Effect of Indocyanine Green-Guided Lymphadenectomy During Gastrectomy on Survival: Individual Patient Data Meta-Analysis
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Data Extraction
2.3. Outcomes of Interest and Definition
2.4. Quality Assessment and Assessment of Certainty of Evidence
2.5. Statistical Analysis
3. Results
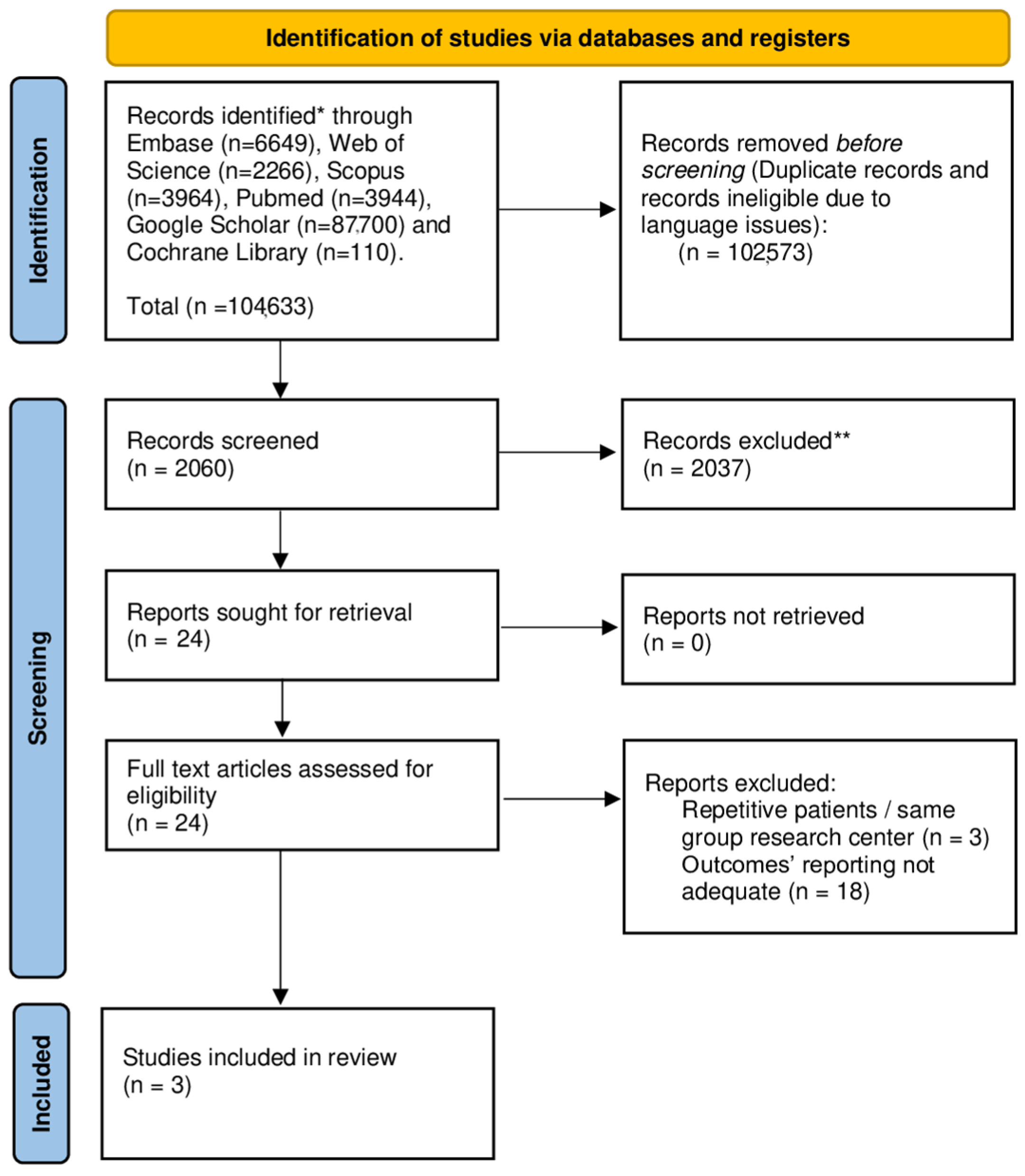
3.1. Systematic Review
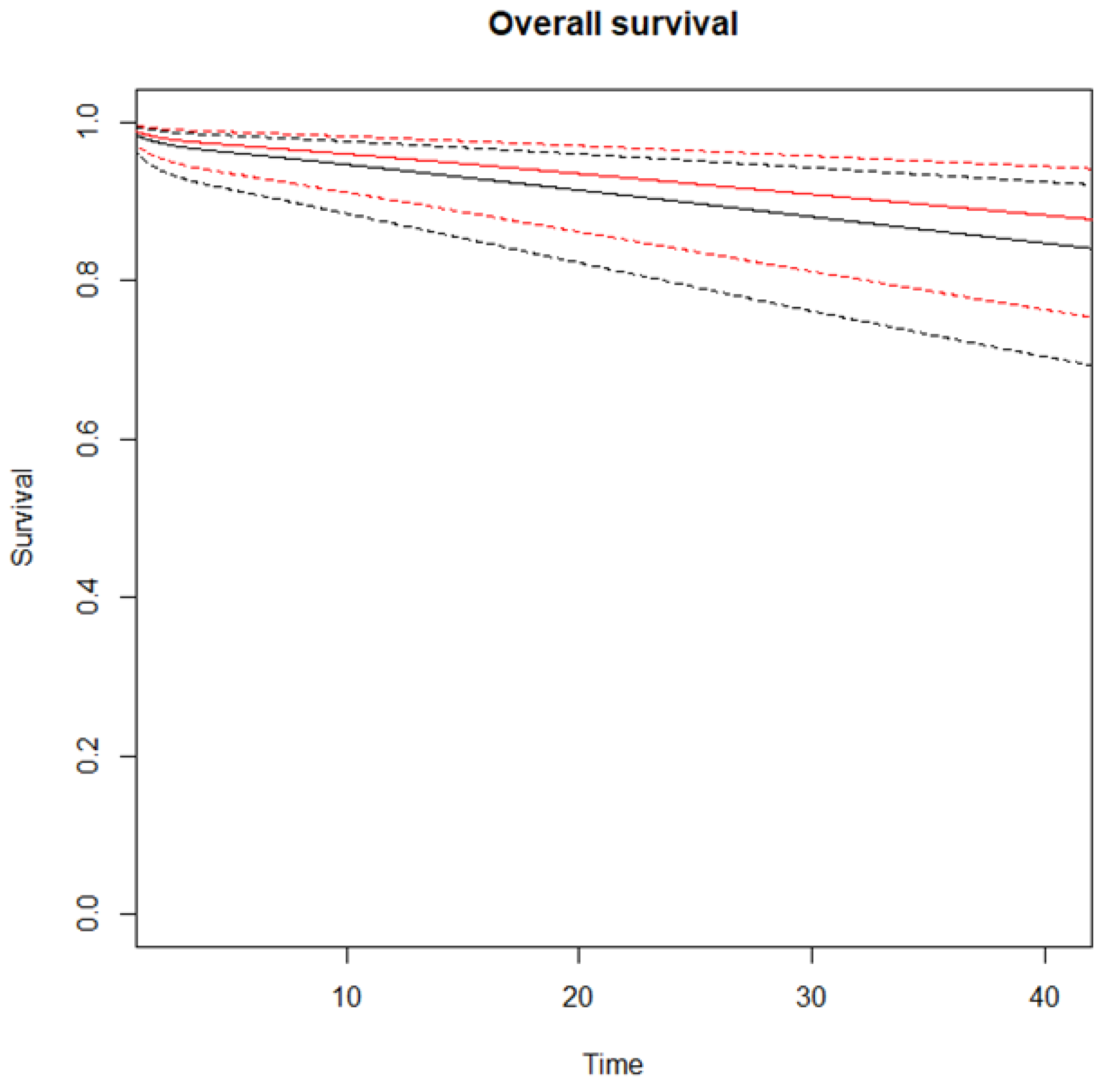
3.2. Meta-Analysis—Primary Outcomes
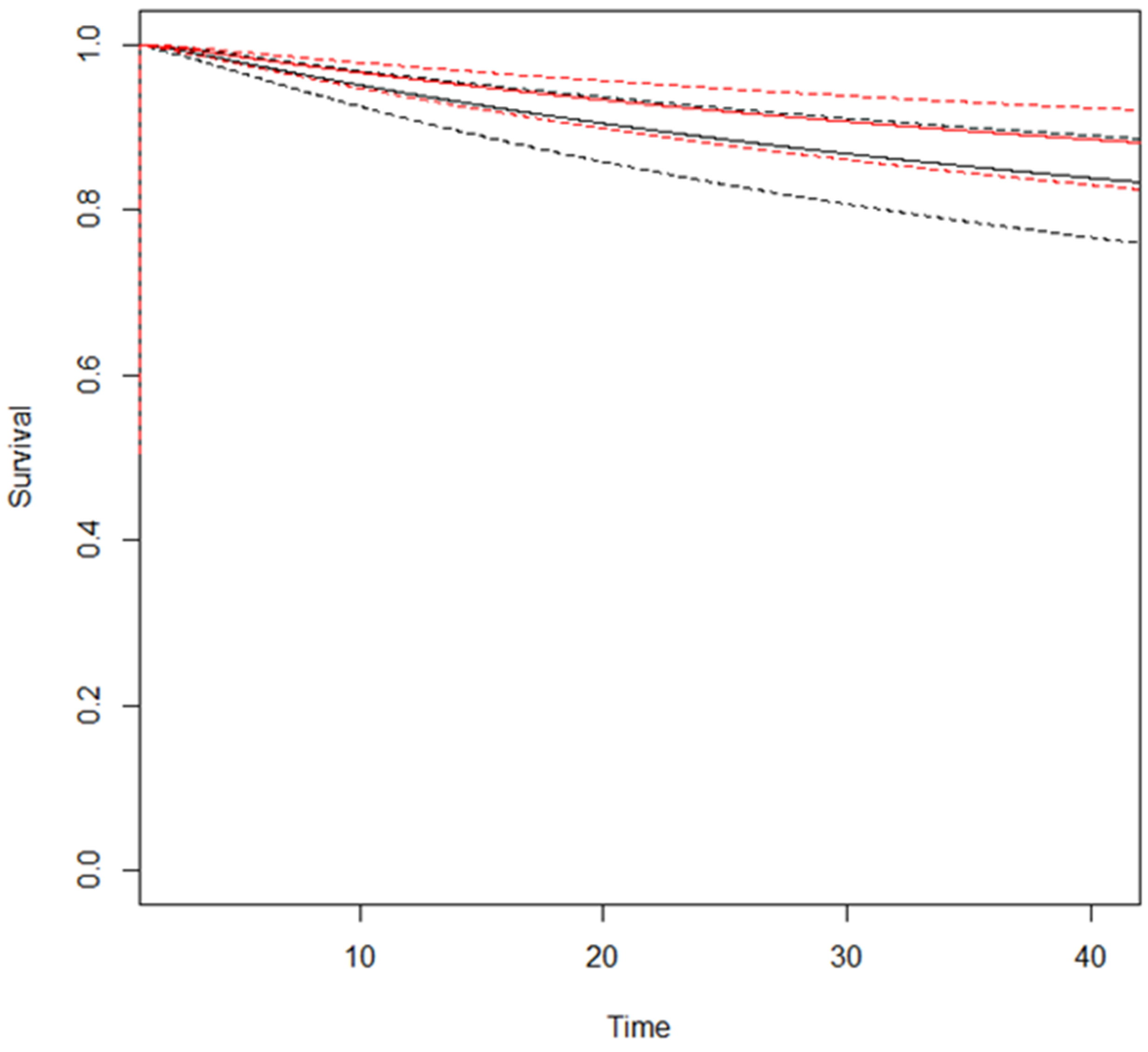
3.3. Secondary Outcomes
3.4. Certainty of Evidence
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
List of Abbreviations
| GC | Gastric Cancer |
| LN | Lymph Node |
| AJCC | American Joint Committee on Cancer |
| BMI | Body Mass Index |
| CI | Confidence Interval |
| OS | Overall Survival |
| DFS | Disease-Free Survival |
| EGJ | Esophagogastric Junction |
| ESMO | European Society for Medical Oncology |
| GRADE | Grading of Recommendations, Assessment, Development, and Evaluation |
| HER2 | Human Epidermal Growth Factor Receptor 2 |
| HR | Hazard Ratio |
| ICG | Indocyanine Green |
| IPD | Individual Patient Data |
| IPTW | Inverse Probability of Treatment Weighting |
| MeSH | Medical Subject Headings |
| MMR/MSI | Mismatch Repair/Microsatellite Instability |
| NCCN | National Comprehensive Cancer Network |
| OR | Odds Ratio |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| RCT | Randomized Controlled Trial |
| RMSTD | Restricted Mean Survival Time Difference |
| ROB | Risk of Bias |
| SE | Standard Error |
| SMD | Standardized Mean Difference |
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Ferlay, J.; Colombet, M.; Soerjomataram, I.; Parkin, D.M.; Piñeros, M.; Znaor, A.; Bray, F. Cancer Statistics for the Year 2020: An Overview. Int. J. Cancer 2021, 149, 778–789. [Google Scholar] [CrossRef] [PubMed]
- Lordick, F.; Carneiro, F.; Cascinu, S.; Fleitas, T.; Haustermans, K.; Piessen, G.; Vogel, A.; Smyth, E.C. Gastric Cancer: ESMO Clinical Practice Guideline for Diagnosis, Treatment and Follow-Up. Ann. Oncol. 2022, 33, 1005–1020. [Google Scholar] [CrossRef] [PubMed]
- van Velzen, M.J.M.; Braemer, M.; Nieuwenhuijzen, G.A.P.; van Sandick, J.W.; Siersema, P.D.; Ruurda, J.P.; Verheij, M.; Spaander, M.C.W.; Beerepoot, L.V.; Haj Mohammad, N.; et al. Incidence, Stage, Treatment, and Survival of Noncardia Gastric Cancer. JAMA Netw. Open 2023, 6, e2330018. [Google Scholar] [CrossRef]
- Ajani, J.A.; D’Amico, T.A.; Bentrem, D.J.; Chao, J.; Cooke, D.; Corvera, C.; Das, P.; Enzinger, P.C.; Enzler, T.; Fanta, P.; et al. Gastric Cancer, Version 2.2022. JNCCN J. Natl. Compr. Cancer Netw. 2022, 20, 167–192. [Google Scholar] [CrossRef]
- Wang, J.; Wang, L.; Li, S.; Bai, F.; Xie, H.; Shan, H.; Liu, Z.; Ma, T.; Tang, X.; Tang, H.; et al. Risk Factors of Lymph Node Metastasis and Its Prognostic Significance in Early Gastric Cancer: A Multicenter Study. Front. Oncol. 2021, 11, 649035. [Google Scholar] [CrossRef]
