Contemporary Outcomes of Robot-Assisted Partial Nephrectomy: Results from Two European Referral Institutions
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population and Variable Definition
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ljungberg, B.; Chair-elect, A.B.; Albiges, L.; Bedke, J.; Capitanio, U.; Dabestani, S.; Hora, M.; Klatte, T.; Kuusk, T.; Lund, L.; et al. Renal Cell Carcinoma EAU Guidelines; EAU Guidelines Office: Arnhem, The Netherlands, 2024. [Google Scholar]
- Scosyrev, E.; Messing, E.M.; Sylvester, R.; Campbell, S.; Van Poppel, H. Renal function after nephron-sparing surgery versus radical nephrectomy: Results from EORTC randomized trial 30904. Eur. Urol. 2014, 65, 372–377. [Google Scholar] [CrossRef]
- Motzer, R.J.; Jonasch, E.; Agarwal, N.; Alva, A.; Baine, M.; Beckermann, K.; Carlo, M.I.; Choueiri, T.K.; Costello, B.A.; Derweesh, I.H.; et al. Kidney Cancer, Version 3.2022, NCCN Clinical Practice Guidelines in Oncology. JNCCN J. Natl. Compr. Cancer Netw. 2022, 20, 71–90. [Google Scholar] [CrossRef]
- Baudo, A.; Incesu, R.B.; Morra, S.; Scheipner, L.; Jannello, L.M.I.; de Angelis, M.; Siech, C.; Tian, Z.; Acquati, P.; Tilki, D.; et al. Other-Cause Mortality, According to Partial vs. Radical Nephrectomy: Age and Stage Analyses. Clin. Genitourin. Cancer 2024, 22, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Marchioni, M.; Preisser, F.; Bandini, M.; Nazzani, S.; Tian, Z.; Kapoor, A.; Cindolo, L.; Abdollah, F.; Tilki, D.; Briganti, A.; et al. Comparison of Partial Versus Radical Nephrectomy Effect on Other-cause Mortality, Cancer-specific Mortality, and 30-day Mortality in Patients Older Than 75 Years. Eur. Urol. Focus 2019, 5, 467–473. [Google Scholar] [CrossRef]
- Wang, Z.; Wang, G.; Xia, Q.; Shang, Z.; Yu, X.; Wang, M.; Jin, X. Partial nephrectomy vs. radical nephrectomy for renal tumors: A meta-analysis of renal function and cardiovascular outcomes. Urol. Oncol. Semin. Orig. Investig. 2016, 34, 533.e11–533.e19. [Google Scholar] [CrossRef]
- Capitanio, U.; Terrone, C.; Antonelli, A.; Minervini, A.; Volpe, A.; Furlan, M.; Matloob, R.; Regis, F.; Fiori, C.; Porpiglia, F.; et al. Nephron-sparing techniques independently decrease the risk of cardiovascular events relative to radical nephrectomy in patients with a T1a-T1b renal mass and normal preoperative renal function. Eur. Urol. 2015, 67, 683–689. [Google Scholar] [CrossRef] [PubMed]
