Health Policy and Screening for Colorectal Cancer in the United States
Simple Summary
Abstract
1. Introduction
- -
- Administration of an index screening test.
- -
- Follow-up colonoscopy for a positive index test.
2. Eligibility and Affordability of Care and the ACA
3. Policies Addressing Screening Before the ACA
4. Effectiveness of the ACA in Improving CRC Screening Rates
4.1. CRC Screening Uptake and Medicare
4.2. CRC Screening Uptake in Medicaid Expansion States
4.3. CRC Screening Uptake and Commercial Insurance
4.4. CRC Screening and Socioeconomic Status
5. Equity in CRC Screening
6. The ACA and CRC Screening—Overall Policy Evaluation
6.1. Economic Criteria
6.2. Equity Criteria
6.3. Technical Criteria
6.4. Political Criteria
6.5. Administrative Criteria
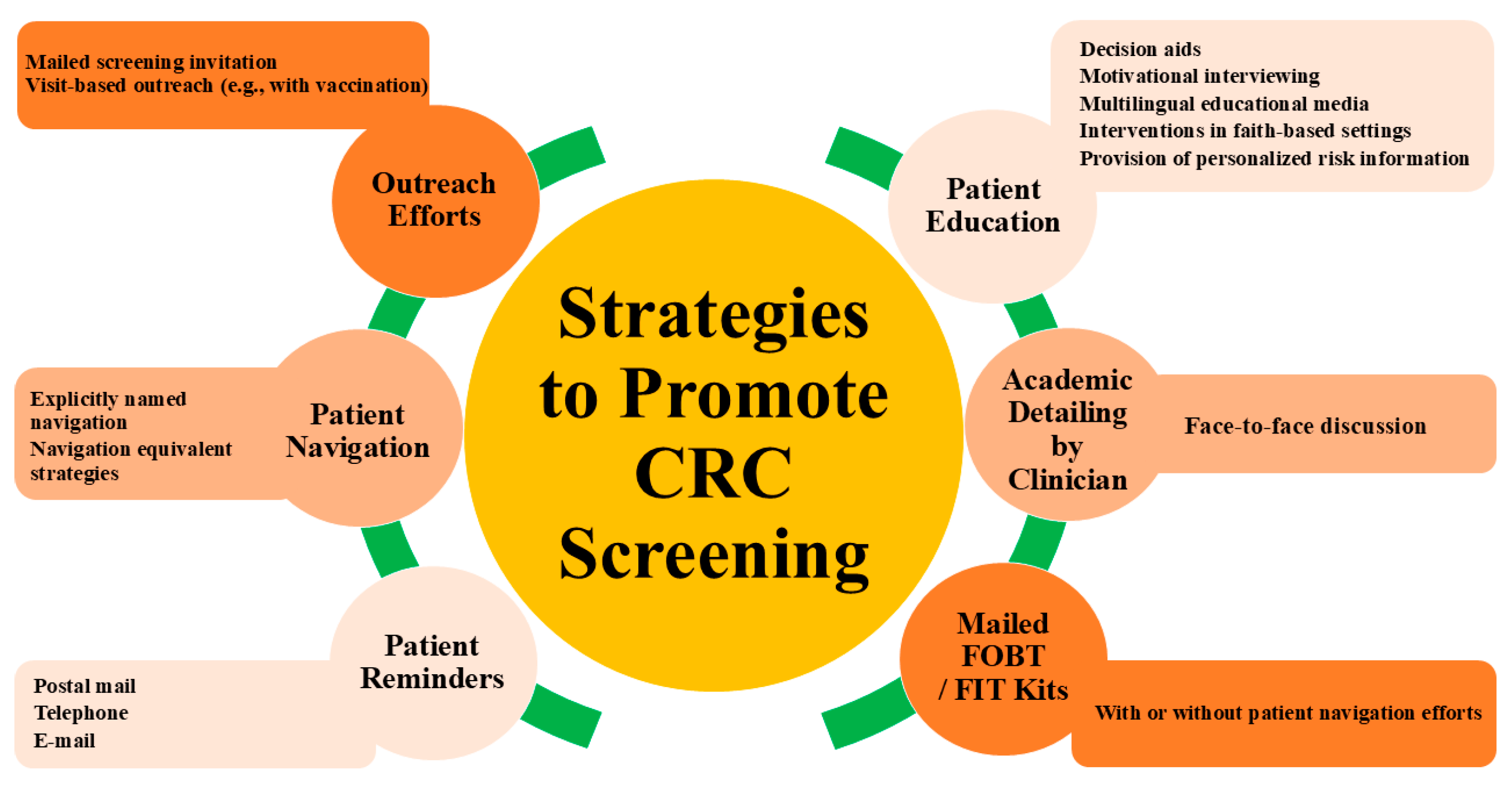
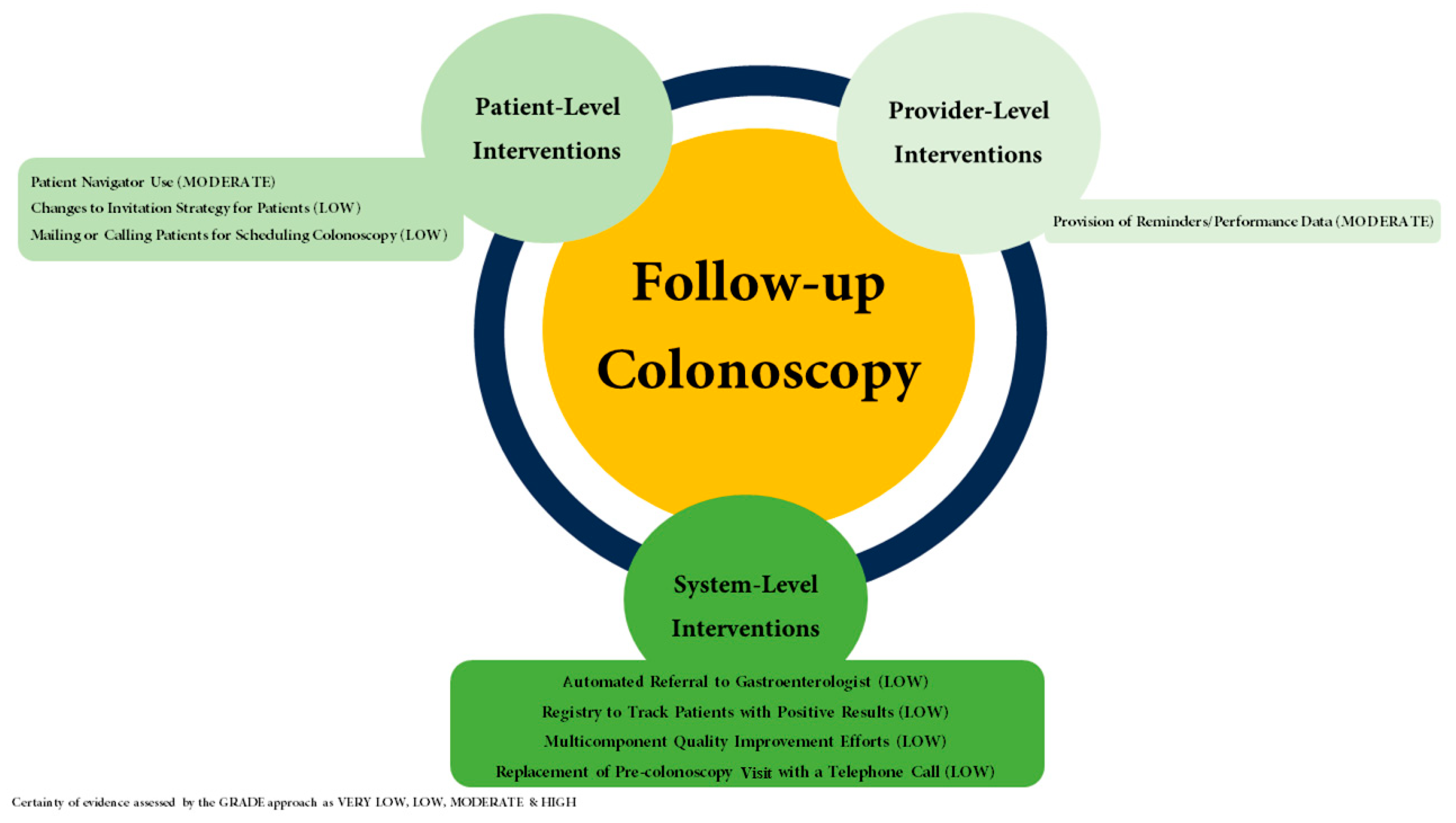
7. Policy Interventions for Colorectal Cancer Screening After the ACA
8. Acceptability of CRC Screening Modalities
9. The Benefits and Shortcomings of a Two-Step Approach to CRC Screening
- Screening colonoscopy: A colonoscopy may be classified as a screening test if it is the index test being performed for CRC screening and is not preceded by a positive non-invasive test.
