Antigenic Dark Matter: Unexplored Post-Translational Modifications of Tumor-Associated and Tumor-Specific Antigens in Pancreatic Cancer
Simple Summary
Abstract
1. Introduction
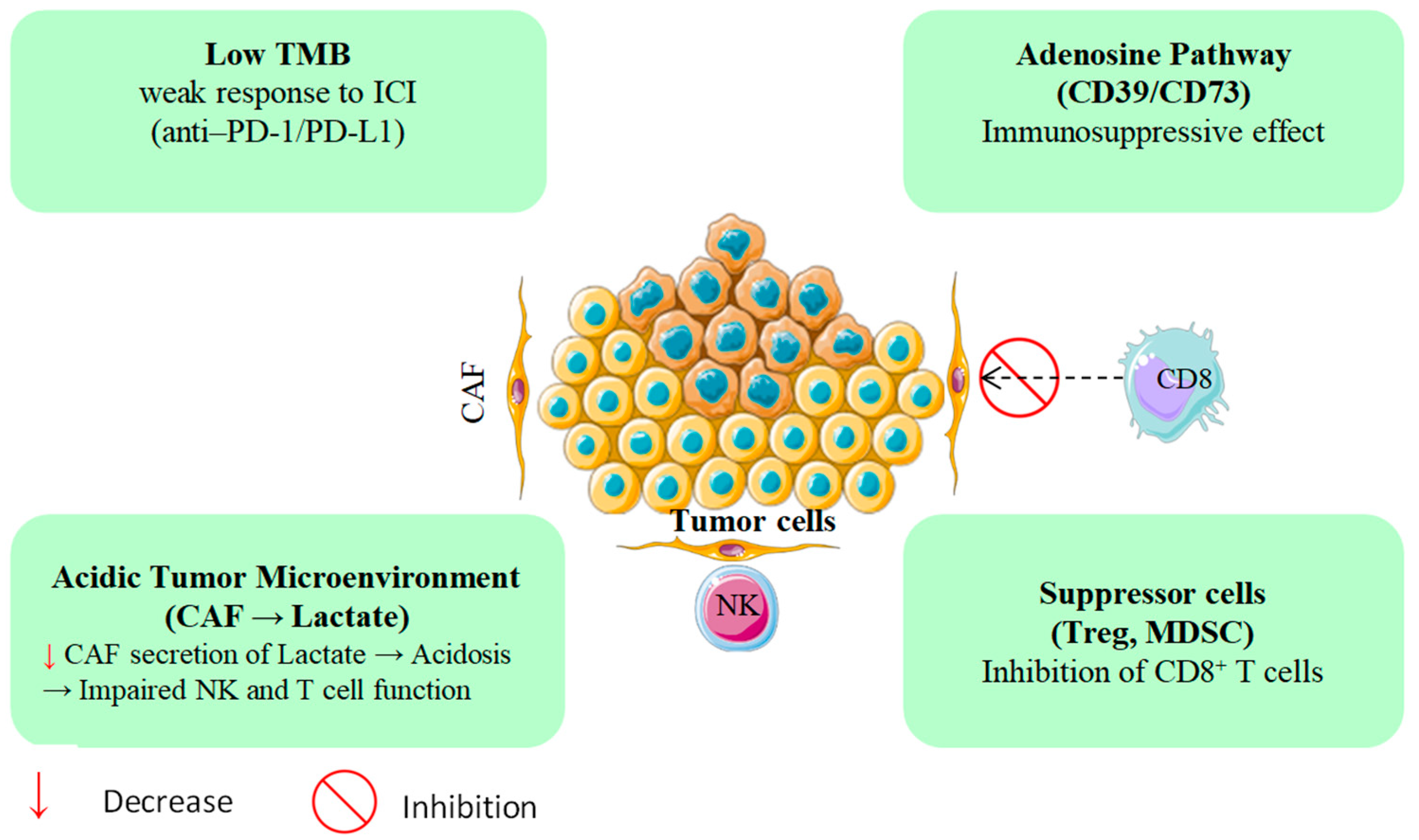
1.1. Pancreatic Cancer: Immune Evasion Beyond Mutational Load
1.2. Post-Translational Modifications: The Subsequent Frontier in Antigen Discovery
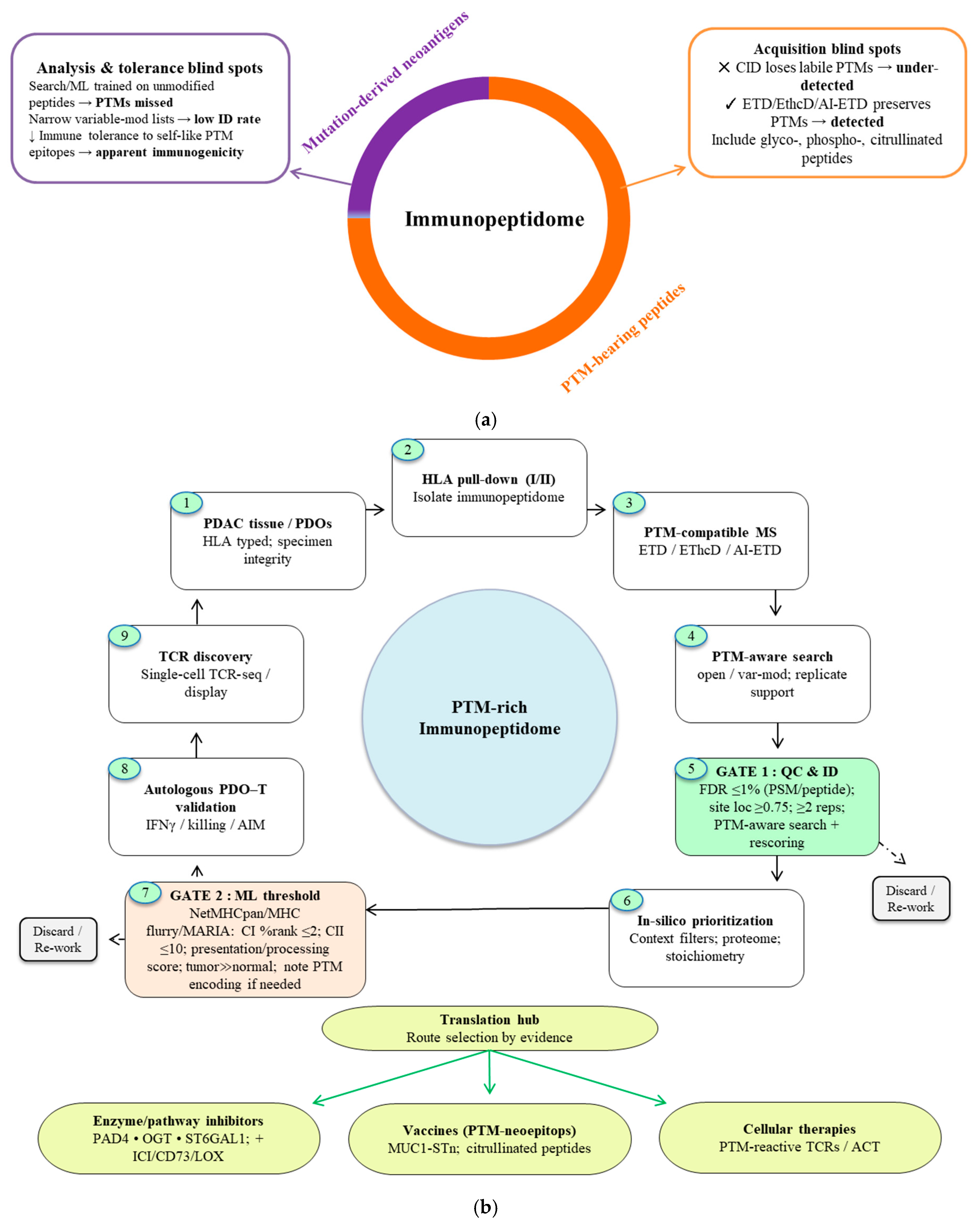
2. The Hypothesis of Antigenic Dark Matter
2.1. Mechanistic Bases of PTM-Mediated Immune Evasion
2.2. Neoantigen Diversity Beyond the Genome
- Contextual Immunogenicity: Although many PTMs favor immune evasion, some enhance recognition. Notably, citrullinated peptides derived from oncogenic KRAS (G12D) elicit CD8+ T cell responses in PDAC patients who do not respond to the corresponding unmodified peptides, revealing fresh avenues for neoantigen targeting [33,81,82].
2.3. Technical Barriers and Emerging Solutions
- Detection Limitations: Conventional mass spectrometry often fails to capture PTM-modified peptides owing to low abundance and chemical lability [83,84]. Advances in MS-based glycoproteomics including size-exclusion-based enrichment are improving the detection of sialylated epitopes that are particularly relevant in PDAC, including within the stromal compartment [85,86].
- Functional Validation: Establishing bona fide immunogenicity requires stringent in vitro and in vivo testing. CRISPR-engineered PDAC organoids, including constructs that recapitulate specific PTMs (e.g., p53 O-GlcNAcylation), are being leveraged to probe T cell reactivity and antigen processing [87,88].
- Clinical Proof-of-Concept: Early clinical experience with vaccines targeting citrullinated vimentin in PDAC, together with preclinical studies of PTM-focused vaccines, points to therapeutic promise. PTMs such as citrullination can yield tumor-associated antigens capable of driving immune responses [34,77,89]. A cohesive strategy to decode this “dark matter” of the immunopeptidome from PTM-compatible discovery platforms to the prioritization and translation of targetable epitopes is therefore essential (Figure 4).Collectively, these data position PTMs as a critical yet underutilized dimension of cancer immunotherapy. Systematically harnessing this antigenic “dark matter” may provide new strategies to overcome immune resistance in antigenically cold tumors such as PDAC.
3. PTMs in Cancer Immunology: Mechanisms and Consequences
3.1. Modifying the Antigenic Code: The Role of PTMs in Epitope Diversification
3.2. Regulation of PTM Landscapes by Microenvironmental Factors
3.3. PTM Interference and Immune Regulation
3.4. Metabolic Hypoxic Axis: Interplay Between O-GlcNAcylation and Phosphorylation
3.5. Epigenetic Immunogenic Axis: Circuits of Acetylation and Ubiquitination
3.6. Stromal Tumor Axis: Networks of SUMOylation and Citrullination
3.7. Evolutionary Consequences of PTM Interactions
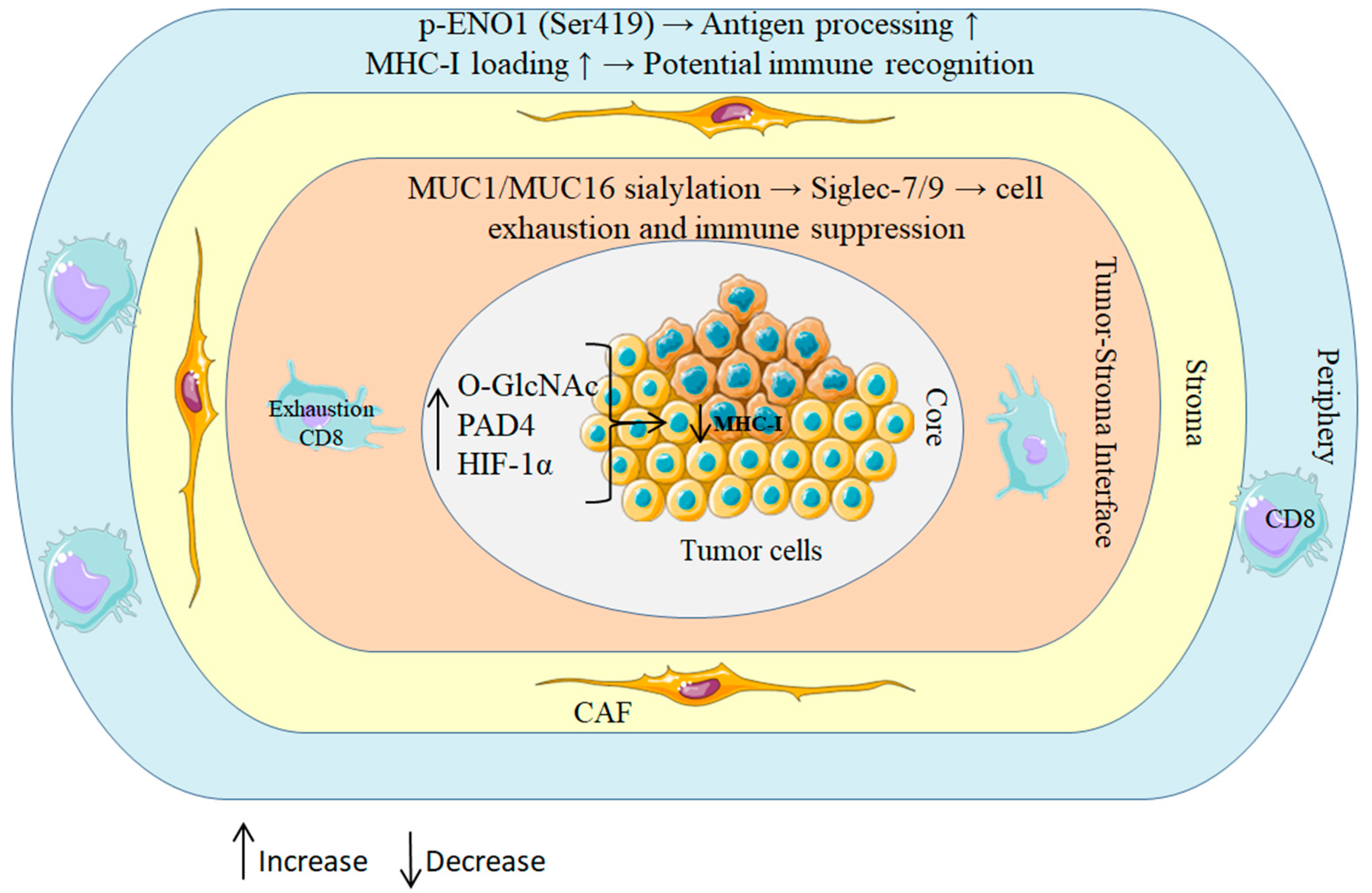
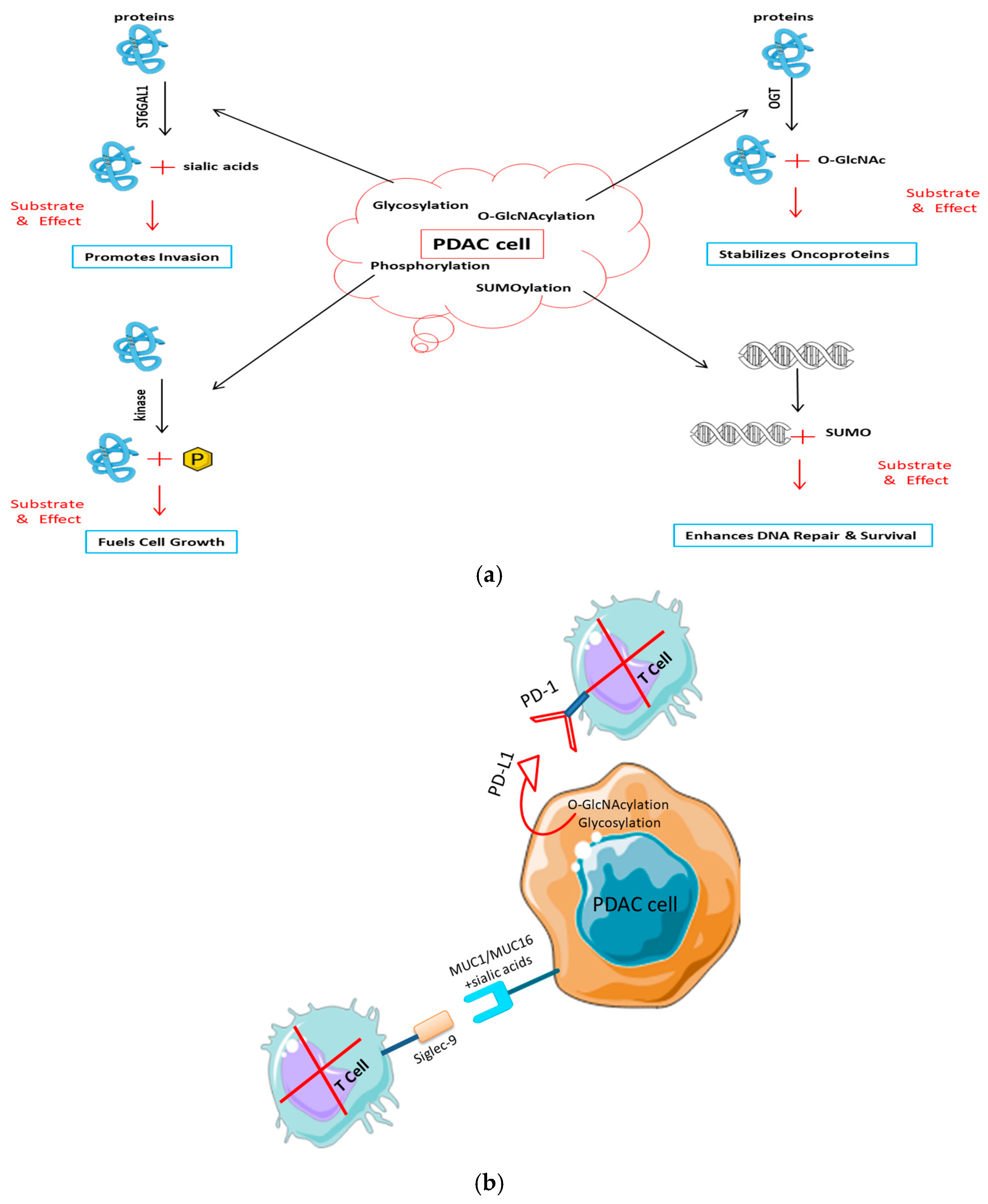
- Hybrid glyco-phospho-signaling on mucins: In PDAC, atypical glycosylation and phosphorylation of MUC1 are recurrent and contribute to immune escape. Hybrid glyco-phospho-PTMs on mucins remodel molecular conformation and binding interfaces, creating steric barriers to immune recognition and altering antigen processing and presentation [116,117].
