Tissue Factor Expression in Penile Squamous Cell Carcinoma: A Potential Marker of HPV-Independent Disease
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Tissues
2.2. Pathological Analysis
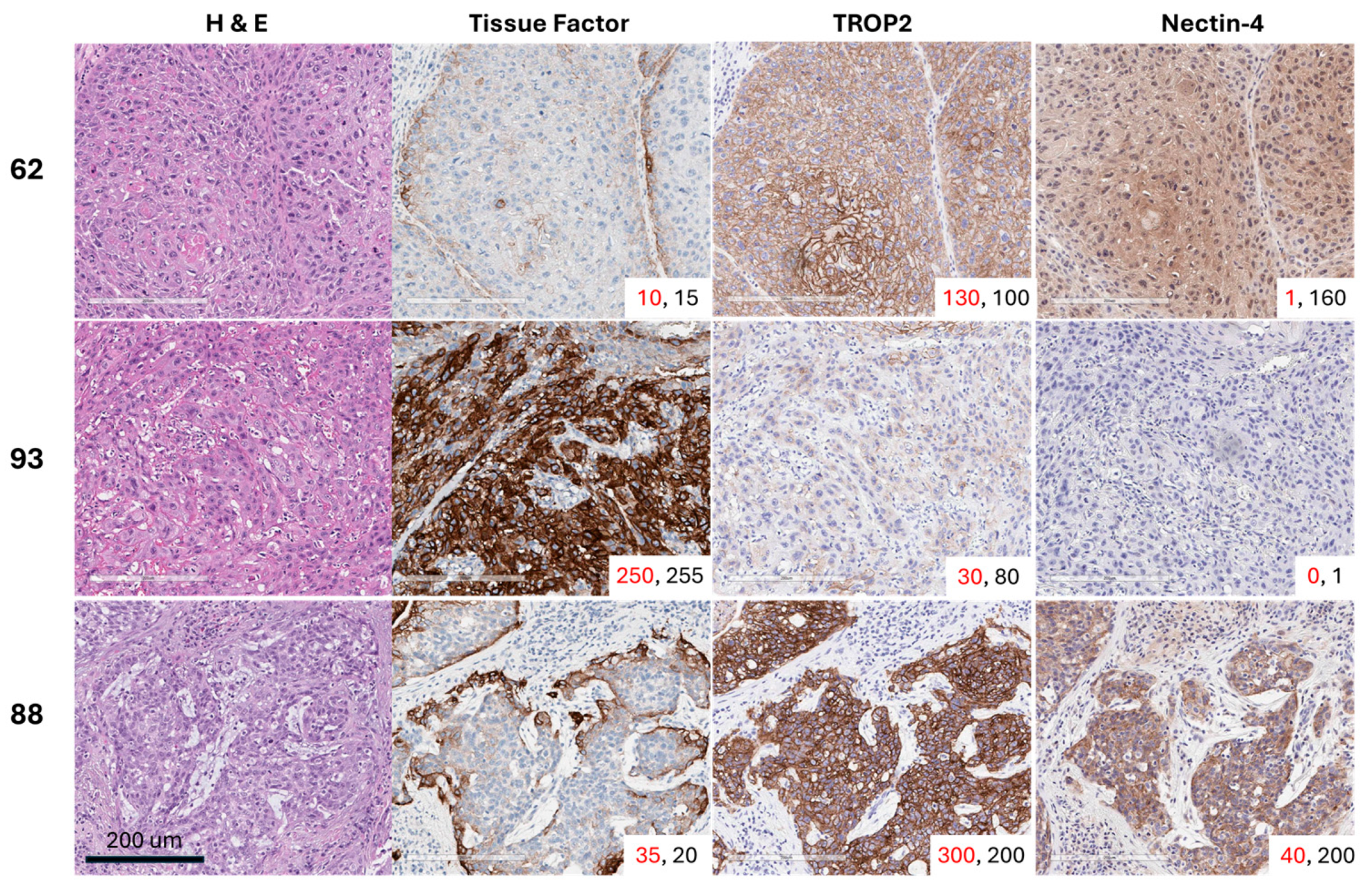
2.3. Immunohistochemistry (IHC) Staining
2.4. Immunohistochemistry (IHC) Scoring Methodology and Analysis
2.5. Study Endpoints and Follow-Up
2.6. Statistical Analysis
3. Results
3.1. Patient Baseline Characteristics
3.2. Study Endpoint Results
3.3. Associations with TF Expression
3.4. Associations with TROP2/Nectin-4 Expression
3.5. Correlations Between Surface Proteins and Other Factors
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ADC | Antibody-drug conjugate |
| AJCC | American Joint Committee on Cancer |
| CSS | Cancer-specific survival |
| FFPE | Formalin-fixed paraffin-embedded |
| H&E | Hematoxylin and eosin |
| HPV | Human papillomavirus |
| JAK | Janus kinase |
| LVI | Lymphovascular invasion |
| MDACC | MD Anderson Cancer Center |
| MMAE | Monomethyl auristatin E |
| PNI | Perineural invasion |
| PSCC | Penile squamous cell carcinoma |
| RFS | Recurrence-free survival |
| STAT | Signal transducer and activator of transcription |
| TF | Tissue factor |
| TIP | Paclitaxel, ifosfamide, and cisplatin |
| TMA | Tissue microarray |
| TRAE | Treatment-related adverse event |
| TROP2 | Trophoblast cell-surface antigen 2 |
| TV | Tisotumab vedotin |
References
- Pow-Sang, M.R.; Ferreira, U.; Pow-Sang, J.M.; Nardi, A.C.; Destefano, V. Epidemiology and natural history of penile cancer. Urology 2010, 76 (Suppl. 1), S2–S6. [Google Scholar] [CrossRef]
- Misra, S.; Chaturvedi, A.; Misra, N.C. Penile carcinoma: A challenge for the developing world. Lancet Oncol. 2004, 5, 240–247. [Google Scholar] [CrossRef] [PubMed]
- Vreeburg, M.T.A.; Donswijk, M.L.; Albersen, M.; Parnham, A.; Ayres, B.; Protzel, C.; Pettaway, C.; Spiess, P.E.; Brouwer, O.R. New EAU/ASCO guideline recommendations on sentinel node biopsy for penile cancer and remaining challenges from a nuclear medicine perspective. Eur. J. Nucl. Med. Mol. Imaging 2024, 51, 2861–2868. [Google Scholar] [CrossRef]
- Ottenhof, S.R.; de Vries, H.M.; Doodeman, B.; Vrijenhoek, G.L.; van der Noort, V.; Donswijk, M.L.; de Feijter, J.M.; Schaake, E.E.; Horenblas, S.; Brouwer, O.R.; et al. A Prospective Study of Chemoradiotherapy as Primary Treatment in Patients With Locoregionally Advanced Penile Carcinoma. Int. J. Radiat. Oncol. Biol. Phys. 2023, 117, 139–147. [Google Scholar] [CrossRef] [PubMed]
