Daylight Photodynamic Therapy for Actinic Keratosis and Field Cancerization: A Narrative Review
Simple Summary
Abstract
1. Introduction
| Treatment Type | Treatment Modality | Mechanism of Action | Application | Indication |
|---|---|---|---|---|
| Lesion-Directed Treatments | Cryotherapy | Induces cellular necrosis through rapid freezing of the lesion | Liquid nitrogen applied directly to lesion | Isolated, well-demarcated AK lesions |
| Surgical Excision | Complete excision of the lesion with scalpel or surgical instrument | Direct surgical removal of lesion | Thick, hypertrophic, or clinically suspicious AK | |
| Curettage and Electrodessication | Physical scraping followed by electrocautery to eliminate abnormal keratinocytes | Curette scraping followed by electrocautery | Hypertrophic or hyperkeratotic AK lesions | |
| Ablative Laser Therapy | Utilizes ablative laser to vaporize and remove AK lesions | CO2 or Er:YAG laser applied directly | Localized AK lesions or cosmetic concerns | |
| Field-Directed Treatments | 5-FU | Inhibits DNA synthesis and induces apoptosis in abnormal keratinocytes | Topical cream applied to affected areas | Multiple AK lesions or areas with field cancerization |
| Imiquimod | Modulates the immune system to enhance the immune-mediated clearance of AK lesions | Topical cream applied 2–3 times per week | Multiple AK lesions or field cancerization | |
| Diclofenac (NSAID Gel) | Inhibits COX-2, leading to apoptosis of AK cells | Topical gel applied twice daily | Mild to moderate AK lesions | |
| Tirbanibulin | Inhibits microtubule polymerization, inducing selective apoptosis of AK cells | Topical ointment applied once daily for 5 consecutive days | Mild AK lesions on the face and scalp | |
| cPDT | Photosensitization of keratinocytes through a photosensitizing agent, followed by light exposure to generate ROS. | Topical application of MAL or ALA followed by light activation | Multiple AK lesions and field cancerization | |
| dPDT | Utilizes natural sunlight to activate the photosensitizing agent, inducing apoptosis through ROS generation | Topical application of MAL or ALA followed by 1–2 h of sun exposure | Extensive AK lesions or field cancerization with reduced pain |
| Adverse Events | Description | Frequency |
|---|---|---|
| Pain, erythema, pruritus, crusting/scaling | Severe pain may occur in a significant proportion of patients, redness, scabbing | Common |
| Dyschromia, photosensitivity reaction | Skin darkening or lightening, delayed sunburn-like reaction | Uncommon |
| Infection, erosion, ulceration, edema | Secondary bacterial infection, skin breakdown, swelling | Rare |
2. Methodology
3. Review of the dPDT Procedure
| Aspect | Daylight PDT (dPDT) | Conventional PDT (cPDT) |
|---|---|---|
| Efficacy | Effective for non-hyperkeratotic AK and field cancerization. | Effective for non-hyperkeratotic AK and field cancerization. |
