & Bond XP + Self Cure Activator − air (5 s) |
| Scotchbond Universal Adhesive | 596935 | Bis GMA, HEMA, Decamethylene Dimethacrylate, Silane Treated Silica, Vitrabond Copolymer, MDP, Initiators, Silane, Ethanol | 3M, Seefeld, Germany | Scotchbond Universal Adhesive (20 s) − air (5 s) − light (10 s) − RelyX Ultimate − light (20 s). RelyX Unicem 2 Automix: None | Scotchbond Universal Adhesive (20 s) − air (5 s) − light (10 s). RelyX Unicem 2 Automix: None |
| OptiBond XTR (Primer) | 6001208 | GPDM, hydrophilic co-monomers, Water, ethanol, acetone, photo-initiator. | Kerr, Orange, CA, USA | OptiBond XTR Primer (20 s) − air (5 s) − OptiBond XTR Adhesive (15 s) − air (5 s) − light (10 s) − NX3 − light (20 s) | Porcelain Primer (091632, Shofu) − air (5 s) − OptiBond XTR Adhesive (15 s) − air (5 s) − light (10 s) |
| OptiBond XTR (Adhesive) | 6001210 | HEMA, dimethacrylate monomers, tri-functional methacrylate monomer, ethanol, photo-initiator, bariumaluminosilicate filler, nano-silica, Sodium hexafluorosilicate. | Kerr, Orange, CA, USA | ||
| Adhese Universal | V18786 | Methacrylates, Water, Ethanol, Highly dispersed silicon dioxide, Initiators and Stabilisers | Ivoclar Vivadent, Schaan, Liechtenstein | Adhese Universal (20 s) − air (5 s) − light (10 s) − MultiCore Flow − light (20 s) | Monobond Plus (60 s) − air (5 s) |
| Monobond Plus | U25466 | Ethanol, Methacrylated phosphoric acid ester | Ivoclar Vivadent, Schaan, Liechtenstein | ||
| G-Premio Bond | 1607212 | Acetone, Water, Dimethacrylate, 4-MET, Phosphoric ester monomer, Thiophosphoric ester monomer, Photoinitiator Butylated hydroxytoluene, Silica | GC, Tokyo, Japan | G-Premio BOND + G-Premio Bond DCA (10 s) − air (5 s) − light (10 s) − UniFil Core EM − light (20 s) | Ceramic Primer II– air (5 s) |
| G-Premio Bond DCA | 1603032 | Ethanol, Water, Catalyst | GC, Tokyo, Japan | ||
| Beauti Dual Bond EX (A) | 41607 | Acetone, Water, Initiator, Others | Shofu, Kyoto, Japan | Beauti Dual Bond EX (A + B, 10 s) − air (5 s) − light (10 s) − BeautiCore Flow Paste − light (20 s) | Porcelain Primer (091632, Shofu) − air (5 s) |
| Beauti Dual Bond EX (B) | 11608 | Acetone, Bis-GMA, Carboxylic acid monomer, TEGDMA, Initiator, Others | Shofu, Kyoto, Japan | ||
| Porcelain Primer | 91632 | Ethanol, silane coupling agent, Others | Shofu, Kyoto, Japan | ||
| i-TFC bond | MS 1 | Bond: Poly-function (math) metacrylates, Acetone, 4-META, Water, Silica, Others. Bond Brush: Aromatic amine, Sodium p-toluenesulfinate. | Sun Medical, Moriyama, Japan | i-TFC bond + i-TFC bond Brush (20 s) − air (5–10 s) − i-TFC system Post Resin − light (20 s) | i-TFC system FiberPost Primer (MF 1) |
| BONDMER lightless | 7067 | Liquid A: Phosphoric acid monomer (New 3D-SR monomer), MTU 6, HEMA, Bis-GMA, TEGDMA, Acetone, Others. Liquid B: γ-MPTES, Borate, Peroxide, Acetone, Isopropyl alcohol, Water, Others | Tokuyama Dental, Tokyo, Japan | BONDMER lightless (1–2 s) − air (5 s) | BONDMER lightless (1–2 s) − air (5 s) |