- Pelc, Z.; Skórzewska, M.; Rawicz-Pruszyński, K.; Polkowski, W.P. Lymph Node Involvement in Advanced Gastric Cancer in the Era of Multimodal Treatment—Oncological and Surgical Perspective. Cancers 2021, 13, 2509. [Google Scholar] [CrossRef]
- Schmidt, B.; Yoon, S.S. D1 versus D2 Lymphadenectomy for Gastric Cancer. J. Surg. Oncol. 2013, 107, 259–264. [Google Scholar] [CrossRef]
- Monrabal Lezama, M.; Murdoch Duncan, N.S.; Bertona, S.; Schlottmann, F. Current Standards of Lymphadenectomy in Gastric Cancer. Updates Surg. 2023, 75, 1751–1758. [Google Scholar] [CrossRef]
- Arigami, T.; Uenosono, Y.; Yanagita, S.; Nakajo, A.; Ishigami, S.; Okumura, H.; Kijima, Y.; Ueno, S.; Natsugoe, S. Clinical Significance of Lymph Node Micrometastasis in Gastric Cancer. Ann. Surg. Oncol. 2013, 20, 515–521. [Google Scholar] [CrossRef]
- Memon, M.A.; Subramanya, M.S.; Khan, S.; Hossain, M.B.; Osland, E.; Memon, B. Meta-Analysis of D1 versus D2 Gastrectomy for Gastric Adenocarcinoma. Ann. Surg. 2011, 253, 900–911. [Google Scholar] [CrossRef] [PubMed]
- Aiolfi, A.; Bona, D.; Bonitta, G.; Lombardo, F.; Manara, M.; Sozzi, A.; Schlanger, D.; Popa, C.; Cavalli, M.; Campanelli, G.; et al. Long-Term Impact of D2 Lymphadenectomy during Gastrectomy for Cancer: Individual Patient Data Meta-Analysis and Restricted Mean Survival Time Estimation. Cancers 2024, 16, 424. [Google Scholar] [CrossRef] [PubMed]
- Lu, J.; Zheng, C.H.; Cao, L.L.; Li, P.; Xie, J.W.; Wang, J.B.; Lin, J.X.; Chen, Q.Y.; Lin, M.; Huang, C.M. The Effectiveness of the 8th American Joint Committee on Cancer TNM Classification in the Prognosis Evaluation of Gastric Cancer Patients: A Comparative Study between the 7th and 8th Editions. Eur. J. Surg. Oncol. 2017, 43, 2349–2356. [Google Scholar] [CrossRef]
- Woo, Y.; Goldner, B.; Ituarte, P.; Lee, B.; Melstrom, L.; Son, T.; Noh, S.H.; Fong, Y.; Hyung, W.J. Lymphadenectomy with Optimum of 29 Lymph Nodes Retrieved Associated with Improved Survival in Advanced Gastric Cancer: A 25,000-Patient International Database Study. J. Am. Coll. Surg. 2017, 224, 546–555. [Google Scholar] [CrossRef]
- Jung, M.K.; Cho, M.; Roh, C.K.; Seo, W.J.; Choi, S.; Son, T.; Il Kim, H.; Hyung, W.J. Assessment of Diagnostic Value of Fluorescent Lymphography-Guided Lymphadenectomy for Gastric Cancer. Gastric Cancer 2021, 24, 515–525. [Google Scholar] [CrossRef]
- Kwon, I.G.; Son, T.; Il Kim, H.; Hyung, W.J. Fluorescent Lymphography-Guided Lymphadenectomy during Robotic Radical Gastrectomy for Gastric Cancer. JAMA Surg. 2019, 154, 141–149. [Google Scholar] [CrossRef]
- Chen, Q.Y.; Xie, J.W.; Zhong, Q.; Bin Wang, J.; Lin, J.X.; Lu, J.; Cao, L.L.; Lin, M.; Tu, R.H.; Huang, Z.N.; et al. Safety and Efficacy of Indocyanine Green Tracer-Guided Lymph Node Dissection during Laparoscopic Radical Gastrectomy in Patients with Gastric Cancer: A Randomized Clinical Trial. JAMA Surg. 2020, 155, 300–311. [Google Scholar] [CrossRef]
- Sposito, C.; Maspero, M.; Conalbi, V.; Magarotto, A.; Altomare, M.; Battiston, C.; Cantù, P.; Mazzaferro, V. Impact of Indocyanine Green Fluorescence Imaging on Lymphadenectomy Quality During Laparoscopic Distal Gastrectomy for Gastric Cancer (Greeneye): An Adaptative, Phase 2, Clinical Trial. Ann. Surg. Oncol. 2023, 30, 6803–6811. [Google Scholar] [CrossRef]