| Pain and Tolerability | Much less painful due to gradual activation of photosensitizer. | Often painful due to rapid activation with intense light. |
| Cosmetic Outcome | Excellent, with minimal inflammation and scarring. | Also good, but potential for more post-treatment erythema and irritation. |
| Convenience | No need for artificial light sources; can be performed outdoors. | Requires a specialized light source and clinical setup. |
| Treatment Setting | Can be performed outside or indoors near windows. | Requires a clinical setting with trained personnel. |
| Weather Dependence | Dependent on sufficient daylight (not ideal for cloudy/rainy days). | Independent of weather conditions. |
| Cost and Equipment | More cost-effective (no expensive light source required). | Higher costs due to specialized light equipment and clinical visits. |
| Treatment Time | Longer exposure (2 h outdoors), but shorter clinic time. | Shorter exposure (7–10 min per lesion) but longer clinic visits. |
| Patient Compliance | Easier for patients due to minimal pain and fewer clinic visits. | Compliance may be lower due to pain and frequent clinic visits. |
| Adverse Effects | Milder side effects (low pain, mild erythema, some scaling). | More erythema, swelling, crusting, and pain post-treatment. |
| Recurrences | Comparable efficacy in mild-to-moderate AK, good for field cancerization. | Potentially better for thicker AKs but with higher local inflammation. |
| Adverse Events | Description | Frequency |
|---|---|---|
| Pain, erythema, pruritus, crusting/scaling | Mild to moderate burning or itching, redness, scabbing | Common |
| Dyschromia, photosensitivity reaction | Skin darkening or lightening, delayed sunburn-like reaction | Uncommon |
| Infection, erosion, ulceration | Secondary bacterial infection, skin breakdown | Rare |
4. Review of Current Evidence
4.1. Comparison of dPDT with cPDT
4.2. Comparison of dPDT with Other Treatments Modalities and Combinations of Treatments
4.3. Significance of Field Cancerization Treatment
5. Discussion
6. Limitations of the Review
7. Suggestions for Future Research
8. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Figueras Nart, I.; Cerio, R.; Dirschka, T.; Dréno, B.; Lear, J.T.; Pellacani, G.; Peris, K.; Ruiz de Casas, A. Defining the actinic keratosis field: A literature review and discussion. J. Eur. Acad. Dermatol. Venereol. 2018, 32, 544–563. [Google Scholar] [CrossRef] [PubMed]
- Werner, R.N.; Sammain, A.; Erdmann, R.; Hartmann, V.; Stockfleth, E.; Nast, A. The natural history of actinic keratosis: A systematic review. Br. J. Dermatol. 2013, 169, 502–518. [Google Scholar] [CrossRef] [PubMed]
- Malvehy, J.; Stratigos, A.J.; Bagot, M.; Stockfleth, E.; Ezzedine, K.; Delarue, A. Actinic keratosis: Current challenges and unanswered questions. J. Eur. Acad. Dermatol. Venereol. 2024, 38 (Suppl. 5), 3–11. [Google Scholar] [CrossRef] [PubMed]
