Abstract
The aim of this study was to evaluate the mechanical properties (flexural strength (FS), flexural modulus (FM), Vickers microhardness (VMN), and shear bond strength (SBS)) of preheated composites. Two preheated composites (Z350XT and Proclinic) and one self-adhesive resin cement (RelyX™ U200) were used to fabricate specimens. All the specimens were subjected to thermocycling before their mechanical properties were evaluated. One-way ANOVA was used for statistical analysis, followed by Tukey’s post hoc test. The chi-square test was used to evaluate the failure modes after SBS test. Results: RelyX™ U200 had a significantly higher FS (106.22 ± 14.23 MPa) than Proclinic (85.76 ± 12.75 MPa) and Z350 (71.47 ± 22.98 MPa). Z350 (118.10 ± 11.3 GPa) and RelyX™ U200 (110.88 ± 13.44 GPa) had significantly higher FMs than Proclinic (83.72 ± 9.3 GPa). A significantly higher VHN was seen with Z350 (136.84 ± 11.52 VHN) compared to Proclinic (115.25 ± 17.15 VHN) and RelyX™ U200 (100.83 ± 12.69 VHN). Z350 had a higher SBS (20.75 ± 5.6 MPa) than RelyX™ U200 (15.4 ± 3.46 MPa), while Proclinic was the weakest among all the groups (6.76 ± 1.44 MPa). In the failure mode analysis, the mixed failure mode was predominantly seen in all groups. In conclusion, not all preheated composites behave the same and it is the clinician’s responsibility to select the appropriate material for every clinical situation.
1. Introduction
Cementation plays a critical role in establishing proper retention and a marginal seal, as well as ensuring the longevity of indirect restorations. The ideal luting material must exhibit excellent adhesive properties, biocompatibility, mechanical strength, and long-term stability [1,2,3]. Resin cements are widely utilized because of their good bond strength and esthetics [4,5,6,7]. Nevertheless, their clinical efficacy may be limited by significant polymerization shrinkage and minimal color stability. These factors can influence the longevity and overall appearance of restorations [8,9,10].
Resin composites are one of the most adaptable materials in dentistry and are commonly utilized for direct restorations, allowing dentists to design the tooth morphology and replicate the optical properties of dental components [11,12,13,14]. Because of their esthetic qualities, ease of use, availability, capacity to bond to ceramic materials as well as the tooth structure, and relatively lower cost compared to resin cement, the use of restorative composite resins as luting agents has become more popular [1,15,16,17,18,19]. The higher viscosity of restorative composite resins due to their high-molecular-weight monomers and increased filler content makes their use as luting agents more challenging. Preheating the composite resins can effectively decrease the viscosity, improving the flowability and adaptation without compromising any of their other favorable properties [20,21].
Comprehensive investigations into the effects of heating on luting agents remain relatively limited. Understanding the effects of preheating on the mechanical properties and efficacy of composite luting agents is critical for determining their potential advantages or limitations in clinical practice. In order to address this knowledge gap, this in vitro study was conducted to systematically assess the mechanical properties (flexural strength, flexural modulus, Vickers microhardness, and shear bond strength) of preheated composites and compare them with those of self-adhesive resin cement. This study aimed to offer important insights into the viability and effectiveness of preheated composites in improving the mechanical properties of luting agents by utilizing standardized testing protocols. The null hypothesis was that there are no significant differences in mechanical properties between preheated composites and self-adhesive resin cement.
2. Materials and Methods
In this study, two preheated composites (FiltekTM Z350XT, 3M ESPE, Seefeld, Germany, and Proclinic Expert, SDI Limited, Victoria, Australia) and one self-adhesive resin cement (RelyX™ U200 Automix, 3M ESPE, Seefeld, Germany) were evaluated for flexural strength, flexural modulus, Vickers microhardness, and shear bond strength when bonded to lithium disilicate glass ceramics. This research study was reviewed and approved by the Research Ethics Committee of the Faculty of Dentistry at King Abdulaziz University (protocol number: 244-11-23; approval date: 7 January 2024). The required sample size was calculated using G*Power 3.1.9.7 statistical software. An effect size (f) of 0.5 was used, with a significance level (α) of 0.05 and a power of 80%, across the three test groups. The resulting total sample size was determined to be 42 specimens (14 specimens/group). We used 15 specimens/group which gave us a total sample size of 45 specimens/test. The composites were subjected to heating temperatures of 50° Celsius using a composite heater (AR composite heater, Fencia, Foshan, China), while the resin cement was used as supplied by the manufacturer without further heating. Table 1 details all the materials used in this study.

Table 1.
Materials used in this study and their composition.
2.1. Fabrication of Specimens
For the flexural strength test, 45 bar specimens (n = 15/group), each measuring 2 × 2 × 25 mm, were manufactured using a split stainless-steel mold following the ISO standard 4049 specifications. An additional 45 disk specimens measuring 10 × 2 mm were created for the Vickers microhardness test by packing the resin material in a split stainless-steel mold between transparent Mylar sheets. Using an E-Morlit curing light (Apoza, New Taipei, Taiwan) with a power output of 1200 mW/cm2, these specimens were light-cured for 40 s. The specimens were removed from the mold once the resin had fully polymerized, and flashes were cut off using a sharp scalpel. Any specimen with voids or defects was excluded. The specimens were then polished using silicon carbide abrasive paper (MetaServ 250, Buehler; Lake Bluff, IL, USA) with 220, 320, 600, and 1200 grit.
For the shear bond strength test, lithium disilicate blocks (IPS e. max CAD; Ivoclar Vivadent, Schaan, Liechtenstein) were sectioned using a low-speed diamond saw (Allied High Tech, Compton, CA, USA) into 45 slices measuring 10 × 7 × 2 mm. To obtain a standardized, flat surface, the cementation surfaces were sequentially polished with 220-, 320-, 600-, and 1200-grit silicon carbide abrasive paper. Each specimen was then sintered following the manufacturer’s guidelines. Afterward, they were embedded in self-cured acrylic resin measuring 15 mm in diameter and 10 mm in height, with the cementation surface left exposed. After 15 s of acid etching with 9.6% hydrofluoric acid, the cementation surfaces were rinsed with an oil-free water spray for 20 s. A universal ceramic primer (Monobond N; Ivoclar Vivadent, Schaan, Liechtenstein) was applied to the pretreated surface using a microbrush, left to react for 60 s, then air-dried to remove any excess primer. A split stainless-steel mold (2 mm in diameter and 3 mm in height) was used to bond the preheated composites and cement cylinders to the pretreated lithium disilicate surfaces, followed by a 40-second light curing using an E-Morlit curing light.
