Laser Therapy for Cutaneous Kaposi Sarcoma: A Systematic Review and Meta-Analysis
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol and Reporting
2.2. Search Strategy
2.3. Eligibility Criteria
2.4. Outcomes
2.5. Study Selection and Data Extraction
2.6. Data Analysis and Synthesis
3. Results
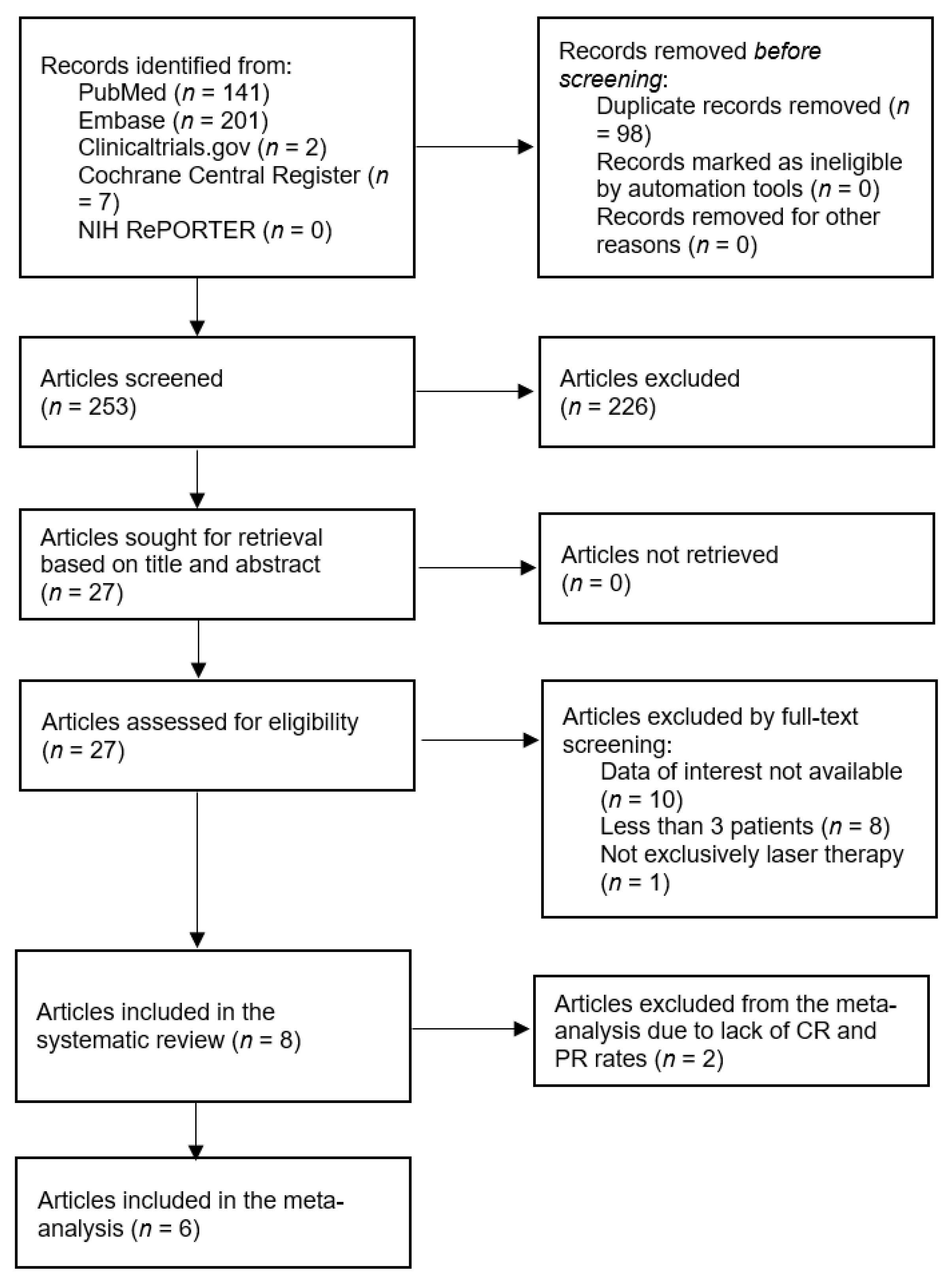
3.1. Study Selection
3.2. Study Characteristics
3.3. Risk of Bias
3.4. Laser Modality and Treatment Parameters
3.5. Treatment Outcomes
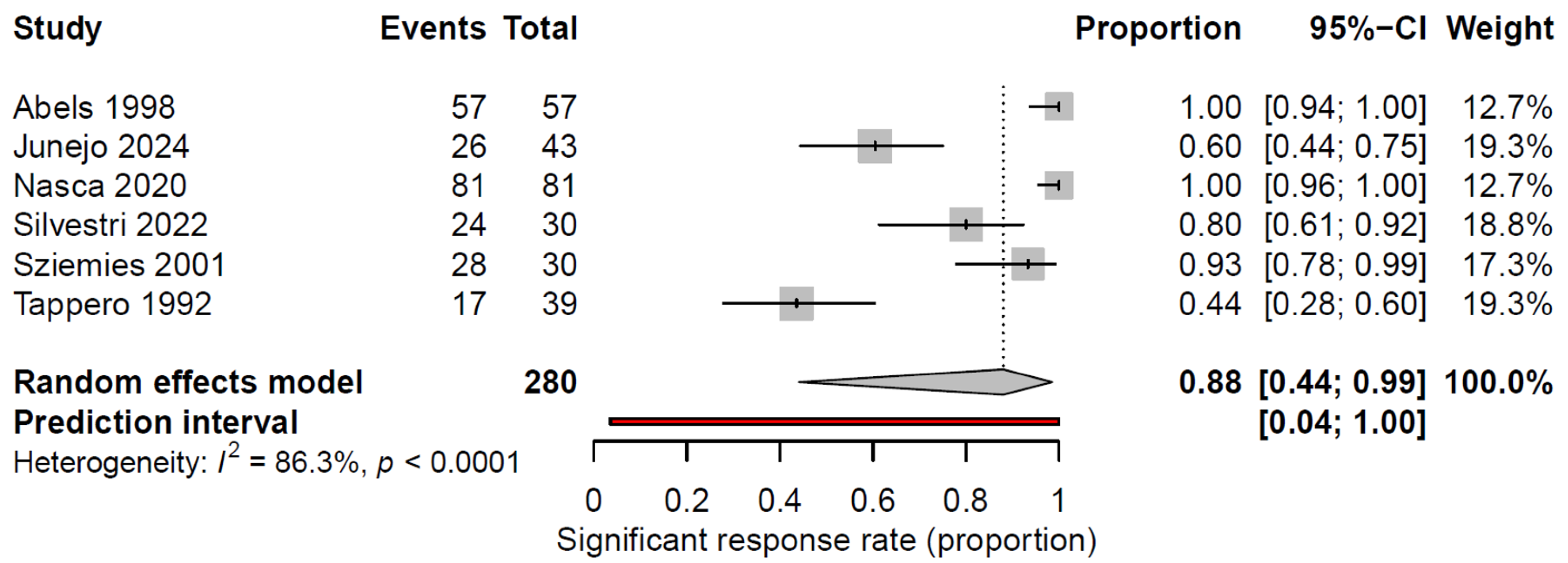
3.6. Meta-Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Chang, Y.; Cesarman, E.; Pessin, M.S.; Lee, F.; Culpepper, J.; Knowles, D.M.; Moore, P.S. Identification of herpesvirus-like DNA sequences in AIDS-associated Kaposi’s sarcoma. Science 1994, 266, 1865–1869. [Google Scholar] [CrossRef] [PubMed]
- Antman, K.; Chang, Y. Kaposi’s Sarcoma. N. Engl. J. Med. 2000, 342, 1027–1038. [Google Scholar] [CrossRef] [PubMed]
- Tsai, K.Y. Kaposi sarcoma, Chapter 139. In Rook’s Textbook of Dermatology, 9th ed.; Griffiths, C., Barker, J., Bleiker, T., Chalmers, R., Creamer, D., Eds.; Wiley: London, UK, 2016. [Google Scholar]
- Di Lorenzo, G. Update on classic Kaposi sarcoma therapy: New look at an old disease. Crit. Rev. Oncol. Hematol. 2008, 68, 242–249. [Google Scholar] [CrossRef] [PubMed]
- Lebbe, C.; Garbe, C.; Stratigos, A.J.; Harwood, C.; Peris, K.; del Marmol, V.; Malvehy, J.; Zalaudek, I.; Hoeller, C.; Dummer, R.; et al. Diagnosis and treatment of Kaposi’s sarcoma: European consensus-based interdisciplinary guideline (EDF/EADO/EORTC). Eur. J. Cancer 2019, 114, 117–127. [Google Scholar] [CrossRef]
- Landthaler, M.; Hohenleutner, U. Laser therapy of vascular lesions. Photodermatol. Photoimmunol. Photomed. 2006, 22, 324–332. [Google Scholar] [CrossRef]
- Özdemir, M.; Balevi, A. Successful treatment of classic Kaposi sarcoma with long-pulse neodymium-doped yttrium aluminum garnet laser: A preliminary study. Dermatol. Surg. 2017, 43, 366–370. [Google Scholar] [CrossRef]
- Chun, Y.; Chang, S.; Park, W.H. A case of classical Kaposi’s sarcoma of the penis showing a good response to high-energy pulsed carbon dioxide laser therapy. J. Dermatol. 1999, 26, 240–243. [Google Scholar] [CrossRef]
- Wheeland, R.G. Clinical uses of lasers in dermatology. Lasers Surg. Med. 1995, 16, 2–23. [Google Scholar] [CrossRef]