| Clearfil Universal Bond Quick | B30218 | 10-Methacryloyloxydecyl dihydrogen phosphate (10-MDP), HEMA, Bis-GMA, Ethanol, Water, Hydrophilic amide monomers, Colloidal silica, Sodium fluoride, dl-Camphorquinone. | Kuraray Noritake Dental, Tainai, Niigata, Japan | Clearfil Universal Bond Quick (1–2 s) − air (5 s) − light (10 s) − Clearfil DC Core Automix ONE − light (20 s) | Clearfil Universal Bond Quick + Clearfil Porcelain Bond Activator − air (5 s) |
| Clearfil Porcelain Bond Activator | 9D0033 | 3-MPTS, Hydrophobic aromatic dimethacrylate | Kuraray Noritake Dental, Tainai, Niigata, Japan |
| Product (Diameter) | Composition | Manufacturer | Batch No. |
|---|---|---|---|
| FluoroPost (1.6 mm) | Quartz fibers 60 vol.%, Epoxy resin vol.40% | Dentsply/Caulk, Milford, DE, USA | 160613 |
| RelyX FiberPost (1.6 mm) | Glass fibers, Composite resin matrix | 3M, Seefeld, Germany | 306831603 |
| FRC Postec Plus (1.6 mm) | Glass fibers, Dimethacrylates, Ytterbium fluoride | Ivoclar Vivadent AG, Schaan, Liechtenstein | V30339 |
| GC Fiber Post (1.6 mm) | Glass fibers, Metacrylate | GC, Tokyo, Japan | 1609021 |
| BeautiCore FiberPost (1.6 mm) | Glass fiber, Copolymer of Bis-GMA and Methacrylic ester monomer | Shofu, Kyoro, Japan | 41601 |
| i-TFC system Fiber Post (1.6 mm) | Glass fiber, Optical fiber, others | Sun Medical, Moriyama, Shiga, Japan | ML2 |
| Tokuyama FR Post (1.6 mm) | Glass fibers, Colpolymer Bis-GMA resin | Tokuyama Dental, Tokyo, Japan | 1604251 |
| Clearfil AD Fiber Post (1.6 mm) | Glass fibers, Colpolymer Bis-GMA and Methacrylic acid monomer | Kuraray Noritake Dental, Tainai, Niigata, Japan | 7U0001 |
| Time | |||
|---|---|---|---|
| Immediate | After One-Day Storage | TC 20k | |
| FluoriCore 2 | 83.3 (8.8) | 132.0 (8.4) | 122.4 (10.6) |
| RelyX Ultimate | 71.4 (4.6) | 119.4 (3.6) | 100.3 (4.9) |
| RelyX Unicem 2 Automix | 71.9 (5.7) | 108.0 (6.8) | 83.8 (5.1) |
| Filtek BulkFill Flowable Restorative | 50.3 (1.8) | 144.9 (5.3) | 129.7 (8.3) |
| NX3 | 39.1 (5.2) | 123.7 (9.8) | 97.9 (8.7) |
| MultiCore Flow | 99.4 (7.4) | 142.1 (9.1) | 126.3 (8.2) |
| UniFil Core EM | 90.8 (7.3) | 153.6 (11.4) | 151.2 (12.1) |
| BeautiCore Flow Paste | 112.4 (9.3) | 140.7 (7.9) | 131.1 (5.8) |
| i-TFC system Post Resin | 84.3 (4.1) | 139.4 (6.4) | 131.0 (7.6) |
| ESTECORE | 122.3 (9.1) | 172.8 (10.2) | 153.9 (13.3) |
| Clearfil DC Core Automix ONE | 97.3 (19.4) | 140.6 (9.6) | 140.9 (8.6) |
| FluoroCore 2 | RelyX Ultimate | RelyX Unicem 2 Automix | Filtek BulkFill Flowable Restorative | NX3 | MultiCore Flow | UniFil Core EM | BeautiCore Flow Paste | i-TFC System Post Resin | ESTECORE | Clearfil DC Core Automix One |
|---|---|---|---|---|---|---|---|---|---|---|
