Implementation and Evaluation of a Patient-Reported Health Status Survey for Survivors of Childhood Malignancies Treated with Radiation †
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Inclusion and Survey Eligibility
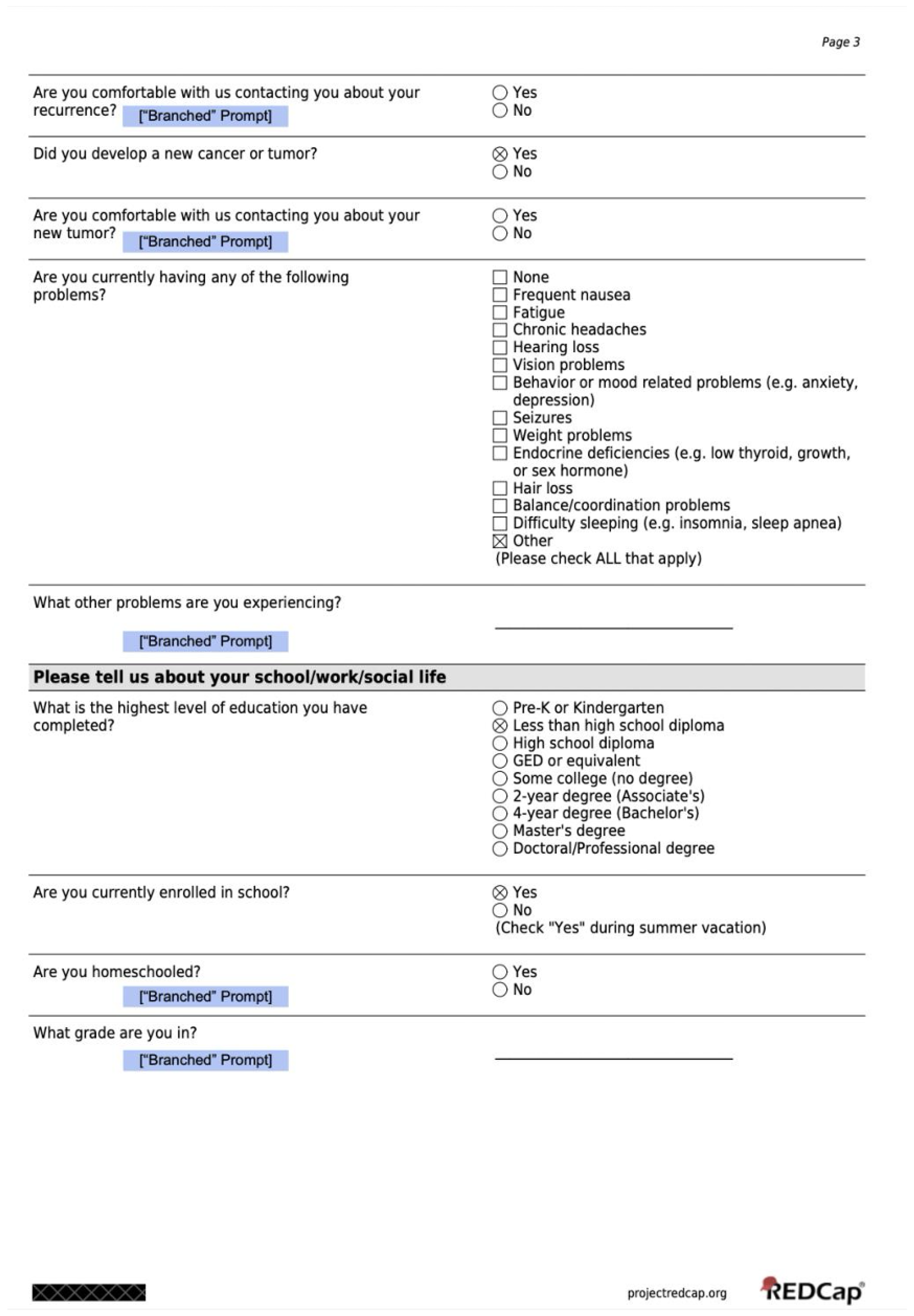
2.2. Overview of the Health Status Survey
2.3. Statistical Analysis
3. Results
3.1. Description of the Eligible Population and Responding Study Population
3.2. Contact Information Updates Varied by Age
3.3. Reminders and Extension of Follow Up
3.4. Medical Visits and Issues in the Past Year
3.5. Prevalence of Recurrence, Second Malignancies, and Deaths Discovered
3.6. Social and Educational Status of Patients Post Treatment
4. Discussion
4.1. Responses Received and Limitations of Response Rate
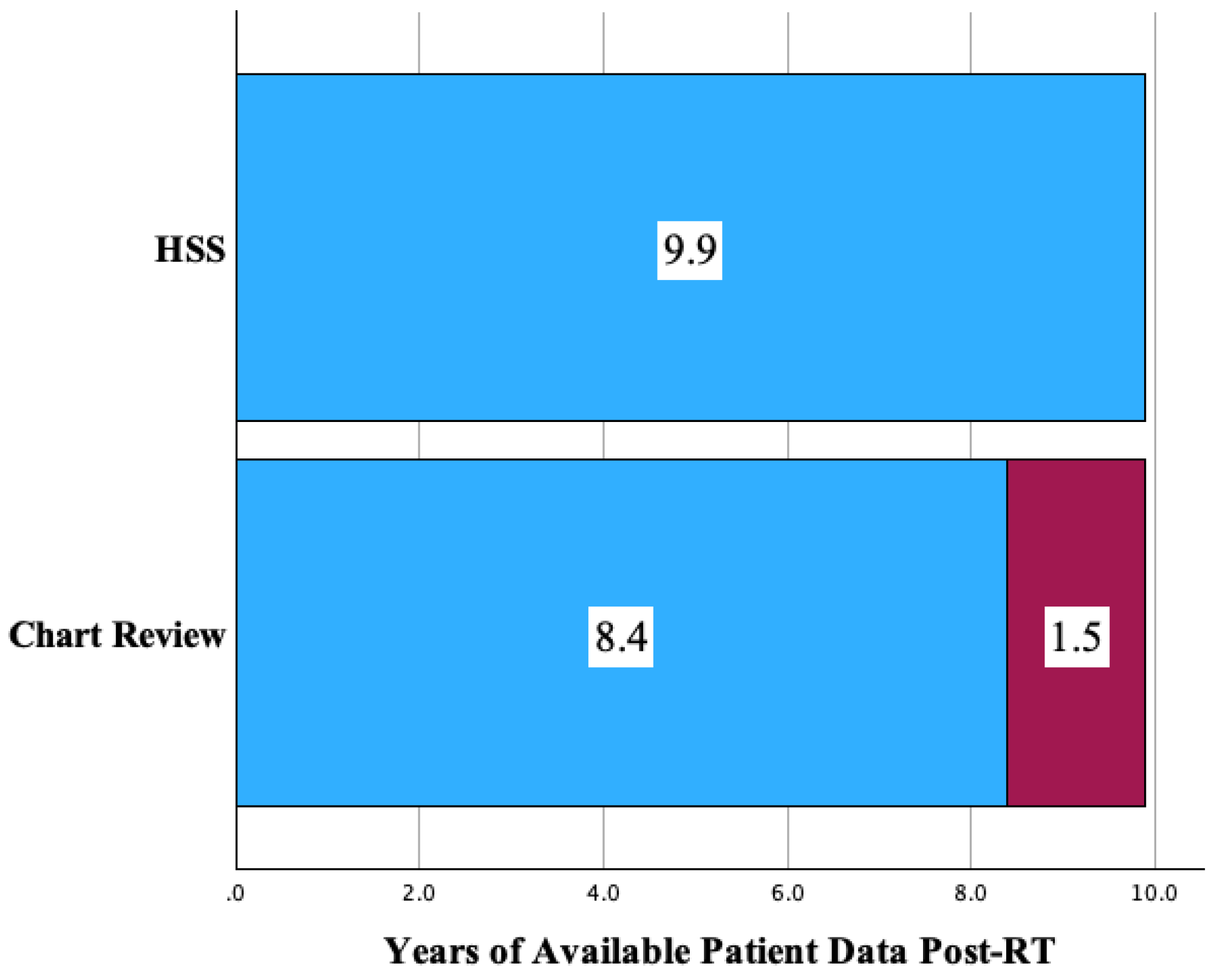
4.2. Follow Up Extended by the HSS
4.3. Recurrence, Second Malignancies, and Deaths
4.4. Health Management Practices
4.5. Social, Educational, and Employment Impact
4.6. Free Expression
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A


References
- Zahnreich, S.; Schmidberger, H. Childhood Cancer: Occurrence, Treatment and Risk of Second Primary Malignancies. Cancers 2021, 13, 2607. [Google Scholar] [CrossRef]
- Chang, W.H.; Katsoulis, M.; Tan, Y.Y.; Mueller, S.H.; Green, K.; Lai, A.G. Late effects of cancer in children, teenagers and young adults: Population-based study on the burden of 183 conditions, in-patient and critical care admissions and years of life lost. Lancet Reg. Health—Eur. 2022, 12, 100248. [Google Scholar] [CrossRef]
- Krasin, M.J.; Constine, L.S.; Friedman, D.; Marks, L.B. Radiation-Related Treatment Effects across the Age Spectrum: Differences and Similarities or What The Old and Young Can Learn From Each Other. Semin. Radiat. Oncol. 2010, 20, 21–29. [Google Scholar] [CrossRef]
- Eaton, B.R.; Goldberg, S.; Tarbell, N.J.; Lawell, M.P.; Gallotto, S.L.; Weyman, E.A.; Kuhlthau, K.A.; Ebb, D.H.; MacDonald, S.M.; Yock, T.I. Long-term health-related quality of life in pediatric brain tumor survivors receiving proton radiotherapy at <4 years of age. Neuro-Oncology 2020, 22, 1379–1387. [Google Scholar] [CrossRef]