- Tappero, J.W.; Grekin, R.C.; Zanelli, G.A.; Berger, T.G. Pulsed-dye laser therapy for cutaneous Kaposi’s sarcoma associated with acquired immunodeficiency syndrome. J. Am. Acad. Dermatol. 1992, 27, 526–530. [Google Scholar] [CrossRef]
- Marchell, N.; Alster, T.S. Successful treatment of cutaneous Kaposi’s sarcoma by the 585-nm pulsed dye laser. Dermatol. Surg. 1997, 23, 973–975. [Google Scholar] [CrossRef]
- Hughes, R.; Lacour, J.-P.; Passeron, T. Pigmentary sequelae of AIDS-related cutaneous Kaposi sarcoma. Arch. Dermatol. 2011, 147, 779–781. [Google Scholar] [CrossRef] [PubMed]
- İlhan, S.; Bayramgürler, D.; Demirbaş, A.; Demirsoy, E.O.; Aktürk, A.Ş.; Kıran, R.; Sayman, N. Efficacy of pro-yellow laser versus cryotherapy in treating cutaneous lesions of Kaposi’s sarcoma: A comparative study. Arch. Dermatol. Res. 2025, 317, 627. [Google Scholar] [CrossRef] [PubMed]
- Abels, C.; Karrer, S.; Bäumler, W.; Goetz, A.; Landthaler, M.; Szeimies, R.-M. Indocyanine green and laser light for the treatment of AIDS-associated cutaneous Kaposi’s sarcoma. Br. J. Cancer 1998, 77, 1021–1024. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C.; et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef]
- Ottawa Hospital Research Institute. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 2 September 2025).
- Junejo, M.H.; Hibler, B.P.; Levin, L.; Menzer, C.; Aleisa, A.; Rossi, A.M. Nonablative laser therapy for cutaneous Kaposi sarcoma: A single-centre proof-of-concept study of six patients. Clin. Exp. Dermatol. 2024, 50, 455–457. [Google Scholar] [CrossRef]
- Bostanci, S.; Alizada, M.A.; Farabi, B.; Akay, B.N. Efficacy of long-pulsed Nd:YAG laser for classic Kaposi’s sarcoma: A dermoscopic study. Dermatol. Pract. Concept. 2024, 14, e2024150. [Google Scholar] [CrossRef]
- Nasca, M.R.; Luppino, I.; Catena, A.S.; Micali, G. Nodular classic Kaposi’s sarcoma treated with neodymium-doped yttrium aluminum garnet laser delivered through a tilted angle: Outcome and 12-month follow up. Lasers Surg. Med. 2020, 52, 979–983. [Google Scholar] [CrossRef]
- Silvestri, M.; Latini, A.; La Parola, I.L.; Messina, C.; Nisticò, S.P.; Cameli, N. Effectiveness and safety of treatment with neodymium:YAG laser 1064 nm in patients with classic and epidemic Kaposi sarcoma. Bioengineering 2022, 9, 106. [Google Scholar] [CrossRef]