| Immediate | Immediate | Immediate b | Immediate | Immediate | Immediate | Immediate | Immediate | Immediate | Immediate | Immediate |
| TC 20k a | TC 20k | TC 20k b | TC 20k | TC 20k | TC 20k | TC 20k c | TC 20k d | TC 20k e | TC 20k | One-day f |
| One-day a | One-day | One-day | One-day | One-day | One-day | One-day c | One-day d | One-day e | One-day | TC 20k f |
| Immediately | After One-Day Storage | TC 20k |
|---|---|---|
| NX3 a | RelyX Unicem 2 Automix j | RelyX Unicem 2 Automix |
| Filtek BulkFill Flowable Restorative a | RelyX Ultimate j k | NX3 o |
| RelyX Ultimate b | NX3 k | RelyX Ultimate o |
| RelyX Unicem 2 Automix b | FluoriCore 2 k l | FluoriCore 2 p |
| FluoriCore 2 b c | i-TFC system Post Resin l m | MultiCore Flow p |
| i-TFC system Post Resin b c d e | Clearfil DC Core Automix ONE l m n | Filtek BulkFill Flowable Restorative p q |
| UniFil Core EM c d e f | BeautiCore Flow Paste l m n | i-TFC system Post Resin p q |
| Clearfil DC Core Automix ONE d e f g | MultiCore Flow l m n | BeautiCore Flow Paste p q |
| MultiCore Flow f g h | Filtek BulkFill Flowable Restorative l m n | Clearfil DC Core Automix ONE q r |
| BeautiCore Flow Paste h i | UniFil Core EM n | UniFil Core EM r |
| ESTECORE i | ESTECORE | ESTECORE r |
| Time | |||
|---|---|---|---|
| Immediately | After One-Day Storage | TC 20k | |
| FluoriCore 2 | 11.9 (3.6, 0) | 19.7 (2.3, 0) | 11.6 (2.9, 0) |
| RelyX Ultimate | 16.4 (3.8, 0) | 21.2 (4.9, 0) | 19.5 (3.3, 0) |
| RelyX Unicem 2 Automix | 9.8 (2.6, 0) | 15.3 (5.3, 0) | 11.3 (2.3, 0) |
| Filtek BulkFill Flowable Restorative | 16.8 (2.5, 0) | 22.1 (3.3, 0) | 20.8 (3.2, 0) |
| NX3 | 14.0 (2.1, 0) | 25.5 (3.5, 0) | 19.9 (3.6, 0) |
| MultiCore Flow | 25.6 (4.2, 0) | 24.9 (4.3, 0) | 22.2 (4.4, 0) |
| UniFil Core EM | 15.1 (3.2, 0) | 19.3 (5.3, 0) | 14.5 (3.2, 0) |
| BeautiCore Flow Paste | 12.6 (2.4, 0) | 18.5 (3.9, 0) | 16.0 (3.2, 0) |
| i-TFC system Post Resin | 14.9 (2.4, 0) | 23.9 (4.1, 0) | 18.1 (4.0, 0) |
| ESTECORE | 19.0 (4.9, 0) | 22.5 (4.3, 0) | 17.9 (3.2, 0) |
| Clearfil DC Core Automix ONE | 17.6 (4.0, 0) | 22.7 (4.0, 0) | 20.2 (4.0, 0) |
| FluoroCore 2 | RelyX Ultimate | RelyX Unicem 2 Automix | Filtek BulkFill Flowable Restorative | NX3 | MultiCore Flow | UniFil Core EM | BeautiCore Flow Paste | i-TFC System Post Resin | ESTECORE | Clearfil DC Core Automix ONE |
|---|---|---|---|---|---|---|---|---|---|---|
| TC 20k a | Immediate b | Immediate c | Immediate d | Immediate | TC 20k f | TC 20k g | Immediate h | Immediate i | TC 20k j | Immediate k |
| Immediate a | TC 20k b | TC 20k c | TC 20k d | TC 20k e | One-day f | Immediate g | TC 20k h | TC 20k i | Immediate j | TC 20k k |
| One-day | One-day b | One-day c | One-day d | One-day e | Immediate f | One-day g | One-day h | One-day | One-day j | One-day k |