- Lawell, M.P.; Rose, M.L.; Joshi, J.; Marinelli, J.A.; Upton, M.J.; Dennehy, S.L.; Kang, S.L.; Weyman, E.A.; Allison, K.W.; Tarbell, N.J.; et al. Self-Reported Health Status Survey Creation and Distribution Outcomes in a Large Cohort of Pediatric Oncology Patients Treated with Proton Radiation Therapy. Adv. Radiat. Oncol. 2025, 10, 101748. [Google Scholar] [CrossRef] [PubMed]
- Elliott, M.N.; Brown, J.A.; Hambarsoomian, K.; Parast, L.; Beckett, M.K.; Lehrman, W.G.; Giordano, L.A.; Goldstein, E.H.; Cleary, P.D. Survey Protocols, Response Rates, and Representation of Underserved Patients: A Randomized Clinical Trial. JAMA Health Forum 2024, 5, e234929. [Google Scholar] [CrossRef]
- Wang, K.; Eftang, C.N.; Jakobsen, R.B.; Årøen, A. Review of response rates over time in registry-based studies using patient-reported outcome measures. BMJ Open 2020, 10, e030808. [Google Scholar] [CrossRef]
- Meyer, V.M.; Benjamens, S.; Moumni, M.E.; Lange, J.F.M.; Pol, R.A. Global Overview of Response Rates in Patient and Health Care Professional Surveys in Surgery. Ann. Surg. 2022, 275, e75–e81. [Google Scholar] [CrossRef] [PubMed]
- Neve, O.M.; van Benthem, P.P.G.; Stiggelbout, A.M.; Hensen, E.F. Response rate of patient reported outcomes: The delivery method matters. BMC Med. Res. Methodol. 2021, 21, 220. [Google Scholar] [CrossRef] [PubMed]
- Ruseckaite, R.; Mudunna, C.; Caruso, M.; Ahern, S. Response rates in clinical quality registries and databases that collect patient reported outcome measures: A scoping review. Health Qual. Life Outcomes 2023, 21, 71. [Google Scholar] [CrossRef] [PubMed]
- Otth, M.; Wyss, J.; Scheinemann, K. Long-Term Follow-Up of Pediatric CNS Tumor Survivors—A Selection of Relevant Long-Term Issues. Children 2022, 9, 447. [Google Scholar] [CrossRef] [PubMed]
- Salloum, R.; Baum, K.; Gerstle, M.; Spoudeas, H.; Rose, S.R. Late Effects of Treatment for Childhood Brain and Spinal Tumors. In Brain and Spinal Tumors of Childhood, 2nd ed.; CRC Press: Boca Raton, FL, USA, 2020. [Google Scholar]