2.2. Thermocycling
All specimens were subjected to 5000 cycles of artificial aging at temperatures ranging from 5 to 55 °C (SD Mechatronik Thermocycler; JULABO GmbH, Seelbach, Germany). Each cycle lasted about 1 min. This aging protocol is equivalent to six months of clinical service [22].
2.3. Mechanical Testing
- Flexural Strength Test
A three-point bending test was conducted using a universal testing machine (INSTRON Model #5944, load cell 2 KN; Norwood, MA, USA) at a crosshead speed of 1 mm/min, with a 20 mm distance between the supports. The flexural strength and modulus were determined using the Bluehill 3 program (version 3.24.1496; Instron Worldwide Headquarters, Norwood, MA, USA). The flexural strength (S) was calculated using the following formula: S = 3FL/2bd2, where S is the flexural strength (MPa), F is the load at break (Newtons), L is the specimen span between supports (20 mm), b is the specimen width (2 mm), and d is the specimen thickness (2 mm). The flexural modulus (E) was calculated in MPa using the formula E = F1L3/4bd3D1, where E denotes the elastic modulus, F1 is the deflection force, L is the length of the specimen span between supports (20 mm), b is the specimen’s width, d is the specimen’s thickness, and D1 represents the deflection in the linear portion of the load-deflection curves.
- Vickers Microhardness Test
The microhardness of the specimens was tested using a Vickers hardness tester (HMV microhardness tester; SHIMADZU, Kyoto, Japan). Each specimen was subjected to five indentations for ten seconds using a 9.8 N load. After measuring each indent separately, the mean value was determined. Utilizing the following formula, the Vickers hardness number (VHN) was calculated: VHN = 1.8544 P/d2, where P is the applied weight (kg) and d is the mean of the indentations (mm).
- Shear Bond Strength Test
The shear bond strength test was conducted using a universal testing machine (INSTRON, Norwood, MA, USA). A compressive load was applied to the interface between the lithium disilicate and cement cylinders using a knife edge chisel at a crosshead speed of 1 mm/min until failure was observed. The shear bond strength (MPa) was determined by dividing the applied load (Newtons) at fracture by the area of the resin–lithium disilicate interface (mm2). Figure 1 shows the flowchart of the study and the materials used.
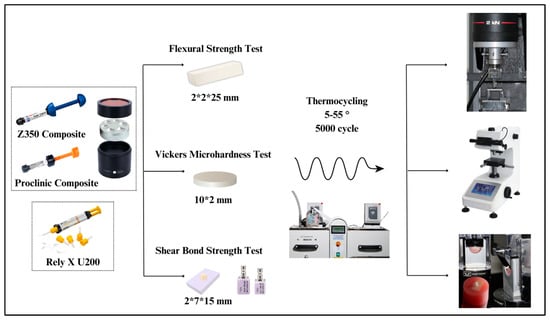
Figure 1.
Flowchart of the study design.
2.4. Failure Evaluation
For failure evaluation, the fracture surfaces of all the lithium disilicate specimens after the SBS test were inspected using a light stereomicroscope (MX 7520; Meiji Techno, Hicksville, NY, USA) at 40× magnification. The observed failure modes were recorded. The recorded modes of failure were adhesive failure (completely exposed lithium disilicate surface), cohesive failure (failure within the resin button), or mixed failure (exposed lithium disilicate surface with remnants of resin).
2.5. Statistical Analysis
Statistical analysis was conducted using JMP 17 Statistical Discovery software from SAS (SAS Campus Drive, Cary, NC, USA). Shapiro’s test of normality showed that all quantitative variables (flexural strength, flexural modulus, Vickers microhardness, and shear bond strength) maintained a normal distribution, allowing for parametric testing. The influence of the resin type on the mechanical properties was assessed using one-way ANOVA, followed by post hoc Tukey testing for pairwise comparisons, at a significance level of α = 0.05.
3. Results
Three different dental materials were tested to evaluate their mechanical characteristics: two preheated composites (FiltekTM Z350XT and Proclinic Expert) and one self-adhesive resin cement (RelyX™ U200 Automix). There were significant differences in flexural strength, flexural modulus, Vickers microhardness, and shear bond strength between the tested materials, so the null hypothesis was rejected (p < 0.05). Table 2 summarizes the descriptive and statistical analyses of the mechanical properties evaluated in the study.

Table 2.
Results of descriptive and statistical analyses of the mechanical properties evaluated in this study.
For flexural strength, one-way ANOVA revealed a significant difference between the test groups (p = 0.0002 *) (Table 2). The post hoc Tukey test showed that the RelyX™ U200 resin cement (106.22 ± 14.23 MPa) had a significantly higher flexural strength than the preheated Proclinic (85.76 ± 12.75 MPa) and Z350 (71.47 ± 22.98 MPa) composites. The two preheated composites were not significantly different from each other (Figure 2).
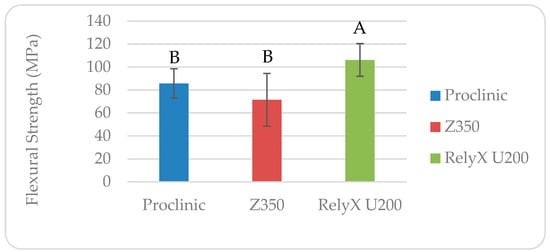
Figure 2.
Flexural strength of different materials evaluated in this study. Similar letters indicate that the difference is not significant (p > 0.05).
For flexural modulus, one-way ANOVA indicated significant differences between the groups (p < 0.0001) (Table 2). The post hoc Tukey test results showed that the preheated Z350 composite (118.10 ± 11.3 GPa) and RelyX™ U200 resin cement (110.88 ± 13.44 GPa) had significantly higher flexural moduli than the preheated Proclinic composite (83.72 ± 9.3 GPa) (Figure 3).
