The Role of Multidisciplinary Ocular and Periocular Cancers Meetings in Uveal Melanoma Management: A 2-Year Analysis
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. MDTB Composition
2.2. Satisfaction Questionnaire
- Would you be in favor of having your case discussed in a multidisciplinary meeting? Meetings are held fortnightly and this could lengthen the clinical-therapeutic decision time. Response: yes or no.
- 2.
- Discussing your case in a multidisciplinary meeting how much more confident you feel in the suggested treatment? Answer score range 1 to 5.
- 3.
- How involved do you feel in the decision-making process about your case? answer score range 1 to 5.
- 4.
- Would you like to be involved in multidisciplinary meetings whenever possible? Answer score range 1 to 5.
- 5.
- Do you believe that a multidisciplinary discussion can provide a stronger adherence of the suggested clinical-therapeutic pathway to the international guidelines? answer score range 1 to 5.
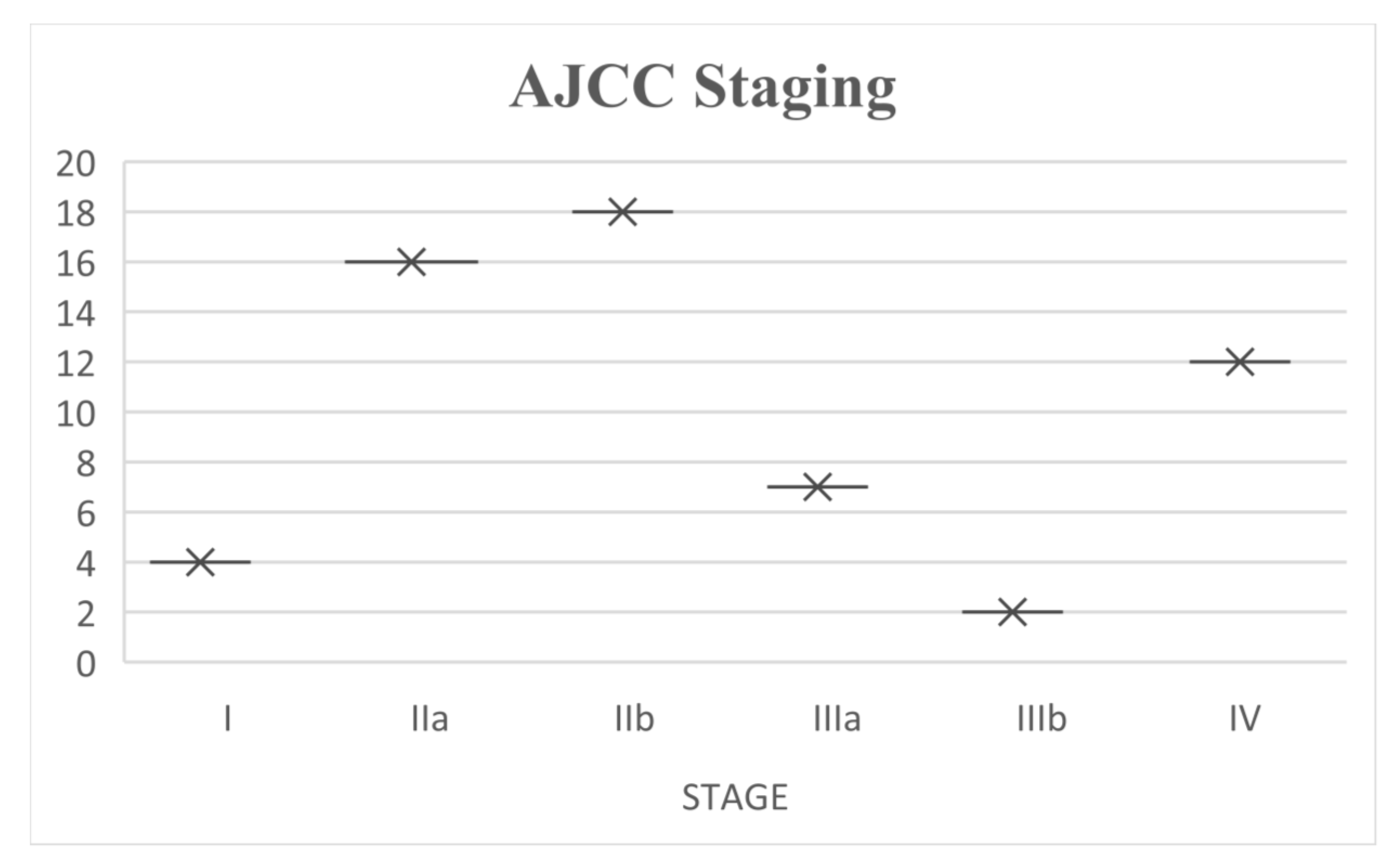
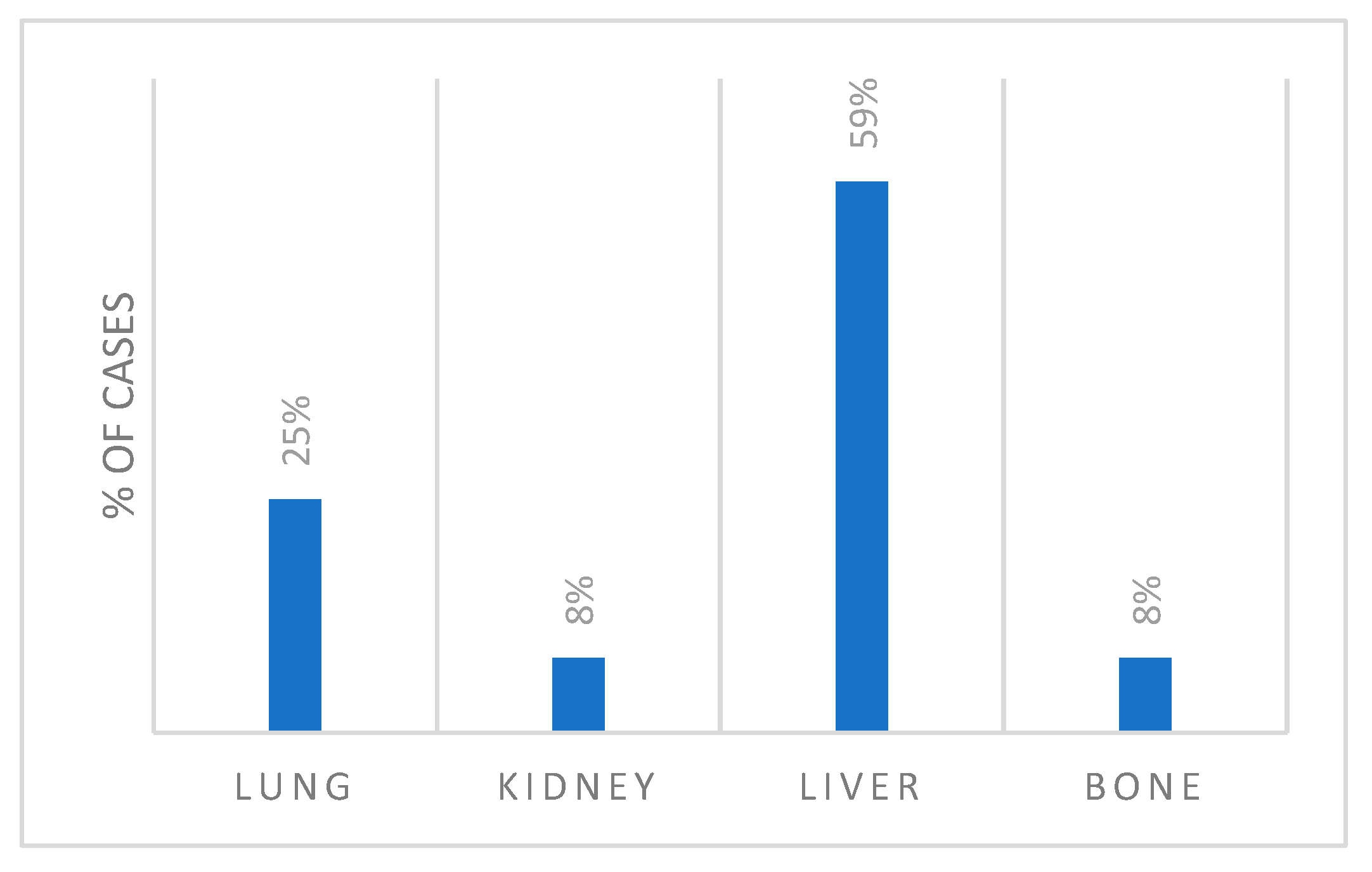