- Brouwer, O.R.; Albersen, M.; Parnham, A.; Protzel, C.; Pettaway, C.A.; Ayres, B.; Antunes-Lopes, T.; Barreto, L.; Campi, R.; Crook, J.; et al. European Association of Urology-American Society of Clinical Oncology Collaborative Guideline on Penile Cancer: 2023 Update. Eur. Urol. 2023, 83, 548–560. [Google Scholar] [CrossRef]
- Rose, K.M.; Pham, R.; Zacharias, N.M.; Ionescu, F.; Paravathaneni, M.; Marchetti, K.A.; Sanchez, D.; Mustasam, A.; Sandstrom, R.; Vikram, R.; et al. Neoadjuvant platinum-based chemotherapy and lymphadenectomy for penile cancer: An international, multi-institutional, real-world study. J. Natl. Cancer Inst. 2024, 116, 966–973. [Google Scholar] [CrossRef]
- Elst, L.; Vandermaesen, K.; Albersen, M. Emerging Advances in the Molecular Landscape of Penile Cancer and Their Implications for Precision Medicine. Curr. Treat. Options Oncol. 2025, 26, 367–374. [Google Scholar] [CrossRef] [PubMed]
- Rouvinov, K.; Mazor, G.; Kozlener, E.; Meirovitz, A.; Shrem, N.S.; Abu Saleh, O.; Shalata, S.; Yakobson, A.; Shalata, W. Cemiplimab as First Line Therapy in Advanced Penile Squamous Cell Carcinoma: A Real-World Experience. J. Pers. Med. 2023, 13, 1623. [Google Scholar] [CrossRef]
- Wang, J.; Pettaway, C.A.; Pagliaro, L.C. Treatment for Metastatic Penile Cancer After First-line Chemotherapy Failure: Analysis of Response and Survival Outcomes. Urology 2015, 85, 1104–1110. [Google Scholar] [CrossRef]
- Tekin, B.; Cheville, J.C.; Herrera Hernandez, L.; Negron, V.; Smith, C.Y.; Jenkins, S.M.; Dasari, S.; Enninga, E.A.L.; Norgan, A.P.; Menon, S.; et al. Assessment of PD-L1, TROP2, and nectin-4 expression in penile squamous cell carcinoma. Hum. Pathol. 2023, 142, 42–50. [Google Scholar] [CrossRef]
- Grass, G.D.; Chahoud, J.; Lopez, A.; Dhillon, J.; Eschrich, S.A.; Johnstone, P.A.S.; Spiess, P.E. An Analysis of Nectin-4 (PVRL4) in Penile Squamous Cell Carcinoma. Eur. Urol. Open Sci. 2023, 49, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Versteeg, H.H. Tissue Factor: Old and New Links with Cancer Biology. Semin. Thromb. Hemost. 2015, 41, 747–755. [Google Scholar] [CrossRef]
- Rondon, A.M.R.; Kroone, C.; Kapteijn, M.Y.; Versteeg, H.H.; Buijs, J.T. Role of Tissue Factor in Tumor Progression and Cancer-Associated Thrombosis. Semin. Thromb. Hemost. 2019, 45, 396–412. [Google Scholar] [CrossRef]
- Coleman, R.L.; Lorusso, D.; Gennigens, C.; Gonzalez-Martin, A.; Randall, L.; Cibula, D.; Lund, B.; Woelber, L.; Pignata, S.; Forget, F.; et al. Efficacy and safety of tisotumab vedotin in previously treated recurrent or metastatic cervical cancer (innovaTV 204/GOG-3023/ENGOT-cx6): A multicentre, open-label, single-arm, phase 2 study. Lancet Oncol. 2021, 22, 609–619. [Google Scholar] [CrossRef] [PubMed]