- Kandolf, L.; Peris, K.; Malvehy, J.; Mosterd, K.; Heppt, M.V.; Fargnoli, M.C.; Berking, C.; Arenberger, P.; Bylaite-Bučinskiene, M.; Del Marmol, V.; et al. European consensus-based interdisciplinary guideline for diagnosis, treatment and prevention of actinic keratoses, epithelial UV-induced dysplasia and field cancerization on behalf of European Association of Dermato-Oncology, European Dermatology Forum. J. Eur. Acad. Dermatol. Venereol. 2024, 38, 1024–1047. [Google Scholar] [CrossRef]
- Criscione, V.D.; Weinstock, M.A.; Naylor, M.F.; Luque, C.; Eide, M.J.; Bingham, S.F. Actinic keratoses: Natural history and risk of malignant transformation in the Veterans Affairs Topical Tretinoin Chemoprevention Trial. Cancer 2009, 115, 2523–2530. [Google Scholar] [CrossRef]
- Marks, R.; Rennie, G.; Selwood, T.S. Malignant transformation of solar keratoses to squamous cell carcinoma. Lancet 1988, 1, 795–797. [Google Scholar] [CrossRef]
- Gupta, A.K.; Paquet, M.; Villanueva, E.; Brintnell, W. Interventions for actinic keratoses. Cochrane Database Syst. Rev. 2012, 12, CD004415. [Google Scholar] [CrossRef]
- Arcuri, D.; Ramchatesingh, B.; Lagacé, F.; Iannattone, L.; Netchiporouk, E.; Lefrançois, P.; Litvinov, I.V. Pharmacological Agents Used in the Prevention and Treatment of Actinic Keratosis: A Review. Int. J. Mol. Sci. 2023, 24, 4989. [Google Scholar] [CrossRef]
- Bernal Masferrer, L.; Gracia Cazaña, T.; Bernad Alonso, I.; Álvarez-Salafranca, M.; Almenara Blasco, M.; Gallego Rentero, M.; Juarranz de la Fuente, Á.; Gilaberte, Y. Topical Immunotherapy for Actinic Keratosis and Field Cancerization. Cancers 2024, 16, 1133. [Google Scholar] [CrossRef]
- Singh, R.; Shah, M.A.; Feldman, S.R. Reasons for Patient Call-backs while being Treated with Topical 5-fluorouracil: A Retrospective Chart Review. J. Clin. Aesthet. Dermatol. 2023, 16, 53–54. [Google Scholar]
- Wiegell, S.R.; Fredman, G.; Andersen, F.; Bjerring, P.; Paasch, U.; Hædersdal, M. Pre-treatment with topical 5-fluorouracil increases the efficacy of daylight photodynamic therapy for actinic keratoses—A randomized controlled trial. Photodiagnosis Photodyn. Ther. 2024, 46, 104069. [Google Scholar] [PubMed]
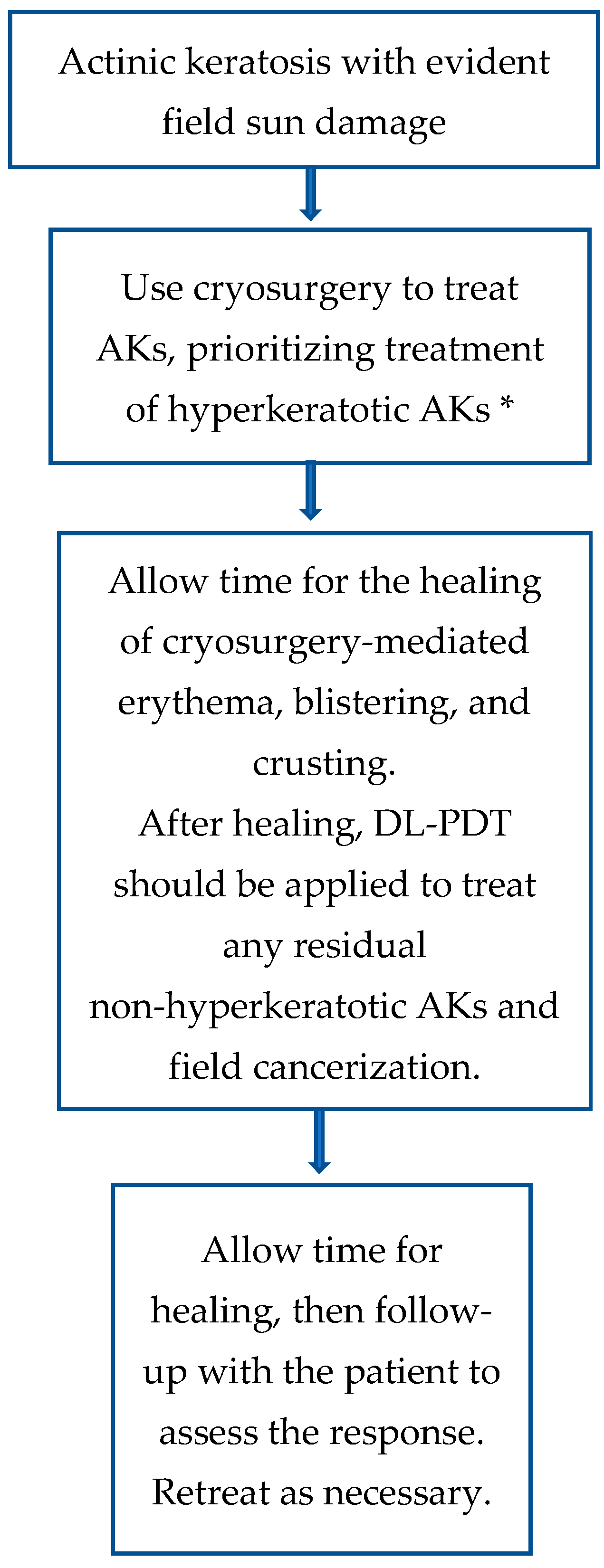
- Calzavara-Pinton, P.; Hædersdal, M.; Barber, K.; Basset-Seguin, N.; Del Pino Flores, M.E.; Foley, P.; Galimberti, G.; Gerritsen, R.; Gilaberte, Y.; Ibbotson, S.; et al. Structured Expert Consensus on Actinic Keratosis: Treatment Algorithm Focusing on Daylight PDT. J. Cutan. Med. Surg. 2017, 21 (Suppl. 1), 3S–16S. [Google Scholar] [PubMed]
- Niculescu, A.-G.; Grumezescu, A.M. Photodynamic Therapy—An Up-to-Date Review. Appl. Sci. 2021, 11, 3626. [Google Scholar] [CrossRef]