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Singh, A.D.; Turell, M.E.; Topham, A.K. Uveal melanoma: Trends in incidence, treatment, and survival. Ophthalmology 2011, 118, 1881–1885. [Google Scholar] [CrossRef] [PubMed]
- Krantz, B.A.; Dave, N.; Komatsubara, K.M.; Marr, B.P.; Carvajal, R.D. Uveal melanoma: Epidemiology, etiology, and treatment of primary disease. Clin. Ophthalmol. 2017, 11, 279–289. [Google Scholar] [CrossRef] [PubMed]
- Damato, B.; Heimann, H. Personalized treatment of uveal melanoma. Eye 2013, 27, 172–179. [Google Scholar] [CrossRef]
- Diener-West, M.; Earle, J.D.; Fine, S.L.; Hawkins, B.S.; Moy, C.S.; Reynolds, S.M.; Schachat, A.P.; Straatsma, B.R. The COMS randomized trial of iodine 125 brachytherapy for choroidal melanoma, III: Initial mortality findings. COMS Report No. 18. Arch. Ophthalmol. 2001, 119, 969–982. [Google Scholar] [CrossRef]
- Dell’Istituto Superiore di Sanità. Diagnosi e Trattamento del Melanoma Uveale; Associazione Italiana Medici Oculisti: Rome, Italy, 2024. [Google Scholar]