- Vergote, I.; Gonzalez-Martin, A.; Fujiwara, K.; Kalbacher, E.; Bagameri, A.; Ghamande, S.; Lee, J.Y.; Banerjee, S.; Maluf, F.C.; Lorusso, D.; et al. Tisotumab Vedotin as Second- or Third-Line Therapy for Recurrent Cervical Cancer. N. Engl. J. Med. 2024, 391, 44–55. [Google Scholar] [CrossRef]
- Chahoud, J.; Zacharias, N.M.; Pham, R.; Qiao, W.; Guo, M.; Lu, X.; Alaniz, A.; Segarra, L.; Martinez-Ferrer, M.; Gleber-Netto, F.O.; et al. Prognostic Significance of p16 and Its Relationship with Human Papillomavirus Status in Patients with Penile Squamous Cell Carcinoma: Results of 5 Years Follow-Up. Cancers 2022, 14, 6024. [Google Scholar] [CrossRef]
- Jawhar, N.M. Tissue Microarray: A rapidly evolving diagnostic and research tool. Ann. Saudi Med. 2009, 29, 123–127. [Google Scholar] [CrossRef]
- de Bono, J.S.; Harris, J.R.; Burm, S.M.; Vanderstichele, A.; Houtkamp, M.A.; Aarass, S.; Riisnaes, R.; Figueiredo, I.; Nava Rodrigues, D.; Christova, R.; et al. Systematic study of tissue factor expression in solid tumors. Cancer Rep. 2023, 6, e1699. [Google Scholar] [CrossRef]
- Jeon, Y.; Jo, U.; Hong, J.; Gong, G.; Lee, H.J. Trophoblast cell-surface antigen 2 (TROP2) expression in triple-negative breast cancer. BMC Cancer 2022, 22, 1014. [Google Scholar] [CrossRef]
- Klumper, N.; Tran, N.K.; Zschabitz, S.; Hahn, O.; Buttner, T.; Roghmann, F.; Bolenz, C.; Zengerling, F.; Schwab, C.; Nagy, D.; et al. NECTIN4 Amplification Is Frequent in Solid Tumors and Predicts Enfortumab Vedotin Response in Metastatic Urothelial Cancer. J. Clin. Oncol. 2024, 42, 2446–2455. [Google Scholar] [CrossRef] [PubMed]
- Hoffman-Censits, J.H.; Lombardo, K.A.; Parimi, V.; Kamanda, S.; Choi, W.; Hahn, N.M.; McConkey, D.J.; McGuire, B.M.; Bivalacqua, T.J.; Kates, M.; et al. Expression of Nectin-4 in Bladder Urothelial Carcinoma, in Morphologic Variants, and Nonurothelial Histotypes. Appl. Immunohistochem. Mol. Morphol. 2021, 29, 619–625. [Google Scholar] [CrossRef]
- Tessier-Cloutier, B.; Kortekaas, K.E.; Thompson, E.; Pors, J.; Chen, J.; Ho, J.; Prentice, L.M.; McConechy, M.K.; Chow, C.; Proctor, L.; et al. Major p53 immunohistochemical patterns in in situ and invasive squamous cell carcinomas of the vulva and correlation with TP53 mutation status. Mod. Pathol. 2020, 33, 1595–1605. [Google Scholar] [CrossRef]
- Kobel, M.; Kang, E.Y. The Many Uses of p53 Immunohistochemistry in Gynecological Pathology: Proceedings of the ISGyP Companion Society Session at the 2020 USCAP Annual9 Meeting. Int. J. Gynecol. Pathol. 2021, 40, 32–40. [Google Scholar] [CrossRef]