- Enzymatic crosstalk among PAD4 and OGT: Tumors with altered PAD4 activity including putative loss-of-function variants frequently display concomitant O-GlcNAc transferase (OGT) overexpression, revealing coordinated dysregulation across PTM enzymes. The resulting imbalance between citrullination (PAD4) and O-GlcNAcylation (OGT) fosters a protumor immunosuppressive niche across multiple cancer types [58,118].
3.8. Immune Editing Pressures and Post-Translational Modification-Driven Antigenic Landscapes
3.9. Immune Evasion Induced by Hypoxia
3.10. Thymic Tolerance and Context-Dependent Immunogenicity
4. The PTM Landscape in Pancreatic Cancer
4.1. The PDAC Paradox: Minimal Mutational Load, Elevated Antigenic Complexity
4.2. Universal Hyperactivation of PTM-Regulating Enzymes
4.3. Spatial Heterogeneity of Post-Translational Modifications in the Tumor Microenvironment
4.4. Stromal Contributions and Tumor Microenvironmental Influences
4.5. Case Studies and Notable PTM-Modified Antigens in PDAC
5. Challenges: Why PTMs Remain Dark Matter in Oncology
5.1. Challenges in Technical Detection
5.2. Complexities of HLA Presentation and Immune Recognition
5.3. Telling the Difference Between Driver and Passenger PTMs
6. Novel Solutions and Innovations
7. Therapeutic Horizons: Targeting PTM Antigens
7.1. Vaccines Aimed at PTM Neoepitopes
7.2. Enzyme Inhibitors to Block PTM Machinery
7.3. Risks of Clinical Translation
8. Outlook and Strategic Recommendations
8.1. Thorough Mapping of PTM–Immune Interfaces
8.2. Immunogenicity Assessment in Patient-Derived Organoids and Models
8.3. Collaborative Frameworks: International PTM Antigen Discovery Consortia
9. Additional Regulatory Mechanisms in Pancreatic Cancer
10. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ACT | Adoptive Cell Therapy |
| APM | Antigen-Processing Machinery |
| β-HB | β-hydroxybutyrate |
| β2M | β2-microglobulin |
| CA19-9 | Carbohydrate Antigen 19-9 |
| CAF | Cancer-Associated Fibroblast |
| CARM1 | Coactivator-Associated Arginine Methyltransferase 1 |
| CAV1 | Caveolin-1 |
| CD | Cluster of Differentiation |
| CID | Collision-Induced Dissociation |
| CTLA-4 | Cytotoxic T-Lymphocyte-Associated Protein 4 |
| CXCL | C-X-C Motif Chemokine Ligand |
| DIA | Data-Independent Acquisition |
| DNA | Deoxyribonucleic Acid |
| DUB | Deubiquitinating Enzyme |
| ECM | Extracellular Matrix |
| EGFR | Epidermal Growth Factor Receptor |
| EMT | Epithelial–Mesenchymal Transition |
| ENO1 | Enolase 1 |
| ERAP1 | Endoplasmic Reticulum Aminopeptidase 1 |
| ERK | Extracellular Signal-Regulated Kinase |
| ETD | Electron Transfer Dissociation |
| EThcD | Electron Transfer/Higher-Energy Collision Dissociation |
| EZH2 | Enhancer of Zeste Homolog 2 |
| FDR | False Discovery Rate |
| FOXP3 | Forkhead Box P3 |
| FOLFIRINOX | Folinic Acid, Fluorouracil, Irinotecan, Oxaliplatin |
| GALNTs | Polypeptide N-Acetylgalactosaminyltransferases |
| GFAT | Glutamine:Fructose-6-Phosphate Aminotransferase |
| GPX4 | Glutathione Peroxidase 4 |
| GR | Glucocorticoid Receptor |
| GSK3β | Glycogen Synthase Kinase 3 Beta |
| HBP | Hexosamine Biosynthetic Pathway |
| HCD | Higher-Energy Collisional Dissociation |
| HDAC | Histone Deacetylase |
| HER2 | Human Epidermal Growth Factor Receptor 2 |
| HIF | Hypoxia-Inducible Factor |
| HIPP | Human Immuno-Peptidome Project |
| HLA | Human Leukocyte Antigen |
| HSP | Heat Shock Protein |
| ICI | Immune Checkpoint Inhibitor |
| IL | Interleukin |
| iNOS | Inducible Nitric Oxide Synthase |
| JAK | Janus Kinase |
| KRAS | Kirsten Rat Sarcoma Viral Oncogene Homolog |
| LOX | Lysyl Oxidase |
| MAPK | Mitogen-Activated Protein Kinase |
| MDSC | Myeloid-Derived Suppressor Cell |
| MHC | Major Histocompatibility Complex |
| MS | Mass Spectrometry |
| MSS | Microsatellite Stable |
| MSI-H | Microsatellite Instability-High |
| MUC | Mucin |
| NET | Neutrophil Extracellular Trap |
| NF-κB | Nuclear Factor Kappa B |
| NK | Natural Killer |
| NO | Nitric Oxide |
| NOS | Nitric Oxide Synthase |
| OGT | O-GlcNAc Transferase |
| ORR | Objective Response Rate |
| PAD | Peptidylarginine Deiminase |
| PD-1 | Programmed Cell Death Protein 1 |
| PD-L1 | Programmed Death-Ligand 1 |
| PDAC | Pancreatic Ductal Adenocarcinoma |
| PDO | Patient-Derived Organoid |
| PIAS | Protein Inhibitor of Activated STAT |
| PKM2 | Pyruvate Kinase M2 |
| PRMT | Protein Arginine Methyltransferase |
| PTM | Post-Translational Modification |
| QC | Quality Control |
| RAF1 | Raf-1 Proto-Oncogene, Serine/Threonine Kinase |
| SER | Serine |
| STAT | Signal Transducer and Activator of Transcription |
| ST6GAL1 | β-Galactoside α-2,6-Sialyltransferase 1 |
| ST3GAL | β-Galactoside α-2,3-Sialyltransferase |
| STING | Stimulator of Interferon Genes |
| SUMO | Small Ubiquitin-like Modifier |
| TAM | Tumor-Associated Macrophage |
| TAP | Transporter Associated with Antigen Processing |
| TCR | T cell Receptor |
| TGF-β | Transforming Growth Factor Beta |
| Th | T Helper Cell |
| TIGIT | T Cell Immunoreceptor with Ig and ITIM Domains |
| TMB | Tumor Mutational Burden |
| TME | Tumor Microenvironment |
| Tn | Thomsen-nouvelle Antigen |
| TP53 | Tumor Protein P53 |
| Treg | Regulatory T Cell |
| TSA | Tumor-Specific Antigen |
| UBA2 | Ubiquitin-Like Modifier Activating Enzyme 2 |
| UBC9 | Ubiquitin Conjugating Enzyme 9 |
| UDP | Uridine Diphosphate |
| USP | Ubiquitin Specific Peptidase |
References
- Muaddi, H.; Kearse, L.; Warner, S. Multimodal Approaches to Patient Selection for Pancreas Cancer Surgery. Curr. Oncol. 2024, 31, 2260–2273. [Google Scholar] [CrossRef] [PubMed]
- Ju, Y.; Xu, D.; Liao, M.-M.; Sun, Y.; Bao, W.-D.; Yao, F.; Ma, L. Barriers and opportunities in pancreatic cancer immunotherapy. Npj Precis. Oncol. 2024, 8, 199. [Google Scholar] [CrossRef] [PubMed]
- Duan, X.; Zhang, T.; Feng, L.; de Silva, N.; Greenspun, B.; Wang, X.; Moyer, J.; Martin, M.L.; Chandwani, R.; Elemento, O.; et al. A pancreatic cancer organoid platform identifies an inhibitor specific to mutant KRAS. Cell Stem Cell 2023, 31, 71–88.e8. [Google Scholar] [CrossRef]
- Stefanoudakis, D.; Frountzas, M.; Schizas, D.; Michalopoulos, N.V.; Drakaki, A.; Toutouzas, K.G. Significance of TP53, CDKN2A, SMAD4 and KRAS in Pancreatic Cancer. Curr. Issues Mol. Biol. 2024, 46, 2827–2844. [Google Scholar] [CrossRef]
- Lorentzen, C.L.; Haanen, J.B.; Met, Ö.; Svane, I.M. Clinical advances and ongoing trials of mRNA vaccines for cancer treatment. Lancet Oncol. 2022, 23, e450–e458. [Google Scholar] [CrossRef] [PubMed]
- Zhou, S.; Fan, C.; Zeng, Z.; Young, K.H.; Li, Y. Clinical and Immunological Effects of p53-Targeting Vaccines. Front. Cell Dev. Biol. 2021, 9, 762796. [Google Scholar] [CrossRef]
- Zhang, W.; Li, S.; Liu, Y.; Xing, R.; Jin, Z.; Yan, X.; Xue, H. Immunosuppressive microenvironment improvement and treatment of aggressive malignancy pancreatic ductal adenocarcinoma based on local administration of injectable hydrogel. Nano Today 2023, 50, 101832. [Google Scholar] [CrossRef]
- Vruzhaj, I.; Gambirasi, M.; Busato, D.; Giacomin, A.; Toffoli, G.; Safa, A. Gut Microbiota-Based Immunotherapy: Engineered Escherichia coli Nissle 1917 for Oral Delivery of Glypican-1 in Pancreatic Cancer. Medicina 2025, 61, 633. [Google Scholar] [CrossRef]
- Glapiński, F.; Zając, W.; Fudalej, M.; Deptała, A.; Czerw, A.; Sygit, K.; Kozłowski, R.; Badowska-Kozakiewicz, A. The Role of the Tumor Microenvironment in Pancreatic Ductal Adenocarcinoma: Recent Advancements and Emerging Therapeutic Strategies. Cancers 2025, 17, 1599. [Google Scholar] [CrossRef]
- Jia, H.; Chen, X.; Zhang, L.; Chen, M. Cancer associated fibroblasts in cancer development and therapy. J. Hematol. Oncol. 2025, 18, 36. [Google Scholar] [CrossRef]
- Turpin, A.; Neuzillet, C.; Colle, E.; Dusetti, N.; Nicolle, R.; Cros, J.; de Mestier, L.; Bachet, J.-B.; Hammel, P. Therapeutic advances in metastatic pancreatic cancer: A focus on targeted therapies. Ther. Adv. Med. Oncol. 2022, 14, 17588359221118019. [Google Scholar] [CrossRef] [PubMed]
- Bear, A.S.; Vonderheide, R.H.; O’Hara, M.H. Challenges and Opportunities for Pancreatic Cancer Immunotherapy. Cancer Cell 2020, 38, 788–802. [Google Scholar] [CrossRef]
- Qi, Y.; Zhang, L.; Wang, Z.; Kong, X.; Zhai, J.; Fang, Y.; Wang, J. Efficacy and Safety of Anti-PD-1/ PD-L1 Monotherapy for Metastatic Breast Cancer: Clinical Evidence. Front. Pharmacol. 2021, 12, 653521. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Huang, X.; Shi, F.; Song, J.; Guo, C.; Yang, J.; Liang, T.; Bai, X. Combination therapy for pancreatic cancer: Anti-PD-(L)1-based strategy. J. Exp. Clin. Cancer Res. 2022, 41, 56. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Zhou, Y.; Wu, Y.; Shi, M.; Sun, W.; Wang, R. Evaluation of the efficacy and predictive indicators of PD- 1 inhibitors combined with chemotherapy in advanced pancreatic cancer. Sci. Rep. 2025, 15, 12175. [Google Scholar] [CrossRef]
- Ye, X.; Yu, Y.; Zheng, X.; Ma, H. Clinical immunotherapy in pancreatic cancer. Cancer Immunol. Immunother. 2024, 73, 64. [Google Scholar] [CrossRef]
- O’Reilly, E.M.; Oh, D.-Y.; Dhani, N.; Renouf, D.J.; Lee, M.A.; Sun, W.; Fisher, G.; Hezel, A.; Chang, S.-C.; Vlahovic, G.; et al. Durvalumab With or Without Tremelimumab for Patients With Metastatic Pancreatic Ductal Adenocarcinoma: A Phase 2 Randomized Clinical Trial. JAMA Oncol. 2019, 5, 1431–1438. [Google Scholar] [CrossRef]
- Ely, Z.A.; Kulstad, Z.J.; Gunaydin, G.; Addepalli, S.; Verzani, E.K.; Casarrubios, M.; Clauser, K.R.; Wang, X.; Lippincott, I.E.; Louvet, C.; et al. Pancreatic cancer–restricted cryptic antigens are targets for T cell recognition. Science 2025, 388, eadk3487. [Google Scholar] [CrossRef]
- Vigano, S.; Alatzoglou, D.; Irving, M.; Ménétrier-Caux, C.; Caux, C.; Romero, P.; Coukos, G. Targeting Adenosine in Cancer Immunotherapy to Enhance T-Cell Function. Front. Immunol. 2019, 10, 925. [Google Scholar] [CrossRef]
- Lu, Y.; Chen, Q.; Zhu, S.; Gong, X. Hypoxia promotes immune escape of pancreatic cancer cells by lncRNA NNT-AS1/METTL3-HuR-mediated ITGB1 m6A modification. Exp. Cell Res. 2023, 432, 113764. [Google Scholar] [CrossRef]
- Jacoberger-Foissac, C.; Cousineau, I.; Bareche, Y.; Allard, D.; Chrobak, P.; Allard, B.; Pommey, S.; Messaoudi, N.; McNicoll, Y.; Soucy, G.; et al. CD73 Inhibits cGAS–STING and Cooperates with CD39 to Promote Pancreatic Cancer. Cancer Immunol. Res. 2022, 11, 56–71. [Google Scholar] [CrossRef]
- Xia, C.; Yin, S.; To, K.K.W.; Fu, L. CD39/CD73/A2AR pathway and cancer immunotherapy. Mol. Cancer 2023, 22, 44. [Google Scholar] [CrossRef]
- Zhang, F.; Ma, Y.; Li, D.; Wei, J.; Chen, K.; Zhang, E.; Liu, G.; Chu, X.; Liu, X.; Liu, W.; et al. Cancer associated fibroblasts and metabolic reprogramming: Unraveling the intricate crosstalk in tumor evolution. J. Hematol. Oncol. 2024, 17, 80. [Google Scholar] [CrossRef]
- Zheng, R.; Liu, X.; Zhang, Y.; Liu, Y.; Wang, Y.; Guo, S.; Jin, X.; Zhang, J.; Guan, Y.; Liu, Y. Frontiers and future of immunotherapy for pancreatic cancer: From molecular mechanisms to clinical application. Front. Immunol. 2024, 15, 1383978. [Google Scholar] [CrossRef] [PubMed]
- Di Federico, A.; Mosca, M.; Pagani, R.; Carloni, R.; Frega, G.; De Giglio, A.; Rizzo, A.; Ricci, D.; Tavolari, S.; Di Marco, M.; et al. Immunotherapy in Pancreatic Cancer: Why Do We Keep Failing? A Focus on Tumor Immune Microenvironment, Predictive Biomarkers and Treatment Outcomes. Cancers 2022, 14, 2429. [Google Scholar] [CrossRef] [PubMed]