- Diagnostic colonoscopy: A colonoscopy is classified as diagnostic for a variety of reasons. For this discussion, a colonoscopy is considered diagnostic rather than a screening test when it is preceded by a positive non-invasive test such as a positive stool test. Efforts are underway to label follow-up colonoscopies as screening rather than diagnostic after positive non-endoscopic CRC screening tests.
- Therapeutic colonoscopy: A colonoscopy is considered therapeutic when a polyp resection or intervention of a similar nature is performed. A screening or diagnostic colonoscopy may convert to a therapeutic colonoscopy when a polyp is removed.
- Health system-related factors: The delivery of instructions on diet and bowel preparation, adjusted by individual health literacy, acknowledging reservations and stigma that may exist surrounding a procedure performed trans-anally. Also worth considering is the administrative burden of scheduling and triaging colonoscopies; in a resource-limited health system, this variable is critical to the timely completion of a colonoscopy.
- Comorbidity-related factors: Obtaining peri-operative clearances; this may include appointments with consultants, the completion of tests required to give clearance, holding or bridging anti-coagulation therapy, and the follow-up appointment(s) for final pre-operative clearance.
- Logistical factors: Arranging transport in cases where sedation is used, a common practice for colonoscopies performed within the US. This may also entail arranging and paying for a child-care or an adult-care provider for the family member(s).
10. CRC Screening and Survival
11. CRC Screening and Health Policy—Bottom Line
12. Conclusions and Policy Recommendations
- Establishing the proportion of patients with an abnormal non-invasive screening test with a completed follow-up colonoscopy as a HEDIS quality metric. The US Multisociety Task Force on Colorectal Cancer (USMSTF) recommends at least an 80% completion rate of colonoscopy for patients with a positive FIT [2].
- Tracking time to a follow-up colonoscopy after a positive index screening test and establishing time to a follow-up colonoscopy as a HEDIS quality metric, with the aim to complete a follow-up colonoscopy within 9 months [50].
- The removal of all cost-sharing for a follow-up colonoscopy. This includes addressing insurance-related issues as has been performed under the “Removing Barriers to Colorectal Cancer Screening Act of 2020”. The implementation of such guidance does not extend to Medicare yet and should be a topic of future policymaking debates.
- Enabling reimbursement for outreach efforts with established efficacy in the completion of index CRC screening, the completion of a follow-up colonoscopy after a non-invasive screening test, and the completion of follow-up screening after a negative index screening test (Figure 2 and Figure 3) [67,68].
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- SEER Cancer Stat Facts Colorecatal Cancer. Available online: https://seer.cancer.gov/statfacts/html/colorect.html (accessed on 22 March 2023).
- US Preventive Services Task Force. Screening for Colorectal Cancer: US Preventive Services Task Force Recommendation Statement. JAMA 2021, 325, 1965–1977. [Google Scholar] [CrossRef]
- Explaining Litigation Challenging the ACA’s Preventive Services Requirements: Braidwood Management Inc. v. Becerra|KFF. Available online: https://www.kff.org/womens-health-policy/issue-brief/explaining-litigation-challenging-the-acas-preventive-services-requirements-braidwood-management-inc-v-becerra/ (accessed on 31 March 2023).
- FIT DNA Screening Results Have Multiple Implications for Follow-up Colonoscopy—Gastroenterology & Endoscopy News. Available online: https://www.gastroendonews.com/Endoscopy-Suite/Article/01-23/FIT-DNA-Screening-Results-Have-Multiple-Implications-for-Follow-up-Colonoscopy/69108 (accessed on 22 March 2023).
- ACA Income Limits: What Will Change in 2023?—GoodRx. Available online: https://www.goodrx.com/insurance/aca/aca-income-limits (accessed on 11 December 2022).
- Affordable Care Act Statistics and Facts|Policy Advice|Policy Advice. Available online: https://policyadvice.net/insurance/insights/affordable-care-act-statistics/ (accessed on 11 December 2022).