- Bravi, C.A.; Larcher, A.; Capitanio, U.; Mari, A.; Antonelli, A.; Artibani, W.; Barale, M.; Bertini, R.; Bove, P.; Brunocilla, E.; et al. Perioperative Outcomes of Open, Laparoscopic, and Robotic Partial Nephrectomy: A Prospective Multicenter Observational Study (The RECORd 2 Project). Eur. Urol. Focus 2021, 7, 390–396. [Google Scholar] [CrossRef] [PubMed]
- Bertolo, R.; Garisto, J.; Dagenais, J.; Sagalovich, D.; Stein, R.; Fareed, K.; Gao, T.; Armanyous, S.; Fergany, A.; Lioudis, M.; et al. Transperitoneal Robot-assisted Partial Nephrectomy with Minimum Follow-up of 5 Years: Oncological and Functional Outcomes from a Single Institution. Eur. Urol. Oncol. 2019, 2, 207–213. [Google Scholar] [CrossRef]
- Tappero, S.; Bravi, C.A.; Khene, Z.E.; Campi, R.; Pecoraro, A.; Diana, P.; Re, C.; Giulioni, C.; Beksac, A.T.; Bertolo, R.; et al. Assessing Functional Outcomes of Partial Versus Radical Nephrectomy for T1b-T2 Renal Masses: Results from a Multi-institutional Collaboration. Ann. Surg. Oncol. 2024, 31, 5465–5472. [Google Scholar] [CrossRef]
- Larcher, A.; Muttin, F.; Peyronnet, B.; De Naeyer, G.; Khene, Z.E.; Dell’Oglio, P.; Ferreiro, C.; Schatteman, P.; Capitanio, U.; D’Hondt, F.; et al. The Learning Curve for Robot-assisted Partial Nephrectomy: Impact of Surgical Experience on Perioperative Outcomes. Eur. Urol. 2019, 75, 253–256. [Google Scholar] [CrossRef]
- Vickers, A.J.; Bianco, F.J.; Serio, A.M.; Eastham, J.A.; Schrag, D.; Klein, E.A.; Reuther, A.M.; Kattan, M.W.; Pontes, J.E.; Scardino, P.T. The surgical learning curve for prostate cancer control after radical prostatectomy. J. Natl. Cancer Inst. 2007, 99, 1171–1177. [Google Scholar] [CrossRef] [PubMed]
- Bravi, C.A.; Mottaran, A.; Sarchi, L.; Piro, A.; Paciotti, M.; Nocera, L.; Piramide, F.; Balestrazzi, E.; Peraire, M.; Farinha, R.; et al. Transitioning from Da Vinci Si to Xi: Assessing surgical outcomes at a high-volume robotic center. World J. Urol. 2023, 41, 3737–3744. [Google Scholar] [CrossRef]
- Cignoli, D.; Fallara, G.; Larcher, A.; Rosiello, G.; Montorsi, F.; Capitanio, U. How to improve outcome in nephron-sparing surgery: The impact of new techniques. Curr. Opin. Urol. 2021, 31, 255–261. [Google Scholar] [CrossRef]
- Mottrie, A.; Koliakos, N.; Denaeyer, G.; Willemsen, P.; Buffi, N.; Schatteman, P.; Fonteyne, E. Tumor enucleoresection in robot-assisted partial nephrectomy. J. Robot. Surg. 2009, 3, 65–69. [Google Scholar] [CrossRef]
- Kutikov, A.; Uzzo, R.G. The R.E.N.A.L. Nephrometry Score: A Comprehensive Standardized System for Quantitating Renal Tumor Size, Location and Depth. J. Urol. 2009, 182, 844–853. [Google Scholar] [CrossRef] [PubMed]