- Puccetti, F.; Cinelli, L.; Genova, L.; Battaglia, S.; Barbieri, L.A.; Treppiedi, E.; Cossu, A.; Elmore, U.; Rosati, R. Applicative Limitations of Indocyanine Green Fluorescence Assistance to Laparoscopic Lymph Node Dissection in Total Gastrectomy for Cancer. Ann. Surg. Oncol. 2022, 29, 5875–5882. [Google Scholar] [CrossRef]
- Lan, Y.T.; Huang, K.H.; Chen, P.H.; Liu, C.A.; Lo, S.S.; Wu, C.W.; Shyr, Y.M.; Fang, W.L. A Pilot Study of Lymph Node Mapping with Indocyanine Green in Robotic Gastrectomy for Gastric Cancer. SAGE Open Med. 2017, 5, 2050312117727444. [Google Scholar] [CrossRef]
- Cianchi, F.; Indennitate, G.; Paoli, B.; Ortolani, M.; Lami, G.; Manetti, N.; Tarantino, O.; Messeri, S.; Foppa, C.; Badii, B.; et al. The Clinical Value of Fluorescent Lymphography with Indocyanine Green During Robotic Surgery for Gastric Cancer: A Matched Cohort Study. J. Gastrointest. Surg. 2019, 24, 2197–2203. [Google Scholar] [CrossRef] [PubMed]
- Dong, B.; Zhang, A.; Zhang, Y.; Ye, W.; Liao, L.; Li, Z. Efficacy of Indocyanine Green Fluorescence Imaging-Guided Lymphadenectomy in Radical Gastrectomy for Gastric Cancer: A Systematic Review and Meta-Analysis. Front. Oncol. 2022, 12, 998159. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Goossen, K.; Tenckhoff, S.; Probst, P.; Grummich, K.; Mihaljevic, A.L.; Büchler, M.W.; Diener, M.K. Optimal Literature Search for Systematic Reviews in Surgery. Langenbecks Arch. Surg. 2018, 403, 119–129. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C. The Cochrane Collaboration’s Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A Tool for Assessing Risk of Bias in Non-Randomised Studies of Interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef]
- McGuinness, L.A.; Higgins, J.P.T. Risk-of-Bias VISualization (Robvis): An R Package and Shiny Web App for Visualizing Risk-of-Bias Assessments. Res. Synth. Methods 2021, 12, 55–61. [Google Scholar] [CrossRef]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.E.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schünemann, H.J. GRADE: An Emerging Consensus on Rating Quality of Evidence and Strength of Recommendations. BMJ 2008, 336, 924–926. [Google Scholar] [CrossRef]
- Schünemann, H.J.; Oxman, A.D.; Brozek, J.; Glasziou, P.; Jaeschke, R.; Vist, G.E.; Williams, J.W.; Kunz, R.; Craig, J.; Montori, V.M.; et al. Grading quality of evidence and strength of recommendations for diagnostic tests and strategies. BMJ 2008, 336, 1106–1110. [Google Scholar] [CrossRef]
- Royston, P.; Parmar, M.K. Parmar Restricted Mean Survival Time: An Alternative to the Hazard Ratio for the Design and Analysis of Randomized Trials with a Time-to-Event Outcome. BMC Med. Res. Methodol. 2013, 13, 152. [Google Scholar] [CrossRef]
- Jackson, D.; White, I.R.; Riley, R.D. A Matrix-Based Method of Moments for Fitting the Multivariate Random Effects Model for Meta-Analysis and Meta-Regression. Biom. J. 2013, 55, 231–245. [Google Scholar] [CrossRef] [PubMed]