- McKenna, R.M.; Langellier, B.A.; Alcalá, H.E.; Roby, D.H.; Grande, D.T.; Ortega, A.N. The Affordable Care Act Attenuates Financial Strain According to Poverty Level. Inq. J. Health Care Organ. Provis. Financ. 2018, 55, 0046958018790164. [Google Scholar] [CrossRef]
- Allen, H.; Swanson, A.; Wang, J.; Gross, T. Early Medicaid Expansion Associated with Reduced Payday Borrowing in California. Health Aff. 2017, 36, 1769–1776. [Google Scholar] [CrossRef]
- Caswell, K.J.; Waidmann, T.A. The Affordable Care Act Medicaid Expansions and Personal Finance. Med. Care Res. Rev. 2017, 76, 538–571. [Google Scholar] [CrossRef]
- Campbell, A.L.; Sheppard, S. The Social, Political, and Economic Effects of the Affordable Care Act: Introduction to the Issue. RSF Russell Sage Found. J. Soc. Sci. 2020, 6, 1–40. [Google Scholar] [CrossRef]
- Altice, C.K.; Banegas, M.P.; Tucker-Seeley, R.D.; Yabroff, K.R. Financial Hardships Experienced by Cancer Survivors: A Systematic Review. JNCI J. Natl. Cancer Inst. 2016, 109, djw205. [Google Scholar] [CrossRef] [PubMed]
- Financial Toxicity and Cancer Treatment (PDQ®)—NCI. Available online: https://www.cancer.gov/about-cancer/managing-care/track-care-costs/financial-toxicity-hp-pdq (accessed on 16 July 2023).
- Herriges, M.J.; Shenhav-Goldberg, R.; Peck, J.I.; Bhanvadia, S.K.; Morgans, A.; Chino, F.; Chandrasekar, T.; Shapiro, O.; Jacob, J.M.; Basnet, A.; et al. Financial Toxicity and Its Association With Prostate and Colon Cancer Screening. J. Natl. Compr. Cancer Netw. 2022, 20, 981–988. [Google Scholar] [CrossRef]
- Uninsured Americans: Key Statistics & Facts|Fortunly. Available online: https://fortunly.com/statistics/uninsured-americans/ (accessed on 11 December 2022).
- The Affordable Care Act Helps America’s Uninsured|whitehouse.gov. Available online: https://obamawhitehouse.archives.gov/blog/2010/09/16/affordable-care-act-helps-america-s-uninsured (accessed on 11 December 2022).
- Kasich, J.R. H.R.2015—105th Congress (1997–1998): Balanced Budget Act of 1997. Published online 1997. Available online: http://www.congress.gov/ (accessed on 11 December 2022).
- Thomas, W.M. H.R.5661—106th Congress (1999–2000): Medicare, Medicaid, and SCHIP Benefits Improvement and Protection Act of 2000. Published online 2000. Available online: http://www.congress.gov/ (accessed on 11 December 2022).
- Bhandari, N.R.; Li, C. Impact of The Affordable Care Act’s Elimination of Cost-Sharing on the Guideline-Concordant Utilization of Cancer Preventive Screenings in the United States Using Medical Expenditure Panel Survey. Healthcare 2019, 7, 36. [Google Scholar] [CrossRef]
- Fedewa, S.A.; Goodman, M.; Flanders, W.D.; Han, X.; Smith, R.A.; Ward, E.M.; Doubeni, C.A.; Sauer, A.G.; Jemal, A. Elimination of cost-sharing and receipt of screening for colorectal and breast cancer. Cancer 2015, 121, 3272–3280. [Google Scholar] [CrossRef]
- Huguet, N.; Angier, H.; Rdesinski, R.; Hoopes, M.; Marino, M.; Holderness, H.; DeVoe, J.E. Cervical and colorectal cancer screening prevalence before and after Affordable Care Act Medicaid expansion. Prev. Med. 2019, 124, 91–97. [Google Scholar] [CrossRef]
- Davis, M.M.; Shafer, P.; Renfro, S.; Lich, K.H.; Shannon, J.; Coronado, G.D.; McConnell, K.J.; Wheeler, S.B. Does a transition to accountable care in Medicaid shift the modality of colorectal cancer testing? BMC Health Serv. Res. 2019, 19, 54. [Google Scholar] [CrossRef]