- Muscarella, P.; Bekaii-Saab, T.; McIntyre, K.; Rosemurgy, A.; Ross, S.B.; Richards, D.A.; Fisher, W.E.; Flynn, P.J.; Mattson, A.; Coeshott, C.; et al. A Phase 2 Randomized Placebo-Controlled Adjuvant Trial of GI-4000, a Recombinant Yeast Expressing Mutated RAS Proteins in Patients with Resected Pancreas Cancer. J. Pancreat. Cancer 2021, 7, 8–19. [Google Scholar] [CrossRef]
- Wang, B.; Pei, J.; Xu, S.; Liu, J.; Yu, J. Recent advances in mRNA cancer vaccines: Meeting challenges and embracing opportunities. Front. Immunol. 2023, 14, 1246682. [Google Scholar] [CrossRef] [PubMed]
- Wainberg, Z.A.; Weekes, C.D.; Furqan, M.; Kasi, P.M.; Devoe, C.E.; Leal, A.D.; Chung, V.; Perry, J.R.; Kheoh, T.; McNeil, L.K.; et al. Lymph node-targeted, mKRAS-specific amphiphile vaccine in pancreatic and colorectal cancer: Phase 1 AMPLIFY-201 trial final results. Nat. Med. 2025, 1–6. [Google Scholar] [CrossRef]
- Zhang, F.; Zhong, W.; Li, H.; Huang, K.; Yu, M.; Liu, Y. TP53 Mutational Status-Based Genomic Signature for Prognosis and Predicting Therapeutic Response in Pancreatic Cancer. Front. Cell Dev. Biol. 2021, 9, 665265. [Google Scholar] [CrossRef]
- Marabelle, A.; Le, D.T.; Ascierto, P.A.; Di Giacomo, A.M.; De Jesus-Acosta, A.; Delord, J.-P.; Geva, R.; Gottfried, M.; Penel, N.; Hansen, A.R.; et al. Efficacy of Pembrolizumab in Patients With Noncolorectal High Microsatellite Instability/Mismatch Repair–Deficient Cancer: Results From the Phase II KEYNOTE-158 Study. J. Clin. Oncol. 2020, 38, 1–10. [Google Scholar] [CrossRef]
- Rojas, L.A.; Sethna, Z.; Soares, K.C.; Olcese, C.; Pang, N.; Patterson, E.; Lihm, J.; Ceglia, N.; Guasp, P.; Chu, A.; et al. Personalized RNA neoantigen vaccines stimulate T cells in pancreatic cancer. Nature 2023, 618, 144–150. [Google Scholar] [CrossRef]
- Strickler, J.H.; Satake, H.; George, T.J.; Yaeger, R.; Hollebecque, A.; Garrido-Laguna, I.; Schuler, M.; Burns, T.F.; Coveler, A.L.; Falchook, G.S.; et al. Sotorasib in KRAS p.G12C–Mutated Advanced Pancreatic Cancer. N. Engl. J. Med. 2023, 388, 33–43. [Google Scholar] [CrossRef]
- Leidner, R.; Silva, N.S.; Huang, H.; Sprott, D.; Zheng, C.; Shih, Y.-P.; Leung, A.; Payne, R.; Sutcliffe, K.; Cramer, J.; et al. Neoantigen T-Cell Receptor Gene Therapy in Pancreatic Cancer. N. Engl. J. Med. 2022, 386, 2112–2119. [Google Scholar] [CrossRef]
- Srivastava, A.K.; Guadagnin, G.; Cappello, P.; Novelli, F. Post-Translational Modifications in Tumor-Associated Antigens as a Platform for Novel Immuno-Oncology Therapies. Cancers 2022, 15, 138. [Google Scholar] [CrossRef] [PubMed]
- Xie, N.; Shen, G.; Gao, W.; Huang, Z.; Huang, C.; Fu, L. Neoantigens: Promising targets for cancer therapy. Signal Transduct. Target. Ther. 2023, 8, 9. [Google Scholar] [CrossRef] [PubMed]
- Ge, X.; Zhang, K.; Zhu, J.; Chen, Y.; Wang, Z.; Wang, P.; Xu, P.; Yao, J. Targeting protein modification: A new direction for immunotherapy of pancreatic cancer. Int. J. Biol. Sci. 2025, 21, 63–74. [Google Scholar] [CrossRef] [PubMed]
- Radziejewska, I. Tumor-associated carbohydrate antigens of MUC1—Implication in cancer development. Biomed. Pharmacother. 2024, 174, 116619. [Google Scholar] [CrossRef]
- Rajesh, C.; Radhakrishnan, P. The (Sialyl) Tn antigen: Contributions to immunosuppression in gastrointestinal cancers. Front. Oncol. 2023, 12, 1093496. [Google Scholar] [CrossRef]
- Pienkowski, T.; Wawrzak-Pienkowska, K.; Tankiewicz-Kwedlo, A.; Ciborowski, M.; Kurek, K.; Pawlak, D. Leveraging glycosylation for early detection and therapeutic target discovery in pancreatic cancer. Cell Death Dis. 2025, 16, 227. [Google Scholar] [CrossRef]
- Sreejith, T.; Kamalasanan, K.; Sneha, S.; Keechilat, P.; Harb, H. Advancing Cancer Treatment Through Nanotechnology Driven Immunotherapy for Pancreatic Cancer. ACS Appl. Nano Mater. 2023, 6, 18670–18697. [Google Scholar] [CrossRef]
- Alghamdi, M.; Alasmari, D.; Assiri, A.; Mattar, E.; Aljaddawi, A.A.; Alattas, S.G.; Redwan, E.M. An Overview of the Intrinsic Role of Citrullination in Autoimmune Disorders. J. Immunol. Res. 2019, 2019, 7592851. [Google Scholar] [CrossRef]
- Chen, Y.; Teng, Y.; Xu, P.; Wang, S. The Role of Citrullination Modification in CD4+ T Cells in the Pathogenesis of Immune-Related Diseases. Biomolecules 2024, 14, 400. [Google Scholar] [CrossRef]
- Lee, J.B.; Pyo, K.-H.; Kim, H.R. Role and Function of O-GlcNAcylation in Cancer. Cancers 2021, 13, 5365. [Google Scholar] [CrossRef]
- Zhu, Q.; Zhou, H.; Wu, L.; Lai, Z.; Geng, D.; Yang, W.; Zhang, J.; Fan, Z.; Qin, W.; Wang, Y.; et al. O-GlcNAcylation promotes pancreatic tumor growth by regulating malate dehydrogenase 1. Nat. Chem. Biol. 2022, 18, 1087–1095. [Google Scholar] [CrossRef]
- Li, Y.; Patel, S.P.; Roszik, J.; Qin, Y. Hypoxia-Driven Immunosuppressive Metabolites in the Tumor Microenvironment: New Approaches for Combinational Immunotherapy. Front. Immunol. 2018, 9, 1591. [Google Scholar] [CrossRef] [PubMed]
- Marshall, M.L.; Fung, K.Y.; Jans, D.A.; Wagstaff, K.M. Tumour-specific phosphorylation of serine 419 drives alpha-enolase (ENO1) nuclear export in triple negative breast cancer progression. Cell Biosci. 2024, 14, 1591. [Google Scholar] [CrossRef]
- Tulamaiti, A.; Xiao, S.-Y.; Yang, Y.; Mutailifu, M.; Li, X.-Q.; Yin, S.-Q.; Ma, H.-T.; Yao, H.-F.; Yao, L.-L.; Hu, L.-P.; et al. ENO1 promotes PDAC progression by inhibiting CD8+ T cell infiltration through upregulating PD-L1 expression via HIF-1α signaling. Transl. Oncol. 2025, 52, 102261. [Google Scholar] [CrossRef]
- Belisle, J.A.; Horibata, S.; Jennifer, G.A.; Petrie, S.; Kapur, A.; André, S.; Gabius, H.-J.; Rancourt, C.; Connor, J.; Paulson, J.C.; et al. Identification of Siglec-9 as the receptor for MUC16 on human NK cells, B cells, and monocytes. Mol. Cancer 2010, 9, 118. [Google Scholar] [CrossRef]
- Rosenstock, P.; Kaufmann, T. Sialic Acids and Their Influence on Human NK Cell Function. Cells 2021, 10, 263. [Google Scholar] [CrossRef]
- Guerreiro, A.; Compañón, I.; Lazaris, F.S.; Labão-Almeida, C.; Oroz, P.; Ghirardello, M.; Marques, M.C.; Corzana, F.; Bernardes, G.J.L. Non-Natural MUC1 Glycopeptide Homogeneous Cancer Vaccine with Enhanced Immunogenicity and Therapeutic Activity. Angew. Chem. Int. Ed. Engl. 2024, 63, e202411009. [Google Scholar] [CrossRef]
- Mann, M.; Jensen, O.N. Proteomic analysis of post-translational modifications. Nat. Biotechnol. 2003, 21, 255–261. [Google Scholar] [CrossRef]
- Karpievitch, Y.V.; Polpitiya, A.D.; Anderson, G.A.; Smith, R.D.; Dabney, A.R. Liquid chromatography mass spectrometry-based proteomics: Biological and technological aspects. Ann. Appl. Stat. 2010, 4, 1797–1823. [Google Scholar] [CrossRef]
- Aebersold, R.; Mann, M. Mass-spectrometric exploration of proteome structure and function. Nature 2016, 537, 347–355. [Google Scholar] [CrossRef]
- Slavov, N. Single-cell protein analysis by mass spectrometry. Curr. Opin. Chem. Biol. 2021, 60, 1–9. [Google Scholar] [CrossRef]
- Liu, X.; Arfman, T.; Wichapong, K.; Reutelingsperger, C.P.; Voorberg, J.; Nicolaes, G.A. PAD4 takes charge during neutrophil activation: Impact of PAD4 mediated NET formation on immune-mediated disease. J. Thromb. Haemost. 2021, 19, 1607–1617. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, E.; Boelaars, K.; Brown, K.; Li, R.J.E.; Kruijssen, L.; Bruijns, S.C.M.; van Ee, T.; Schetters, S.T.T.; Crommentuijn, M.H.W.; van der Horst, J.C.; et al. Sialic acids in pancreatic cancer cells drive tumour-associated macrophage differentiation via the Siglec receptors Siglec-7 and Siglec-9. Nat. Commun. 2021, 12, 1270. [Google Scholar] [CrossRef]
- Bhalerao, N.; Chakraborty, A.; Marciel, M.P.; Hwang, J.; Britain, C.M.; Silva, A.D.; Eltoum, I.E.; Jones, R.B.; Alexander, K.L.; Smythies, L.E.; et al. ST6GAL1 sialyltransferase promotes acinar to ductal metaplasia and pancreatic cancer progression. J. Clin. Investig. 2023, 8, e161563. [Google Scholar] [CrossRef]
- Zhu, Q.; Wang, H.; Chai, S.; Xu, L.; Lin, B.; Yi, W.; Wu, L. O-GlcNAcylation promotes tumor immune evasion by inhibiting PD-L1 lysosomal degradation. Proc. Natl. Acad. Sci. USA 2023, 120, e2216796120. [Google Scholar] [CrossRef]
- Zhang, H.-R.; Li, T.-J.; Yu, X.-J.; Liu, C.; Wu, W.-D.; Ye, L.-Y.; Jin, K.-Z. The GFPT2-O-GlcNAcylation-YBX1 axis promotes IL-18 secretion to regulate the tumor immune microenvironment in pancreatic cancer. Cell Death Dis. 2024, 15, 224. [Google Scholar] [CrossRef]
- Uysal-Onganer, P.; D’alessio, S.; Mortoglou, M.; Kraev, I.; Lange, S. Peptidylarginine Deiminase Inhibitor Application, Using Cl-Amidine, PAD2, PAD3 and PAD4 Isozyme-Specific Inhibitors in Pancreatic Cancer Cells, Reveals Roles for PAD2 and PAD3 in Cancer Invasion and Modulation of Extracellular Vesicle Signatures. Int. J. Mol. Sci. 2021, 22, 1396. [Google Scholar] [CrossRef] [PubMed]
- Mahat, D.B.; Kumra, H.; Castro, S.A.; Metcalf, E.; Nguyen, K.; Morisue, R.; Ho, W.W.; Chen, I.; Sullivan, B.; Yim, L.H.; et al. Mutant p53 exploits enhancers to elevate immunosuppressive chemokine expression and impair immune checkpoint inhibitors in pancreatic cancer. Immunity 2025, 58, 1688–1705.e9. [Google Scholar] [CrossRef] [PubMed]
- McCubrey, J.A.; Yang, L.V.; Abrams, S.L.; Steelman, L.S.; Follo, M.Y.; Cocco, L.; Ratti, S.; Martelli, A.M.; Augello, G.; Cervello, M. Effects of TP53 Mutations and miRs on Immune Responses in the Tumor Microenvironment Important in Pancreatic Cancer Progression. Cells 2022, 11, 2155. [Google Scholar] [CrossRef]
- Biederstädt, A.; Hassan, Z.; Schneeweis, C.; Schick, M.; Schneider, L.; Muckenhuber, A.; Hong, Y.; Siegers, G.; Nilsson, L.; Wirth, M.; et al. SUMO pathway inhibition targets an aggressive pancreatic cancer subtype. Gut 2020, 69, 1472–1482. [Google Scholar] [CrossRef]
- Ma, Y.; Xia, P.; Wang, Z.; Xu, J.; Zhang, L.; Jiang, Y. PDIA6 promotes pancreatic cancer progression and immune escape through CSN5-mediated deubiquitination of β-catenin and PD-L1. Neoplasia 2021, 23, 912–928. [Google Scholar] [CrossRef]
- Yang, H.; Zhang, X.; Lao, M.; Sun, K.; He, L.; Xu, J.; Duan, Y.; Chen, Y.; Ying, H.; Li, M.; et al. Targeting ubiquitin-specific protease 8 sensitizes anti-programmed death-ligand 1 immunotherapy of pancreatic cancer. Cell Death Differ. 2022, 30, 560–575. [Google Scholar] [CrossRef] [PubMed]
- Looi, C.-K.; Gan, L.-L.; Sim, W.; Hii, L.-W.; Chung, F.F.-L.; Leong, C.-O.; Lim, W.-M.; Mai, C.-W. Histone Deacetylase Inhibitors Restore Cancer Cell Sensitivity towards T Lymphocytes Mediated Cytotoxicity in Pancreatic Cancer. Cancers 2022, 14, 3709. [Google Scholar] [CrossRef] [PubMed]
- Tan, C.; Li, Y.; Huang, X.; Wei, M.; Huang, Y.; Tang, Z.; Huang, H.; Zhou, W.; Wang, Y.; Hu, J. Extensive protein S-nitrosylation associated with human pancreatic ductal adenocarcinoma pathogenesis. Cell Death Dis. 2019, 10, 914. [Google Scholar] [CrossRef]
- Pereira, P.M.; Edwards, K.J.; Mandleywala, K.; Carter, L.M.; Escorcia, F.E.; Campesato, L.F.; Cornejo, M.; Abma, L.; Mohsen, A.-A.; Iacobuzio-Donahue, C.A.; et al. iNOS Regulates the Therapeutic Response of Pancreatic Cancer Cells to Radiotherapy. Cancer Res. 2020, 80, 1681–1692. [Google Scholar] [CrossRef]
- Suskiewicz, M.J. The logic of protein post-translational modifications (PTMs): Chemistry, mechanisms and evolution of protein regulation through covalent attachments. BioEssays 2024, 46, e2300178. [Google Scholar] [CrossRef]
- Huang, X.; Gan, Z.; Cui, H.; Lan, T.; Liu, Y.; Caron, E.; Shao, W. The SysteMHC Atlas v2.0, an updated resource for mass spectrometry-based immunopeptidomics. Nucleic Acids Res. 2023, 52, D1062–D1071. [Google Scholar] [CrossRef]