- Trias, I.; Saco, A.; Marimon, L.; Lopez Del Campo, R.; Manzotti, C.; Ordi, O.; Del Pino, M.; Perez, F.M.; Vega, N.; Alos, S.; et al. P53 in Penile Squamous Cell Carcinoma: A Pattern-Based Immunohistochemical Framework with Molecular Correlation. Cancers 2023, 15, 2719. [Google Scholar] [CrossRef]
- Kashofer, K.; Winter, E.; Halbwedl, I.; Thueringer, A.; Kreiner, M.; Sauer, S.; Regauer, S. HPV-negative penile squamous cell carcinoma: Disruptive mutations in the TP53 gene are common. Mod. Pathol. 2017, 30, 1013–1020. [Google Scholar] [CrossRef] [PubMed]
- Chahoud, J.; Gleber-Netto, F.O.; McCormick, B.Z.; Rao, P.; Lu, X.; Guo, M.; Morgan, M.B.; Chu, R.A.; Martinez-Ferrer, M.; Eterovic, A.K.; et al. Whole-exome Sequencing in Penile Squamous Cell Carcinoma Uncovers Novel Prognostic Categorization and Drug Targets Similar to Head and Neck Squamous Cell Carcinoma. Clin. Cancer Res. 2021, 27, 2560–2570. [Google Scholar] [CrossRef] [PubMed]
- Elst, L.; Van Rompuy, A.S.; Roussel, E.; Spans, L.; Vanden Bempt, I.; Necchi, A.; Ross, J.; Jacob, J.M.; Baietti, M.F.; Leucci, E.; et al. Establishment and Characterization of Advanced Penile Cancer Patient-derived Tumor Xenografts: Paving the Way for Personalized Treatments. Eur. Urol. Focus. 2022, 8, 1787–1794. [Google Scholar] [CrossRef]
- Hisada, Y.; Mackman, N. Tissue Factor and Cancer: Regulation, Tumor Growth, and Metastasis. Semin. Thromb. Hemost. 2019, 45, 385–395. [Google Scholar] [CrossRef]
- Yu, J.L.; May, L.; Lhotak, V.; Shahrzad, S.; Shirasawa, S.; Weitz, J.I.; Coomber, B.L.; Mackman, N.; Rak, J.W. Oncogenic events regulate tissue factor expression in colorectal cancer cells: Implications for tumor progression and angiogenesis. Blood 2005, 105, 1734–1741. [Google Scholar] [CrossRef] [PubMed]
- Rao, B.; Gao, Y.; Huang, J.; Gao, X.; Fu, X.; Huang, M.; Yao, J.; Wang, J.; Li, W.; Zhang, J.; et al. Mutations of p53 and K-ras correlate TF expression in human colorectal carcinomas: TF downregulation as a marker of poor prognosis. Int. J. Color. Dis. 2011, 26, 593–601. [Google Scholar] [CrossRef]
- Regina, S.; Valentin, J.B.; Lachot, S.; Lemarie, E.; Rollin, J.; Gruel, Y. Increased tissue factor expression is associated with reduced survival in non-small cell lung cancer and with mutations of TP53 and PTEN. Clin. Chem. 2009, 55, 1834–1842. [Google Scholar] [CrossRef]
- Regina, S.; Rollin, J.; Blechet, C.; Iochmann, S.; Reverdiau, P.; Gruel, Y. Tissue factor expression in non-small cell lung cancer: Relationship with vascular endothelial growth factor expression, microvascular density, and K-ras mutation. J. Thorac. Oncol. 2008, 3, 689–697. [Google Scholar] [CrossRef]