- Gan, T.; Sinner, H.F.; Walling, S.C.; Chen, Q.; Huang, B.; Tucker, T.C.; Patel, J.A.; Evers, B.M.; Bhakta, A.S. Impact of the Affordable Care Act on Colorectal Cancer Screening, Incidence, and Survival in Kentucky. J. Am. Coll. Surg. 2019, 228, 342–353.e1. [Google Scholar] [CrossRef]
- Zerhouni, Y.A.; Trinh, Q.-D.; Lipsitz, S.; Goldberg, J.; Irani, J.; Bleday, R.; Haider, A.H.; Melnitchouk, N. Effect of Medicaid Expansion on Colorectal Cancer Screening Rates. Dis. Colon Rectum 2019, 62, 97–103. [Google Scholar] [CrossRef]
- Fedewa, S.A.; Yabroff, K.R.; Smith, R.A.; Sauer, A.G.; Han, X.; Jemal, A. Changes in Breast and Colorectal Cancer Screening After Medicaid Expansion Under the Affordable Care Act. Am. J. Prev. Med. 2019, 57, 3–12. [Google Scholar] [CrossRef]
- Hendryx, M.; Luo, J. Increased Cancer Screening for Low-income Adults Under the Affordable Care Act Medicaid Expansion. Med. Care 2018, 56, 944–949. [Google Scholar] [CrossRef]
- Qian, Z.; Chen, X.; Pucheril, D.; Al Khatib, K.; Lucas, M.; Nguyen, D.-D.; McNabb-Baltar, J.; Lipsitz, S.R.; Melnitchouk, N.; Cole, A.P.; et al. Long-Term Impact of Medicaid Expansion on Colorectal Cancer Screening in Its Targeted Population. Dig. Dis. Sci. 2023, 68, 1780–1790. [Google Scholar] [CrossRef]
- Adult Core Set Reporting Resources|Medicaid. Available online: https://www.medicaid.gov/medicaid/quality-of-care/performance-measurement/adult-and-child-health-care-quality-measures/adult-core-set-reporting-resources/index.html (accessed on 4 July 2023).
- Mehta, S.J.; Polsky, D.; Zhu, J.; Lewis, J.D.; Kolstad, J.T.; Loewenstein, G.; Volpp, K.G. ACA-Mandated Elimination of Cost Sharing for Preventive Screening Has Had Limited Early Impact. Am. J. Manag. Care 2015, 21, 511–517. [Google Scholar] [CrossRef]
- Wharam, J.F.M.; Zhang, F.; Landon, B.E.M.; LeCates, R.M.; Soumerai, S.S.; Ross-Degnan, D.S. Colorectal Cancer Screening in a Nationwide High-deductible Health Plan Before and After the Affordable Care Act. Med. Care 2016, 54, 466–473. [Google Scholar] [CrossRef]
- Hamman, M.K.; Kapinos, K.A. Mandated Coverage of Preventive Care and Reduction in Disparities: Evidence from Colorectal Cancer Screening. Am. J. Public Health 2015, 105, S508–S516. [Google Scholar] [CrossRef] [PubMed]
- Richman, I.; Asch, S.M.; Bhattacharya, J.; Owens, D.K. Colorectal Cancer Screening in the Era of the Affordable Care Act. J. Gen. Intern. Med. 2015, 31, 315–320. [Google Scholar] [CrossRef] [PubMed]
- Fendrick, A.M.; Princic, N.; Miller-Wilson, L.-A.; Wilson, K.; Limburg, P. Out-of-Pocket Costs for Colonoscopy After Noninvasive Colorectal Cancer Screening Among US Adults with Commercial and Medicare Insurance. JAMA Netw. Open 2021, 4, e2136798. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.Y.; Joo, J.H.; Zhou, L.; Goswami, R.; Liao, J.M. The Impact of Payment Reform on Medicaid Access and Quality: A National Survey of Physicians. Perm. J. 2025, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Song, L.D.; Newhouse, J.P.; Garcia-De-Albeniz, X.; Hsu, J. Changes in screening colonoscopy following Medicare reimbursement and cost-sharing changes. Health Serv. Res. 2019, 54, 839–850. [Google Scholar] [CrossRef] [PubMed]
- Demb, J.; Gupta, S. Racial and Ethnic Disparities in Colorectal Cancer Screening Pose Persistent Challenges to Health Equity. Clin. Gastroenterol. Hepatol. 2019, 18, 1691–1693. [Google Scholar] [CrossRef]
- In Every Community—National Colorectal Cancer Roundtable. Available online: https://nccrt.org/80-in-every-community/ (accessed on 11 December 2022).