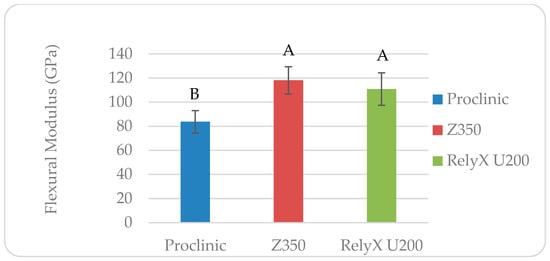
Figure 3.
Flexural modulus of different materials evaluated in this study. Similar letters indicate that the difference is not significant (p > 0.05).
For Vickers microhardness, one-way ANOVA revealed significant differences between the tested materials (p < 0.0001) (Table 2). The post hoc Tukey test results showed that the preheated Z350 composite (136.84 ± 11.52 VHN) had a significantly higher microhardness than the Proclinic composite (100.83 ± 12.69 VHN) and RelyX™ U200 resin cement (115.25 ± 17.15 VHN). The RelyX™ U200 self-adhesive resin cement had a significantly lower VHN than the other groups (Figure 4).
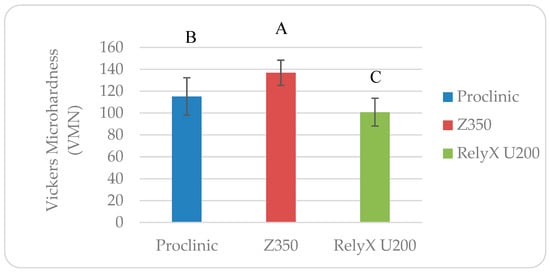
Figure 4.
Vickers microhardness of the different materials evaluated in this study. Similar letters indicate that the difference is not significant (p > 0.05).
For the shear bond strength (SBS) when bonded to lithium disilicate, the one-way ANOVA results showed significant differences between the tested materials (p < 0.0001) (Table 2). The post hoc Tukey test indicated that the preheated Z350 composite (20.75 ± 5.6 MPa) had a significantly higher SBS than the RelyX U200 resin cement (15.4 ± 3.46 MPa) and preheated Proclinic composite (6.76 ± 1.44 MPa). The preheated Proclinic composite had a significantly lower SBS compared to the other groups (Figure 5).
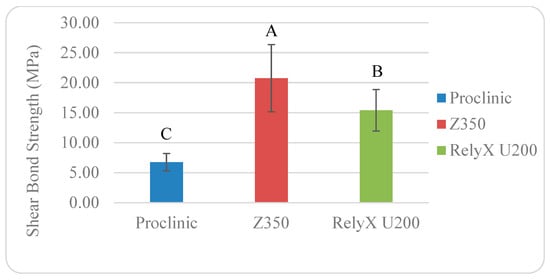
Figure 5.
Shear bond strength of different materials evaluated in this study. Similar letters indicate that the difference is not significant (p > 0.05).
The chi-square test revealed significant differences in the mode of failure (p < 0.000) within each cement group, with predominantly mixed failures (66.67% in Proclinic, 86.67% in RelyX™ U200, and 66.67% in Z350). When the failure modes of different cements were compared, the distribution of failure modes was statistically similar (p = 0.162) (Table 3 and Figure 6).

Table 3.
Results of descriptive and statistical analyses of failure modes of the different materials evaluated in this study.

Figure 6.
Modes of failure: (A) adhesive failure (completely exposed lithium disilicate surface), (B) cohesive failure (failure within the resin button), and (C) mixed failure (exposed lithium disilicate surface with remnants of resin).
4. Discussion
There is conflicting and unclear information regarding the impact of preheating on the mechanical properties of composite resins. Thus, it is important to assess whether dental clinicians can utilize them as an alternative to resin cement to obtain stronger luting and better mechanical characteristics. To assess this issue, this study compared different mechanical properties (flexural strength, flexural modulus, Vickers microhardness, and shear bond strength) of preheated composites to those of a self-adhesive resin cement. Significant differences were found between the test groups in all the tested properties, so the null hypothesis was rejected. The preheated Z350 nanocomposite performed better in terms of flexural modulus, microhardness, and shear bond strength than the other nanohybrid Proclinic composite and the RelyX™ U200 self-adhesive resin cement. Interestingly, RelyX™ U200 recorded a significantly higher flexural strength compared to the preheated composite resins. The preheated nanohybrid Proclinic composite performed the worst in almost all the mechanical properties evaluated.
Recently, there has been growing interest in using preheated composites as a luting agent. They have better mechanical properties because of a higher filler load compared to traditional resin cement [16,19]. Various techniques have been developed for preheating composite materials in dentistry [16]. The Calset oven by AdDent Inc. [2,23,24,25,26,27,28,29,30] has been a popular heating device in previous studies. Additionally, other preheating devices such as the Digital Wax Pot by SJK [31], ENA Heat by Micerium S.P.A [32], and Wax Heater Pot 4 [33] have also been used. The ideal heating device should be moisture-free, able to attain a certain temperature (between 50 °C and 68 °C), and stable once heated [16]. The composite material is often heated with a device to a particular temperature, which then must be maintained by storing it in a heater. This approach increases the resin conversion rate to match those of dual-polymerized resin cements, improves flow homogeneity, and allows for a thinner cementation layer [16]. To avoid harming the pulp, it is recommended to keep the composite resin temperature between 50 °C and 60 °C, as this range has little influence on the intra-pulpal tissue. According to Lopes et al., the remaining dentin thickness acts as a shield, protecting the tooth pulp from harmful stimuli [34]. Moreover, a study by Sokołowska et al. [35] tested composites at room temperature (20 °C), 39 °C, and 50 °C. It was concluded that the samples heated to 50 °C demonstrated noticeably better mechanical properties compared to the samples heated to 39 °C.
Several factors might affect preheated composite materials, including the heating temperature, rate, and time, and the composition of the composite [16]. Excessive heat may compromise the material’s integrity by initiating premature polymerization or degrading sensitive components [16]. Similarly, the heating rate needs to be carefully controlled to avoid thermal stresses: slower rates promote uniform softening, whereas rapid heating can lead to inconsistencies [36]. The duration of heating is another key variable; longer heating times help maintain the flowable state of the material, while overexposure can disrupt the composite’s chemical balance or partially polymerize the resin [37]. Moreover, the composition of the composite itself, including the resin matrix and filler content, dictates its response to preheating. Composites with a high filler content retain heat better, while low-viscosity monomers enhance adaptability and the ease of handling [38]. Carefully optimizing these factors ensures workability and long-term success in clinical applications.