- Borgmann, H.; Reiss, A.K.; Kurosch, M.; Filmann, N.; Frees, S.; Mager, R.; Tsaur, I.; Haferkamp, A. R.E.N.A.L. Score Outperforms PADUA Score, C-Index and DAP Score for Outcome Prediction of Nephron Sparing Surgery in a Selected Cohort. J. Urol. 2016, 196, 664–671. [Google Scholar] [CrossRef]
- O’Callaghan, C.A.; Shine, B.; Lasserson, D.S. Chronic kidney disease: A large-scale population-based study of the effects of introducing the CKD-EPI formula for eGFR reporting. BMJ Open 2011, 1, e000308. [Google Scholar] [CrossRef] [PubMed]
- Clavien, P.A.; Barkun, J.; De Oliveira, M.L.; Vauthey, J.N.; Dindo, D.; Schulick, R.D.; De Santibañes, E.; Pekolj, J.; Slankamenac, K.; Bassi, C.; et al. The clavien-dindo classification of surgical complications: Five-year experience. Ann. Surg. 2009, 250, 187–196. [Google Scholar] [CrossRef]
- Assel, M.; Sjoberg, D.; Elders, A.; Wang, X.; Huo, D.; Botchway, A.; Delfino, K.; Fan, Y.; Zhao, Z.; Koyama, T.; et al. Guidelines for reporting of statistics for clinical research in urology. J. Urol. 2019, 201, 595–604. [Google Scholar] [CrossRef]
- Vickers, A.J.; Assel, M.J.; Sjoberg, D.D.; Qin, R.; Zhao, Z.; Koyama, T.; Botchway, A.; Wang, X.; Huo, D.; Kattan, M.; et al. Guidelines for Reporting of Figures and Tables for Clinical Research in Urology. BJU Int. 2020, 126, 14–25. [Google Scholar] [CrossRef]
- R Foundation. The R Project for Statistical Computing; R Foundation: Vienna, Austria, 2023. [Google Scholar]
- Paulucci, D.J.; Abaza, R.; Eun, D.D.; Hemal, A.K.; Badani, K.K. Robot-assisted partial nephrectomy: Continued refinement of outcomes beyond the initial learning curve. BJU Int. 2017, 119, 748–754. [Google Scholar] [CrossRef]
- Thompson, R.H.; Lane, B.R.; Lohse, C.M.; Leibovich, B.C.; Fergany, A.; Frank, I.; Gill, I.S.; Blute, M.L.; Campbell, S.C. Every minute counts when the renal hilum is clamped during partial nephrectomy. Eur. Urol. 2010, 58, 340–345. [Google Scholar] [CrossRef] [PubMed]
- Antonelli, A.; Cindolo, L.; Sandri, M.; Veccia, A.; Annino, F.; Bertagna, F.; Carini, M.; Celia, A.; D’ Orta, C.; De Concilio, B.; et al. Is off-clamp robot-assisted partial nephrectomy beneficial for renal function? Data from the CLOCK trial. BJU Int. 2022, 129, 217–224. [Google Scholar] [CrossRef] [PubMed]