- Beatson, R.; Tajadura-Ortega, V.; Achkova, D.; Picco, G.; Tsourouktsoglou, T.-D.; Klausing, S.; Hillier, M.; Maher, D.A.J.; Noll, S.K.T.; Crocker, P.R.; et al. The mucin MUC1 modulates the tumor immunological microenvironment through engagement of the lectin Siglec-9. Nat. Immunol. 2016, 17, 1273–1281. [Google Scholar] [CrossRef]
- Chen, X.; Sandrine, I.K.; Yang, M.; Tu, J.; Yuan, X. MUC1 and MUC16: Critical for immune modulation in cancer therapeutics. Front. Immunol. 2024, 15, 1356913. [Google Scholar] [CrossRef]
- Luo, X.; Chang, S.; Xiao, S.; Peng, Y.; Gao, Y.; Hu, F.; Liang, J.; Xu, Y.; Du, K.; Chen, Y.; et al. PAD4-dependent citrullination of nuclear translocation of GSK3β promotes colorectal cancer progression via the degradation of nuclear CDKN1A. Neoplasia 2022, 33, 100835. [Google Scholar] [CrossRef]
- Brentville, V.; Vankemmelbeke, M.; Metheringham, R.; Durrant, L. Post-translational modifications such as citrullination are excellent targets for cancer therapy. Semin. Immunol. 2020, 47, 101393. [Google Scholar] [CrossRef]
- Ehrentraut, H.; Clambey, E.T.; McNamee, E.N.; Brodsky, K.S.; Ehrentraut, S.F.; Poth, J.M.; Riegel, A.K.; Westrich, J.A.; Colgan, S.P.; Eltzschig, H.K. CD73 + regulatory T cells contribute to adenosine-mediated resolution of acute lung injury. FASEB J. 2013, 27, 2207–2219. [Google Scholar] [CrossRef]
- Zhong, Q.; Xiao, X.; Qiu, Y.; Xu, Z.; Chen, C.; Chong, B.; Zhao, X.; Hai, S.; Li, S.; An, Z.; et al. Protein posttranslational modifications in health and diseases: Functions, regulatory mechanisms, and therapeutic implications. MedComm 2023, 4, e261. [Google Scholar] [CrossRef] [PubMed]
- Dai, X.; Zhang, J.; North, B.J.; Guo, J. Editorial: Post-translational modifications of proteins in cancer immunity and immunotherapy. Front. Immunol. 2022, 13, 1006145. [Google Scholar] [CrossRef] [PubMed]
- Kitamura, N.; Galligan, J.J. A global view of the human post-translational modification landscape. Biochem. J. 2023, 480, 1241–1265. [Google Scholar] [CrossRef]
- Scott, E.; Goode, E.A.; Garnham, R.; Hodgson, K.; Orozco-Moreno, M.; Turner, H.; Livermore, K.; Nangkana, K.P.; Frame, F.M.; Bermudez, A.; et al. ST6GAL1-mediated aberrant sialylation promotes prostate cancer progression. J. Pathol. 2023, 261, 71–84. [Google Scholar] [CrossRef] [PubMed]
- Garnham, R.; Scott, E.; Livermore, K.E.; Munkley, J. ST6GAL1: A key player in cancer (Review). Oncol. Lett. 2019, 18, 983–989. [Google Scholar] [CrossRef]
- Bannoura, S.F.; Khan, H.Y.; Azmi, A.S. KRAS G12D targeted therapies for pancreatic cancer: Has the fortress been conquered? Front. Oncol. 2022, 12, 1013902. [Google Scholar] [CrossRef]
- Doubleday, P.F.; Fornelli, L.; Ntai, I.; Kelleher, N.L. Oncogenic KRAS creates an aspartate metabolism signature in colorectal cancer cells. FEBS J. 2021, 288, 6683–6699. [Google Scholar] [CrossRef] [PubMed]
- Doll, S.; Burlingame, A.L. Mass Spectrometry-Based Detection and Assignment of Protein Posttranslational Modifications. ACS Chem. Biol. 2014, 10, 63–71. [Google Scholar] [CrossRef] [PubMed]
- Silva, A.M.; Vitorino, R.; Domingues, M.M.; Spickett, C.M.; Domingues, P. Post-translational Modifications and Mass Spectrometry Detection. Free Radic. Biol. Med. 2013, 65, 925–941. [Google Scholar] [CrossRef]
- Tabang, D.N.; Ford, M.; Li, L. Recent Advances in Mass Spectrometry-Based Glycomic and Glycoproteomic Studies of Pancreatic Diseases. Front. Chem. 2021, 9, 707387. [Google Scholar] [CrossRef]
- Alvarez-Manilla, G.; Atwood, J.; Guo, Y.; Warren, N.L.; Orlando, R.; Pierce, M. Tools for Glycoproteomic Analysis: Size Exclusion Chromatography Facilitates Identification of Tryptic Glycopeptides with N-linked Glycosylation Sites. J. Proteome Res. 2006, 5, 701–708. [Google Scholar] [CrossRef]
- Ouyang, M.; Yu, C.; Deng, X.; Zhang, Y.; Zhang, X.; Duan, F. O-GlcNAcylation and Its Role in Cancer-Associated Inflammation. Front. Immunol. 2022, 13, 861559. [Google Scholar] [CrossRef]
- Yang, H.; Bailey, P.; Pilarsky, C. CRISPR Cas9 in Pancreatic Cancer Research. Front. Cell Dev. Biol. 2019, 7, 239. [Google Scholar] [CrossRef]
- Jardim-Perassi, B.V.; Irrera, P.; Oluwatola, O.E.; Abrahams, D.; Estrella, V.C.; Ordway, B.; Byrne, S.R.; Ojeda, A.A.; Whelan, C.J.; Kim, J.; et al. L-DOS47 Elevates Pancreatic Cancer Tumor pH and Enhances Response to Immunotherapy. Biomedicines 2024, 12, 461. [Google Scholar] [CrossRef]
- Molvi, Z.; Klatt, M.G.; Dao, T.; Urraca, J.; Scheinberg, D.A.; O’Reilly, R.J. The landscape of MHC-presented phosphopeptides yields actionable shared tumor antigens for cancer immunotherapy across multiple HLA alleles. J. Immunother. Cancer 2023, 11, e006889. [Google Scholar] [CrossRef] [PubMed]
- Mahoney, K.E.; Reser, L.; Cuevas, M.V.R.; Abelin, J.G.; Shabanowitz, J.; Hunt, D.F.; Malaker, S.A. Identification of Post-translationally Modified MHC Class I–Associated Peptides as Potential Cancer Immunotherapeutic Targets. Mol. Cell. Proteom. 2025, 24, 100971. [Google Scholar] [CrossRef]
- León-Letelier, R.A.; Katayama, H.; Hanash, S. Mining the Immunopeptidome for Antigenic Peptides in Cancer. Cancers 2022, 14, 4968. [Google Scholar] [CrossRef]
- Duan, Z.; Shi, R.; Gao, B.; Cai, J. N-linked glycosylation of PD-L1/PD-1: An emerging target for cancer diagnosis and treatment. J. Transl. Med. 2024, 22, 705. [Google Scholar] [CrossRef]
- Rajesh, C.; Cummings, R.D.; Radhakrishnan, P. Unraveling the glyco-immunity nexus in pancreatic cancer. Mol. Cancer 2025, 24, 211. [Google Scholar] [CrossRef]
- Karamitopoulou, E. Tumour microenvironment of pancreatic cancer: Immune landscape is dictated by molecular and histopathological features. Br. J. Cancer 2019, 121, 5–14. [Google Scholar] [CrossRef]
- Estephan, H.; Tailor, A.; Parker, R.; Kreamer, M.; Papandreou, I.; Campo, L.; Easton, A.; Moon, E.J.; Denko, N.C.; Ternette, N.; et al. Hypoxia promotes tumor immune evasion by suppressing MHC-I expression and antigen presentation. EMBO J. 2025, 44, 903–922. [Google Scholar] [CrossRef]
- De Meo, M.L.; Spicer, J.D. The role of neutrophil extracellular traps in cancer progression and metastasis. In Seminars in Immunology; Academic Press: Cambridge, MA, USA, 2021; Volume 57. [Google Scholar] [CrossRef]
- Mitsis, M.; Drosou, P.; Tatsis, V.; Markopoulos, G.S. Neutrophil Extracellular Traps and Pancreatic Cancer Development: A Vicious Cycle. Cancers 2022, 14, 3339. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, A.; Hashimoto, S. Plasticity and Tumor Microenvironment in Pancreatic Cancer: Genetic, Metabolic, and Immune Perspectives. Cancers 2024, 16, 4094. [Google Scholar] [CrossRef] [PubMed]
- Ferrer, C.M.; Lynch, T.P.; Sodi, V.L.; Falcone, J.N.; Schwab, L.P.; Peacock, D.L.; Vocadlo, D.J.; Seagroves, T.N.; Reginato, M.J. O-GlcNAcylation Regulates Cancer Metabolism and Survival Stress Signaling via Regulation of the HIF-1 Pathway. Mol. Cell 2014, 54, 820–831. [Google Scholar] [CrossRef] [PubMed]
- Olivier-Van Stichelen, S.; Dehennaut, V.; Buzy, A.; Zachayus, J.-L.; Guinez, C.; Mir, A.-M.; El Yazidi-Belkoura, I.; Copin, M.-C.; Boureme, D.; Loyaux, D.; et al. O-GlcNAcylation stabilizes β-catenin through direct competition with phosphorylation at threonine 41. FASEB J. 2014, 28, 3325–3338. [Google Scholar] [CrossRef]
- Wang, Y.; Liu, J.; Jin, X.; Zhang, D.; Li, D.; Hao, F.; Feng, Y.; Gu, S.; Meng, F.; Tian, M.; et al. O- GlcNAcylation destabilizes the active tetrameric PKM2 to promote the Warburg effect. Proc. Natl. Acad. Sci. USA 2017, 114, 13732–13737. [Google Scholar] [CrossRef]
- Lu, Q.; Zhang, X.; Liang, T.; Bai, X. O-GlcNAcylation: An important post-translational modification and a potential therapeutic target for cancer therapy. Mol. Med. 2022, 28, 115. [Google Scholar] [CrossRef]
- Lumibao, J.C.; Tremblay, J.R.; Hsu, J.; Engle, D.D. Altered glycosylation in pancreatic cancer and beyond. J. Exp. Med. 2022, 219, e20211505. [Google Scholar] [CrossRef]
- Backe, S.J.; Sager, R.A.; Woodford, M.R.; Makedon, A.M.; Mollapour, M. Post-translational modifications of Hsp90 and translating the chaperone code. J. Biol. Chem. 2020, 295, 11099–11117. [Google Scholar] [CrossRef] [PubMed]
- Bali, P.; Pranpat, M.; Bradner, J.; Balasis, M.; Fiskus, W.; Guo, F.; Rocha, K.; Kumaraswamy, S.; Boyapalle, S.; Atadja, P.; et al. Inhibition of Histone Deacetylase 6 Acetylates and Disrupts the Chaperone Function of Heat Shock Protein 90. J. Biol. Chem. 2005, 280, 26729–26734. [Google Scholar] [CrossRef] [PubMed]
- Scroggins, B.T.; Robzyk, K.; Wang, D.; Marcu, M.G.; Tsutsumi, S.; Beebe, K.; Cotter, R.J.; Felts, S.; Toft, D.; Karnitz, L.; et al. An Acetylation Site in the Middle Domain of Hsp90 Regulates Chaperone Function. Mol. Cell 2007, 25, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Menezes, S.; Okail, M.H.; Jalil, S.M.A.; Kocher, H.M.; Cameron, A.J.M. Cancer-associated fibroblasts in pancreatic cancer: New subtypes, new markers, new targets. J. Pathol. 2022, 257, 526–544. [Google Scholar] [CrossRef]
- Morgan, A.; Griffin, M.; Kameni, L.; Wan, D.C.; Longaker, M.T.; Norton, J.A. Medical Biology of Cancer-Associated Fibroblasts in Pancreatic Cancer. Biology 2023, 12, 1044. [Google Scholar] [CrossRef]
- Zou, S.; Tong, Q.; Liu, B.; Huang, W.; Tian, Y.; Fu, X. Targeting STAT3 in Cancer Immunotherapy. Mol. Cancer 2020, 19, 145. [Google Scholar] [CrossRef]
- Demel, U.M.; Böger, M.; Yousefian, S.; Grunert, C.; Zhang, L.; Hotz, P.W.; Gottschlich, A.; Köse, H.; Isaakidis, K.; Vonficht, D.; et al. Activated SUMOylation restricts MHC class I antigen presentation to confer immune evasion in cancer. J. Clin. Investig. 2022, 132, e152383. [Google Scholar] [CrossRef]
- Miller-Ocuin, J.L.; Liang, X.; Boone, B.A.; Doerfler, W.R.; Singhi, A.D.; Tang, D.; Kang, R.; Lotze, M.T.; Zeh, H.J., III. DNA released from neutrophil extracellular traps (NETs) activates pancreatic stellate cells and enhances pancreatic tumor growth. OncoImmunology 2019, 8, e1605822. [Google Scholar] [CrossRef]
- Deng, H.; Lin, C.; Garcia-Gerique, L.; Fu, S.; Cruz, Z.; Bonner, E.E.; Rosenwasser, M.; Rajagopal, S.; Sadhu, M.N.; Gajendran, C.; et al. A Novel Selective Inhibitor JBI-589 Targets PAD4-Mediated Neutrophil Migration to Suppress Tumor Progression. Cancer Res. 2022, 82, 3561–3572. [Google Scholar] [CrossRef]
- Wang, Y.; Yang, K.; Li, J.; Wang, C.; Li, P.; Du, L. Neutrophil extracellular traps in cancer: From mechanisms to treatments. Clin. Transl. Med. 2025, 15, e70368. [Google Scholar] [CrossRef]
- Ortega-Batista, A.; Jaén-Alvarado, Y.; Moreno-Labrador, D.; Gómez, N.; García, G.; Guerrero, E.N. Single-Cell Sequencing: Genomic and Transcriptomic Approaches in Cancer Cell Biology. Int. J. Mol. Sci. 2025, 26, 2074. [Google Scholar] [CrossRef]
- Liu, J.; Xu, X.; Zhong, H.; Yu, M.; Abuduaini, N.; Zhang, S.; Yang, X.; Feng, B. Glycosylation and Its Role in Immune Checkpoint Proteins: From Molecular Mechanisms to Clinical Implications. Biomedicines 2024, 12, 1446. [Google Scholar] [CrossRef] [PubMed]
- Kufe, D.W. MUC1-C oncoprotein as a target in breast cancer: Activation of signaling pathways and therapeutic approaches. Oncogene 2012, 32, 1073–1081. [Google Scholar] [CrossRef]
- Zhu, D.; Lu, Y.; Wang, Y.; Wang, Y. PAD4 and Its Inhibitors in Cancer Progression and Prognosis. Pharmaceutics 2022, 14, 2414. [Google Scholar] [CrossRef] [PubMed]
- Tao, J.; Yang, G.; Zhou, W.; Qiu, J.; Chen, G.; Luo, W.; Zhao, F.; You, L.; Zheng, L.; Zhang, T.; et al. Targeting hypoxic tumor microenvironment in pancreatic cancer. J. Hematol. Oncol. 2021, 14, 14. [Google Scholar] [CrossRef]