Heating resin composites has been reported to have certain limitations, including a limited working time before the viscosity of the resin composite is restored. When the heated composite resin is withdrawn from the heating unit, it cools rapidly, typically losing 50% of its heat in 2 min [39]. As a result, the material has to be quickly inserted and fitted, and the restoration is seated and light polymerized. Maintaining the high temperature will result in a greater monomer conversion than at room temperature (23 °C) [16]. The equipment used in this technique was designed to maintain temperatures of 54 °C and 60 °C; however, in the research by Daronch et al. using the Calset oven (Addent Inc.), the maximum temperatures measured were only 48.3 °C and 54.7 °C, despite the manufacturer’s claims [16,39]. Therefore, to obtain the required quality and performance of the final composite product, proper optimization and control of the preheating process are essential [15,16].
The mechanical properties of luting materials have a significant influence on the durability and strength of dental restorations in the dynamic oral cavity [40]. By examining these mechanical properties, a more complete picture of the material’s performance under actual settings can be obtained, which can be used to inform decision-making in clinical practice. Additionally, this study’s findings might serve as a baseline for additional research aimed at optimizing the use of composite materials in various dental applications, which would ultimately improve patient outcomes and satisfaction.
Flexural strength is an important mechanical feature that reveals how resistant a material is to fracture. It is defined as the greatest stress that a sample can withstand until it breaks, which reflects its capacity to sustain occlusal stresses and functional loads [41]. In this study, RelyX™ U200 exhibited the highest mean flexural strength, followed by Proclinic and Z350. This result can be explained by the lower filler load in RelyX™ U200, which results in a higher proportion of resin matrix. The higher resin matrix content enhances the material’s flexibility, allowing it to bend more during testing, which indicates that more energy can be absorbed before fracturing. The findings for the composites align with the research by Fróes-Salgado, Nívea Regina et al. [42] which found that preheating the composite did not have a significant impact on the flexural strength or monomer conversion. As previously mentioned by Lovell et al. and Daronch et al., the quick drop in composite temperature during handling can help to explain this result. They proposed that the temperature of the composite likely drops by the time it is light-cured. Thus, the temperature was not high enough at this point to improve the mechanical qualities of the composite [39,43]. On the other hand, these findings were different from those of previous studies [44,45,46]; this discrepancy might be due to the different materials, test settings, and aging protocols. The relatively high standard deviation values for flexural strength may be attributed to the inherent heterogeneity in the composite matrix, as well as potential variations introduced during the manual sample preparation and curing processes [47,48].
The flexural modulus measures the stiffness or rigidity of the material. A material with a high flexural modulus can resist bending, which is essential for the long-term performance of dental restorations [49]. In ceramic restorations, the cement’s capacity to transfer forces from the restoration to the tooth structure and its ability to tolerate elastic deformation are significantly influenced by its modulus of elasticity [50,51]. Furthermore, the fracture resistance of all-ceramic restorations is greatly influenced by the elastic characteristics of the supporting dental structure, emphasizing the need to maintain compatibility between the cement and the dental substrate for optimal performance [52,53,54]. In this study, the preheated Z350 composite exhibited the highest flexural modulus compared to the other groups. This can be attributed to the composite’s higher molecular weight and the presence of more rigid monomers, which contribute to its rigidity. However, when plastic deformation occurs, preheated composites are more brittle and tend to fracture, leading to a lower flexural strength. These findings are in agreement with those of previous studies [1,55]. The studies by D’Amario et al., Sharafeddin et al., and Mohammadi et al. showed that preheating composites induces significant improvements in mechanical properties [44,55,56,57]. Nada et al. and Deb et al. also found that preheating improved the flexural strength and decreased polymerization shrinkage [58,59]. However, Kim et al. and D’Amario et al. found no significant effect of preheating in some composite formulations, suggesting that the effectiveness of preheating is dependent on the filler quantity and resin composition [56,60].
Microhardness is an important mechanical characteristic that indicates a material’s resistance to indentation or penetration. The material’s composition in terms of filler size, shape, and proportions of components affects its microhardness. In addition, when it comes to long-term restoration success, a microhardness test can provide valuable information about the material’s overall strength, wear resistance, and occlusal force tolerance [61,62,63]. However, the increased surface hardness after heating is most likely the result of the creation of a strongly crosslinked network due to a greater conversion rate [61]. Raising the temperature reduces the viscosity, increases the mobility of free radicals [61,64], and increases the possibility of interactions between free radicals and active groups due to the greater thermal energy [59]. Consequently, the warmed composite resin has enhanced microhardness due to an increased conversion rate [13,61]. However, not all preheated composites behave the same. One possible explanation for this is the variation in the resin monomers’ molecular structure, which affects the composite resins’ surface microhardness. According to Daronch et al.’s investigation, resin composites polymerized at ambient temperature have a lower amount of monomer conversion than warmed composites [37]. In another study, Eliades et al. discovered that as the amount of inorganic filler increased, so did the hardness levels. Several other parameters also affected hardness levels, including the monomer type and ratio, filler particle distribution and morphology, polymer crosslinking, particle density and shape, and degree of monomer conversion. These variations may have affected the surface microhardness of the materials investigated in that study [65]. Nonetheless, conflicting results exist in the literature, with some research claiming that excessive preheating might reduce microhardness due to the degradation of or changes in the composite’s resin matrix [66]. Regarding Vickers microhardness, Z350 showed the highest mean value, followed by the Proclinic composite and then the RelyX™ U200 resin cement.