- Hitchcock, M.E.; Green, B.B.; Anderson, D.S. Advancing Health Equity for Medicaid Beneficiaries by Adding Colorectal Cancer Screening to the Centers for Medicare and Medicaid Services Adult Core Set. Gastroenterology 2022, 162, 710–714. [Google Scholar] [CrossRef]
- Siegel, R.L.; Wagle, N.S.; Cercek, A.; Smith, R.A.; Jemal, A. Colorectal cancer statistics, 2023. CA A Cancer J. Clin. 2023, 73, 233–254. [Google Scholar] [CrossRef]
- McLeod, M.R.; Galoosian, A.; May, F.P. Racial and Ethnic Disparities in Colorectal Cancer Screening and Outcomes. Hematol. Clin. N. Am. 2022, 36, 415–428. [Google Scholar] [CrossRef]
- Colorectal Cancer Screening|Cancer Trends Progress Report. Available online: https://progressreport.cancer.gov/detection/colorectal_cancer (accessed on 4 July 2023).
- Joseph, D.A.; King, J.B.; Dowling, N.F.; Thomas, C.C.; Richardson, L.C. Vital signs: Colorectal cancer screening test use—United States, 2018. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 253–259. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7075255/ (accessed on 4 July 2023). [CrossRef]
- Cancer Statistics Review, 1975–2018—SEER Statistics. Available online: https://seer.cancer.gov/archive/csr/1975_2018/ (accessed on 6 August 2023).
- Text-H.R.1570—116th Congress (2019–2020): Removing Barriers to Colorectal Cancer Screening Act of 2020. Published online 2020. Available online: http://www.congress.gov/ (accessed on 11 December 2022).
- Changes to Beneficiary Coinsurance When Colorectal Cancer Screenings Become Diagnostic—CIPROMS, Inc. Available online: https://www.cms.gov/files/document/mm12656-changes-beneficiary-coinsurance-additional-procedures-furnished-during-same-clinical.pdf (accessed on 22 March 2023).
- Federal Register: Medicare and Medicaid Programs; CY 2023 Payment Policies. Available online: https://www.federalregister.gov/documents/2022/07/29/2022-14562/medicare-and-medicaid-programs-cy-2023-payment-policies-under-the-physician-fee-schedule-and-other (accessed on 11 December 2022).
- Zhu, X.; Parks, P.D.; Weiser, E.; Fischer, K.; Griffin, J.M.; Limburg, P.J.; Rutten, L.J.F. National Survey of Patient Factors Associated with Colorectal Cancer Screening Preferences. Cancer Prev. Res. 2021, 14, 603–614. [Google Scholar] [CrossRef]
- Makaroff, K.E.; Shergill, J.; Lauzon, M.; Khalil, C.; Ahluwalia, S.C.; Spiegel, B.M.; Almario, C.V. Patient Preferences for Colorectal Cancer Screening Tests in Light of Lowering the Screening Age to 45 Years. Clin. Gastroenterol. Hepatol. 2022, 21, 520–531.e10. [Google Scholar] [CrossRef]
- Castells, A.; Quintero, E.; Bujanda, L.; Castán-Cameo, S.; Cubiella, J.; Díaz-Tasende, J.; Lanas, Á.; Ono, A.; Serra-Burriel, M.; Frías-Arrocha, E.; et al. Effect of invitation to colonoscopy versus faecal immunochemical test screening on colorectal cancer mortality (COLONPREV): A pragmatic, randomised, controlled, non-inferiority trial. Lancet 2025, 405, 1231–1239. [Google Scholar] [CrossRef] [PubMed]
- Rutten, L.J.F.; Parks, P.D.; Weiser, E.; Fan, C.; Jacobson, D.J.; Jenkins, G.D.; Zhu, X.; Griffin, J.M.; Limburg, P.J. Health Care Provider Characteristics Associated With Colorectal Cancer Screening Preferences and Use. Mayo Clin. Proc. 2021, 97, 101–109. [Google Scholar] [CrossRef] [PubMed]