- Guyot, P.; Ades, A.E.; Ouwens, M.J.N.M.; Welton, N.J. Enhanced Secondary Analysis of Survival Data: Reconstructing the Data from Published Kaplan-Meier Survival Curves. BMC Med. Res. Methodol. 2012, 12, 9. [Google Scholar] [CrossRef] [PubMed]
- Charvat, H.; Belot, A. Mexhaz: An r Package for Fitting Flexible Hazard-Based Regression Models for Overall and Excess Mortality with a Random Effect. J. Stat. Softw. 2021, 98, 1–36. [Google Scholar] [CrossRef]
- Dersimonian, R.; Laird, N. Meta-Analysis in Clinical Trials. Control Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Aiolfi, A.; Bona, D.; Riva, C.G.; Micheletto, G.; Rausa, E.; Campanelli, G.; Olmo, G.; Bonitta, G.; Bonavina, L. Systematic Review and Bayesian Network Meta-Analysis Comparing Laparoscopic Heller Myotomy, Pneumatic Dilatation, and Peroral Endoscopic Myotomy for Esophageal Achalasia. J. Laparoendosc. Adv. Surg. Tech. 2020, 30, 147–155. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring Inconsistency in Meta-Analyses Testing for Heterogeneity. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.T.; Rothstein, H.R. A Basic Introduction to Fixed-Effect and Random-Effects Models for Meta-Analysis. Res. Synth. Methods 2010, 1, 97–111. [Google Scholar] [CrossRef]
- Bona, D.; Micheletto, G.; Bonitta, G.; Panizzo, V.; Cavalli, M.; Rausa, E.; Cirri, S.; Aiolfi, A. Does C-Reactive Protein Have a Predictive Role in the Early Diagnosis of Postoperative Complications After Bariatric Surgery? Systematic Review and Bayesian Meta-Analysis. Obes. Surg. 2019, 29, 3448–3456. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2023. [Google Scholar]
- Wei, M.; Liang, Y.; Wang, L.; Li, Z.; Chen, Y.; Yan, Z.; Sun, D.; Huang, Y.; Zhong, X.; Liu, P.; et al. Clinical Application of Indocyanine Green Fluorescence Technology in Laparoscopic Radical Gastrectomy. Front. Oncol. 2022, 12, 847341. [Google Scholar] [CrossRef]
- Chen, Q.Y.; Zhong, Q.; Liu, Z.Y.; Li, P.; Lin, G.T.; Zheng, Q.L.; Bin Wang, J.; Lin, J.X.; Lu, J.; Cao, L.L.; et al. Indocyanine Green Fluorescence Imaging-Guided versus Conventional Laparoscopic Lymphadenectomy for Gastric Cancer: Long-Term Outcomes of a Phase 3 Randomised Clinical Trial. Nat. Commun. 2023, 14, 7413. [Google Scholar] [CrossRef]
- Kim, K.Y.; Hwang, J.; Park, S.H.; Cho, M.; Kim, Y.M.; Il Kim, H.; Hyung, W.J. Superior Lymph Node Harvest by Fluorescent Lymphography during Minimally Invasive Gastrectomy for Gastric Cancer Patients with High Body Mass Index. Gastric Cancer 2024, 27, 622–634. [Google Scholar] [CrossRef] [PubMed]
- Aiolfi, A.; Lombardo, F.; Matsushima, K.; Sozzi, A.; Cavalli, M.; Panizzo, V.; Bonitta, G.; Bona, D. Systematic Review and Updated Network Meta-Analysis of Randomized Controlled Trials Comparing Open, Laparoscopic-Assisted, and Robotic Distal Gastrectomy for Early and Locally Advanced Gastric Cancer. Surgery 2021, 170, 942–951. [Google Scholar] [CrossRef] [PubMed]