Several studies have investigated the influence of preheating on shear bond strength. The shear bond strength test measures the highest force that an adhesive joint is capable of withstanding before breaking. Shear bond strength plays an essential role in indirect restorations as it determines their longevity, stability, and functional performance [2,31]. The SBS needs to be optimized through the selection of suitable adhesive methods, surface treatments, and materials to ensure the optimal clinical outcomes [2]. The effects of preheating on the shear bond strength of composite resins could be attributed to its ability to enhance the flowability, increase the degree of conversion, enhance the adaptation between the tooth structure and the composite resin, and decrease the polymerization shrinkage stress [31,61]. Nonetheless, the effectiveness is influenced by the temperature, material composition, and clinical technique [2]. Preheating has been shown to increase the shear bond strength of dental composites to varying degrees. An increased temperature can facilitate better wetting, leading to improved bonding between the composite and the tooth structure. Moreover, the bonding between the restoration and the tooth structure can improve the restoration’s overall mechanical strength [67]. In 2023, an in vitro study suggested that preheated composites used with feldspathic ceramic as a luting agent resulted in a comparable bond strength to that of adhesive cementation [68]. Reboul et al. [18] found that the shear bond strength was lower for the heated composite group with a bonding agent than for the Panavia V5 (resin cement) groups with or without immediate dentin sealing (IDS). Furthermore, another study also compared the shear bond strength of preheated microhybrid and nanohybrid composites with that of resin cement and showed significant variations in the results among the groups. The resin cement group had the highest shear bond strength [69]. However, it is important to remember that the optimum temperature for preheating may differ depending on the composite material. Some composites may reach their optimal shear bond strength at lower temperatures, while others may require higher temperatures for the best results. Furthermore, the duration of preheating might affect the shear bond strength. Prolonged heating over the recommended temperature range can impair the composite’s mechanical characteristics, reducing its bonding capacity [56]. Dental composites are often warmed to temperatures ranging from 37 °C to 60 °C (98.6 °F to 140 °F) to improve handling and flowability [34,70]. Daronch et al. showed a 50% decline in temperature in composite samples 2 min after removal from the heating unit. As a result, the researchers proposed that dentists need to work quickly to minimize the drop in temperature for optimal clinical performance [39]. In our study, we found that the preheated Z350 composite exhibited the highest mean SBS value at 20.75 ± 5.6 MPa, followed by RelyX™ U200 and Proclinic. This suggests that preheating the Z350 composite improved its rigidity, flow, and adaptation to surfaces, resulting in a stronger bond compared to RelyX™ U200 and Proclinic.
The modes of failure were assessed by examining the fracture surfaces of all the lithium disilicate specimens under 40× magnification using a light stereomicroscope. Three failure modes were noted: cohesive, adhesive, and mixed failure modes. There was a consistent trend towards mixed failure modes in all the materials, with the Z350 and Proclinic composites showing nearly identical distributions. Mixed failure was shown to be the predominant type of failure, which indicates that all the materials had a good bond strength. This result can be attributed to the chemical bond produced by the surface treatment using 9.6% hydrofluoric acid and the universal ceramic primer. These findings underscore the importance of considering material characteristics in dental applications and suggest a need for further investigation into the factors influencing failure modes to optimize material performance. Mixed and cohesive failures indicate good bond strength, while adhesive failures indicate poor bonding [71]. However, preheating composite resins is a promising method for cementation of indirect restorations. It can lower the viscosities and improve the mechanical characteristics of composite materials, producing cement film thicknesses that are clinically acceptable [16]. In a separate study, Foes-Salgado et al. discovered that, while various mechanical parameters remained unaffected, preheating significantly improved the marginal adaptation of Filtek Z350, primarily due to energy density considerations [42].
There are several limitations in this study. First, this was an in vitro study. Evaluations of the mechanical properties of preheated composites after controlled humidity cycles, representative salivary microbiota, and thermal–pH fluctuations to approximate intra-oral conditions could be considered for future studies. Another limitation is the heating device. The effects of preheating composites are sensitive to the technique and might be improved with more standard devices. Moreover, only one heating temperature (50 °C) was used so it would be interesting to evaluate the effects of different heating temperatures. In addition, the cement film thickness of the preheated composite was not evaluated. Thus, further in vitro and clinical studies incorporating various composite types and testing at different temperatures are essential to obtain more conclusive results.
5. Conclusions
The following conclusions from this in vitro study were drawn: The preheated Z350 nanocomposite performed better in terms of flexural modulus, microhardness, and shear bond strength than the other nanohybrid Proclinic composite and the RelyX™ U200 self-adhesive resin cement. Higher flexural strength values were seen with RelyX™ U200, indicating that more energy was absorbed before fracture. The preheated nanohybrid Proclinic composite showed the worst mechanical properties, highlighting the variability among resin composites and emphasizing careful material selection. The predominant mixed failure mode indicated that the material had a good bond strength when bonded to lithium disilicate glass ceramics.
Author Contributions
Conceptualization, M.S.H.; Data curation, L.F.A. and R.S.A.; Formal analysis, M.S.H., L.F.A., R.S.A. and S.J.A.; Investigation, L.F.A. and R.S.A.; Methodology, M.S.H., L.F.A. and R.S.A.; Project administration, M.S.H.; Resources, L.F.A. and R.S.A.; Software, M.S.H., L.F.A. and R.S.A.; Supervision, M.S.H.; Validation, Y.M.M., H.K.F., M.B., K.A.A., N.A.T. and S.J.A.; Visualization, Y.M.M., H.K.F., M.B., K.A.A., N.A.T. and S.J.A.; Writing—original draft, M.S.H., L.F.A. and R.S.A.; Writing—review and editing, Y.M.M., H.K.F., M.B., K.A.A., N.A.T. and S.J.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki and approved by the Research Ethics Committee of the Faculty of Dentistry, King Abdulaziz University (protocol number: 244-11-23; approval date: 7 January 2024).