| Immediately | After One-Day Storage | TC 20k |
|---|---|---|
| RelyX Unicem 2 Automix a | RelyX Unicem 2 Automix d | RelyX Unicem 2 Automix g |
| FluoriCore 2 a b | BeautiCore Flow Paste d e | FluoriCore 2 g h |
| BeautiCore Flow Paste a b | UniFil Core EM d e f | UniFil Core EM g h i |
| NX3 a b c | FluoriCore 2 d e f | BeautiCore Flow Paste g h i j |
| i-TFC system Post Resin a b c | RelyX Ultimate d e f | ESTECORE h i j |
| UniFil Core EM a b c | Filtek BulkFill Flowable Restorative e f | i-TFC system Post Resin i j |
| RelyX Ultimate b c | ESTECORE e f | RelyX Ultimate i j |
| Filtek BulkFill Flowable Restorative b c | Clearfil DC Core Automix ONE e f | NX3 i j |
| Clearfil DC Core Automix ONE b c | i-TFC system Post Resin e f | Clearfil DC Core Automix ONE i j |
| ESTECORE c | MultiCore Flow f | Filtek BulkFill Flowable Restorative i j |
| MultiCore Flow | NX3 f | MultiCore Flow j |
| Materials/Fiber Post (Pretreating Agent) | Time | ||
|---|---|---|---|
| Immediately | After One-Day Storage | TC 20k | |
| FluoriCore 2/Fluoropost (XP Bond + Self cure Activator) | 264.6 (40.2, 1) | 314.6 (40.2, 2) | 263.6 (33.3, 0) |
| RelyX Ultimate/RelyX Fiber Post (Scotchbond Universal Adhesive) | 253.8 (40.2, 2) | 286.2 (25.5, 2) | 250.9 (26.5, 1) |
| RelyX Unicem 2 Automix/RelyX Fiber Post (None) | 230.3 (22.5, 1) | 274.4 (14.7, 0) | 224.4 (30.1, 1) |
| Filtek BulkFill Flowable Restorative/RelyX Fiber Post (Scotchbond Universal Adhesive) | 295.0 (61.7, 1) | 296.0 (31.4, 0) | 242.1 (28.4, 0) |
| NX3/BeautiCore Fiber (Porcelain Primer (Shofu) + OptiBond XTR (Adhesive)) | 278.3 (47.0, 1) | 394.0 (44.1, 2) | 273.4 (45.1, 2) |
| MultiCore Flow/FRC Postec Plus (Monobond Plus) | 213.6 (34.3, 0) | 254.8 (19.6, 0) | 203.8 (34.3, 0) |
| UniFil Core EM/GC Fiber Post (Ceramic Primer II) | 229.3 (40.2, 0) | 229.3 (28.4, 0) | 237.2 (26.5, 0) |
| BeautiCore Flow Paste/BeautiCore FiberPost (Shofu Porcelain Primer) | 330.3 (46.1, 1) | 402.8 (31.4, 1) | 312.6 (75.5, 0) |
| i-TFC system Post Resin/i-TFC system Fiber Post (i-TFC system Fiber Post Primer) | 271.5 (41.2, 1) | 332.2 (39.2, 0) | 319.5 (49.0, 0) |
| ESTECORE/Tokuyama FR Post (BONDMER Lightless) | 353.8 (32.3, 0) | 385.1 (34.3, 0) | 391.0 (25.5, 0) |
| Clearfil DC Core Automix ONE/Clearfil AD Fiber Post (Universal Bond Quick + Porcelain Activator) | 306.7 (38.2, 1) | 303.8 (29.4, 1) | 323.4 (41.2, 0) |
| FluoroCore 2 | RelyX Ultimate | RelyX Unicem 2 Automix | Filtek BulkFill Flowable Restorative | NX3 | MultiCore Flow | UniFil Core EM | BeautiCore Flow Paste | i-TFC System Post Resin | ESTECORE | Clearfil DC Core Automix ONE |
|---|---|---|---|---|---|---|---|---|---|---|
| TC 20k a | TC 20k b | TC 20k c | TC 20k | TC 20k e | TC 20k f | Immediate g | TC 20k h | Immediate i | Immediate j | One-day k |