- Hawkins, B.S. The Collaborative Ocular Melanoma Study (COMS) randomized trial of pre-enucleation radiation of large choroidal melanoma: IV. Ten-year mortality findings and prognostic factors. COMS report number 24. Am. J. Ophthalmol. 2004, 138, 936–951. [Google Scholar] [CrossRef] [PubMed]
- Amin, M.B.; Greene, F.L.; Edge, S.B.; Compton, C.C.; Gershenwald, J.E.; Brookland, R.K.; Meyer, L.; Gress, D.M.; Byrd, D.R.; Winchester, D.P. The Eighth Edition AJCC Cancer Staging Manual: Continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J. Clin. 2017, 67, 93–99. [Google Scholar] [CrossRef]
- Rao, P.K.; Barker, C.; Coit, D.G.; Joseph, R.W.; Materin, M.; Rengan, R.; Sosman, J.; Thompson, J.A.; Albertini, M.R.; Boland, G.; et al. NCCN Guidelines Insights: Uveal Melanoma, Version 1.2019. J. Natl. Compr. Cancer Netw. 2020, 18, 120–131. [Google Scholar] [CrossRef]
- Hussain, R.N.; Chiu, A.; Pittam, B.; Taktak, A.; Damato, B.E.; Kacperek, A.; Errington, D.; Cauchi, P.; Chadha, V.; Connolly, J.; et al. Proton beam radiotherapy for choroidal and ciliary body melanoma in the UK-national audit of referral patterns of 1084 cases. Eye 2023, 37, 1033–1036. [Google Scholar] [CrossRef]
- NCCN Guidelines-Melanoma: Uveal.