- Du, L.; Lee, J.-H.; Jiang, H.; Wang, C.; Wang, S.; Zheng, Z.; Shao, F.; Xu, D.; Xia, Y.; Li, J.; et al. β-Catenin induces transcriptional expression of PD-L1 to promote glioblastoma immune evasion. J. Exp. Med. 2020, 217, e20191115. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Jenkins, R.W.; Sullivan, R.J. Mechanisms of Resistance to Immune Checkpoint Blockade. Am. J. Clin. Dermatol. 2018, 20, 41–54. [Google Scholar] [CrossRef]
- Kwee, S.A.; Tiirikainen, M. Beta-catenin activation and immunotherapy resistance in hepatocellular carcinoma: Mechanisms and biomarkers. Hepatoma Res. 2021, 2021, 8. [Google Scholar] [CrossRef]
- Griesemer, A.D.; Sorenson, E.C.; Hardy, M.A. The Role of the Thymus in Tolerance. Transplantation 2010, 90, 465–474. [Google Scholar] [CrossRef]
- Zhai, J.; Gu, X.; Liu, Y.; Hu, Y.; Jiang, Y.; Zhang, Z. Chemotherapeutic and targeted drugs-induced immunogenic cell death in cancer models and antitumor therapy: An update review. Front. Pharmacol. 2023, 14, 1152934. [Google Scholar] [CrossRef]
- Borrello, M.G.; Degl’innocenti, D.; Pierotti, M.A. Inflammation and cancer: The oncogene-driven connection. Cancer Lett. 2008, 267, 262–270. [Google Scholar] [CrossRef]
- Peng, H.; James, C.A.; Cullinan, D.R.; Hogg, G.D.; Mudd, J.L.; Zuo, C.; Takchi, R.; Caldwell, K.E.; Liu, J.; DeNardo, D.G.; et al. Neoadjuvant FOLFIRINOX Therapy Is Associated with Increased Effector T Cells and Reduced Suppressor Cells in Patients with Pancreatic Cancer. Clin. Cancer Res. 2021, 27, 6761–6771. [Google Scholar] [CrossRef]
- Mowen, K.A.; David, M. Unconventional post-translational modifications in immunological signaling. Nat. Immunol. 2014, 15, 512–520. [Google Scholar] [CrossRef] [PubMed]
- De Sanctis, F.; Sandri, S.; Ferrarini, G.; Pagliarello, I.; Sartoris, S.; Ugel, S.; Marigo, I.; Molon, B.; Bronte, V. The Emerging Immunological Role of Post-Translational Modifications by Reactive Nitrogen Species in Cancer Microenvironment. Front. Immunol. 2014, 5, 69. [Google Scholar] [CrossRef] [PubMed]
- Brentville, V.A.; Metheringham, R.L.; Daniels, I.; Atabani, S.; Symonds, P.; Cook, K.W.; Vankemmelbeke, M.; Choudhury, R.; Vaghela, P.; Gijon, M.; et al. Combination vaccine based on citrullinated vimentin and enolase peptides induces potent CD4-mediated anti-tumor responses. J. Immunother. Cancer 2020, 8, e000560. [Google Scholar] [CrossRef]
- Imamura, T.; Ashida, R.; Ohshima, K.; Uesaka, K.; Sugiura, T.; Ohgi, K.; Yamada, M.; Otsuka, S.; Hatakeyama, K.; Nagashima, T.; et al. Characterization of pancreatic cancer with ultra-low tumor mutational burden. Sci. Rep. 2023, 13, 4359. [Google Scholar] [CrossRef] [PubMed]
- Lui, I.; Schaefer, K.; Kirkemo, L.L.; Zhou, J.; Perera, R.M.; Leung, K.K.; Wells, J.A. Hypoxia Induces Extensive Protein and Proteolytic Remodeling of the Cell Surface in Pancreatic Adenocarcinoma (PDAC) Cell Lines. J. Proteome Res. 2025, 24, 2791–2800. [Google Scholar] [CrossRef]
- Li, K.; Yuan, J.; Trafton, D.; Wang, J.; Niu, N.; Yuan, C.; Liu, X.; Zheng, L. Pancreatic ductal adenocarcinoma immune microenvironment and immunotherapy prospects. Chronic Dis. Transl. Med. 2020, 6, 6–17. [Google Scholar] [CrossRef]
- Kroemer, G.; Galluzzi, L.; Kepp, O.; Zitvogel, L. Immunogenic Cell Death in Cancer Therapy. Annu. Rev. Immunol. 2013, 31, 51–72. [Google Scholar] [CrossRef] [PubMed]
- Lau, A.N.; Heiden, M.G.V. Metabolism in the Tumor Microenvironment. Annu. Rev. Cancer Biol. 2020, 4, 17–40. [Google Scholar] [CrossRef]
- Ying, H.; Kimmelman, A.C.; Lyssiotis, C.A.; Hua, S.; Chu, G.C.; Fletcher-Sananikone, E.; Locasale, J.W.; Son, J.; Zhang, H.; Coloff, J.L.; et al. Oncogenic Kras Maintains Pancreatic Tumors through Regulation of Anabolic Glucose Metabolism. Cell 2012, 149, 656–670. [Google Scholar] [CrossRef]
- Guillaumond, F.; Leca, J.; Olivares, O.; Lavaut, M.-N.; Vidal, N.; Berthezène, P.; Dusetti, N.J.; Loncle, C.; Calvo, E.; Turrini, O.; et al. Strengthened glycolysis under hypoxia supports tumor symbiosis and hexosamine biosynthesis in pancreatic adenocarcinoma. Proc. Natl. Acad. Sci. USA 2013, 110, 3919–3924. [Google Scholar] [CrossRef] [PubMed]
- Rohrbach, A.S.; Slade, D.J.; Thompson, P.R.; Mowen, K.A. Activation of PAD4 in NET formation. Front. Immunol. 2012, 3, 360. [Google Scholar] [CrossRef]
- Karamitopoulou, E.; Wenning, A.S.; Acharjee, A.; Aeschbacher, P.; Marinoni, I.; Zlobec, I.; Gloor, B.; Perren, A. Spatial Heterogeneity of Immune Regulators Drives Dynamic Changes in Local Immune Responses, Affecting Disease Outcomes in Pancreatic Cancer. Clin. Cancer Res. 2024, 30, 4215–4226. [Google Scholar] [CrossRef]
- Xia, Y.; Ma, J.; Yang, X.; Liu, D.; Zhu, Y.; Zhao, Y.; Fei, X.; Xu, D.; Dai, J. Identifying the Spatial Architecture That Restricts the Proximity of CD8+ T Cells to Tumor Cells in Pancreatic Ductal Adenocarcinoma. Cancers 2024, 16, 1434. [Google Scholar] [CrossRef]
- Sethumadhavan, S.; Silva, M.; Philbrook, P.; Nguyen, T.; Hatfield, S.M.; Ohta, A.; Sitkovsky, M.V. Hypoxia and hypoxia-inducible factor (HIF) downregulate antigen-presenting MHC class I molecules limiting tumor cell recognition by T cells. PLoS ONE 2017, 12, e0187314. [Google Scholar] [CrossRef]
- Lyman, M.R.; Mitchell, J.T.; Raghavan, S.; Kagohara, L.T.; Huff, A.L.; Haldar, S.D.; Shin, S.M.; Guinn, S.; Barrett, B.; Longway, G.; et al. Spatial Proteomics and Transcriptomics Reveal Early Immune Cell Organization in Pancreatic Intraepithelial Neoplasia. J. Clin. Investig. 2025, 10, e191595. [Google Scholar] [CrossRef]
- Zhu, D.; Zhang, Y.; Wang, S. Histone citrullination: A new target for tumors. Mol. Cancer 2021, 20, 90. [Google Scholar] [CrossRef]
- Rappu, P.; Suwal, U.; Siljamäki, E.; Heino, J. Inflammation-related citrullination of matrisome proteins in human cancer. Front. Oncol. 2022, 12, 1035188. [Google Scholar] [CrossRef]
- Zhu, T.; Yang, Q.; Qian, X.; Wu, X.; Fang, J.; Lin, Y.; Feng, Y.; Gao, J.; Xia, Q. GPRC5A/CXCL8/NLRP3-mediated neutrophil extracellular traps drive gemcitabine-nab-paclitaxel resistance in pancreatic adenocarcinoma. Cancer Biol. Med. 2025, 22, 832–853. [Google Scholar] [CrossRef]
- Boelaars, K.; Rodriguez, E.; Huinen, Z.R.; Liu, C.; Wang, D.; Springer, B.O.; Olesek, K.; Goossens-Kruijssen, L.; van Ee, T.; Lindijer, D.; et al. Pancreatic cancer-associated fibroblasts modulate macrophage differentiation via sialic acid-Siglec interactions. Commun. Biol. 2024, 7, 430. [Google Scholar] [CrossRef] [PubMed]
- Jiang, K.-Y.; Qi, L.-L.; Kang, F.-B.; Wang, L. The intriguing roles of Siglec family members in the tumor microenvironment. Biomark. Res. 2022, 10, 22. [Google Scholar] [CrossRef]
- van Houtum, E.J.H.; Büll, C.; Cornelissen, L.A.M.; Adema, G.J. Siglec Signaling in the Tumor Microenvironment. Front. Immunol. 2021, 12, 790317. [Google Scholar] [CrossRef]
- Peng, L.; Wang, D.; Han, Y.; Huang, T.; He, X.; Wang, J.; Ou, C. Emerging Role of Cancer-Associated Fibroblasts-Derived Exosomes in Tumorigenesis. Front. Immunol. 2022, 12, 795372. [Google Scholar] [CrossRef]
- Nedaeinia, R.; Najafgholian, S.; Salehi, R.; Goli, M.; Ranjbar, M.; Nickho, H.; Javanmard, S.H.; Ferns, G.A.; Manian, M. The role of cancer-associated fibroblasts and exosomal miRNAs-mediated intercellular communication in the tumor microenvironment and the biology of carcinogenesis: A systematic review. Cell Death Discov. 2024, 10, 380. [Google Scholar] [CrossRef] [PubMed]
- Silva, A.D.; Hwang, J.; Marciel, M.P.; Bellis, S.L. The pro-inflammatory cytokines IL-1β and IL-6 promote upregulation of the ST6GAL1 sialyltransferase in pancreatic cancer cells. J. Biol. Chem. 2024, 300, 107752. [Google Scholar] [CrossRef]
- Berglund, A.K.; Hinson, A.L.; Schnabel, L.V. TGF-β downregulates antigen processing and presentation genes and MHC I surface expression through a Smad3-dependent mechanism. bioRxiv 2023. [Google Scholar] [CrossRef]
- Gu, Y.; Fang, Y.; Wu, X.; Xu, T.; Hu, T.; Xu, Y.; Ma, P.; Wang, Q.; Shu, Y. The emerging roles of SUMOylation in the tumor microenvironment and therapeutic implications. Exp. Hematol. Oncol. 2023, 12, 58. [Google Scholar] [CrossRef]
- Park, S.; Paszek, M. Abstract 1549: Mucins form a nanoscale material barrier against immune cell attack. J. Biol. Chem. 2023, 299, S390. [Google Scholar] [CrossRef]
- Lustig, M.; Chan, C.; Jansen, J.H.M.; Bräutigam, M.; Kölling, M.A.; Gehlert, C.L.; Baumann, N.; Mester, S.; Foss, S.; Andersen, J.T.; et al. Disruption of the sialic acid/Siglec-9 axis improves antibody-mediated neutrophil cytotoxicity towards tumor cells. Front. Immunol. 2023, 14, 1178817. [Google Scholar] [CrossRef]
- Dobie, C.; Skropeta, D. Insights into the role of sialylation in cancer progression and metastasis. Br. J. Cancer 2020, 124, 76–90. [Google Scholar] [CrossRef] [PubMed]
- Boelaars, K.; van Kooyk, Y. Targeting myeloid cells for cancer immunotherapy: Siglec-7/9/10/15 and their ligands. Trends Cancer 2023, 10, 230–241. [Google Scholar] [CrossRef] [PubMed]
- Patskovsky, Y.; Natarajan, A.; Patskovska, L.; Nyovanie, S.; Joshi, B.; Morin, B.; Brittsan, C.; Huber, O.; Gordon, S.; Michelet, X.; et al. Molecular mechanism of phosphopeptide neoantigen immunogenicity. Nat. Commun. 2023, 14, 3763. [Google Scholar] [CrossRef] [PubMed]
- Apoorvi, T.; Yury, P.; Iryna, V.; Michelle, K. Phosphopeptide Neoantigens as Emerging Targets in Cancer Immunotherapy. J. Cancer Immunol. 2024, 6, 135–147. [Google Scholar] [CrossRef]
- Koning, T.; Cordova, F.; Aguilar, G.; Sarmiento, J.; Mardones, G.A.; Boric, M.; Varas-Godoy, M.; Lladser, A.; Duran, W.N.; Ehrenfeld, P.; et al. S-Nitrosylation in endothelial cells contributes to tumor cell adhesion and extravasation during breast cancer metastasis. Biol. Res. 2023, 56, 51. [Google Scholar] [CrossRef]
- Chen, C.-Y.; Lin, Y.-S.; Chen, C.-H.; Chen, Y.-J. Annexin A2-mediated cancer progression and therapeutic resistance in nasopharyngeal carcinoma. J. Biomed. Sci. 2018, 25, 30. [Google Scholar] [CrossRef]
- Shi, H.; Han, X.; Sun, Y.; Shang, C.; Wei, M.; Ba, X.; Zeng, X. Chemokine (C-X-C motif) ligand 1 and CXCL2 produced by tumor promote the generation of monocytic myeloid-derived suppressor cells. Cancer Sci. 2018, 109, 3826–3839. [Google Scholar] [CrossRef]
- Smith, L.E.; Rogowska-Wrzesinska, A. The challenge of detecting modifications on proteins. Essays Biochem. 2020, 64, 135–153. [Google Scholar] [CrossRef]
- Pinkse, M.; Evaristo, G.; Pieterse, M.; Yu, Y.; Verhaert, P. MS approaches to select peptides with post-translational modifications from amphibian defense secretions prior to full sequence elucidation. EuPA Open Proteom. 2014, 5, 32–40. [Google Scholar] [CrossRef]
- Geiszler, D.J.; Polasky, D.A.; Yu, F.; Nesvizhskii, A.I. Detecting diagnostic features in MS/MS spectra of post-translationally modified peptides. Nat. Commun. 2023, 14, 4132. [Google Scholar] [CrossRef]
- Bons, J.; Hunter, C.L.; Chupalov, R.; Causon, J.; Antonoplis, A.; Rose, J.; MacLean, B.; Schilling, B. Localization and Quantification of Post-Translational Modifications of Proteins Using Electron Activated Dissociation Fragmentation on a Fast-Acquisition Time-of-Flight Mass Spectrometer. J. Am. Soc. Mass Spectrom. 2023, 34, 2199–2210. [Google Scholar] [CrossRef]
- Ma, J.; Hart, G.W. O-GlcNAc profiling: From proteins to proteomes. Clin. Proteom. 2014, 11, 8. [Google Scholar] [CrossRef]
- Udeshi, N.D.; Hart, G.W.; Slawson, C. From Fringe to the Mainstream: How ETD MS Brought O-GlcNAc to the Masses. Mol. Cell. Proteom. 2024, 23, 100859. [Google Scholar] [CrossRef] [PubMed]