- Alias, H.; Morthy, S.K.; Zakaria, S.Z.S.; Muda, Z.; Tamil, A.M. Behavioral outcome among survivors of childhood brain tumor: A case control study. BMC Pediatr. 2020, 20, 53. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, G.T.; Khan, R.B.; Chemaitilly, W. Long-Term Outcomes Among Survivors of Childhood Central Nervous System Malignancies: Late Mortality, Subsequent Neoplasms, Endocrine and Neurologic Morbidity. In Brain Tumors in Children; Gajjar, A., Reaman, G.H., Racadio, J.M., Smith, F.O., Eds.; Springer International Publishing: Cham, Switzerland, 2018; pp. 347–378. [Google Scholar] [CrossRef]
- van Schaik, J.; van Roessel, I.M.A.A.; Schouten-van Meeteren, N.A.Y.N.; van Iersel, L.; Clement, S.C.; Boot, A.M.; Claahsen-van der Grinten, H.L.; Fiocco, M.; Janssens, G.O.; van Vuurden, D.G.; et al. High Prevalence of Weight Gain in Childhood Brain Tumor Survivors and Its Association with Hypothalamic-Pituitary Dysfunction. J. Clin. Oncol. 2021, 39, 1264–1273. [Google Scholar] [CrossRef]
- Institute of Medicine (US) and National Research Council (US) National Cancer Policy Board. Late Effects of Childhood Cancer; Hewitt, M., Weiner, S.L., Simone, J.V., Eds.; National Academies Press (US): Washington, DC, USA, 2003. [Google Scholar]
- Wilson, R.L.; Soja, J.; Yunker, A.G.; Uno, H.; Gordon, E.; Cooney, T.; Dieli-Conwright, C.M. Obesity Risk of Pediatric Central Nervous System Tumor Survivors: A Cross-Sectional Study. Nutrients 2023, 15, 2269. [Google Scholar] [CrossRef]
- Vatner, R.E.; Niemierko, A.; Misra, M.; Weyman, E.A.; Goebel, C.P.; Ebb, D.H.; Jones, R.M.; Huang, M.S.; Mahajan, A.; Grosshans, D.R.; et al. Endocrine Deficiency As a Function of Radiation Dose to the Hypothalamus and Pituitary in Pediatric and Young Adult Patients With Brain Tumors. J. Clin. Oncol. 2018, 36, 2854–2862. [Google Scholar] [CrossRef]
- Casano-Sancho, P.; Izurieta-Pacheco, A.C. Endocrine Late Effects in Childhood Cancer Survivors. Cancers 2022, 14, 2630. [Google Scholar] [CrossRef]
- Varedi, M.; Lu, L.; Phillips, N.S.; Partin, R.E.; Brinkman, T.M.; Armstrong, G.T.; Chase, E.; Khan, R.B.; Powell, D.; McKenna, R.F.; et al. Balance Impairment in Survivors of Pediatric Brain Cancers: Risk Factors and Associated Physical Limitations. J. Cancer Surviv. Res. Pract. 2021, 15, 311–324. [Google Scholar] [CrossRef] [PubMed]
- Mader, L.; Michel, G.; Roser, K. Unemployment Following Childhood Cancer. Dtsch. Ärzteblatt Int. 2017, 114, 805–812. [Google Scholar] [CrossRef] [PubMed]