- Manara, M.; Aiolfi, A.; Bonitta, G.; Schlanger, D.; Popa, C.; Lombardo, F.; Manfredini, L.; Biondi, A.; Bonavina, L.; Bona, D. Short-Term Outcomes Analysis Comparing Open, Lap-Assisted, Totally Laparoscopic, and Robotic Total Gastrectomy for Gastric Cancer: A Network Meta-Analysis. Cancers 2024, 16, 340. [Google Scholar] [CrossRef]
- Hartgritik, H.H.; Van De Velde, C.J.H.; Putter, H.; Bonenkamp, J.J.; Kranenbarg, E.K.; Songun, I.; Welvaart, K.; Van Krieken, J.H.J.M.; Meijer, S.; Plukker, J.T.M.; et al. Extended Lymph Node Dissection for Gastric Cancer: Who May Benefit? Final Results of the Randomized Dutch Gastric Cancer Group Trial. J. Clin. Oncol. 2004, 22, 2069–2077. [Google Scholar] [CrossRef]
- Degiuli, M.; Sasako, M.; Ponti, A.; Vendrame, A.; Tomatis, M.; Mazza, C.; Borasi, A.; Capussotti, L.; Fronda, G.; Morino, M. Randomized Clinical Trial Comparing Survival after D1 or D2 Gastrectomy for Gastric Cancer. Br. J. Surg. 2014, 101, 23–31. [Google Scholar] [CrossRef]
- Wu, C.W.; Hsiung, C.A.; Lo, S.S.; Hsieh, M.C.; Shia, L.T.; Whang-Peng, J. Randomized Clinical Trial of Morbidity after D1 and D3 Surgery for Gastric Cancer. Br. J. Surg. 2004, 91, 283–287. [Google Scholar] [CrossRef]
- McCulloch, P.; Niita, M.E.; Kazi, H.; Gama-Rodrigues, J.J. Gastrectomy with Extended Lymphadenectomy for Primary Treatment of Gastric Cancer. Br. J. Surg. 2005, 92, 5–13. [Google Scholar] [CrossRef]
- Seevaratnam, R.; Bocicariu, A.; Cardoso, R.; Mahar, A.; Kiss, A.; Helyer, L.; Law, C.; Coburn, N. A Meta-Analysis of D1 versus D2 Lymph Node Dissection. Gastric Cancer 2012, 15, 60–69. [Google Scholar] [CrossRef]
- Mocellin, S.; Nitti, D. Lymphadenectomy Extent and Survival of Patients with Gastric Carcinoma: A Systematic Review and Meta-Analysis of Time-to-Event Data from Randomized Trials. Cancer Treat. Rev. 2015, 41, 448–454. [Google Scholar] [CrossRef]
- Mocellin, S.; Mcculloch, P.; Kazi, H.; Gama-Rodrigues, J.J.; Yuan, Y.; Nitti, D. Extent of Lymph Node Dissection for Adenocarcinoma of the Stomach. Cochrane Database Syst. Rev. 2015, 2015, CD001964. [Google Scholar] [CrossRef]
- El-Sedfy, A.; Dixon, M.; Seevaratnam, R.; Bocicariu, A.; Cardoso, R.; Mahar, A.; Kiss, A.; Helyer, L.; Law, C.; Coburn, N.G. Personalized Surgery for Gastric Adenocarcinoma: A Meta-Analysis of D1 versus D2 Lymphadenectomy. Ann. Surg. Oncol. 2015, 22, 1820–1827. [Google Scholar] [CrossRef] [PubMed]
- Robertson, C.S.; Chung, S.C.S.; Woods, S.D.S.; Griffin, S.M.; Raimes, S.A.; Lau, J.T.F.; Li, A.K.C. A Prospective Randomized Trial Comparing R1 Subtotal Gastrectomy with R3 Total Gastrectomy for Antral Cancer. Ann. Surg. 1994, 220, 176–182. [Google Scholar] [CrossRef] [PubMed]
- Surgical Co-operative Group; Cuschieri, A.; Weeden, S.; Fielding, J.; Bancewicz, J.; Craven, J.; Joypaul, V.; Sydes, M.; Fayers, P. Patient Survival after D1 and D2 Resections for Gastric Cancer: Long-Term Results of the MRC Randomized Surgical Trial. Br. J. Cancer 1999, 79, 1522–1530. [Google Scholar] [CrossRef]