- Burt, R.A.; Alghusen, I.M.; Ephrame, S.J.; Villar, M.T.; Artigues, A.; Slawson, C. Mapping the O-GlcNAc Modified Proteome: Applications for Health and Disease. Front. Mol. Biosci. 2022, 9, 920727. [Google Scholar] [CrossRef]
- Mechref, Y.; Madera, M.; Novotny, M.V. Glycoprotein enrichment through lectin affinity techniques. Methods Mol. Biol. 2008, 424, 373–396. [Google Scholar] [CrossRef]
- Wu, F.; Li, W.; Lu, H.; Li, L. Recent Advances in Mass Spectrometry-Based Studies of Post-Translational Modifications in Alzheimer’s Disease. Mol. Cell. Proteom. 2025, 24, 101003. [Google Scholar] [CrossRef]
- Morgenstern, D.; Wolf-Levy, H.; Tickotsky-Moskovitz, N.; Cooper, I.; Buchman, A.S.; Bennett, D.A.; Beeri, M.S.; Levin, Y. Optimized Glycopeptide Enrichment Method–It Is All About the Sauce. Anal. Chem. 2022, 94, 10308–10313. [Google Scholar] [CrossRef]
- Flender, D.; Vilenne, F.; Adams, C.; Boonen, K.; Valkenborg, D.; Baggerman, G. Exploring the dynamic landscape of immunopeptidomics: Unravelling posttranslational modifications and navigating bioinformatics terrain. Mass Spectrom. Rev. 2024, 44, 599–629. [Google Scholar] [CrossRef]
- Arshad, S.; Cameron, B.; Joglekar, A.V. Immunopeptidomics for autoimmunity: Unlocking the chamber of immune secrets. npj Syst. Biol. Appl. 2025, 11, 10. [Google Scholar] [CrossRef] [PubMed]
- Pongcharoen, S.; Kaewsringam, N.; Somaparn, P.; Roytrakul, S.; Maneerat, Y.; Pintha, K.; Topanurak, S. Immunopeptidomics in the cancer immunotherapy era. Explor. Target. Anti Tumor Ther. 2024, 5, 801–817. [Google Scholar] [CrossRef]
- Brown, R.; Stuart, S.S.; Houel, S.; Ahn, N.G.; Old, W.M. Large-Scale Examination of Factors Influencing Phosphopeptide Neutral Loss during Collision Induced Dissociation. J. Am. Soc. Mass Spectrom. 2015, 26, 1128–1142. [Google Scholar] [CrossRef]
- Potel, C.M.; Lemeer, S.; Heck, A.J.R. Phosphopeptide Fragmentation and Site Localization by Mass Spec-trometry: An Update. Anal. Chem. 2018, 91, 126–141. [Google Scholar]
- Myers, S.A.; Daou, S.; Affar, E.B.; Burlingame, A. Electron transfer dissociation (ETD): The mass spectrometric breakthrough essential for O-GlcNAc protein site assignments—A study of the O-GlcNAcylated protein Host Cell Factor C1. Proteomics 2013, 13, 982–991. [Google Scholar] [CrossRef]
- Riley, N.M.; Malaker, S.A.; Driessen, M.D.; Bertozzi, C.R. Optimal Dissociation Methods Differ for N- and O-Glycopeptides. J. Proteome Res. 2020, 19, 3286–3301. [Google Scholar] [CrossRef] [PubMed]
- Riley, N.M.; Sikora, J.W.; Seckler, H.S.; Greer, J.B.; Fellers, R.T.; LeDuc, R.D.; Westphall, M.S.; Thomas, P.M.; Kelleher, N.L.; Coon, J.J. The Value of Activated Ion Electron Transfer Dissociation for High-Throughput Top-Down Characterization of Intact Proteins. Anal. Chem. 2018, 90, 8553–8560. [Google Scholar] [CrossRef]
- Kessler, A.L.; Fort, K.L.; Resemann, H.C.; Krüger, P.; Wang, C.; Koch, H.; Hauschild, J.-P.; Marino, F.; Heck, A.J. Increased EThcD Efficiency on the Hybrid Orbitrap Excedion Pro Mass Analyzer Extends the Depth in Identification and Sequence Coverage of HLA Class I Immunopeptidomes. Mol. Cell. Proteom. 2025, 24, 101049. [Google Scholar] [CrossRef]
- Qi, Y.A.; Maity, T.K.; Cultraro, C.M.; Misra, V.; Zhang, X.; Ade, C.; Gao, S.; Milewski, D.; Nguyen, K.D.; Ebrahimabadi, M.H.; et al. Proteogenomic Analysis Unveils the HLA Class I-Presented Immunopeptidome in Melanoma and EGFR-Mutant Lung Adenocarcinoma. Mol. Cell. Proteom. 2021, 20, 100136. [Google Scholar] [CrossRef]
- Yang, K.L.; Yu, F.; Teo, G.C.; Li, K.; Demichev, V.; Ralser, M.; Nesvizhskii, A.I. MSBooster: Improving peptide identification rates using deep learning-based features. Nat. Commun. 2023, 14, 4539. [Google Scholar] [CrossRef]
- Sandalova, T.; Sala, B.M.; Achour, A. Structural aspects of chemical modifications in the MHC-restricted immunopeptidome; Implications for immune recognition. Front. Chem. 2022, 10, 861609. [Google Scholar] [CrossRef]
- Purcell, A.W.; van Driel, I.R.; Gleeson, P.A. Impact of glycans on T-cell tolerance to glycosylated self-antigens. Immunol. Cell Biol. 2008, 86, 574–579. [Google Scholar] [CrossRef] [PubMed]
- Schnaar, R.L. Glycans and glycan-binding proteins in immune regulation: A concise introduction to glycobiology for the allergist. J. Allergy Clin. Immunol. 2015, 135, 609–615. [Google Scholar] [CrossRef] [PubMed]
- van Kooyk, Y.; Rabinovich, G.A. Protein-glycan interactions in the control of innate and adaptive immune responses. Nat. Immunol. 2008, 9, 593–601. [Google Scholar] [CrossRef] [PubMed]
- Yu, Q.; Wang, B.; Chen, Z.; Urabe, G.; Glover, M.S.; Shi, X.; Guo, L.-W.; Kent, K.C.; Li, L. Electron-Transfer/Higher-Energy Collision Dissociation (EThcD)-Enabled Intact Glycopeptide/Glycoproteome Characterization. J. Am. Soc. Mass Spectrom. 2017, 28, 1751–1764. [Google Scholar] [CrossRef]
- Baliban, R.C.; DiMaggio, P.A.; Plazas-Mayorca, M.D.; Young, N.L.; Garcia, B.A.; Floudas, C.A. A Novel Approach for Untargeted Post-translational Modification Identification Using Integer Linear Optimization and Tandem Mass Spectrometry. Mol. Cell. Proteom. 2010, 9, 764–779. [Google Scholar] [CrossRef]
- Steckel, A.; Uray, K.; Schlosser, G. Detection of protein posttranslational modifications by mass spectrometry. In Amino Acids, Peptides and Proteins; Ryadnov, M., Hudecz, F., Eds.; The Royal Society of Chemistry: London, UK, 2020; Volume 44, pp. 140–170. [Google Scholar]
- Rebak, A.S.; Hendriks, I.A.; Nielsen, M.L. Characterizing citrullination by mass spectrometry-based proteomics. Philos. Trans. R. Soc. B Biol. Sci. 2023, 378, 20220237. [Google Scholar] [CrossRef] [PubMed]
- Kacen, A.; Javitt, A.; Kramer, M.P.; Morgenstern, D.; Tsaban, T.; Shmueli, M.D.; Teo, G.C.; Leprevost, F.d.V.; Barnea, E.; Yu, F.; et al. Post-translational modifications reshape the antigenic landscape of the MHC I immunopeptidome in tumors. Nat. Biotechnol. 2022, 41, 239–251. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, J.B.; Kaabinejadian, S.; Yari, H.; Peters, B.; Barra, C.; Gragert, L.; Hildebrand, W.; Nielsen, M. Machine learning reveals limited contribution of trans-only encoded variants to the HLA-DQ immunopeptidome. Commun. Biol. 2023, 6, 442. [Google Scholar] [CrossRef]
- Wilhelm, M.; Zolg, D.P.; Graber, M.; Gessulat, S.; Schmidt, T.; Schnatbaum, K.; Schwencke-Westphal, C.; Seifert, P.; Krätzig, N.d.A.; Zerweck, J.; et al. Deep learning boosts sensitivity of mass spectrometry-based immunopeptidomics. Nat. Commun. 2021, 12, 3346. [Google Scholar] [CrossRef] [PubMed]
- Yi, X.; Liao, Y.; Wen, B.; Li, K.; Dou, Y.; Savage, S.R.; Zhang, B. caAtlas: An immunopeptidome atlas of human cancer. iScience 2021, 24, 103107. [Google Scholar] [CrossRef]
- Wen, B.; Wang, C.; Li, K.; Han, P.; Holt, M.V.; Savage, S.R.; Lei, J.T.; Dou, Y.; Shi, Z.; Li, Y.; et al. DeepMVP: Deep learning models trained on high-quality data accurately predict PTM sites and variant-induced alterations. Nat. Methods 2025, 22, 1857–1867. [Google Scholar] [CrossRef]
- Wang, J.; Tao, X.; Zhu, J.; Dai, Z.; Du, Y.; Xie, Y.; Chu, X.; Fu, G.; Lei, Z. Tumor organoid-immune co-culture models: Exploring a new perspective of tumor immunity. Cell Death Discov. 2025, 11, 195. [Google Scholar] [CrossRef] [PubMed]
- Dijkstra, K.K.; Cattaneo, C.M.; Weeber, F.; Chalabi, M.; Van De Haar, J.; Fanchi, L.F.; Slagter, M.; Van Der Velden, D.L.; Kaing, S.; Kelderman, S.; et al. Generation of Tumor-Reactive T Cells by Co-culture of Peripheral Blood Lymphocytes and Tumor Organoids. Cell 2018, 174, 1586–1598.e12. [Google Scholar] [CrossRef]
- Moravec, Z.; Zhao, Y.; Voogd, R.; Cook, D.R.; Kinrot, S.; Capra, B.; Yang, H.; Raud, B.; Ou, J.; Xuan, J.; et al. Discovery of tumor-reactive T cell receptors by massively parallel library synthesis and screening. Nat. Biotechnol. 2024, 43, 214–222. [Google Scholar] [CrossRef]
- Wang, X.; Song, X.; Li, Y.; Ding, Y.; Yin, C.; Ren, T.; Zhang, W. Integrated system for screening tumor-specific TCRs, epitopes, and HLA subtypes using single-cell sequencing data. J. Immunother. Cancer 2025, 13, e012029. [Google Scholar] [CrossRef]
- Kuilman, T.; Schrikkema, D.S.; Gadiot, J.; Gomez-Eerland, R.; Bies, L.; Walker, J.; Spaapen, R.M.; Kok, H.; Houg, D.; Viyacheva, M.; et al. Enabling next-generation engineered TCR-T therapies based on high-throughput TCR discovery from diagnostic tumor biopsies. Nat. Commun. 2025, 16, 649. [Google Scholar] [CrossRef]
- Ramanathan, R.K.; Lee, K.M.; McKolanis, J.; Hitbold, E.; Schraut, W.; Moser, A.J.; Warnick, E.; Whiteside, T.; Osborne, J.; Kim, H.; et al. Phase I study of a MUC1 vaccine composed of different doses of MUC1 peptide with SB-AS2 adjuvant in resected and locally advanced pancreatic cancer. Cancer Immunol. Immunother. 2004, 54, 254–264. [Google Scholar] [CrossRef] [PubMed]
- Engelhard, V.H.; Obeng, R.C.; Cummings, K.L.; Petroni, G.R.; Ambakhutwala, A.L.; Chianese-Bullock, K.A.; Smith, K.T.; Lulu, A.; Varhegyi, N.; Smolkin, M.E.; et al. MHC-restricted phosphopeptide antigens: Preclinical validation and first-in-humans clinical trial in participants with high-risk melanoma. J. Immunother. Cancer 2020, 8, e000262. [Google Scholar] [CrossRef] [PubMed]
- Gutierrez, M.; Hamid, O.; Shum, E.; Wise, D.R.; Balar, A.V.; Weber, J.S.; LoRusso, P.; Shafi, S.; Rimm, D.L.; Tolcher, A.W.; et al. Trial in progress: A phase I/II, open-label, dose-escalation, safety and tolerability study of NC318 in subjects with advanced or metastatic solid tumors. J. Clin. Oncol. 2020, 38, TPS3166. [Google Scholar] [CrossRef]
- Assouline, S.E.; Mehta, A.; Hanel, W.; Doucet, S.; Johnston, P.B.; Danilov, A.; Cooper, B.W.; Chudnovsky, A.; Ding, J.; Long, T.; et al. Phase I/II Study of Subasumstat (TAK-981) in Combination With Rituximab in Relapsed/Refractory Non-Hodgkin Lymphoma. Clin. Lymphoma Myeloma Leuk. 2025, 25, 788–799.e11. [Google Scholar] [CrossRef] [PubMed]
- Ottensmeier, C.H.; Pinato, D.J.J.; Armstrong, A.C.; Symeonides, S.N.; Patel, P.M.; Danson, S.; Korolewicz, J.; Cameron, D.; Miller, R.M.; Master, F.; et al. Modi-1, anti-citrullinated neoepitope vaccine, alone and combined with checkpoint inhibitors in patients with head and neck, breast, renal, and ovarian cancers: ModiFy phase I/II basket clinical trial—Report after completion of monotherapy dose-finding. J. Clin. Oncol. 2023, 41, 2566. [Google Scholar] [CrossRef]
- Durrant, L.G.; Masters, F.; Paston, S.; Miller, R.; Pinato, D.J.; Herbertson, R.; Armstrong, A.; Symeonides, S.; Ottensmeier, C. Abstract CT256: Modi-1, anti-citrullinated neoepitope vaccine alone and combined with checkpoint inhibitors in patients with head and neck, breast, renal and ovarian carcinoma: Protocol for the ModiFY phase I/II basket clinical Ttial. Cancer Res. 2023, 83, CT256. [Google Scholar] [CrossRef]
- Penny, S.A.; Abelin, J.G.; Malaker, S.A.; Myers, P.T.; Saeed, A.Z.; Steadman, L.G.; Bai, D.L.; Ward, S.T.; Shabanowitz, J.; Hunt, D.F.; et al. Tumor Infiltrating Lymphocytes Target HLA-I Phosphopeptides Derived From Cancer Signaling in Colorectal Cancer. Front. Immunol. 2021, 12, 723566. [Google Scholar] [CrossRef]
- Lepisto, A.J.; Moser, A.J.; Zeh, H.; Lee, K.; Bartlett, D.; McKolanis, J.R.; Geller, B.A.; Schmotzer, A.; Potter, D.P.; Whiteside, T.; et al. A phase I/II study of a MUC1 peptide pulsed autologous dendritic cell vaccine as adjuvant therapy in patients with resected pancreatic and biliary tumors. Cancer Ther. 2008, 6, 955–964. [Google Scholar]
- Ota, S.; Miyashita, M.; Yamagishi, Y.; Ogasawara, M. Baseline immunity predicts prognosis of pancreatic cancer patients treated with WT1 and/or MUC1 peptide-loaded dendritic cell vaccination and a standard chemotherapy. Hum. Vaccines Immunother. 2021, 17, 5563–5572. [Google Scholar] [CrossRef]