- McLean, L.C.I.W.; Foster, W.D.; Zimmerman, L.E. Uveal melanoma: Location, size, cell type, and enucleation as risk factors in metastasis. Human. Pathol. 1982, 13, 123–132. [Google Scholar] [CrossRef]
- Savino, G.; Piccinni, F.; Pagliara, M.M.; Sammarco, M.G.; Caputo, C.G.; Moro, A.; Barbera, G.; Tagliaferri, L.; Fionda, B.; Schinzari, G.; et al. Multidisciplinary ocular and periocular cancers meetings: Implementation in a tertiary referral center and analysis over a 12-months period. BMC Ophthalmol. 2022, 22, 497. [Google Scholar] [CrossRef]
- El Saghir, N.S.; Keating, N.L.; Carlson, R.W.; Khoury, K.E.; Fallowfield, L. Tumor boards: Optimizing the structure and improving efficiency of multidisciplinary management of patients with cancer worldwide. In American Society of Clinical Oncology Educational Book; American Society of Clinical Oncology: Alexandria, VA, USA, 2014; pp. e461–e466. [Google Scholar] [CrossRef]
- Keating, N.L.; Landrum, M.B.; Lamont, E.B.; Bozeman, S.R.; Shulman, L.N.; McNeil, B.J. Tumor boards and the quality of cancer care. J. Natl. Cancer Inst. 2013, 105, 113–121. [Google Scholar] [CrossRef]
- Vinod, S.K.; Sidhom, M.A.; Delaney, G.P. Do multidisciplinary meetings follow guideline-based care? J. Oncol. Pract. 2010, 6, 276–281. [Google Scholar] [CrossRef] [PubMed]
- Krause, A.; Stocker, G.; Gockel, I.; Seehofer, D.; Hoffmeister, A.; Bläker, H.; Denecke, T.; Kluge, R.; Lordick, F.; Knödler, M. Guideline adherence and implementation of tumor board therapy recommendations for patients with gastrointestinal cancer. J. Cancer Res. Clin. Oncol. 2023, 149, 1231–1240. [Google Scholar] [CrossRef] [PubMed]
- Walter, J.; Moeller, C.; Resuli, B.; Kauffmann-Guerrero, D.; Manapov, F.; Dinkel, J.; Neumann, J.; Kovacs, J.; Schneider, C.; Huber, R.M.; et al. Guideline adherence of tumor board recommendations in lung cancer and transfer into clinical practice. J. Cancer Res. Clin. Oncol. 2023, 149, 11679–11688. [Google Scholar] [CrossRef] [PubMed]
- Licitra, L.; Keilholz, U.; Tahara, M.; Lin, J.-C.; Chomette, P.; Ceruse, P.; Harrington, K.; Mesia, R. Evaluation of the benefit and use of multidisciplinary teams in the treatment of head and neck cancer. Oral. Oncol. 2016, 59, 73–79. [Google Scholar] [CrossRef]
- Shah, M.A.; Lynch, E.; Cauchi, P.; Chadha, V. One Year of the Ocular Oncology Multidisciplinary Team Meeting—Has it Made a Difference? Clin. Oncol. (R. Coll. Radiol.) 2019, 31, 400. [Google Scholar] [CrossRef]
- Virgili, G.; Gatta, G.; Ciccolallo, L.; Capocaccia, R.; Biggeri, A.; Crocetti, E.; Lutz, J.M.; Paci, E. Incidence of uveal melanoma in Europe. Ophthalmology 2007, 114, 2309–2315. [Google Scholar] [CrossRef]
- Collaborative Ocular Melanoma Study Group. Histopathologic characteristics of uveal melanomas in eyes enucleated from the Collaborative Ocular Melanoma Study. COMS report no. 6. Am. J. Ophthalmol. 1998, 125, 745–766. [Google Scholar] [CrossRef]
- Khoja, L.; Atenafu, E.G.; Suciu, S.; Leyvraz, S.; Sato, T.; Marshall, E.; Keilholz, U.; Zimmer, L.; Patel, S.P.; Piperno-Neumann, S.; et al. Meta-analysis in metastatic uveal melanoma to determine progression free and overall survival benchmarks: An international rare cancers initiative (IRCI) ocular melanoma study. Ann. Oncol. 2019, 30, 1370–1380. [Google Scholar] [CrossRef]