- Degiuli, M.; Reddavid, R.; Tomatis, M.; Ponti, A.; Morino, M.; Sasako, M.; Rebecchi, F.; Garino, M.; Vigano, L.; Scaglione, D.; et al. D2 Dissection Improves Disease-Specific Survival in Advanced Gastric Cancer Patients: 15-Year Follow-up Results of the Italian Gastric Cancer Study Group D1 versus D2 Randomised Controlled Trial. Eur. J. Cancer 2021, 150, 10–22. [Google Scholar] [CrossRef]
- Songun, I.; Putter, H.; Kranenbarg EM, K.; Sasako, M.; van de Velde, C.J. Surgical Treatment of Gastric Cancer: 15-Year Follow-up Results of the Randomised Nationwide Dutch D1D2 Trial. Lancet Oncol. 2010, 11, 439–488. [Google Scholar] [CrossRef]
- Calì, M.; Bona, D.; Kim, Y.M.; Hyung, W.; Cammarata, F.; Bonitta, G.; Bonavina, L.; Aiolfi, A. Effect of Minimally Invasive versus Open Distal Gastrectomy on Long-Term Survival in Patients with Gastric Cancer: Individual Patient Data Meta-Analysis. Ann. Surg. Oncol. 2024, 32, 2161–2171. [Google Scholar] [CrossRef]
- Aiolfi, A.; Calì, M.; Cammarata, F.; Grasso, F.; Bonitta, G.; Biondi, A.; Bonavina, L.; Bona, D. Minimally Invasive Versus Open Distal Gastrectomy for Locally Advanced Gastric Cancer: Trial Sequential Analysis of Randomized Trials. Cancers 2024, 16, 4098. [Google Scholar] [CrossRef]
- Gathje, J.; Steuer, R.R.; K Nicholes, K.R.; Clinic, M.; Fuundutiun, M.; Karl Nicholes, A.R. Stability studies on indocyanine green dye. J. Appl. Physiol. 1970, 29, 181–185. [Google Scholar] [CrossRef]
- Kim, Y.-W.; Min, J.-S.; Man Yoon, H.; Yeong An, J.; Wool Eom, B.; Hur, H.; Joon Lee, Y.; Seok Cho, G.; Park, Y.-K.; Ran Jung, M.; et al. Laparoscopic Sentinel Node Navigation Surgery for Stomach Preservation in Patients with Early Gastric Cancer: A Randomized Clinical Trial. J. Clin. Oncol. 2022, 40, 2342–2351. [Google Scholar] [CrossRef]
- Kim, D.W.; Jeong, B.; Shin, I.H.; Kang, U.; Lee, Y.; Park, Y.S.; Ahn, S.H.; Park, D.J.; Kim, H.H. Sentinel Node Navigation Surgery Using Near-Infrared Indocyanine Green Fluorescence in Early Gastric Cancer. Surg. Endosc. 2019, 33, 1235–1243. [Google Scholar] [CrossRef]
- Cho, M.; Kim, K.Y.; Park, S.H.; Kim, Y.M.; Il Kim, H.; Hyung, W.J. Securing Resection Margin Using Indocyanine Green Diffusion Range on Gastric Wall during NIR Fluorescence-Guided Surgery in Early Gastric Cancer Patients. Cancers 2022, 14, 5223. [Google Scholar] [CrossRef] [PubMed]
- Park, S.H.; Kim, K.Y.; Cho, M.; Kim, Y.M.; Il Kim, H.; Hyung, W.J. Prognostic Impact of Fluorescent Lymphography on Gastric Cancer. Int. J. Surg. 2023, 109, 2926–2933. [Google Scholar] [CrossRef] [PubMed]
- Japanese Gastric Cancer Association. Japanese Gastric Cancer Treatment Guidelines 2021. Gastric Cancer 2023, 26, 1–25. [Google Scholar] [CrossRef]
- Lu, J.; Wang, W.; Zheng, C.H.; Fang, C.; Li, P.; Xie, J.W.; Wang, J.B.; Lin, J.X.; Chen, Q.Y.; Cao, L.L.; et al. Influence of Total Lymph Node Count on Staging and Survival After Gastrectomy for Gastric Cancer: An Analysis From a Two-Institution Database in China. Ann. Surg. Oncol. 2017, 24, 486–493. [Google Scholar] [CrossRef]
- Jeon, C.H.; Park, K.B.; Lee, H.; Kim, D.J.; Seo, H.S.; Lee, J.; Jun, K.H.; Kim, J.J.; Lee, H.H. Refining Gastric Cancer Staging: Examining the Interplay between Number and Anatomical Location of Metastatic Lymph Nodes—A Retrospective Multi-Institutional Study. BMC Cancer 2023, 23, 1192. [Google Scholar] [CrossRef]