Data Availability Statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
Acknowledgments
The authors would like to thank the Advanced Technology Dental Research Laboratory at the Faculty of Dentistry, King Abdulaziz University, for the help with the laboratory work in this project.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Skapska, A.; Komorek, Z.; Cierech, M.; Mierzwinska-Nastalska, E. Comparison of mechanical properties of a self-adhesive composite cement and a heated composite material. Polymers 2022, 14, 2686. [Google Scholar] [CrossRef]
- Acquaviva, P.A.; Cerutti, F.; Adami, G.; Gagliani, M.; Ferrari, M.; Gherlone, E.; Cerutti, A. Degree of conversion of three composite materials employed in the adhesive cementation of indirect restorations: A micro-raman analysis. J. Dent. 2009, 37, 610–615. [Google Scholar] [CrossRef]
- Sinha, I. Adhesive cementation of ceramic restorations: A comprehensive review. INNOSC Theranostics Pharmacol. Sci. 2023, 6, 28–34. [Google Scholar] [CrossRef]
- Hill, E.E.; Lott, J. A clinically focused discussion of luting materials. Aust. Dent. J. 2011, 56 (Suppl. S1), 67–76. [Google Scholar] [CrossRef] [PubMed]
- Leung, G.K.; Wong, A.W.; Chu, C.H.; Yu, O.Y. Update on dental luting materials. Dent. J. 2022, 10, 208. [Google Scholar] [CrossRef]
- Maletin, A.; Knezevic, M.J.; Koprivica, D.D.; Veljovic, T.; Puskar, T.; Milekic, B.; Ristic, I. Dental resin-based luting materials—Review. Polymers 2023, 15, 4156. [Google Scholar] [CrossRef]
- Stamatacos, C.; Simon, J.F. Cementation of indirect restorations: An overview of resin cements. Compend. Contin. Educ. Dent. 2013, 34, 42–44, 46. [Google Scholar] [PubMed]
- Lee, S.M.; Choi, Y.S. Effect of ceramic material and resin cement systems on the color stability of laminate veneers after accelerated aging. J. Prosthet. Dent. 2018, 120, 99–106. [Google Scholar] [CrossRef]
- Alkhudhairy, F.; Vohra, F.; Naseem, M.; Owais, M.M.; Amer, A.H.B.; Almutairi, K.B. Color stability and degree of conversion of a novel dibenzoyl germanium derivative containing photo-polymerized resin luting cement. J. Appl. Biomater. Funct. Mater. 2020, 18, 2280800020917326. [Google Scholar] [CrossRef]
- Bouschlicher, M.R.; Rueggeberg, F.A. Effect of ramped light intensity on polymerization force and conversion in a photoactivated composite. J. Esthet. Restor. Dent. 2000, 12, 328–339. [Google Scholar] [CrossRef]
- Cho, K.; Rajan, G.; Farrar, P.; Prentice, L.; Prusty, B.G. Dental resin composites: A review on materials to product realizations. Compos. Part B Eng. 2022, 230, 109495. [Google Scholar]
- Lopes, G.C.; Vieira, L.C.; Araujo, E. Direct composite resin restorations: A review of some clinical procedures to achieve predictable results in posterior teeth. J. Esthet. Restor. Dent. 2004, 16, 19–31. [Google Scholar] [CrossRef] [PubMed]
- Bhopatkar, J.; Ikhar, A.; Chandak, M.; Mankar, N.; Sedani, S. Composite pre-heating: A novel approach in restorative dentistry. Cureus 2022, 14, e27151. [Google Scholar] [CrossRef]
- Darabi, F.; Tayefeh-Davalloo, R.; Tavangar, S.M.; Naser-Alavi, F.; Boorboo-Shirazi, M. The effect of composite resin preheating on marginal adaptation of class II restorations. J. Clin. Exp. Dent. 2020, 12, e682–e687. [Google Scholar] [CrossRef]
- Raposo, C.C.; Nery, L.M.S.; Carvalho, E.M.; Ferreira, P.V.C.; Ardenghi, D.M.; Bauer, J.; Lima, D.M. Effect of preheating on the physicochemical properties and bond strength of composite resins utilized as dental cements: An in vitro study. J. Prosthet. Dent. 2023, 129, 229.E1–229.E7. [Google Scholar] [CrossRef]
- Lousan do Nascimento Poubel, D.; Zanon, A.E.G.; Almeida, J.C.F.; de Lucas Rezende, L.V.M.; Garcia, F.C.P. Composite resin preheating techniques for cementation of indirect restorations. Int. J. Biomater. 2022, 2022, 5935668. [Google Scholar] [CrossRef]
- Gugelmin, B.P.; Miguel, L.C.M.; Filho, F.B.; Cunha, L.F.D.; Correr, G.M.; Gonzaga, C.C. Color stability of ceramic veneers luted with resin cements and pre-heated composites: 12 months follow-up. Braz. Dent. J. 2020, 31, 69–77. [Google Scholar] [CrossRef]
- Reboul, T.; Thai, H.A.H.; Cetik, S.; Atash, R. Comparison between shear forces applied on the overlay-dental tissue interface using different bonding techniques: An in vitro study. J. Indian Prosthodont. Soc. 2018, 18, 212–218. [Google Scholar] [CrossRef]
- Teyagirwa, P.F.; Aquin, C.; Kharouf, N.; Roman, T.; Senger, B.; Reitzer, F.; Etienne, O. Operator versus material influence on film thickness using adhesive resin cement or pre-heated resin composite. J. Esthet. Restor. Dent. 2023, 35, 517–524. [Google Scholar] [CrossRef]
- El-Deeb, H.A.; El-Aziz, S.A.; Mobarak, E.H. Effect of preheating of low shrinking resin composite on intrapulpal temperature and microtensile bond strength to dentin. J. Adv. Res. 2015, 6, 471–478. [Google Scholar] [CrossRef]
- O’cOnnor, C.; Gavriil, D. Predictable bonding of adhesive indirect restorations: Factors for success. Br. Dent. J. 2021, 231, 287–293. [Google Scholar] [CrossRef]
- Morresi, A.L.; D’Amario, M.; Capogreco, M.; Gatto, R.; Marzo, G.; D’Arcangelo, C.; Monaco, A. Thermal cycling for restorative materials: Does a standardized protocol exist in laboratory testing? A literature review. J. Mech. Behav. Biomed. Mater. 2014, 29, 295–308. [Google Scholar] [CrossRef] [PubMed]