- Rantala, E.S.; Hernberg, M.; Kivelä, T.T. Overall survival after treatment for metastatic uveal melanoma: A systematic review and meta-analysis. Melanoma Res. 2019, 29, 561–568. [Google Scholar] [CrossRef]
- Carvajal, R.D.; Nathan, P.; Sacco, J.J.; Orloff, M.; Hernandez-Aya, L.F.; Yang, J.; Luke, J.J.; Butler, M.O.; Stanhope, S.; Collins, L.; et al. Phase I Study of Safety, Tolerability, and Efficacy of Tebentafusp Using a Step-Up Dosing Regimen and Expansion in Patients with Metastatic Uveal Melanoma. J. Clin. Oncol. 2022, 40, 1939–1948. [Google Scholar] [CrossRef] [PubMed]
| MDTB Outcome | n = 59 |
|---|---|
| Referral to Liver Surgeon | 2 (4%) |
| Ruthenium Plaque Brachytherapy | 12 (21%) |
| Liver Radiotherapy | 2 (4%) |
| Ocular Oncology Follow-Up | 7 (12%) |
| Further Imaging Request | 12(21%) |
| Enucleation | 4 (7%) |
| External Beam Radiotherapy | 1(1%) |
| Referral to Medical Oncologist | 12 (20%) |
| Proton Beam Therapy | 5 (9%) |
| Referral to Radiotherapist | 1 (1%) |
| Transscleral Resection | 1(1%) |
| Question | 1 (n=) | 2 (n=) | 3 (n=) | 4 (n=) | 5 (n=) | No Score |
|---|---|---|---|---|---|---|
| Discussing your case in a multidisciplinary meeting how much more confident you feel in the suggested treatment? | - | - | - | 17 | 42 | - |
| How involved do you feel in the decision-making process about your case? | 1 | 4 | 9 | 11 | 35 | - |
| Would you like to be involved in multidisciplinary meetings whenever possible? | - | - | - | - | 59 | - |
| Do you believe that a multidisciplinary discussion can provide a stronger adherence of the suggested clinical-therapeutic pathway to the international guidelines? | - | - | - | 12 | 41 | 6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Savino, G.; Pagliara, M.M.; Sammarco, M.G.; Caputo, C.G.; Blasi, M.A.; Mattei, R.; Marcelli, S.; Tagliaferri, L.; Fionda, B.; Schinzari, G.; et al. The Role of Multidisciplinary Ocular and Periocular Cancers Meetings in Uveal Melanoma Management: A 2-Year Analysis. Cancers 2025, 17, 2274. https://doi.org/10.3390/cancers17142274
Savino G, Pagliara MM, Sammarco MG, Caputo CG, Blasi MA, Mattei R, Marcelli S, Tagliaferri L, Fionda B, Schinzari G, et al. The Role of Multidisciplinary Ocular and Periocular Cancers Meetings in Uveal Melanoma Management: A 2-Year Analysis. Cancers. 2025; 17(14):2274. https://doi.org/10.3390/cancers17142274
Chicago/Turabian StyleSavino, Gustavo, Monica Maria Pagliara, Maria Grazia Sammarco, Carmela Grazia Caputo, Maria Antonietta Blasi, Roberta Mattei, Sofia Marcelli, Luca Tagliaferri, Bruno Fionda, Giovanni Schinzari, and et al. 2025. "The Role of Multidisciplinary Ocular and Periocular Cancers Meetings in Uveal Melanoma Management: A 2-Year Analysis" Cancers 17, no. 14: 2274. https://doi.org/10.3390/cancers17142274
APA StyleSavino, G., Pagliara, M. M., Sammarco, M. G., Caputo, C. G., Blasi, M. A., Mattei, R., Marcelli, S., Tagliaferri, L., Fionda, B., Schinzari, G., Rossi, E., Zagaria, L., Tartaglione, T., Ausili Cefaro, L., Todaro, M., Moro, A., & Giannuzzi, F. (2025). The Role of Multidisciplinary Ocular and Periocular Cancers Meetings in Uveal Melanoma Management: A 2-Year Analysis. Cancers, 17(14), 2274. https://doi.org/10.3390/cancers17142274