- Belmonte, M.; Frego, N.; Ticonosco, M.; Pissavini, A.; Balestrazzi, E.; Sorce, G.; Barletta, F.; Rebuffo, S.; Collà Ruvolo, C.; Morra, S.; et al. On-clamp vs off-clamp robot-assisted partial nephrectomy for achieving modified trifecta: Inverse probability of treatment weighting analysis from a high-volume tertiary robotic center. J. Robot. Surg. 2024, 18, 327. [Google Scholar] [CrossRef] [PubMed]
- Simone, G.; Gill, I.S.; Mottrie, A.; Kutikov, A.; Patard, J.J.; Alcaraz, A.; Rogers, C.G. Indications, techniques, outcomes, and limitations for minimally ischemic and off-clamp partial nephrectomy: A systematic review of the literature. Eur. Urol. 2015, 68, 632–640. [Google Scholar] [CrossRef]
- Mihai, I.; Dura, H.; Teodoru, C.A.; Todor, S.B.; Ichim, C.; Grigore, N.; Mohor, C.I.; Mihetiu, A.; Oprinca, G.; Bacalbasa, N.; et al. Intraoperative Ultrasound: Bridging the Gap between Laparoscopy and Surgical Precision during 3D Laparoscopic Partial Nephrectomies. Diagnostics 2024, 14, 942. [Google Scholar] [CrossRef] [PubMed]
- Cignoli, D.; Basile, G.; Fallara, G.; Rosiello, G.; Belladelli, F.; Cei, F.; Musso, G.; Re, C.; Bertini, R.; Karakiewicz, P.; et al. Risks and benefits of partial nephrectomy performed with limited or with zero ischaemia time. BJU Int. 2023, 132, 283–290. [Google Scholar] [CrossRef]
- Mir, M.C.; Ercole, C.; Takagi, T.; Zhang, Z.; Velet, L.; Remer, E.M.; Demirjian, S.; Campbell, S.C. Decline in renal function after partial nephrectomy: Etiology and prevention. J. Urol. 2015, 193, 1889–1898. [Google Scholar] [CrossRef]
- Porpiglia, F.; Fiori, C.; Bertolo, R.; Morra, I.; Russo, R.; Piccoli, G.; Angusti, T.; Podio, V. Long-term functional evaluation of the treated kidney in a prospective series of patients who underwent laparoscopic partial nephrectomy for small renal tumors. Eur. Urol. 2012, 62, 130–135. [Google Scholar] [CrossRef]
| Variables | Overall (n = 333) |
|---|---|
| Age at diagnosis (years) | |
| Median (IQR) | 65 (57–73) |
| R.E.N.A.L. score | |
| Median (IQR) | 7 (5–8) |
| BMI | |
| Median (IQR) | 27 (24–30) |
| Sex | |
| Male | 233 (70) |
| Female | 100 (30) |
| ASA score | |
| 1–2 | 261 (79) |
| 3–4 | 72 (21) |
| Tumor side | |
| Left | 158 (47) |
| Right | 175 (53) |
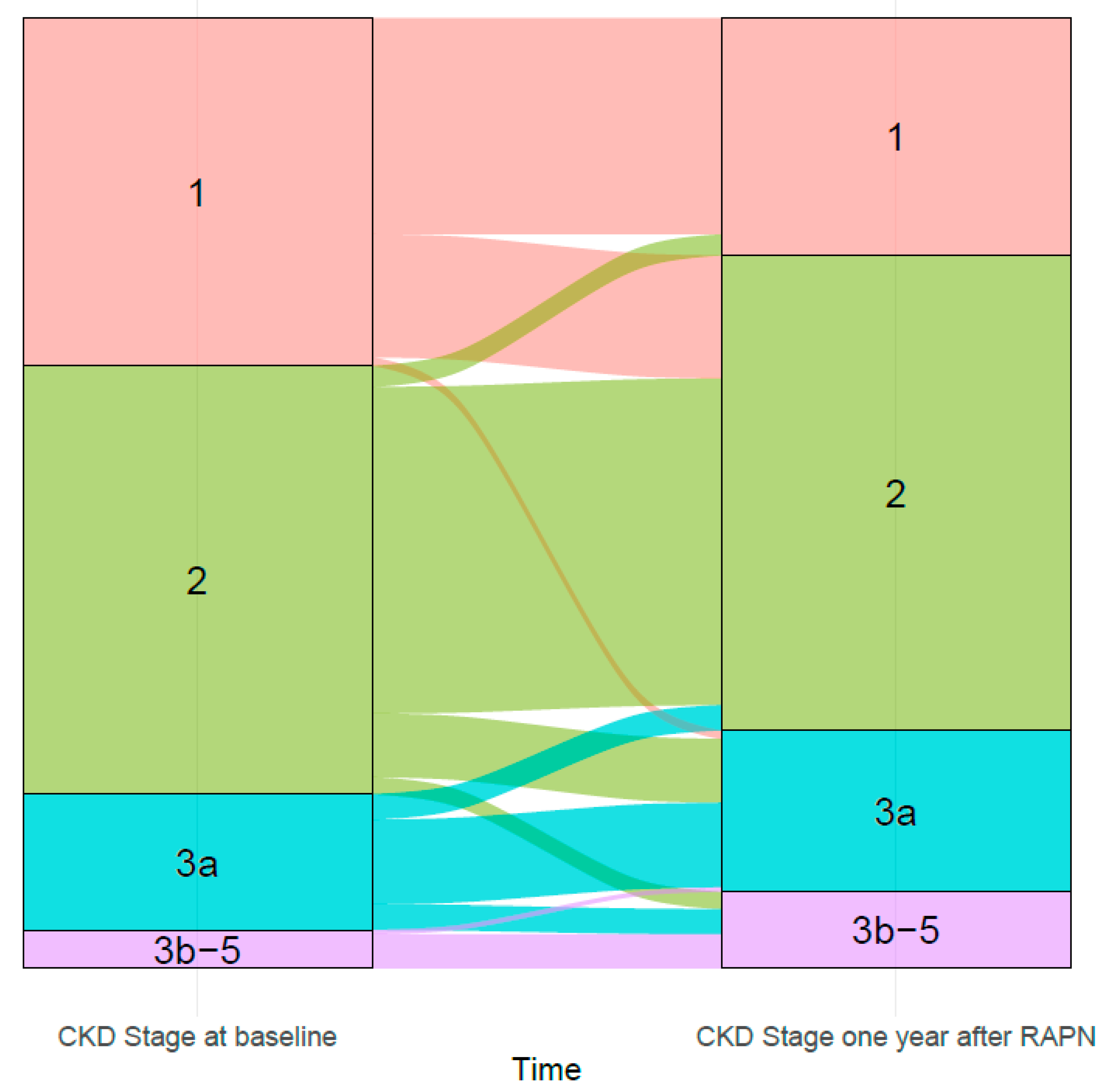
| CKD stage at diagnosis | |
| 1 | 83 (25) |
| 2 | 164 (49) |
| 3a | 43 (13) |
| 3b-5 | 43 (13) |
| CT stage | |
| 1a | 224 (67) |
| 1b | 89 (27) |
| 2 | 20 (6) |
| Console time (min) | 120 (95–150) |
| Median (IQR) | |
| Warm Ischemia time (min) * | 14 (10–18) |
| Median (IQR) | |
| Off-clamp technique | 90 (27) |