- Magne, P.; Oderich, E.; Boff, L.L.; Cardoso, A.C.; Belser, U.C. Fatigue resistance and failure mode of cad/cam composite resin implant abutments restored with type III composite resin and porcelain veneers. Clin. Oral Implant. Res. 2011, 22, 1275–1281. [Google Scholar] [CrossRef]
- Magne, P.; Razaghy, M.; Carvalho, M.A.; Soares, L.M. Luting of inlays, onlays, and overlays with preheated restorative composite resin does not prevent seating accuracy. Int. J. Esthet. Dent. 2018, 13, 318–332. [Google Scholar] [PubMed]
- Oderich, E.; Boff, L.L.; Cardoso, A.C.; Magne, P. Fatigue resistance and failure mode of adhesively restored custom implant zirconia abutments. Clin. Oral Implant. Res. 2012, 23, 1360–1368. [Google Scholar] [CrossRef]
- Rickman, L.J.; Padipatvuthikul, P.; Chee, B. Clinical applications of preheated hybrid resin composite. Br. Dent. J. 2011, 211, 63–67. [Google Scholar] [CrossRef] [PubMed]
- Schlichting, L.H.; Maia, H.P.; Baratieri, L.N.; Magne, P. Novel-design ultra-thin cad/cam composite resin and ceramic occlusal veneers for the treatment of severe dental erosion. J. Prosthet. Dent. 2011, 105, 217–226. [Google Scholar] [CrossRef]
- Soares, L.M.; Razaghy, M.; Magne, P. Optimization of large mod restorations: Composite resin inlays vs. Short fiber-reinforced direct restorations. Dent. Mater. 2018, 34, 587–597. [Google Scholar] [CrossRef]
- Magne, P.; Schlichting, L.H.; Maia, H.P.; Baratieri, L.N. In vitro fatigue resistance of cad/cam composite resin and ceramic posterior occlusal veneers. J. Prosthet. Dent. 2010, 104, 149–157. [Google Scholar] [CrossRef]
- Magne, P.; Knezevic, A. Influence of overlay restorative materials and load cusps on the fatigue resistance of endodontically treated molars. Quintessence Int. 2009, 40, 729–737. [Google Scholar] [PubMed]
- Goulart, M.; Veleda, B.B.; Damin, D.; Ambrosano, G.M.B.; de Souza, F.H.C.; Erhardt, M.C.G. Preheated composite resin used as a luting agent for indirect restorations: Effects on bond strength and resin-dentin interfaces. Int. J. Esthet. Dent. 2018, 13, 86–97. [Google Scholar] [PubMed]
- Mounajjed, R.; Salinas, T.J.; Ingr, T.; Azar, B. Effect of different resin luting cements on the marginal fit of lithium disilicate pressed crowns. J. Prosthet. Dent. 2018, 119, 975–980. [Google Scholar] [CrossRef] [PubMed]
- Olivares, J.M.; Hidalgo, A.; Pavez, J.P.; Benadof, D.; Irribarra, R. Functional and esthetic restorative treatment with preheated resins in a patient with ectodermic dysplasia: A clinical report. J. Prosthet. Dent. 2018, 119, 526–529. [Google Scholar] [CrossRef]
- Lopes, L.C.P.; Terada, R.S.S.; Tsuzuki, F.M.; Giannini, M.; Hirata, R. Heating and preheating of dental restorative materials—A systematic review. Clin. Oral Investig. 2020, 24, 4225–4235. [Google Scholar] [CrossRef] [PubMed]
- Sokołowska, J.; Masre, N.; Domarecka, M.; Sokołowski, J. Influence of polymerization temperature on durability of dental composites. Dent. Med. Probl. 2010, 47, 153–159. [Google Scholar]
- Yang, J. Temperature Effects on Pre-Cure and Post-Cure Properties of Dental Resin Composites. Ph.D. Thesis, University of Manchester, Manchester, UK, 2021. [Google Scholar]
- Daronch, M.; Rueggeberg, F.A.; De Goes, M.F. Monomer conversion of pre-heated composite. J. Dent. Res. 2005, 84, 663–667. [Google Scholar] [CrossRef]
- da Costa, J.B.; Hilton, T.J.; Swift, E.J., Jr. Critical appraisal: Preheating composites. J. Esthet. Restor. Dent. 2011, 23, 269–275. [Google Scholar] [CrossRef]
- Daronch, M.; Rueggeberg, F.A.; Moss, L.; de Goes, M.F. Clinically relevant issues related to preheating composites. J. Esthet. Restor. Dent. 2006, 18, 340–350. [Google Scholar] [CrossRef]
- Mei, M.L.; Chen, Y.M.; Li, H.; Chu, C.H. Influence of the indirect restoration design on the fracture resistance: A finite element study. Biomed. Eng. Online 2016, 15, 3. [Google Scholar] [CrossRef]
- Tribst, J.P.M.; Etoeharnowo, L.; Tadros, M.; Feilzer, A.J.; Werner, A.; Kleverlaan, C.J.; Piva, A.M.O.D. The influence of pre-heating the restoration and luting agent on the flexural strength of indirect ceramic and composite restorations. Biomater. Investig. Dent. 2023, 10, 2279066. [Google Scholar] [CrossRef]
- Froes-Salgado, N.R.; Silva, L.M.; Kawano, Y.; Francci, C.; Reis, A.; Loguercio, A.D. Composite pre-heating: Effects on marginal adaptation, degree of conversion and mechanical properties. Dent. Mater. 2010, 26, 908–914. [Google Scholar] [CrossRef]
- Lovell, L.G.; Newman, S.M.; Bowman, C.N. The effects of light intensity, temperature, and comonomer composition on the polymerization behavior of dimethacrylate dental resins. J. Dent. Res. 1999, 78, 1469–1476. [Google Scholar] [CrossRef] [PubMed]
- D’Amario, M.; De Angelis, F.; Vadini, M.; Marchili, N.; Mummolo, S.; D’Arcangelo, C. Influence of a repeated preheating procedure on mechanical properties of three resin composites. Oper. Dent. 2015, 40, 181–189. [Google Scholar] [CrossRef]
- Kramer, M.R.; Edelhoff, D.; Stawarczyk, B. Flexural strength of preheated resin composites and bonding properties to glass-ceramic and dentin. Materials 2016, 9, 83. [Google Scholar] [CrossRef]
- Kimyai, S.; Mashayekhi, Z.; Mohammadi, N.; Bahari, M.; Kahnamouei, M.A.; Chaharom, M.E.E. Comparison of the effect of preheating on the flexural strength of giomer and nanohybrid composite resin. J. Dent. Res. Dent. Clin. Dent. Prospect. 2022, 16, 159–163. [Google Scholar] [CrossRef]