- de Boer, A.G.E.M.; Verbeek, J.H.A.M.; van Dijk, F.J.H. Adult survivors of childhood cancer and unemployment. Cancer 2006, 107, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Ellenberg, L.; Liu, Q.; Gioia, G.; Yasui, Y.; Packer, R.J.; Mertens, A.; Donaldson, S.S.; Stovall, M.; Kadan-Lottick, N.; Armstrong, G.; et al. Neurocognitive Status in Long-Term Survivors of Childhood CNS Malignancies: A Report from the Childhood Cancer Survivor Study. Neuropsychology 2009, 23, 705–717. [Google Scholar] [CrossRef] [PubMed]
- Remes, T.M.; Hovén, E.; Ritari, N.; Pohjasniemi, H.; Puosi, R.; Arikoski, P.M.; Arola, M.O.; Lähteenmäki, P.M.; Lönnqvist, T.R.I.; Ojaniemi, M.K.; et al. Neurocognitive impairment, employment, and social status in radiotherapy-treated adult survivors of childhood brain tumors. Neuro-Oncol. Pract. 2021, 8, 266–277. [Google Scholar] [CrossRef]
- Eiser, C.; Hill, J.J.; Vance, Y.H. Examining the psychological consequences of surviving childhood cancer: Systematic review as a research method in pediatric psychology. J. Pediatr. Psychol. 2000, 25, 449–460. [Google Scholar] [CrossRef]
- Zebrack, B.J.; Chesler, M.A. Quality of life in childhood cancer survivors. Psycho-Oncology 2002, 11, 132–141. [Google Scholar] [CrossRef] [PubMed]
- Kelaghan, J.; Myers, M.H.; Mulvihill, J.J.; Byrne, J.; Connelly, R.R.; Austin, D.F.; Strong, L.C.; Meigs, J.W.; Latourette, H.B.; Holmes, G.F. Educational achievement of long-term survivors of childhood and adolescent cancer. Med. Pediatr. Oncol. 1988, 16, 320–326. [Google Scholar] [CrossRef] [PubMed]
- Mitby, P.A.; Robison, L.L.; Whitton, J.A.; Zevon, M.A.; Gibbs, I.C.; Tersak, J.M.; Meadows, A.T.; Stovall, M.; Zeltzer, L.K.; Mertens, A.C.; et al. Utilization of special education services and educational attainment among long-term survivors of childhood cancer: A report from the Childhood Cancer Survivor Study. Cancer 2003, 97, 1115–1126. [Google Scholar] [CrossRef] [PubMed]
- Trkova, K.; Vicha, A.; Krskova, L.; Koblizek, M.; Ondrova, B.; Kopecka, M.; Landova, L.; III, V.B.; Zapotocky, M.; Sumerauer, D. QOL-42. Analysis of Late Events After Radiation Therapy for Primary Pediatric Brain Tumors. Neuro-Oncology 2024, 26. [Google Scholar] [CrossRef]