| Blood Loss (mL) | |
| 0–250 | 219 (66) |
| 251–500 | 84 (25) |
| >500 | 30 (9) |
| Clavien–Dindo >= 3a complication after surgery | 11 (3.3) |
| Length of stay (days) | |
| Median (IQR) | 2 (2–3) |
| CKD stage one year after surgery | |
| 1 | 86 (26) |
| 2 | 163 (49) |
| 3a | 57 (17) |
| 3b-5 | 27 (8.1) |
| CKD upstaging one year after surgery | 31 (9.4) |
| Predictors | OR (95%CI) | p-Value |
|---|---|---|
| R.E.N.A.L. Score | 0.69 (0.59–0.81) | <0.001 |
| Body Mass Index | 1.1 (0.99–1.1) | 0.097 |
| Age at surgery | 1.02 (0.98–1.04) | 0.26 |
| Chronic kidney disease stage | ||
| 1 | Ref. | - |
| 2 | 1.4 (0.71–2.85) | 0.3 |
| 3–4 | 1.8 (0.74–4.6) | 0.19 |
| Predictors | OR (95%CI) | p-Value |
|---|---|---|
| R.E.N.A.L. Score | 0.78 (0.65–0.93) | 0.008 |
| Body Mass Index | 0.97 (0.92–1.04) | 0.5 |
| Age at surgery | 0.99 (0.97–1.02) | 0.6 |
| Number of lesions | ||
| 1 | Ref. | - |
| >1 | 0.3 (0.12–0.7) | 0.07 |
| Off-clamp surgery | 1.08 (0.49–2.4) | 0.9 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barletta, F.; Frego, N.; de Angelis, M.; Resca, S.; Ticonosco, M.; Vecchio, E.; Tamburini, S.; Pissavini, A.; Mourullo, A.N.; Kroon, B.K.; et al. Contemporary Outcomes of Robot-Assisted Partial Nephrectomy: Results from Two European Referral Institutions. Cancers 2025, 17, 2104. https://doi.org/10.3390/cancers17132104
Barletta F, Frego N, de Angelis M, Resca S, Ticonosco M, Vecchio E, Tamburini S, Pissavini A, Mourullo AN, Kroon BK, et al. Contemporary Outcomes of Robot-Assisted Partial Nephrectomy: Results from Two European Referral Institutions. Cancers. 2025; 17(13):2104. https://doi.org/10.3390/cancers17132104
Chicago/Turabian StyleBarletta, Francesco, Nicola Frego, Mario de Angelis, Stefano Resca, Marco Ticonosco, Enrico Vecchio, Sara Tamburini, Alessandro Pissavini, Andrea Noya Mourullo, Bin K. Kroon, and et al. 2025. "Contemporary Outcomes of Robot-Assisted Partial Nephrectomy: Results from Two European Referral Institutions" Cancers 17, no. 13: 2104. https://doi.org/10.3390/cancers17132104
APA StyleBarletta, F., Frego, N., de Angelis, M., Resca, S., Ticonosco, M., Vecchio, E., Tamburini, S., Pissavini, A., Mourullo, A. N., Kroon, B. K., Smits, G., Papenburg, B., Lambert, E., D’Hondt, F., De Groote, R., Schatteman, P., Mottrie, A., & De Naeyer, G. (2025). Contemporary Outcomes of Robot-Assisted Partial Nephrectomy: Results from Two European Referral Institutions. Cancers, 17(13), 2104. https://doi.org/10.3390/cancers17132104