- Meenakumari, C.; Bhat, K.M.; Bansal, R.; Singh, N. Evaluation of mechanical properties of newer nanoposterior restorative resin composites: An in vitro study. Contemp. Clin. Dent. 2018, 9, S142–S146. [Google Scholar] [CrossRef] [PubMed]
- Basheer, R.R.; Hasanain, F.A.; Abuelenain, D.A. Evaluating flexure properties, hardness, roughness and microleakage of high-strength injectable dental composite: An in vitro study. BMC Oral Health 2024, 24, 546. [Google Scholar] [CrossRef]
- Banditmahakun, S.; Kuphausuk, W.; Kanchanavasita, W.; Kuphasuk, C. The effect of base materials with different elastic moduli on the fracture loads of machinable ceramic inlays. Oper. Dent. 2006, 31, 180–187. [Google Scholar] [CrossRef]
- Banks, R.G. Conservative posterior ceramic restorations: A literature review. J. Prosthet. Dent. 1990, 63, 619–626. [Google Scholar] [CrossRef]
- Moscovich, H.; Roeters, F.J.; Verdonschot, N.; de Kanter, R.J.; Creugers, N.H. Effect of composite basing on the resistance to bulk fracture of industrial porcelain inlays. J. Dent. 1998, 26, 183–189. [Google Scholar] [CrossRef]
- Lee, S.K.; Wilson, P.R. Fracture strength of all-ceramic crowns with varying core elastic moduli. Aust. Dent. J. 2000, 45, 103–107. Available online: https://www.ncbi.nlm.nih.gov/pubmed/10925505 (accessed on 1 May 2025). [PubMed]
- Braga, R.R.; Cesar, P.F.; Gonzaga, C.C. Mechanical properties of resin cements with different activation modes. J. Oral Rehabil. 2002, 29, 257–262. [Google Scholar] [CrossRef]
- de la Macorra, J.C.; Pradíes, G. Conventional and adhesive luting cements. Clin. Oral Investig. 2002, 6, 198–204. [Google Scholar] [CrossRef] [PubMed]
- Sharafeddin, F.; Motamedi, M.; Fattah, Z. Effect of preheating and precooling on the flexural strength and modulus of elasticity of nanohybrid and silorane-based composite. J. Dent. 2015, 16 (Suppl. S3), 224–229. [Google Scholar] [PubMed]
- D’Amario, M.; Pacioni, S.; Capogreco, M.; Gatto, R.; Baldi, M. Effect of repeated preheating cycles on flexural strength of resin composites. Oper. Dent. 2013, 38, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Mohammadi, N.; Jafari-Navimipour, E.; Kimyai, S.; Ajami, A.A.; Bahari, M.; Ansarin, M.; Ansarin, M. Effect of pre-heating on the mechanical properties of silorane-based and methacrylate-based composites. J. Clin. Exp. Dent. 2016, 8, e373–e378. [Google Scholar] [CrossRef][Green Version]
- Nada, K.; El-Mowafy, O. Effect of precuring warming on mechanical properties of restorative composites. Int. J. Dent. 2011, 2011, 536212. [Google Scholar] [CrossRef] [PubMed]
- Deb, S.; Di Silvio, L.; Mackler, H.E.; Millar, B.J. Pre-warming of dental composites. Dent. Mater. 2011, 27, e51–e59. [Google Scholar] [CrossRef]
- Kim, A.R.; Jeon, Y.C.; Jeong, C.M.; Yun, M.J.; Choi, J.W.; Kwon, Y.H.; Huh, J.B. Effect of activation modes on the compressive strength, diametral tensile strength and microhardness of dual-cured self-adhesive resin cements. Dent. Mater. J. 2016, 35, 298–308. [Google Scholar] [CrossRef]
- Lucey, S.; Lynch, C.D.; Ray, N.J.; Burke, F.M.; Hannigan, A. Effect of pre-heating on the viscosity and microhardness of a resin composite. J. Oral Rehabil. 2010, 37, 278–282. [Google Scholar] [CrossRef]
- Munoz, C.A.; Bond, P.R.; Sy-Munoz, J.; Tan, D.; Peterson, J. Effect of pre-heating on depth of cure and surface hardness of light-polymerized resin composites. Am. J. Dent. 2008, 21, 215–222. [Google Scholar] [PubMed]
- Bausch, J.R.; de Lange, C.; Davidson, C.L. The influence of temperature on some physical properties of dental composites. J. Oral Rehabil. 1981, 8, 309–317. [Google Scholar] [CrossRef] [PubMed]
- Prasanna, N.; Reddy, Y.P.; Kavitha, S.; Narayanan, L.L. Degree of conversion and residual stress of preheated and room-temperature composites. Indian J. Dent. Res. 2007, 18, 173–176. [Google Scholar] [CrossRef] [PubMed]
- Eliades, G.C.; Vougiouklakis, G.J.; Caputo, A.A. Degree of double bond conversion in light-cured composites. Dent. Mater. 1987, 3, 19–25. [Google Scholar] [CrossRef]
- Bhopatkar, J.; Ikhar, A.; Chandak, M.; Patel, A.; Agrawal, P. Examining the impact of preheating on the fracture toughness and microhardness of composite resin: A systematic review. Cureus 2023, 15, e47117. [Google Scholar] [CrossRef]
- de Kok, P.; Pereira, G.K.R.; Fraga, S.; de Jager, N.; Venturini, A.B.; Kleverlaan, C.J. The effect of internal roughness and bonding on the fracture resistance and structural reliability of lithium disilicate ceramic. Dent. Mater. 2017, 33, 1416–1425. [Google Scholar] [CrossRef]
- Grangeiro, M.T.V.; Rodrigues, C.D.S.; Rossi, N.R.; Souza, K.B.; Melo, R.M.; Bottino, M.A. Preheated composite as an alternative for bonding feldspathic and hybrid ceramics: A microshear bond strength study. J. Adhes. Dent. 2023, 25, 159–166. [Google Scholar] [CrossRef]
- Maghfira, H.; Hidayat, R.; Amalina, R. Comparison of shear strength cementation of preheated resin composite and resin cement on indirect lithium disilicate. J. Medali 2022, 4, 110. [Google Scholar] [CrossRef]
- Knight, J.S.; Fraughn, R.; Norrington, D. Effect of temperature on the flow properties of resin composite. Gen. Dent. 2006, 54, 14–16. [Google Scholar] [PubMed]
- Davis, M.J.; Bond, D.A. The importance of failure mode identification in adhesive bonded aircraft structures and repairs. In Proceedings of the 12th International Conference on Composite Materials, Paris, France, 5–9 July 1999. Presented at 2008. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).