- Szeimies, R.-M.; Lorenzen, T.; Karrer, S.; Abels, C.; Plettenberg, A. Photochemotherapie kutaner AIDS-assoziierter Kaposi-Sarkome mit Indocyaningrün und Laserlicht. Hautarzt 2001, 52, 322–326. [Google Scholar] [CrossRef]
- Spicer, M.S.; Goldberg, D.J. Lasers in dermatology. J. Am. Acad. Dermatol. 1996, 34, 1–25. [Google Scholar] [CrossRef]
- Srinivas, C.; Kumaresan, M. Lasers for vascular lesions: Standard guidelines of care. Indian J. Dermatol. Venereol. Leprol. 2011, 77, 349–368. [Google Scholar] [CrossRef]
- Barillari, G.; Sgadari, C.; Palladino, C.; Gendelman, R.; Caputo, A.; Morris, C.B.; Nair, B.C.; Markham, P.; Nel, A.; Stürzl, M.; et al. Inflammatory cytokines synergize with the HIV-1 Tat protein to promote angiogenesis and Kaposi’s sarcoma via induction of basic fibroblast growth factor and the αvβ3 integrin. J. Immunol. 1999, 163, 1929–1935. [Google Scholar] [CrossRef] [PubMed]
- Saran, F.H.; Adamietz, I.A.; Thilmann, C.; Mose, S.; Böttcher, H.D. HIV-associated cutaneous Kaposi’s sarcoma—Palliative local treatment by radiotherapy. Acta Oncol. 1997, 36, 55–58. [Google Scholar] [CrossRef] [PubMed]
- Harrison, M.; Harrington, K.J.; Tomlinson, D.R.; Stewart, J.W. Response and cosmetic outcome of two fractionation regimens for AIDS-related Kaposi’s sarcoma. Radiother. Oncol. 1998, 46, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Geara, F.; Le Bourgeois, J.P.; Piedbois, P.; Pavlovitch, J.M.; Mazeron, J.J. Radiotherapy in the management of cutaneous epidemic Kaposi’s sarcoma. Int. J. Radiat. Oncol. Biol. Phys. 1991, 21, 1517–1522. [Google Scholar] [CrossRef]
- Caccialanza, M.; Marca, S.; Piccinno, R.; Eulisse, G. Radiotherapy of classic and human immunodeficiency virus-related Kaposi’s sarcoma: Results in 1482 lesions. J. Eur. Acad. Dermatol. Venereol. 2008, 22, 297–302. [Google Scholar] [CrossRef]
- Park, J.; Lee, J.E. Localized radiotherapy for classic Kaposi’s sarcoma: An analysis of lesion characteristics and treatment response. Cancers 2024, 16, 3194. [Google Scholar] [CrossRef]
- Ashack, K.A.; Kuritza, V.; Visconti, M.J.; Ashack, L. Dermatologic sequelae associated with radiation therapy. Am. J. Clin. Dermatol. 2020, 21, 541–555. [Google Scholar] [CrossRef]
- Quéro, L.; Palich, R.; Valantin, M.-A.; CANCERVIH Working Group. The role of radiotherapy in treating Kaposi’s sarcoma in HIV-infected patients. Cancers 2022, 14, 1915. [Google Scholar] [CrossRef]