| Immediate a | Immediate b | Immediate c | Immediate d | Immediate e | Immediate f | One-day g | Immediate h | TC 20k i | One-day j | Immediate k |
| One-day | One-day b | One-day c | One-day d | One-day e | One-day f | TC 20k g | One-day | One-day i | TC 20k j | TC 20k k |
| Immediately | After One-Day Storage | TC 20k |
|---|---|---|
| MultiCore Flow/FRC Postec Plus a b | UniFil Core EM/GC Fiber Post f | MultiCore Flow/FRC Postec Plus |
| UniFil Core EM/GC Fiber Post a b | MultiCore Flow/FRC Postec Plus f g h | RelyX Unicem 2 Automix/RelyX Fiber Post l |
| RelyX Unicem 2 Automix/RelyX Fiber Post a b | RelyX Unicem 2 Automix/RelyX Fiber Post f g h | UniFil Core EM/GC Fiber Post l m |
| RelyX Ultimate/RelyX Fiber Post a b c | RelyX Ultimate/RelyX Fiber Post f g | Filtek BulkFill Flowable Restorative/RelyX Fiber Post l m |
| FluoriCore 2/Fluoropost a b c d | Filtek BulkFill Flowable Restorative/RelyX Fiber Post f g h i | RelyX Ultimate/RelyX Fiber Post l m n |
| i-TFC system Post esin/i-TFC system Fiber Post a b c d | Clearfil DC Core Automix ONE/Clearfil AD Fiber Post g h i | FluoriCore 2/Fluoropost l m n o |
| NX3/BeautiCore Fiber a b c d | FluoriCore 2/Fluoropost g h i | NX3/BeautiCore Fiber l m n o |
| Filtek BulkFill Flowable Restorative/RelyX Fiber Post b c d e | i-TFC system Post Resin/i-TFC system Fiber Post h i j | BeautiCore Flow Paste/BeautiCore FiberPost n o |
| Clearfil DC Core Automix ONE/Clearfil AD Fiber Post c d e | ESTECORE/Tokuyama FR Post j k | i-TFC system Post Resin/i-TFC system Fiber Post n o |
| BeautiCore Flow Paste/BeautiCore FiberPost d e | NX3/BeautiCore Fiber j k | Clearfil DC Core Automix ONE/Clearfil AD Fiber Post o p |
| ESTECORE/Tokuyama FR Post e | BeautiCore Flow Paste/BeautiCore FiberPost k | ESTECORE/Tokuyama FR Post p |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Irie, M.; Maruo, Y.; Nishigawa, G.; Yoshihara, K.; Matsumoto, T. Flexural Strength of Resin Core Build-Up Materials: Correlation to Root Dentin Shear Bond Strength and Pull-Out Force. Polymers 2020, 12, 2947. https://doi.org/10.3390/polym12122947
Irie M, Maruo Y, Nishigawa G, Yoshihara K, Matsumoto T. Flexural Strength of Resin Core Build-Up Materials: Correlation to Root Dentin Shear Bond Strength and Pull-Out Force. Polymers. 2020; 12(12):2947. https://doi.org/10.3390/polym12122947
Chicago/Turabian StyleIrie, Masao, Yukinori Maruo, Goro Nishigawa, Kumiko Yoshihara, and Takuya Matsumoto. 2020. "Flexural Strength of Resin Core Build-Up Materials: Correlation to Root Dentin Shear Bond Strength and Pull-Out Force" Polymers 12, no. 12: 2947. https://doi.org/10.3390/polym12122947
APA StyleIrie, M., Maruo, Y., Nishigawa, G., Yoshihara, K., & Matsumoto, T. (2020). Flexural Strength of Resin Core Build-Up Materials: Correlation to Root Dentin Shear Bond Strength and Pull-Out Force. Polymers, 12(12), 2947. https://doi.org/10.3390/polym12122947