- Sotiriou, E.; Apalla, Z.; Vrani, F.; Lazaridou, E.; Vakirlis, E.; Lallas, A.; Ioannides, D. Daylight photodynamic therapy vs. Conventional photodynamic therapy as skin cancer preventive treatment in patients with face and scalp cancerization: An intra-individual comparison study. J. Eur. Acad. Dermatol. Venereol. 2017, 31, 1303–1307. [Google Scholar] [PubMed]
- Morton, C.A.; Wulf, H.C.; Szeimies, R.M.; Gilaberte, Y.; Basset-Seguin, N.; Sotiriou, E.; Piaserico, S.; Hunger, R.E.; Baharlou, S.; Sidoroff, A.; et al. Practical approach to the use of daylight photodynamic therapy with topical methyl aminolevulinate for actinic keratosis: A European consensus. J. Eur. Acad. Dermatol. Venereol. 2015, 29, 1718–1723. [Google Scholar] [CrossRef]
- Jetter, N.; Chandan, N.; Wang, S.; Tsoukas, M. Field Cancerization Therapies for Management of Actinic Keratosis: A Narrative Review. Am. J. Clin. Dermatol. 2018, 19, 543–557. [Google Scholar]
- Eisen, D.B.; Asgari, M.M.; Bennett, D.D.; Connolly, S.M.; Dellavalle, R.P.; Freeman, E.E.; Goldenberg, G.; Leffell, D.J.; Peschin, S.; Sligh, J.E.; et al. Guidelines of care for the management of actinic keratosis: Executive summary. J. Am. Acad. Dermatol. 2021, 85, 945–955. [Google Scholar]
- Bakirtzi, K.; Papadimitriou, I.; Vakirlis, E.; Lallas, A.; Sotiriou, E. Photodynamic Therapy for Field Cancerization in the Skin: Where Do We Stand? Dermatol. Pract. Concept. 2023, 13, e2023291. [Google Scholar] [CrossRef]
- Steeb, T.; Wessely, A.; Schmitz, L.; Heppt, F.; Kirchberger, M.C.; Berking, C.; Heppt, M.V. Interventions for Actinic Keratosis in Nonscalp and Nonface Localizations: Results from a Systematic Review with Network Meta-Analysis. J. Investig. Dermatol. 2021, 141, 345–354.e8. [Google Scholar]
- Lacour, J.-P.; Ulrich, C.; Gilaberte, Y.; Von Felbert, V.; Basset-Seguin, N.; Dreno, B.; Girard, C.; Redondo, P.; Serra-Guillen, C.; Synnerstad, I.; et al. Daylight photodynamic therapy with methyl aminolevulinate cream is effective and nearly painless in treating actinic keratoses: A randomised, investigator-blinded, controlled, phase III study throughout Europe. J. Eur. Acad. Dermatol. Venereol. 2015, 29, 2342–2348. [Google Scholar] [CrossRef]
- Fargnoli, M.C.; Piccioni, A.; Neri, L.; Tambone, S.; Pellegrini, C.; Peris, K. Conventional vs. daylight methyl aminolevulinate photodynamic therapy for actinic keratosis of the face and scalp: An intra-patient, prospective, comparison study in Italy. J. Eur. Acad. Dermatol. Venereol. 2015, 29, 1926–1932. [Google Scholar] [CrossRef] [PubMed]
- Zhu, L.; Wang, P.; Zhang, G.; Zhang, L.; Liu, X.; Hu, C.; Yang, X.; Sroka, R.; Zhou, Z.; Wang, X. Conventional versus daylight photodynamic therapy for actinic keratosis: A randomized and prospective study in China. Photodiagnosis Photodyn. Ther. 2018, 24, 366–371. [Google Scholar] [CrossRef] [PubMed]
- Wiegell, S.R.; Heydenreich, J.; Fabricius, S.; Wulf, H.C. Continuous ultra-low-intensity artificial daylight is not as effective as red LED light in photodynamic therapy of multiple actinic keratoses. Photodermatol. Photoimmunol. Photomed. 2011, 27, 280–285. [Google Scholar] [CrossRef] [PubMed]