- Kutlubay, Z.; Küçüktaş, M.; Yardımcı, G.; Engin, B.; Serdaroğlu, S. Evaluation of effectiveness of cryotherapy on the treatment of cutaneous Kaposi’s sarcoma. Dermatol. Surg. 2013, 39, 1502–1506. [Google Scholar] [CrossRef]
| Author, Publication Year | Country | Study Design | Age at Treatment, Years, Median (Range) | Male, n (%) | HIV Positive, n (%) | KS Subtype, (n, %) | Sample Size, n (Lesion n) | Lesion Type | Lesion Sizes at Treatment, Diameter Range/Area Range | Risk of Bias *** |
|---|---|---|---|---|---|---|---|---|---|---|
| Abels, 1998 [14] | Germany | Observational | 33 (31–67) | 3 (100) | 3 (100) | HIV-associated (3, 100) | 3 (57) | Macules, plaques, nodules | 0.4–2 cm | Moderate |
| Bostanci, 2024 [19] | Turkey | Observational | 76 (57–78) | 2 (66.7) | 0 (0) | Classic (3, 100) | 3 (42) | Nodules | 0.3–12 cm | Moderate |
| Junejo, 2024 [18] | USA | Observational | 42 (35–91) | 5 (83.3) | 3 (50) | Classic (3, 50), HIV-associated (2, 33.3), Iatrogenic (1, 16.7) | 5 * (43) | Papules, plaques | NA | Moderate |
| Nasca, 2020 [20] | Italy | Observational | 83 (64–86) | 7 (77.8) | NA | Classic (9, 100) | 9 (81) | Nodules | 0.5–3 cm | Moderate |
| Özdemir, 2017 [7] | Turkey | Observational | 65 (45–83) | 4 (57.1) | 0 (0) | Classic (7, 100) | 7 (49) | Papulonodular | 1–15 cm | Moderate |
| Silvestri, 2022 [21] | Italy | Observational | 57.5 (34–76) | 28 (93.3) | 15 (50) | Classic (15, 50), HIV-associated (15, 50) | 30 (30) | Macules, papules, plaques, nodules | 0.5–11.1 cm | Low |
| Szeimies, 2001 [22] | Germany | Observational | 52.5 (33–65) | 6 (100) | 6 (100) | HIV-associated (6, 100) | 6 (30) | Macules, plaques, nodules | 0.16–6 cm2 | Moderate |
| Tappero, 1992 [10] | USA | RCT | 36 (26–45) | 15 (100) | 15 (100) | HIV-associated (15, 100) | 13 ** (39) | Papules | 21–247 cm2 | Some concerns (moderate) |
| Author, Publication Year | Laser Type | Wavelength, nm | Laser Size Range, cm | Fluence Range, J/cm2 | Pulse Protocol | Number of Treatment Sessions | Treatment Sessions Intervals, Weeks | CR Rate (%) | PR Rate (%) | Recurrence Rate (%) | Follow-Up Duration, Months |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Abels, 1998 [14] | ICG | 805 | 2 | 100 | 0.5–6 W/cm2 pulse power | 1 | NA | 18/57 (31.6) | 39/57 (68.4) | 0/57 (0) | 0/57 6–15 |