- Shinohara, H.; Kurahashi, Y.; Kanaya, S.; Haruta, S.; Ueno, M.; Udagawa, H.; Sakai, Y. Topographic Anatomy and Laparoscopic Technique for Dissection of No. 6 Infrapyloric Lymph Nodes in Gastric Cancer Surgery. Gastric Cancer 2013, 16, 615–620. [Google Scholar] [CrossRef]
- Potthoff, K.; Dechow, T.; Lorenzen, S.; Reinacher-Schick, A.; Binninger, A.; Matillon, C.; Siebenbach, H.-U.; Haffner, I.; Hacker, U.; Bläker, H.; et al. SAPHIR: Real-World Clinical Research Platform for Molecular Testing, Treatment, and Clinical and Patient-Reported Outcomes in Patients with Gastroesophageal Cancer in Germany. ESMO Real. World Data Digit. Oncol. 2023, 2, 100007. [Google Scholar] [CrossRef]
- Wadhwa, R.; Song, S.; Lee, J.S.; Yao, Y.; Wei, Q.; Ajani, J.A. Gastric Cancer—Molecular and Clinical Dimensions. Nat. Rev. Clin. Oncol. 2013, 10, 643–655. [Google Scholar] [CrossRef]
- Yeoh, K.G.; Tan, P. Mapping the Genomic Diaspora of Gastric Cancer. Nat. Rev. Cancer 2022, 22, 71–84. [Google Scholar] [CrossRef]
- Choi, E.; Shin, J.; Ryu, M.H.; Kim, H.D.; Park, Y.S. Heterogeneity of Claudin 18.2 Expression in Metastatic Gastric Cancer. Sci. Rep. 2024, 14, 17648. [Google Scholar] [CrossRef]
- Mathias-Machado, M.C.; de Jesus, V.H.F.; Jácome, A.; Donadio, M.D.; Aruquipa, M.P.S.; Fogacci, J.; Cunha, R.G.; da Silva, L.M.; Peixoto, R.D. Claudin 18.2 as a New Biomarker in Gastric Cancer—What Should We Know? Cancers 2024, 16, 679. [Google Scholar] [CrossRef] [PubMed]
- Zhou, D.; Quan, Z.; Wang, J.; Zhao, M.; Yang, Y. Laparoscopic-Assisted versus Open Distal Gastrectomy with D2 Lymph Node Resection for Advanced Gastric Cancer: Effect of Learning Curve on Short-Term Outcomes. a Meta-Analysis. J. Laparoendosc. Adv. Surg. Tech. 2014, 24, 139–150. [Google Scholar] [CrossRef] [PubMed]
- Yu, W.; Yun, Y.K.; Whang, I.; Choi, G.S. The Surgeon’s Expertise-Outcome Relationship in Gastric Cancer Surgery. Cancer Res. Treat. Off. J. Korean Cancer Assoc. 2005, 37, 143–147. [Google Scholar] [CrossRef] [PubMed]
- Asplund, J.; Mattsson, F.; Plecka-Östlund, M.; Markar, S.R.; Lagergren, J. Annual Surgeon and Hospital Volume of Gastrectomy and Gastric Adenocarcinoma Survival in a Population-Based Cohort Study. Acta Oncol. 2022, 61, 425–432. [Google Scholar] [CrossRef]
- Aiolfi, A.; Bona, D.; Calì, M.; Manara, M.; Rausa, E.; Bonitta, G.; Elshafei, M.; Markar, S.R.; Bonavina, L. Does Thoracic Duct Ligation at the Time of Esophagectomy Impact Long-Term Survival? An Individual Patient Data Meta-Analysis. J. Clin. Med. 2024, 13, 2849. [Google Scholar] [CrossRef]
- Aiolfi, A.; Sozzi, A.; Bonitta, G.; Lombardo, F.; Cavalli, M.; Campanelli, G.; Bonavina, L.; Bona, D. Short-Term Outcomes of Different Esophagojejunal Anastomotic Techniques during Laparoscopic Total Gastrectomy: A Network Meta-Analysis. Surg. Endosc. 2023, 37, 5777–5790. [Google Scholar] [CrossRef]