- Barrera, M.; Shaw, A.K.; Speechley, K.N.; Maunsell, E.; Pogany, L. Educational and social late effects of childhood cancer and related clinical, personal, and familial characteristics. Cancer 2005, 104, 1751–1760. [Google Scholar] [CrossRef] [PubMed]
- Godono, A.; Felicetti, F.; Conti, A.; Clari, M.; Dionisi-Vici, M.; Gatti, F.; Ciocan, C.; Pinto, T.; Arvat, E.; Brignardello, E.; et al. Employment among Childhood Cancer Survivors: A Systematic Review and Meta-Analysis. Cancers 2022, 14, 4586. [Google Scholar] [CrossRef]
- Kirchhoff, A.C.; Leisenring, W.; Krull, K.R.; Ness, K.K.; Friedman, D.L.; Armstrong, G.T.; Stovall, M.; Park, E.R.; Oeffinger, K.C.; Hudson, M.; et al. Unemployment among Adult Survivors of Childhood Cancer: A report from the Childhood Cancer Survivors Study. Med. Care 2010, 48, 1015–1025. [Google Scholar] [CrossRef]
- Kumar, R.; Narra, L.R.; Sherwani, Z.; Parikh, R.R. Neurological sequalae in pediatric patients with CNS tumors after radiation treatment: A comprehensive review. Semin. Pediatr. Neurol. 2025, 53, 101181. [Google Scholar] [CrossRef] [PubMed]
- Palmer, J.D.; Tsang, D.S.; Tinkle, C.L.; Olch, A.J.; Kremer, L.C.M.; Ronckers, C.M.; Gibbs, I.C.; Constine, L.S. Late effects of radiation therapy in pediatric patients and survivorship. Pediatr. Blood Cancer 2021, 68, e28349. [Google Scholar] [CrossRef] [PubMed]
- Joshi, J.; Lawell, M.; Allison, K.; Bajaj, B.; Gallotto, S.; Rose, M.; Tarbell, N.; MacDonald, S.; Yock, T. Implementation and Evaluation of a Patient-Reported Health Status Survey for Survivors of Childhood Malignancies Treated with Radiation. Int. J. Radiat. Oncol. Biol. Phys. 2024, 120, e694. [Google Scholar] [CrossRef]



| (a) | |
|---|---|
| Respondent Demographics | n = 322 |
| Age at RT (years) 1 | 9.9 (0.88–24.72) |
| Age at time of survey completion (years) 1 | 18.74 (2.34–35.4) |
| Age Status (minor/adult at RT and Survey) 2 | |
| Minor at RT, Minor at Survey | 147 (45.7%) |
| Minor at RT, Adult at Survey | 137 (42.5%) |
| Adult at RT, Adult at Survey | 38 (10.2%) |
| Tumor Site 2 | |
| Central Nervous System (CNS) | 207 (64.3%) |
| Non-CNS | 115 (35.7%) |
| (b) | |
| Tumor Site 2 | |
| Central Nervous System (CNS) | n = 207 |