- Forbes, N.; Hilsden, R.J.; Martel, M.; Ruan, Y.; Dube, C.; Rostom, A.; Shorr, R.; Menard, C.; Brenner, D.R.; Barkun, A.N.; et al. Association Between Time to Colonoscopy After Positive Fecal Testing and Colorectal Cancer Outcomes: A Systematic Review. Clin. Gastroenterol. Hepatol. 2021, 19, 1344–1354.e8. [Google Scholar] [CrossRef] [PubMed]
- Fendrick, A.M.; Borah, B.J.; Ozbay, A.B.; Saoud, L.; Limburg, P.J. Life-years gained resulting from screening colonoscopy compared with follow-up colonoscopy after a positive stool-based colorectal screening test. Prev. Med. Rep. 2022, 26, 101701. [Google Scholar] [CrossRef]
- Fedewa, S.A.; Star, J.; Bandi, P.; Minihan, A.; Han, X.; Yabroff, K.R.; Jemal, A. Changes in Cancer Screening in the US During the COVID-19 Pandemic. JAMA Netw. Open 2022, 5, e2215490. [Google Scholar] [CrossRef]
- Star, J.; Bandi, P.; Siegel, R.L.; Han, X.; Minihan, A.; Smith, R.A.; Jemal, A. Cancer Screening in the United States During the Second Year of the COVID-19 Pandemic. J. Clin. Oncol. 2023, 41, 4352–4359. [Google Scholar] [CrossRef]
- Le, Q.A.; Greene, M.; Gohil, S.; Ozbay, A.B.; Dore, M.; Fendrick, A.M.; Limburg, P. Adherence to multi-target stool DNA testing for colorectal cancer screening in the United States. Int. J. Color. Dis. 2025, 40, 16. [Google Scholar] [CrossRef]
- Zorzi, M.; Battagello, J.; Selby, K.; Capodaglio, G.; Baracco, S.; Rizzato, S.; Chinellato, E.; Guzzinati, S.; Rugge, M. Non-compliance with colonoscopy after a positive faecal immunochemical test doubles the risk of dying from colorectal cancer. Gut 2021, 71, 561–567. [Google Scholar] [CrossRef]
- Bharti, B.; May, F.F.P.; Nodora, J.; Martínez, M.E.; Moyano, K.; Davis, S.L.; Ramers, C.B.; Garcia-Bigley, F.; O’Connell, S.; Ronan, K.; et al. Diagnostic colonoscopy completion after abnormal fecal immunochemical testing and quality of tests used at 8 Federally Qualified Health Centers in Southern California: Opportunities for improving screening outcomes. Cancer 2019, 125, 4203–4209. [Google Scholar] [CrossRef]
- May, F.P.; Yano, E.M.; Provenzale, D.; Brunner, J.; Yu, C.; Phan, J.; Bharath, P.; Aby, E.; Dinh, D.; Ehrlich, D.S.; et al. Barriers to Follow-up Colonoscopies for Patients With Positive Results From Fecal Immunochemical Tests During Colorectal Cancer Screening. Clin. Gastroenterol. Hepatol. 2018, 17, 469–476. [Google Scholar] [CrossRef]
- Martin, J.; Halm, E.A.; Tiro, J.A.; Merchant, Z.; Balasubramanian, B.A.; McCallister, K.; Sanders, J.M.; Ahn, C.; Bishop, W.P.; Singal, A.G. Reasons for Lack of Diagnostic Colonoscopy After Positive Result on Fecal Immunochemical Test in a Safety-Net Health System. Am. J. Med. 2017, 130, 93.e1–93.e7. [Google Scholar] [CrossRef] [PubMed]
- Jetelina, K.K.; Yudkin, J.S.; Miller, S.; Berry, E.; Lieberman, A.; Gupta, S.; Balasubramanian, B.A. Patient-Reported Barriers to Completing a Diagnostic Colonoscopy Following Abnormal Fecal Immunochemical Test Among Uninsured Patients. J. Gen. Intern. Med. 2019, 34, 1730–1736. [Google Scholar] [CrossRef]
- Breen, N.; Skinner, C.S.; Zheng, Y.; Inrig, S.; Corley, D.A.; Beaber, E.F.; Garcia, M.; Chubak, J.; Doubeni, C.; Quinn, V.P.; et al. Time to Follow-up After Colorectal Cancer Screening by Health Insurance Type. Am. J. Prev. Med. 2019, 56, e143–e152. [Google Scholar] [CrossRef] [PubMed]