| Bostanci, 2024 [19] | Nd:YAG | 1064 | 0.3–0.7 | 200–250 | 10–20 ms pulse duration | 1–2 | 4 | NA, clinical and dermoscopic improvements of all lesions | NA | 0/3 (0) | 12 |
| Junejo, 2024 [18] | PDL (N = 3), Nd:YAG (N = 1), PDL + Nd:YAG (N = 1) | 1064 (Nd:YAG), 595 (PDL) | 0.5 (Nd:YAG), 0.7–1 (PDL) | 90–140 (Nd:YAG), 7–9.5 (PDL) | 20–25 ms pulse duration (Nd:YAG), 1.5–40 pulse duration (PDL) | 2–12 | 6 | * PDL: 0/37 (0), Nd:YAG: 0/3 (0), PDL + Nd:YAG: 100 (3/3) | * PDL: 20/37 (54.1), Nd:YAG: 3/3 (100), PDL + Nd:YAG: 0 (0/3) | 0/43 (0) | 7–61 |
| Nasca, 2020 [20] | Nd:YAG | 1064 | 0.5–0.7 | 14–200 | 5 ms pulse duration, triple pulse, 10 ms delay | 1–2 | 4 | 81/81 (100) | 0/81 (0) | 0/81 (0) | 12 |
| Özdemir, 2017 [7] | Nd:YAG | 1064 | 0.4–0.6 | 180–260 | 1.5 ms pulse duration, 5 ms delay | 1–4 | 4 | NA, clinical and dermoscopic improvement of all lesions | NA | 0/49 (0) | 6 |
| Silvestri, 2022 [21] | Nd:YAG | 1064 | 0.25–0.5 | 120–140 | 3 ms pulse duration, double pulse, 20 ms delay | 4 | 4 | 8/30 (26,7) | 16/30 (53.3) | 0/24 (0) | 2.8 |
| Szeimies, 2001 [22] | ICG | 805 | 2 | 100 | 3 W/cm2 pulse power, 33 s per lesion | 1 | NA | 28/30 (93.3) | NA | 0/28 (0) | 24 |
| Tappero, 1992 [10] | PDL | 585 | 0.5 | 8–9.25 | 0.45 ms pulse duration | 2–4 | 4–6 | 17/39 ** (44) | 17/17 (100) | 2.8 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mimouni, T.; Oren-Shabtai, M.; Barzilai, A.; Baum, S.; Noyman, Y.; Michael, S.; Kassem, R. Laser Therapy for Cutaneous Kaposi Sarcoma: A Systematic Review and Meta-Analysis. Cancers 2025, 17, 3708. https://doi.org/10.3390/cancers17223708
Mimouni T, Oren-Shabtai M, Barzilai A, Baum S, Noyman Y, Michael S, Kassem R. Laser Therapy for Cutaneous Kaposi Sarcoma: A Systematic Review and Meta-Analysis. Cancers. 2025; 17(22):3708. https://doi.org/10.3390/cancers17223708
Chicago/Turabian StyleMimouni, Tomer, Meital Oren-Shabtai, Aviv Barzilai, Sharon Baum, Yehonatan Noyman, Shohat Michael, and Riad Kassem. 2025. "Laser Therapy for Cutaneous Kaposi Sarcoma: A Systematic Review and Meta-Analysis" Cancers 17, no. 22: 3708. https://doi.org/10.3390/cancers17223708
APA StyleMimouni, T., Oren-Shabtai, M., Barzilai, A., Baum, S., Noyman, Y., Michael, S., & Kassem, R. (2025). Laser Therapy for Cutaneous Kaposi Sarcoma: A Systematic Review and Meta-Analysis. Cancers, 17(22), 3708. https://doi.org/10.3390/cancers17223708