- Arisi, M.; Rossi, M.T.; Spiazzi, L.; Guasco Pisani, E.; Venturuzzo, A.; Rovati, C.; Tomasi, C.; Venturini, M.; Calzavara-Pinton, P.G. A randomized split-face clinical trial of conventional vs indoor-daylight photodynamic therapy for the treatment of multiple actinic keratosis of the face and scalp and photoaging. J. Dermatol. Treat. 2022, 33, 2250–2256. [Google Scholar] [CrossRef]
- Quinlan, C.; Shutchaidat, V.; Browne, N.; Murphy, G.M. A prospective study of daylight photodynamic therapy for treatment of actinic keratoses in an Irish population. J. Am. Acad. Dermatol. 2016, 74, AB223. [Google Scholar] [CrossRef]
- Dirschka, T.; Ekanayake-Bohlig, S.; Dominicus, R.; Aschoff, R.; Herrera-Ceballos, E.; Botella-Estrada, R.; Hunfeld, A.; Kremser, M.; Schmitz, B.; Lübbert, H.; et al. A randomized, intraindividual, non-inferiority, Phase III study comparing daylight photodynamic therapy with BF-200 ALA gel and MAL cream for the treatment of actinic keratosis. J. Eur. Acad. Dermatol. Venereol. 2019, 33, 288–297. [Google Scholar] [CrossRef]
- Waters, A.J.; Ibbotson, S.H. Parameters associated with severe pain during photodynamic therapy: Results of a large Scottish series. Br. J. Dermatol. 2011, 165, 696–698. [Google Scholar] [CrossRef]
- Ibbotson, S.H.; Wong, T.H.; Morton, C.A.; Collier, N.J.; Haylett, A.; McKenna, K.E.; Mallipeddi, R.; Moseley, H.; Rhodes, L.E.; Seukeran, D.C.; et al. Adverse effects of topical photodynamic therapy: A consensus review and approach to management. Br. J. Dermatol. 2019, 180, 715–729. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Sterne, J.A.; Hernan, M.A.; Reeves, B.C.; Savovic, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef]
- Caccavale, S.; Boccellino, M.P.; Brancaccio, G.; Alfano, R.; Argenziano, G. Keratolytics can replace curettage in daylight photodynamic therapy for actinic keratosis on the face/scalp: A randomized clinical trial. J. Eur. Acad. Dermatol. Venereol. 2024, 38, 594–601. [Google Scholar] [PubMed]
- Lindholm, V.; Salmivuori, M.; Hahtola, S.; Mäkelä, K.; Pitkänen, S.; Isoherranen, K. Ablative Fractional Laser Enhances Artificial or Natural Daylight Photodynamic Therapy of Actinic Field Cancerization: A Randomized and Investigator-initiated Half-side Comparative Study. Acta Derm. Venereol. 2023, 103, adv6579. [Google Scholar] [PubMed]
- Trave, I.; Salvi, I.; Serazzi, F.A.; Schiavetti, I.; Luca, L.; Parodi, A.; Cozzani, E. The impact of occlusive vs non-occlusive application of methyl aminolevulinate on the efficacy and tolerability of daylight photodynamic therapy for actinic keratosis. Photodiagnosis Photodyn. Ther. 2024, 46, 104049. [Google Scholar] [PubMed]
- Peng, Q.; Berg, K.; Moan, J.; Kongshaug, M.; Nesland, J.M. 5-Aminolevulinic acid-based photodynamic therapy: Principles and experimental research. Photochem. Photobiol. 1997, 65, 235–251. [Google Scholar] [CrossRef]