- Zhao, X.T.; Cheng, C.; Gou, J.H.; Yi, T.; Qian, Y.P.; Du, X.; Zhao, X. Expression of tissue factor in human cervical carcinoma tissue. Exp. Ther. Med. 2018, 16, 4075–4081. [Google Scholar] [CrossRef]
- Randall, L.M.; Walker, A.J.; Jia, A.Y.; Miller, D.T.; Zamarin, D. Expanding Our Impact in Cervical Cancer Treatment: Novel Immunotherapies, Radiation Innovations, and Consideration of Rare Histologies. Am. Soc. Clin. Oncol. Educ. Book. 2021, 41, 252–263. [Google Scholar] [CrossRef] [PubMed]
- Dernbach, G.; Eich, M.L.; Dragomir, M.P.; Anders, P.; Jurczok, N.; Stief, C.; Jurmeister, P.; Schlomm, T.; Klauschen, F.; Horst, D.; et al. Spatial Expression of HER2, NECTIN4, and TROP-2 in Muscle-Invasive Bladder Cancer and Metastases: Implications for Pathological and Clinical Management. Mod. Pathol. 2025, 38, 100753. [Google Scholar] [CrossRef]
- Kasthuri, R.S.; Taubman, M.B.; Mackman, N. Role of Tissue Factor in Cancer. J. Clin. Oncol. 2009, 27, 4834–4838. [Google Scholar] [CrossRef] [PubMed]
- Sawada, M.; Miyake, S.; Ohdama, S.; Matsubara, O.; Masuda, S.; Yakumaru, K.; Yoshizawa, Y. Expression of tissue factor in non-small-cell lung cancers and its relationship to metastasis. Br. J. Cancer 1999, 79, 472–477. [Google Scholar] [CrossRef]
- Ueno, T.; Toi, M.; Koike, M.; Nakamura, S.; Tominaga, T. Tissue factor expression in breast cancer tissues: Its correlation with prognosis and plasma concentration. Br. J. Cancer 2000, 83, 164–170. [Google Scholar] [CrossRef]
- Shigemori, C.; Wada, H.; Matsumoto, K.; Shiku, H.; Nakamura, S.; Suzuki, H. Tissue factor expression and metastatic potential of colorectal cancer. Thromb. Haemost. 1998, 80, 894–898. [Google Scholar] [CrossRef]
- Seto, S.; Onodera, H.; Kaido, T.; Yoshikawa, A.; Ishigami, S.; Arii, S.; Imamura, M. Tissue factor expression in human colorectal carcinoma—Correlation with hepatic metastasis and impact on prognosis. Cancer 2000, 88, 295–301. [Google Scholar] [CrossRef]
- Elst, L.; Philips, G.; Vandermaesen, K.; Bassez, A.; Lodi, F.; Vreeburg, M.T.A.; Brouwer, O.R.; Schepers, R.; Van Brussel, T.; Mohanty, S.K.; et al. Single-cell Atlas of Penile Cancer Reveals TP53 Mutations as a Driver of an Aggressive Phenotype, Irrespective of Human Papillomavirus Status, and Provides Clues for Treatment Personalization. Eur. Urol. 2024, 86, 114–127. [Google Scholar] [CrossRef] [PubMed]
- Breij, E.C.W.; de Goeij, B.E.C.G.; Verploegen, S.; Schuurhuis, D.H.; Amirkhosravi, A.; Francis, J.; Miller, V.B.; Houtkamp, M.; Bleeker, W.K.; Satijn, D.; et al. An Antibody-Drug Conjugate That Targets Tissue Factor Exhibits Potent Therapeutic Activity against a Broad Range of Solid Tumors. Cancer Res. 2014, 74, 1214–1226. [Google Scholar] [CrossRef] [PubMed]