| Medulloblastoma/PNET/Pineoblastoma | 62 (30.0%) |
| Glial Tumors/Astrocytoma | 28 (13.5%) |
| Vascular Lesions | 10 (4.8%) |
| Ependymoma | 31 (15.0%) |
| Germ Cell | 31 (15.0%) |
| Craniopharyngioma | 15 (7.2%) |
| Other/Unspecified | 30 (14.5%) |
| CNS Treatment Subtype | n = 207 |
| Received CSI (Craniospinal Irradiation) | 125 (60.4%) |
| Did not receive CSI | 82 (39.6%) |
| Non-CNS | n = 115 |
| Neuroblastoma | 12 (10.4%) |
| Rhabdomyosarcoma | 34 (29.6%) |
| Sarcoma (Bone) | 18 (15.7%) |
| Chordoma | 18 (15.7%) |
| Sarcoma (Soft Tissue) | 7 (6.1%) |
| Hodgkin’s Lymphoma | 7 (6.1%) |
| Other/Unspecified | 19 (16.5%) |
| Contact Information | Changed Any Information | Total |
|---|---|---|
| Age Status (minor/adult at RT and Survey) 1 | 185 (57.8%) | 322 |
| Minor at RT, Minor at Survey | 70 (47.6%) | 147 |
| Minor at RT, Adult at Survey | 89 (65.0%) | 137 |
| Adult at RT, Adult at Survey | 27 (71.0%) | 38 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Joshi, J.; Lawell, M.; Allison, K.; Bajaj, B.; Dennehy, S.; Rose, M.; Tarbell, N.; Yock, T. Implementation and Evaluation of a Patient-Reported Health Status Survey for Survivors of Childhood Malignancies Treated with Radiation. Cancers 2025, 17, 3634. https://doi.org/10.3390/cancers17223634
Joshi J, Lawell M, Allison K, Bajaj B, Dennehy S, Rose M, Tarbell N, Yock T. Implementation and Evaluation of a Patient-Reported Health Status Survey for Survivors of Childhood Malignancies Treated with Radiation. Cancers. 2025; 17(22):3634. https://doi.org/10.3390/cancers17223634
Chicago/Turabian StyleJoshi, Jaitri, Miranda Lawell, Keith Allison, Benjamin Bajaj, Sara Dennehy, Melanie Rose, Nancy Tarbell, and Torunn Yock. 2025. "Implementation and Evaluation of a Patient-Reported Health Status Survey for Survivors of Childhood Malignancies Treated with Radiation" Cancers 17, no. 22: 3634. https://doi.org/10.3390/cancers17223634
APA StyleJoshi, J., Lawell, M., Allison, K., Bajaj, B., Dennehy, S., Rose, M., Tarbell, N., & Yock, T. (2025). Implementation and Evaluation of a Patient-Reported Health Status Survey for Survivors of Childhood Malignancies Treated with Radiation. Cancers, 17(22), 3634. https://doi.org/10.3390/cancers17223634