- McGinty, J.W.; Marré, M.L.; Bajzik, V.; Piganelli, J.D.; James, E.A. T Cell Epitopes and Post-Translationally Modified Epitopes in Type 1 Diabetes. Curr. Diabetes Rep. 2015, 15, 90. [Google Scholar] [CrossRef] [PubMed]
- Gabba, A.; Attariya, R.; Behren, S.; Pett, C.; van der Horst, J.C.; Yurugi, H.; Yu, J.; Urschbach, M.; Sabin, J.; Birrane, G.; et al. MUC1 Glycopeptide Vaccine Modified with a GalNAc Glycocluster Targets the Macrophage Galactose C-type Lectin on Dendritic Cells to Elicit an Improved Humoral Response. J. Am. Chem. Soc. 2023, 145, 13027–13037. [Google Scholar] [CrossRef]
- Gao, T.; Cen, Q.; Lei, H. A review on development of MUC1-based cancer vaccine. Biomed. Pharmacother. 2020, 132, 110888. [Google Scholar] [CrossRef]
- Lakshminarayanan, V.; Supekar, N.T.; Wei, J.; McCurry, D.B.; Dueck, A.C.; Kosiorek, H.E.; Trivedi, P.P.; Bradley, J.M.; Madsen, C.S.; Pathangey, L.B.; et al. MUC1 Vaccines, Comprised of Glycosylated or Non-Glycosylated Peptides or Tumor-Derived MUC1, Can Circumvent Immunoediting to Control Tumor Growth in MUC1 Transgenic Mice. PLoS ONE 2016, 11, e0145920. [Google Scholar] [CrossRef]
- McDonald, D.M.; Byrne, S.N.; Payne, R.J. Synthetic self-adjuvanting glycopeptide cancer vaccines. Front. Chem. 2015, 3, 60. [Google Scholar] [CrossRef] [PubMed]
- Katayama, H.; Kobayashi, M.; Irajizad, E.; Sevillano, A.M.; Patel, N.; Mao, X.; Rusling, L.; Vykoukal, J.; Cai, Y.; Hsiao, F.; et al. Protein citrullination as a source of cancer neoantigens. J. Immunother. Cancer 2021, 9, e002549. [Google Scholar] [CrossRef]
- Loh, T.J.; Lim, J.J.; Jones, C.M.; Dao, H.T.; Tran, M.T.; Baker, D.G.; La Gruta, N.L.; Reid, H.H.; Rossjohn, J. The molecular basis underlying T cell specificity towards citrullinated epitopes presented by HLA-DR4. Nat. Commun. 2024, 15, 6201. [Google Scholar] [CrossRef] [PubMed]
- Cook, K.; Daniels, I.; Symonds, P.; Pitt, T.; Gijon, M.; Xue, W.; Metheringham, R.; Durrant, L.; Brentville, V. Citrullinated α-enolase is an effective target for anti-cancer immunity. OncoImmunology 2017, 7, e1390642. [Google Scholar] [CrossRef]
- Tang, S.; Tang, R.; Chen, G.; Zhang, D.; Lin, K.; Yang, H.; Fu, J.; Guo, Y.; Lin, F.; Dong, X.; et al. Personalized neoantigen hydrogel vaccine combined with PD-1 and CTLA-4 double blockade elicits antitumor response in liver metastases by activating intratumoral CD8+CD69+T cells. J. Immunother. Cancer 2024, 12, e009543. [Google Scholar] [CrossRef]
- Hu, Q.; Shi, Y.; Wang, H.; Bing, L.; Xu, Z. Post-translational modifications of immune checkpoints: Unlocking new potentials in cancer immunotherapy. Exp. Hematol. Oncol. 2025, 14, 37. [Google Scholar] [CrossRef]
- Liu, Z.; Lv, J.; Dang, Q.; Liu, L.; Weng, S.; Wang, L.; Zhou, Z.; Kong, Y.; Li, H.; Han, Y.; et al. Engineering neoantigen vaccines to improve cancer personalized immunotherapy. Int. J. Biol. Sci. 2022, 18, 5607–5623. [Google Scholar] [CrossRef]
- Liao, J.-Y.; Zhang, S. Safety and Efficacy of Personalized Cancer Vaccines in Combination With Immune Checkpoint Inhibitors in Cancer Treatment. Front. Oncol. 2021, 11, 663264. [Google Scholar] [CrossRef]
- Nair, R.; Somasundaram, V.; Kuriakose, A.; Krishn, S.R.; Raben, D.; Salazar, R.; Nair, P. Deciphering T-cell exhaustion in the tumor microenvironment: Paving the way for innovative solid tumor therapies. Front. Immunol. 2025, 16, 1548234. [Google Scholar] [CrossRef]
- Zhu, T.; Wu, X.; Liao, Y.; Yan, Y.; Yu, M.; Wang, L.; Xia, Q. The role of innate immune cells as modulators of the tumor microenvironment in the metastasis and treatment of pancreatic cancer. Clin. Cancer Bull. 2023, 2, 2. [Google Scholar] [CrossRef]
- Jin, L.; Kim, H.; Shi, J. Neutrophil in the Pancreatic Tumor Microenvironment. Biomolecules 2021, 11, 1170. [Google Scholar] [CrossRef] [PubMed]
- Jia, Y.; Jia, R.; Taledaohan, A.; Wang, Y.; Wang, Y. Structure–Activity Relationship of PAD4 Inhibitors and Their Role in Tumor Immunotherapy. Pharmaceutics 2024, 16, 335. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Zhao, B.; Dong, H.; Li, T.; Cheng, X.; Gong, W.; Wang, J.; Zhang, J.; Xin, G.; Yu, Y.; et al. Inhibition of O-GlcNAc transferase activates type I interferon-dependent antitumor immunity by bridging cGAS-STING pathway. eLife 2024, 13, RP94849. [Google Scholar] [CrossRef]
- Al Saoud, R.; Hamrouni, A.; Idris, A.; Mousa, W.K.; Abu Izneid, T. Recent advances in the development of sialyltransferase inhibitors to control cancer metastasis: A comprehensive review. Biomed. Pharmacother. 2023, 165, 115091. [Google Scholar] [CrossRef]
- Lin, S.-Y.; Schmidt, E.N.; Takahashi-Yamashiro, K.; Macauley, M.S. Roles for Siglec-glycan interactions in regulating immune cells. Semin. Immunol. 2024, 77, 101925. [Google Scholar] [CrossRef]
- Egan, H.; Treacy, O.; Lynch, K.; Leonard, N.A.; O’malley, G.; Reidy, E.; O’neill, A.; Corry, S.M.; De Veirman, K.; Vanderkerken, K.; et al. Targeting stromal cell sialylation reverses T cell-mediated immunosuppression in the tumor microenvironment. Cell Rep. 2023, 42, 112475. [Google Scholar] [CrossRef]
- Rao, T.C.; Beggs, R.R.; Ankenbauer, K.E.; Hwang, J.; Ma, V.P.-Y.; Salaita, K.; Bellis, S.L.; Mattheyses, A.L. ST6Gal-I–mediated sialylation of the epidermal growth factor receptor modulates cell mechanics and enhances invasion. J. Biol. Chem. 2022, 298, 101726. [Google Scholar] [CrossRef] [PubMed]
- Zhu, W.; Zhou, Y.; Guo, L.; Feng, S. Biological function of sialic acid and sialylation in human health and disease. Cell Death Discov. 2024, 10, 415. [Google Scholar] [CrossRef]
- Lv, D.; Fei, Y.; Chen, H.; Wang, J.; Han, W.; Cui, B.; Feng, Y.; Zhang, P.; Chen, J. Crosstalk between T lymphocyte and extracellular matrix in tumor microenvironment. Front. Immunol. 2024, 15, 1340702. [Google Scholar] [CrossRef]
- Huang, J.; Zhang, L.; Wan, D.; Zhou, L.; Zheng, S.; Lin, S.; Qiao, Y. Extracellular matrix and its therapeutic potential for cancer treatment. Signal Transduct. Target. Ther. 2021, 6, 153. [Google Scholar] [CrossRef]
- Mai, Z.; Lin, Y.; Lin, P.; Zhao, X.; Cui, L. Modulating extracellular matrix stiffness: A strategic approach to boost cancer immunotherapy. Cell Death Dis. 2024, 15, 307. [Google Scholar] [CrossRef]
- Lundberg, K.; Nijenhuis, S.; Vossenaar, E.R.; Palmblad, K.; van Venrooij, W.J.; Klareskog, L.; Zendman, A.; Harris, H.E. Citrullinated proteins have increased immunogenicity and arthritogenicity and their presence in arthritic joints correlates with disease severity. Arthritis Res. Ther. 2005, 7, R458–67. [Google Scholar] [CrossRef]
- Postow, M.A.; Sidlow, R.; Hellmann, M.D. Immune-Related Adverse Events Associated with Immune Checkpoint Blockade. N. Engl. J. Med. 2018, 378, 158–168. [Google Scholar] [CrossRef] [PubMed]
- Lewis, H.D.; Liddle, J.; Coote, J.E.; Atkinson, S.J.; Barker, M.D.; Bax, B.D.; Bicker, K.L.; Bingham, R.P.; Campbell, M.; Chen, Y.H.; et al. Inhibition of PAD4 activity is sufficient to disrupt mouse and human NET formation. Nat. Chem. Biol. 2015, 11, 189–191. [Google Scholar] [CrossRef]
- Ferrara, B.; Pignatelli, C.; Cossutta, M.; Citro, A.; Courty, J.; Piemonti, L. The Extracellular Matrix in Pancreatic Cancer: Description of a Complex Network and Promising Therapeutic Options. Cancers 2021, 13, 4442. [Google Scholar] [CrossRef] [PubMed]
- Yuan, Z.; Li, Y.; Zhang, S.; Wang, X.; Dou, H.; Yu, X.; Zhang, Z.; Yang, S.; Xiao, M. Extracellular matrix remodeling in tumor progression and immune escape: From mechanisms to treatments. Mol. Cancer 2023, 22, 48. [Google Scholar] [CrossRef] [PubMed]
- Nicolas-Boluda, A.; Vaquero, J.; Vimeux, L.; Guilbert, T.; Barrin, S.; Kantari-Mimoun, C.; Ponzo, M.; Renault, G.; Deptula, P.; Pogoda, K.; et al. Tumor stiffening reversion through collagen crosslinking inhibition improves T cell migration and anti-PD-1 treatment. eLife 2021, 10, e58688. [Google Scholar] [CrossRef]
- Jiang, C.; Wang, M.; Yao, W.; Lv, G.; Liu, X.; Wang, G. Comprehensive Analysis on Prognosis and Immune Infiltration of Lysyl Oxidase Family Members in Pancreatic Adenocarcinoma With Experimental Verification. Front. Mol. Biosci. 2022, 9, 778857. [Google Scholar] [CrossRef]
- Miller, B.W.; Morton, J.P.; Pinese, M.; Saturno, G.; Jamieson, N.B.; McGhee, E.; Timpson, P.; Leach, J.; McGarry, L.; Shanks, E.; et al. Targeting the LOX / hypoxia axis reverses many of the features that make pancreatic cancer deadly: Inhibition of LOX abrogates metastasis and enhances drug efficacy. EMBO Mol. Med. 2015, 7, 1063–1076. [Google Scholar] [CrossRef]
- Mommen, G.P.M.; Frese, C.K.; Meiring, H.D.; Brink, J.v.G.-V.D.; de Jong, A.P.J.M.; van Els, C.A.C.M.; Heck, A.J.R. Expanding the detectable HLA peptide repertoire using electron-transfer/higher-energy collision dissociation (EThcD). Proc. Natl. Acad. Sci. USA 2014, 111, 4507–4512. [Google Scholar] [CrossRef]
- Riley, N.M.; Westphall, M.S.; Coon, J.J. Activated Ion-Electron Transfer Dissociation Enables Comprehensive Top-Down Protein Fragmentation. J. Proteome Res. 2017, 16, 2653–2659. [Google Scholar] [CrossRef]
- Palacios, P.A.; Flores, I.; Cereceda, L.; Otero, F.F.; Müller, M.; Brebi, P.; Contreras, H.R.; Carreño, L.J. Patient-Derived Organoid Models for NKT Cell-Based Cancer Immunotherapy. Cancers 2025, 17, 406. [Google Scholar] [CrossRef] [PubMed]
- Magré, L.; Verstegen, M.M.A.; Buschow, S.; van der Laan, L.J.W.; Peppelenbosch, M.; Desai, J. Emerging organoid-immune co-culture models for cancer research: From oncoimmunology to personalized immunotherapies. J. Immunother. Cancer 2023, 11, e006290. [Google Scholar] [CrossRef] [PubMed]
- Esposito, A.; Agostini, A.; Quero, G.; Piro, G.; Priori, L.; Caggiano, A.; Scaglione, G.; Battaglia, A.; Calegari, M.A.; Salvatore, L.; et al. Colorectal cancer patients-derived immunity-organoid platform unveils cancer-specific tissue markers associated with immunotherapy resistance. Cell Death Dis. 2024, 15, 878. [Google Scholar] [CrossRef]
- Tsai, S.; McOlash, L.; Palen, K.; Johnson, B.; Duris, C.; Yang, Q.; Dwinell, M.B.; Hunt, B.; Evans, D.B.; Gershan, J.; et al. Development of primary human pancreatic cancer organoids, matched stromal and immune cells and 3D tumor microenvironment models. BMC Cancer 2018, 18, 335. [Google Scholar] [CrossRef]
- Caron, E.; Aebersold, R.; Banaei-Esfahani, A.; Chong, C.; Bassani-Sternberg, M. A Case for a Human Immuno-Peptidome Project Consortium. Immunity 2017, 47, 203–208. [Google Scholar] [CrossRef] [PubMed]
- Vizcaíno, J.A.; Kubiniok, P.; Kovalchik, K.A.; Ma, Q.; Duquette, J.D.; Mongrain, I.; Deutsch, E.W.; Peters, B.; Sette, A.; Sirois, I.; et al. The Human Immunopeptidome Project: A Roadmap to Predict and Treat Immune Diseases. Mol. Cell. Proteom. 2020, 19, 31–49. [Google Scholar] [CrossRef]
- Kraemer, A.I.; Chong, C.; Huber, F.; Pak, H.; Stevenson, B.J.; Müller, M.; Michaux, J.; Altimiras, E.R.; Rusakiewicz, S.; Simó-Riudalbas, L.; et al. The immunopeptidome landscape associated with T cell infiltration, inflammation and immune editing in lung cancer. Nat. Cancer 2023, 4, 608–628. [Google Scholar] [CrossRef]
- Xu, H.; Hu, R.; Dong, X.; Kuang, L.; Zhang, W.; Tu, C.; Li, Z.; Zhao, Z. ImmuneApp for HLA-I epitope prediction and immunopeptidome analysis. Nat. Commun. 2024, 15, 8926. [Google Scholar] [CrossRef]
- Schneeweis, C.; Hassan, Z.; Schick, M.; Keller, U.; Schneider, G. The SUMO pathway in pancreatic cancer: Insights and inhibition. Br. J. Cancer 2020, 124, 531–538. [Google Scholar] [CrossRef]