| Patient Characteristics | Total | HPV Negative | HPV Positive | Adjusted p-Value |
| p53 status normal aberrant | 21 (65.6%) 11 (34.4%) | 7 (43.8%) 9 (56.2%) | 14 (87.5) 2 (12.5%) | 0.023 |
| p16 status negative positive | 17 (53.1%) 15 (46.9%) | 15 (93.8%) 1 (6.3%) | 2 (12.5%) 14 (87.5%) | < 0.001 |
| Patient characteristics | Total | p16 negative | p16 positive | Adjusted p-value |
| p53 status normal aberrant | 21 (65.6%) 11 (34.4%) | 6 (35.3%) 11 (64.7%) | 15 (100) 0 (0%) | < 0.001 |
| Recurrence-Free Survival (RFS) | |||
| Variable | Level * | HR (95% Cl for HR) | Adjusted p-Value |
| HPV | positive vs. negative | 0.45 (0.17–1.17) | 0.103 |
| p16 | positive vs. negative | 0.4 (0.15–1.07) | 0.103 |
| p53 | aberrant vs. normal | 4.06 (1.48–11.15) | 0.020 |
| Cancer-Specific Survival (CSS) | |||
| Variable | Level | HR (95% Cl for HR) | Adjusted p-value |
| HPV | positive vs. negative | 0.23 (0.04–1.2) | 0.121 |
| p16 | positive vs. negative | 0.09 (0.01–0.73) | 0.073 |
| p53 | aberrant vs. normal | 4683379200.32 (0-Inf) ** | 1.00 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jackson, J.C.; Johns, A.C.; Campos Clemente, L.; Manuel, C.M.; Qiao, W.; Lu, W.; Khan, K.; Solis Soto, L.M.; Chahoud, J.; Rao, P.; et al. Tissue Factor Expression in Penile Squamous Cell Carcinoma: A Potential Marker of HPV-Independent Disease. Cancers 2025, 17, 3410. https://doi.org/10.3390/cancers17213410
Jackson JC, Johns AC, Campos Clemente L, Manuel CM, Qiao W, Lu W, Khan K, Solis Soto LM, Chahoud J, Rao P, et al. Tissue Factor Expression in Penile Squamous Cell Carcinoma: A Potential Marker of HPV-Independent Disease. Cancers. 2025; 17(21):3410. https://doi.org/10.3390/cancers17213410
Chicago/Turabian StyleJackson, Jamaal C., Andrew C. Johns, Leticia Campos Clemente, Christopher M. Manuel, Wei Qiao, Wei Lu, Khaja Khan, Luisa M. Solis Soto, Jad Chahoud, Priya Rao, and et al. 2025. "Tissue Factor Expression in Penile Squamous Cell Carcinoma: A Potential Marker of HPV-Independent Disease" Cancers 17, no. 21: 3410. https://doi.org/10.3390/cancers17213410
APA StyleJackson, J. C., Johns, A. C., Campos Clemente, L., Manuel, C. M., Qiao, W., Lu, W., Khan, K., Solis Soto, L. M., Chahoud, J., Rao, P., Campbell, M. T., Pettaway, C. A., & Zacharias, N. M. (2025). Tissue Factor Expression in Penile Squamous Cell Carcinoma: A Potential Marker of HPV-Independent Disease. Cancers, 17(21), 3410. https://doi.org/10.3390/cancers17213410