- Austin, E.; Wang, J.Y.; Ozog, D.M.; Zeitouni, N.; Lim, H.W.; Jagdeo, J. Photodynamic Therapy: Overview and Mechanism of Action. J. Am. Acad. Dermatol. 2025, in press. [Google Scholar] [CrossRef]
- Allison, R.R.; Sibata, C.H. Photodynamic therapy: Mechanism of action and role in the treatment of skin disease. G. Ital. Dermatol. Venereol. 2010, 145, 491–507. [Google Scholar]
- Kwiatkowski, S.; Knap, B.; Przystupski, D.; Saczko, J.; Kędzierska, E.; Knap-Czop, K.; Kotlińska, J.; Michel, O.; Kotowski, K.; Kulbacka, J. Photodynamic therapy—Mechanisms, photosensitizers and combinations. Biomed. Pharmacother. 2018, 106, 1098–1107. [Google Scholar] [CrossRef]
- Evangelou, G.; Farrar, M.D.; Cotterell, L.; Andrew, S.; Tosca, A.D.; Watson, R.E.B.; Rhodes, L.E. Topical photodynamic therapy significantly reduces epidermal Langerhans cells during clinical treatment of basal cell carcinoma. Br. J. Dermatol. 2012, 166, 1112–1115. [Google Scholar] [CrossRef]
- Wiegell, S.R.; Haedersdal, M.; Philipsen, P.A.; Eriksen, P.; Enk, C.D.; Wulf, H.C. Continuous activation of PpIX by daylight is as effective as and less painful than conventional photodynamic therapy for actinic keratoses; a randomized, controlled, single-blinded study. Br. J. Dermatol. 2008, 158, 740–746. [Google Scholar]
- Tyrrell, J.; Paterson, C.; Curnow, A. Regression Analysis of Protoporphyrin IX Measurements Obtained During Dermatological Photodynamic Therapy. Cancers 2019, 11, 72. [Google Scholar] [CrossRef]
- Ruiz, A.J.; LaRochelle, E.P.M.; Gunn, J.R.; Hull, S.M.; Hasan, T.; Chapman, M.S.; Pogue, B.W. Smartphone fluorescence imager for quantitative dosimetry of protoporphyrin-IX-based photodynamic therapy in skin. J. Biomed. Opt. 2019, 25, 063802. [Google Scholar]
- Karrer, S.; Szeimies, R.-M.; Philipp-Dormston, W.G.; Gerber, P.A.; Prager, W.; Datz, E.; Zeman, F.; Müller, K.; Koller, M. Repetitive Daylight Photodynamic Therapy versus Cryosurgery for Prevention of Actinic Keratoses in Photodamaged Facial Skin: A Prospective, Randomized Controlled Multicentre Two-armed Study. Acta Derm. Venereol. 2021, 101, adv00355. [Google Scholar] [PubMed]
- Fredman, G.; Jacobsen, K.; Philipsen, P.A.; Wiegell, S.R.; Haedersdal, M. Prebiotic and panthenol-containing dermocosmetic improves tolerance from daylight photodynamic therapy: A randomized controlled trial in patients with actinic keratosis. Photodiagnosis Photodyn. Ther. 2024, 50, 104394. [Google Scholar] [PubMed]
- Assikar, S.; Labrunie, A.; Kerob, D.; Couraud, A.; Bédane, C. Daylight photodynamic therapy with methyl aminolevulinate cream is as effective as conventional photodynamic therapy with blue light in the treatment of actinic keratosis: A controlled randomized intra-individual study. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 1730–1735. [Google Scholar]