- de Lima, P.N.; Matrajt, L.; Coronado, G.; Escaron, A.L.; Rutter, C.M. Cost-Effectiveness of Noninvasive Colorectal Cancer Screening in Community Clinics. JAMA Netw. Open 2025, 8, e2454938. [Google Scholar] [CrossRef]
- Lissenden, B.; Yao, N. Affordable Care Act Changes to Medicare Led to Increased Diagnoses of Early-Stage Colorectal Cancer Among Seniors. Health Aff. 2017, 36, 101–107. [Google Scholar] [CrossRef]
- Jemal, A.; Lin, C.C.; Davidoff, A.J.; Han, X. Changes in Insurance Coverage and Stage at Diagnosis Among Nonelderly Patients with Cancer After the Affordable Care Act. J. Clin. Oncol. 2017, 35, 3906–3915. [Google Scholar] [CrossRef]
- Lee, C.; Kushi, L.H.; Reed, M.E.; Eldridge, E.H.; Lee, J.K.; Zhang, J.; Spiegelman, D. Impact of the Affordable Care Act on Colorectal Cancer Incidence and Mortality. Am. J. Prev. Med. 2021, 62, 387–394. [Google Scholar] [CrossRef]
- Bretthauer, M.; Løberg, M.; Wieszczy, P.; Kalager, M.; Emilsson, L.; Garborg, K.; Rupinski, M.; Dekker, E.; Spaander, M.; Bugajski, M.; et al. Effect of Colonoscopy Screening on Risks of Colorectal Cancer and Related Death. N. Engl. J. Med. 2022, 387, 1547–1556. [Google Scholar] [CrossRef] [PubMed]
- Fendrick, A.M.; Lieberman, D.; Vahdat, V.; Chen, J.V.; Ozbay, A.B.; Limburg, P.J. Cost-Effectiveness of Waiving Coinsurance for Follow-Up Colonoscopy after a Positive Stool-Based Colorectal Screening Test in a Medicare Population. Cancer Prev. Res. 2022, 15, 653–660. [Google Scholar] [CrossRef]
- Selby, K.; Baumgartner, C.; Levin, T.R.; Doubeni, C.A.; Zauber, A.G.; Schottinger, J.; Jensen, C.D.; Lee, J.K.; Corley, D.A. Interventions to Improve Follow-up of Positive Results on Fecal Blood Tests. Ann. Intern. Med. 2017, 167, 565–575. [Google Scholar] [CrossRef]
- Dougherty, M.K.; Brenner, A.T.; Crockett, S.D.; Gupta, S.; Wheeler, S.B.; Coker-Schwimmer, M.; Cubillos, L.; Malo, T.; Reuland, D.S. Evaluation of Interventions Intended to Increase Colorectal Cancer Screening Rates in the United States. JAMA Intern. Med. 2018, 178, 1645–1658. [Google Scholar] [CrossRef] [PubMed]

| Age Range | Recommendation | Grade | Screening Options |
|---|---|---|---|
| 45–49 years | Colorectal cancer screening is recommended for average-risk individuals | B | Colonoscopy—every 10 years High-sensitivity gFOBT—every year FIT—every year sDNA-FIT—every 1–3 years CT colonography—every 5 years Flexible sigmoidoscopy—every 5 years |
| 50–75 years | Colorectal cancer screening is recommended for average-risk individuals | A | |
| 76–85 years | Selectively offer colorectal cancer screening | C |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hussain, M.R.; Ali, F.S.; Larson, S.A.; Al Snih, S. Health Policy and Screening for Colorectal Cancer in the United States. Cancers 2025, 17, 2003. https://doi.org/10.3390/cancers17122003
Hussain MR, Ali FS, Larson SA, Al Snih S. Health Policy and Screening for Colorectal Cancer in the United States. Cancers. 2025; 17(12):2003. https://doi.org/10.3390/cancers17122003
Chicago/Turabian StyleHussain, Maryam R., Faisal S. Ali, Scott A. Larson, and Soham Al Snih. 2025. "Health Policy and Screening for Colorectal Cancer in the United States" Cancers 17, no. 12: 2003. https://doi.org/10.3390/cancers17122003
APA StyleHussain, M. R., Ali, F. S., Larson, S. A., & Al Snih, S. (2025). Health Policy and Screening for Colorectal Cancer in the United States. Cancers, 17(12), 2003. https://doi.org/10.3390/cancers17122003