| Author, Country, Year | Study Period | Study Design | Group | No. Pts | Age (yrs) | Gender (M) | BMI (kg/m2) | Surgical Procedure (DG/TG/PG) | Staging System | Tumor Location | Extent of Lymphadenectomy | Metastatic LNs | Total No. LNs |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wei et al., China, 2022 [40] | January 2018–August 2019 | Ret | ICG | 107 | 59.3 ± 8.9 | 57/50 | 24.6 ± 3.4 | 59/48/0 | AJCC 8th | nr | D2 | 6.4 ± 10.9 | 49.5 ± 12.7 |
| no-ICG | 88 | 61.5 ± 10.3 | 48/40 | 24.9 ± 2.6 | 41/47/0 | 3.3 ± 6.4 | 44.4 ± 10.2 | ||||||
| Chen et al., China, 2023 [41] | November 2018–July 2019 | RCT | ICG | 129 | 57.8 (10.7) | 86/43 | 23.2 (3.2) | nr | AJCC 7th | 33F/21B/75A | D2 | 5.6 (11.2) | 50.5 (15.9) |
| no-ICG | 129 | 60.1 (9.1) | 87/42 | 22.8 (3.1) | 66F/14B/49A | 5.7 (8.9) | 42.0 (10.3) | ||||||
| Kim et al., South Korea, 2024 [42] | January 2013–December 2021 | Ret IPTW | ICG | 2397 | 59.8 (12.3) | 1409/988 | 23.6 (3.1) | 1948/276/172 | nr | 303F/757B/1316A/27EGJ | 1650 D1+ 747 D2 | nr | 48.4 (18.5) |
| no-ICG | 3475 | 59.5 (12.3) | 1979/1496 | 23.6 (3.1) | 2828/407/239 | 434F/1080B/ 1924A/37EGJ | 2350 D1+ 1125 D2 | nr | 39.8 (16.3) |
| Time Horizon | No. Studies | RMSTD (mos) | 95% CI | p Value |
|---|---|---|---|---|
| 12 months | 3 | 0.1 | −0.20, 0.39 | 0.51 |
| 24 months | 3 | 0.2 | −0.14, 0.63 | 0.21 |
| 36 months | 3 | 0.4 | −0.01, 0.87 | 0.06 |
| 42 months | 3 | 0.5 | −0.01, 1.1 | 0.05 |
| Time Horizon | No. Studies | RMSTD (mos) | 95% CI | p Value |
|---|---|---|---|---|
| 12 months | 3 | 0.1 | 0.03, 0.15 | 0.002 |
| 24 months | 3 | 0.5 | 0.18, 0.85 | 0.002 |
| 36 months | 3 | 1 | 0.32, 1.72 | 0.004 |
| 42 months | 3 | 1.3 | 0.39, 2.15 | 0.004 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Calì, M.; Aiolfi, A.; Sato, S.; Hwang, J.; Bonitta, G.; Albanesi, F.; Bonavina, G.; Cavalli, M.; Campanelli, G.; Biondi, A.; et al. Effect of Indocyanine Green-Guided Lymphadenectomy During Gastrectomy on Survival: Individual Patient Data Meta-Analysis. Cancers 2025, 17, 980. https://doi.org/10.3390/cancers17060980
Calì M, Aiolfi A, Sato S, Hwang J, Bonitta G, Albanesi F, Bonavina G, Cavalli M, Campanelli G, Biondi A, et al. Effect of Indocyanine Green-Guided Lymphadenectomy During Gastrectomy on Survival: Individual Patient Data Meta-Analysis. Cancers. 2025; 17(6):980. https://doi.org/10.3390/cancers17060980
Chicago/Turabian StyleCalì, Matteo, Alberto Aiolfi, Sho Sato, Jawon Hwang, Gianluca Bonitta, Francesca Albanesi, Giulia Bonavina, Marta Cavalli, Giampiero Campanelli, Antonio Biondi, and et al. 2025. "Effect of Indocyanine Green-Guided Lymphadenectomy During Gastrectomy on Survival: Individual Patient Data Meta-Analysis" Cancers 17, no. 6: 980. https://doi.org/10.3390/cancers17060980
APA StyleCalì, M., Aiolfi, A., Sato, S., Hwang, J., Bonitta, G., Albanesi, F., Bonavina, G., Cavalli, M., Campanelli, G., Biondi, A., Bonavina, L., & Bona, D. (2025). Effect of Indocyanine Green-Guided Lymphadenectomy During Gastrectomy on Survival: Individual Patient Data Meta-Analysis. Cancers, 17(6), 980. https://doi.org/10.3390/cancers17060980