- Fargnoli, M.C.; Piccioni, A.; Neri, L.; Tambone, S.; Pellegrini, C.; Peris, K. Long-term efficacy and safety of daylight photodynamic therapy with methyl amninolevulinate for actinic keratosis of the face and scalp. Eur. J. Dermatol. 2017, 27, 89–91. [Google Scholar]
- Rubel, D.M.; Spelman, L.; Murrell, D.F.; See, J.-A.; Hewitt, D.; Foley, P.; Bosc, C.; Kerob, D.; Kerrouche, N.; Wulf, H.C.; et al. Daylight photodynamic therapy with methyl aminolevulinate cream as a convenient, similarly effective, nearly painless alternative to conventional photodynamic therapy in actinic keratosis treatment: A randomized controlled trial. Br. J. Dermatol. 2014, 171, 1164–1171. [Google Scholar]
- Ruiz, A.J.; LaRochelle, E.P.M.; Fahrner, M.-C.P.; Emond, J.A.; Samkoe, K.S.; Pogue, B.W.; Chapman, M.S. Equivalent efficacy of indoor daylight and lamp-based 5-aminolevulinic acid photodynamic therapy for treatment of actinic keratosis. Ski. Health Dis. 2023, 3, e226. [Google Scholar] [CrossRef]
- Sotiriou, E.; Evangelou, G.; Papadavid, E.; Apalla, Z.; Vrani, F.; Vakirlis, E.; Panagiotou, M.; Stefanidou, M.; Pombou, T.; Krasagakis, K.; et al. Conventional vs. daylight photodynamic therapy for patients with actinic keratosis on face and scalp: 12-month follow-up results of a randomized, intra-individual comparative analysis. J. Eur. Acad. Dermatol. Venereol. 2018, 32, 595–600. [Google Scholar] [CrossRef]
- Togsverd-Bo, K.; Lei, U.; Erlendsson, A.M.; Taudorf, E.H.; Philipsen, P.A.; Wulf, H.C.; Skov, L.; Hædersdal, M. Combination of ablative fractional laser and daylight-mediated photodynamic therapy for actinic keratosis in organ transplant recipients—A randomized controlled trial. Br. J. Dermatol. 2015, 172, 467–474. [Google Scholar]
- Galimberti, G.N. Daylight Photodynamic Therapy Versus 5-Fluorouracil for the Treatment of Actinic Keratosis: A Case Series. Dermatol. Ther. 2018, 8, 137–141. [Google Scholar]
- Wiegell, S.R.; Fredman, G.; Andersen, F.; Bjerring, P.; Paasch, U.; Haedersdal, M. Is the benefit of sequential 5-fluorouracil and daylight photodynamic therapy versus daylight photodynamic therapy alone sustained over time?—12-month follow-up of a randomized controlled trial. Photodiagnosis Photodyn. Ther. 2025, 51, 104445. [Google Scholar] [PubMed]
- Nissen, C.V.; Heerfordt, I.M.; Wiegell, S.R.; Mikkelsen, C.S.; Wulf, H.C. Pretreatment with 5-Fluorouracil Cream Enhances the Efficacy of Daylight-mediated Photodynamic Therapy for Actinic Keratosis. Acta Derm. Venereol. 2017, 97, 617–621. [Google Scholar] [CrossRef] [PubMed]
- Piaserico, S.; Piccioni, A.; Gutiérrez Garcìa-Rodrigo, C.; Sacco, G.; Pellegrini, C.; Fargnoli, M.C. Sequential treatment with calcitriol and methyl aminolevulinate-daylight photodynamic therapy for patients with multiple actinic keratoses of the upper extremities. Photodiagnosis Photodyn. Ther. 2021, 34, 102325. [Google Scholar] [PubMed]