- Kumar, S.; Schoonderwoerd, M.J.A.; Kroonen, J.S.; de Graaf, I.J.; Sluijter, M.; Ruano, D.; González-Prieto, R.; Vries, M.V.-D.; Rip, J.; Arens, R.; et al. Targeting pancreatic cancer by TAK-981: A SUMOylation inhibitor that activates the immune system and blocks cancer cell cycle progression in a preclinical model. Gut 2022, 71, 2266–2283. [Google Scholar] [CrossRef]
- Luo, Y.; Li, Z.; Kong, Y.; He, W.; Zheng, H.; An, M.; Lin, Y.; Zhang, D.; Yang, J.; Zhao, Y.; et al. KRAS mutant–driven SUMOylation controls extracellular vesicle transmission to trigger lymphangiogenesis in pancreatic cancer. J. Clin. Investig. 2022, 132, e157644. [Google Scholar] [CrossRef]
- de la Torre Medina, J.; Joshi, U.; Sonowal, H.; Kuang, Y.; Ren, T.; Chen, D.H.; Tharuka, M.D.N.; Nguyen-Ta, K.; Gros, H.; Mikulski, Z.; et al. Immunomodulation of Pancreatic Cancer via Inhibition of SUMOylation and CD155/TIGIT Pathway. bioRxiv 2025. [Google Scholar] [CrossRef]
- Zheng, Y.; Sun, W.; Shan, C.; Li, B.; Liu, J.; Xing, H.; Xu, Q.; Cui, B.; Zhu, W.; Chen, J.; et al. β-hydroxybutyrate inhibits ferroptosis-mediated pancreatic damage in acute liver failure through the increase of H3K9bhb. Cell Rep. 2022, 41, 111847. [Google Scholar] [CrossRef]
- Liang, X.; Tian, R.; Li, T.; Wang, H.; Qin, Y.; Qian, M.; Fan, J.; Wang, D.; Cui, H.-Y.; Jiang, J. Integrative insights into the role of CAV1 in ketogenic diet and ferroptosis in pancreatic cancer. Cell Death Discov. 2025, 11, 139. [Google Scholar] [CrossRef] [PubMed]
- Ku, B.; Eisenbarth, D.; Baek, S.; Jeong, T.-K.; Kang, J.-G.; Hwang, D.; Noh, M.-G.; Choi, C.; Choi, S.; Seol, T.; et al. PRMT1 promotes pancreatic cancer development and resistance to chemotherapy. Cell Rep. Med. 2024, 5, 101461. [Google Scholar] [CrossRef] [PubMed]
- Baretti, M.; Ahuja, N.; Azad, N.S. Targeting the epigenome of pancreatic cancer for therapy: Challenges and opportunities. Ann. Pancreat. Cancer 2019, 2, 18. [Google Scholar] [CrossRef]
- Chen, G.; Guo, G.; Zhou, X.; Chen, H. Potential mechanism of ferroptosis in pancreatic cancer (Review). Oncol. Lett. 2019, 19, 579–587. [Google Scholar] [CrossRef]
- Shen, X.; Chen, Y.; Tang, Y.; Lu, P.; Liu, M.; Mao, T.; Weng, Y.; Yu, F.; Liu, Y.; Tang, Y.; et al. Targeting pancreatic cancer glutamine dependency confers vulnerability to GPX4-dependent ferroptosis. Cell Rep. Med. 2025, 6, 101928. [Google Scholar] [CrossRef]
| Therapy/Agent | Target Mutation(s) | Trial Phase/ID | ORR/Clinical Outcome | Resistance Mechanism (TME) | Resistance Mechanism (Immune) | Key Insights | Ref |
|---|---|---|---|---|---|---|---|
| GI-4000 (yeast vaccine) | Mutant KRAS | Phase II (NCT00300950) | No survival benefit; immune responses in subset | Desmoplastic stroma; immune exclusion | Weak effector T cell priming despite immune activation | Residual tumor drives immune response. Immune activation correlates with survival. Proteomic biomarkers predict response. | [26] |
| mRNA-5671 (V941) | KRAS G12D/V/R/C | Phase I (NCT03948763) | Trial terminated (futility) | CAF/MDSC-mediated immune suppression | Lack of durable T cell responses to KRAS epitopes | Personalized vaccine approach. Combination therapy potential. Safety and tolerability. | [27] |
| ELI-002 (liposomal vaccine) | KRAS G12D/R | Phase I (NCT04853017) | ~21% KRAS-specific T cell response | Antigen presentation barriers; TME-driven T cell exhaustion | Limited cytotoxicity of expanded CD8+ T cells | Personalized approach Combination potential Preliminary immune response | [28] |
| TP53 synthetic long-peptide vaccine | Mutant TP53 | Phase I/II | 0% ORR in PDAC cohort | Stromal desmoplasia; TGF-β signaling | Immune ignorance; Treg/MDSC induction | TP53 mutation as a prognostic marker. Immune landscape correlation. Therapeutic implications. | [29] |
| Durvalumab ± Tremelimumab (ICIs) | PD-1 / CTLA-4 | Phase II (NCT02558894) | 3.1% (Durva), 0% (combo) | Low neoantigen load; CD73/CD39 adenosine pathway | T cell exclusion; exhausted phenotype | Limited efficacy of dual immune checkpoint inhibition. Absence of response to monotherapy. safety profile. | [17] |
| Pembrolizumab (ICI) | PD-1 | Phase II (KEYNOTE-158, NCT02628067) | ~1% ORR in PDAC, benefit restricted to MSI-H subset | Poor T cell infiltration; immunosuppressive stroma | Lack of neoantigens in MSS tumors; PD-1+ exhausted T cells | Efficacy of pembrolizumab in MSI-H/dMMR cancers. Durable responses and survival outcomes. Safety profile consistent with previous experience. | [30] |
| Personalized mRNA vaccines | Patient-specific neoAg | Phase I (NCT04161755, etc.) | Limited efficacy in PDAC | Low mutational load limits high-affinity targets | Immunodominance of weak responses; MDSC suppression | High response rate. Long-term T cell persistence. Correlation with delayed recurrence. Safety profile. | [31] |
| Sotorasib (KRAS G12C inhibitor) | KRAS G12C (rare in PDAC) | Phase I/II (CodeBreaK100) | ~21% ORR, short-lived | Very low G12C prevalence (~1–2%); adaptive resistance | Epitope loss; bypass pathway activation | Efficacy of Sotorasib in KRAS p.G12C-mutated pancreatic cancer. Objective response rate. Safety profile. | [32] |
| TCR-T (engineered TCR, KRAS G12D) | KRAS G12D (HLA-C*08:02) | Case report (NCT03745326) | Partial response (~72% shrinkage) | Tumor heterogeneity; stromal barrier | Restricted HLA subtype; limited persistence of engineered TCR clones | Targeted TCR gene therapy. Objective tumor regression. Immune response monitoring. | [33] |
| PTM Type | Key Enzymes | Example Substrates/Sites | Immune Mechanism in PDAC (Concise) | Biomarker Potential | Therapeutic Strategies | Ref. |
|---|---|---|---|---|---|---|
| Aberrant O-glycosylation and hypersialylation (Tn/STn; α2-6 sialylation) | GALNTs, ST6GAL1, ST3GALs | MUC1/MUC16; PD-L1; EGFR | Siglec-7/9 engagement → myeloid immunosuppression; epitope masking | ST6GAL1 overexpression; hypersialylation signatures; MUC1-STn | Sialyltransferase inhibitors; anti-Siglec; desialylating biologics; glycopeptide vaccines | [56,57] |
| O-GlcNAcylation (HBP–OGT axis) | OGT, GFAT1/2 | PD-L1; SIRT7; YBX1 | PD-L1 stabilization; M2-skewing via GFPT2→O-GlcNAc→YBX1/IL-18 | Global O-GlcNAc; OGT/GFPT2 expression | OGT/HBP inhibitors; ± PD-1/PD-L1 blockade | [58,59] |
| Citrullination → NETs | PAD4, PAD2 | Histone H3Cit; extracellular vimentin | NET-mediated T cell exclusion; pro-metastatic trapping | H3Cit (tissue/serum); PAD4 expression/activity | PAD4 inhibitors; DNase; NET-targeting ± ICB | [60] |
| Phosphorylation (MAPK/ERK; JAK/STAT) | EGFR→MEK/ERK; JAK/STAT3 | p-ERK; p-STAT3 | EGFR/MAPK↑ PD-L1 on tumor cells; ERK-i + anti-PD-L1 synergy | p-ERK/MEK; STAT3 activity | MEK/ERK or STAT3 inhibitors + ICB | [61,62] |
| SUMOylation | SAE1/UBA2 (E1), UBC9 (E2), PIAS E3s | Broad (MYC-linked programs) | SUMO-addicted MYC-high subtype; SUMOi activates antitumor immunity | SUMO-pathway signature; UBC9/SAE1 IHC | TAK-981 (sumoylation E1 inhibitor) ± ICB | [63] |
| Ubiquitination/Deubiquitination (PD-L1 stability) | TRIM E3s; USP8, CSN5 (DUBs) | PD-L1, β-catenin | DUB-stabilized PD-L1; DUB-i + anti-PD-L1 boosts CD8+ T cells | DUB (USP8/CSN5) expression; PD-L1 levels | DUB inhibitors (USP8); PD-L1 degraders/PROTACs; E3 activation | [64,65] |
| Acetylation (HDAC/p300-CBP) | HDACs; p300/CBP | Histones; NF-κB/STATs | APM/MHC-I repression; HDACi restores CTL sensitivity | HDAC expression; histone acetylation patterns | HDAC inhibitors ± ICB; epigenetic immunotherapy | [66] |
| S-Nitrosylation (iNOS/NO) | iNOS (NOS2) | STAT3, RAF1, multiple targets | Proteome-wide S-nitrosylation; myeloid NO suppresses T cells | iNOS expression; S-nitrosylome panels | iNOS inhibition; myeloid-targeting ± ICB | [67,68] |
| Workflow | PTM Retention | Best for | Strengths | Limitations | Ref |
|---|---|---|---|---|---|
| CID/HCD | Low for labile PTMs (neutral loss common) | Fast general proteomics; glyco survey (oxonium ions) | High speed and IDs; robust DIA/DDA backbone | Neutral loss hampers site localization (e.g., phospho); O-GlcNAc/O-glyco often degrade | [175,176] |
| ETD | High (preserves labile PTMs) | Phospho, O-GlcNAc, fragile HLA peptides | Retains labile groups; improves site calls; complements HCD | Lower efficiency for short/low-charge peptides; slower | [177] |
| EThcD (ETD + gentle HCD) | High with better sequence coverage | O-glycopeptides; broader PTM mapping | Outperforms ETD/HCD for O-glyco; richer spectra (b/y + c/z) | Slightly slower; needs ETD-capable Orbitrap/Tribrid | [178] |
| AI-ETD (activated-ion ETD) | High with higher fragmentation yield | Phospho, intact glyco (incl. O-glyco); top/middle-down | More IDs and coverage than ETD; better for low-charge density precursors | Requires IR-enabled ETD cell; throughput < HCD | [179] |
| EThcD for HLA immunopeptidomes | Preserves fragile motifs; ↑ sequence coverage vs. HCD | HLA-I (9–12mers; internal Arg, low-charge density) | Deeper HLA coverage with minimal duty-cycle penalty (newer hardware) | Needs ETD/EThcD-capable instruments | [180] |
| Stage | Modality | Representative Example | Indication(s) Tested | Current Status | Ref |
|---|---|---|---|---|---|
| Tested in humans | Glycopeptide/peptide vaccine (MUC1) | MUC1 100-mer peptide + adjuvant (or DC-pulsed MUC1) | Pancreatic cancer (resected/advanced) | Phase I trials show safety and immunogenicity; no definitive efficacy | [201] |
| Phosphopeptide vaccine | HLA-I phosphopeptides (e.g., pBCAR3, pIRS2) | Melanoma/solid tumors (first-in-human) | Phase I: safe, immunogenic; supports further development | [202] | |
| Myeloid checkpoint blockade (anti-Siglec-15) | NC318 (± pembrolizumab) | Solid tumors (multitumor baskets) | Ongoing Phase I/II; mixed early activity | [203] | |
| SUMO-pathway inhibitor | Subasumstat/TAK-981 | Solid and hematologic malignancies | Phase I/II: acceptable safety; early signals (combo settings) | [204] | |
| Citrullinated peptide vaccine | Modi-1 (cit-vimentin/enolase) | Solid tumors | Solid tumorsPhase I/II ongoing | [205] | |
| Promising preclinical | Citrullinated peptide vaccines | Modi-1 (cit-vimentin/enolase) | Solid tumors (basket) | Phase I/II ongoing; preclinical efficacy + early clinical immunogenicity reported | [206] |
| Global sialylation blockade | 3Fax-Neu5Ac derivatives/prodrugs | Solid tumors (preclinical) | In vivo reduction in Siglec signaling; safety optimization ongoing | [207] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Safa, A.; Vruzhaj, I.; Gambirasi, M.; Toffoli, G. Antigenic Dark Matter: Unexplored Post-Translational Modifications of Tumor-Associated and Tumor-Specific Antigens in Pancreatic Cancer. Cancers 2025, 17, 3506. https://doi.org/10.3390/cancers17213506
Safa A, Vruzhaj I, Gambirasi M, Toffoli G. Antigenic Dark Matter: Unexplored Post-Translational Modifications of Tumor-Associated and Tumor-Specific Antigens in Pancreatic Cancer. Cancers. 2025; 17(21):3506. https://doi.org/10.3390/cancers17213506
Chicago/Turabian StyleSafa, Amin, Idris Vruzhaj, Marta Gambirasi, and Giuseppe Toffoli. 2025. "Antigenic Dark Matter: Unexplored Post-Translational Modifications of Tumor-Associated and Tumor-Specific Antigens in Pancreatic Cancer" Cancers 17, no. 21: 3506. https://doi.org/10.3390/cancers17213506
APA StyleSafa, A., Vruzhaj, I., Gambirasi, M., & Toffoli, G. (2025). Antigenic Dark Matter: Unexplored Post-Translational Modifications of Tumor-Associated and Tumor-Specific Antigens in Pancreatic Cancer. Cancers, 17(21), 3506. https://doi.org/10.3390/cancers17213506