- Singh, R.; McCain, S.; Feldman, S.R. Refusal of Retreatment With Topical 5-Fluorouracil Among Patients With Actinic Keratosis: Qualitative Analysis. JMIR Dermatol. 2023, 6, e39988. [Google Scholar]
- Emmerich, V.K.; Cull, D.; Kelly, K.A.; Feldman, S.R. Patient assessment of 5-fluorouracil and imiquimod for the treatment of actinic keratoses: A retrospective study of real-world effectiveness. J. Dermatol. Treat. 2022, 33, 2075–2078. [Google Scholar]
- Vale, S.M.; Hill, D.; Feldman, S.R. Pharmacoeconomic Considerations in Treating Actinic Keratosis: An Update. Pharmacoeconomics 2017, 35, 177–190. [Google Scholar]
- Philipp-Dormston, W.G.; Brückner, M.; Hoffmann, M.; Baé, M.; Fränken, J.; Großmann, B.; Paasch, U.; Quist, S.; Lang, B.M.; Chavda, R.; et al. Artificial daylight photodynamic therapy using methyl aminolevulinate in a real-world setting in Germany—Results from the non-interventional study ArtLight. Br. J. Dermatol. 2024, 192, 510–519. [Google Scholar]
- See, J.-A.; Gebauer, K.; Wu, J.K.; Manoharan, S.; Kerrouche, N.; Sullivan, J. High Patient Satisfaction with Daylight-Activated Methyl Aminolevulinate Cream in the Treatment of Multiple Actinic Keratoses: Results of an Observational Study in Australia. Dermatol. Ther. 2017, 7, 525–533. [Google Scholar]
- Lang, B.M.; Zielbauer, S.; Stege, H.; Grabbe, S.; Staubach, P. If patients had a choice—Treatment satisfaction and patients’ preference in therapy of actinic keratoses. JDDG J. Dtsch. Dermatol. Ges. 2024, 22, 1362–1368. [Google Scholar]
- Neittaanmäki-Perttu, N.; Grönroos, M.; Karppinen, T.; Snellman, E.; Rissanen, P. Photodynamic Therapy for Actinic Keratoses: A Randomized Prospective Non-sponsored Cost-effectiveness Study of Daylight-mediated Treatment Compared with Light-emitting Diode Treatment. Acta Derm. Venereol. 2016, 96, 241–244. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sotiriou, E.; Kiritsi, D.; Chaitidis, N.; Arabatzis, M.; Lallas, A.; Vakirlis, E. Daylight Photodynamic Therapy for Actinic Keratosis and Field Cancerization: A Narrative Review. Cancers 2025, 17, 1050. https://doi.org/10.3390/cancers17061050
Sotiriou E, Kiritsi D, Chaitidis N, Arabatzis M, Lallas A, Vakirlis E. Daylight Photodynamic Therapy for Actinic Keratosis and Field Cancerization: A Narrative Review. Cancers. 2025; 17(6):1050. https://doi.org/10.3390/cancers17061050
Chicago/Turabian StyleSotiriou, Elena, Dimitra Kiritsi, Nikolaos Chaitidis, Michael Arabatzis, Aimilios Lallas, and Efstratios Vakirlis. 2025. "Daylight Photodynamic Therapy for Actinic Keratosis and Field Cancerization: A Narrative Review" Cancers 17, no. 6: 1050. https://doi.org/10.3390/cancers17061050
APA StyleSotiriou, E., Kiritsi, D., Chaitidis, N., Arabatzis, M., Lallas, A., & Vakirlis, E. (2025). Daylight Photodynamic Therapy for Actinic Keratosis and Field Cancerization: A Narrative Review. Cancers, 17(6), 1050. https://doi.org/10.3390/cancers17061050