Italian Oncology at the Crossroads: Between Hospital Bed Cuts and the Need for a Transition to Integrated Community-Based Simultaneous Care
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample
2.2. Statistical Analysis
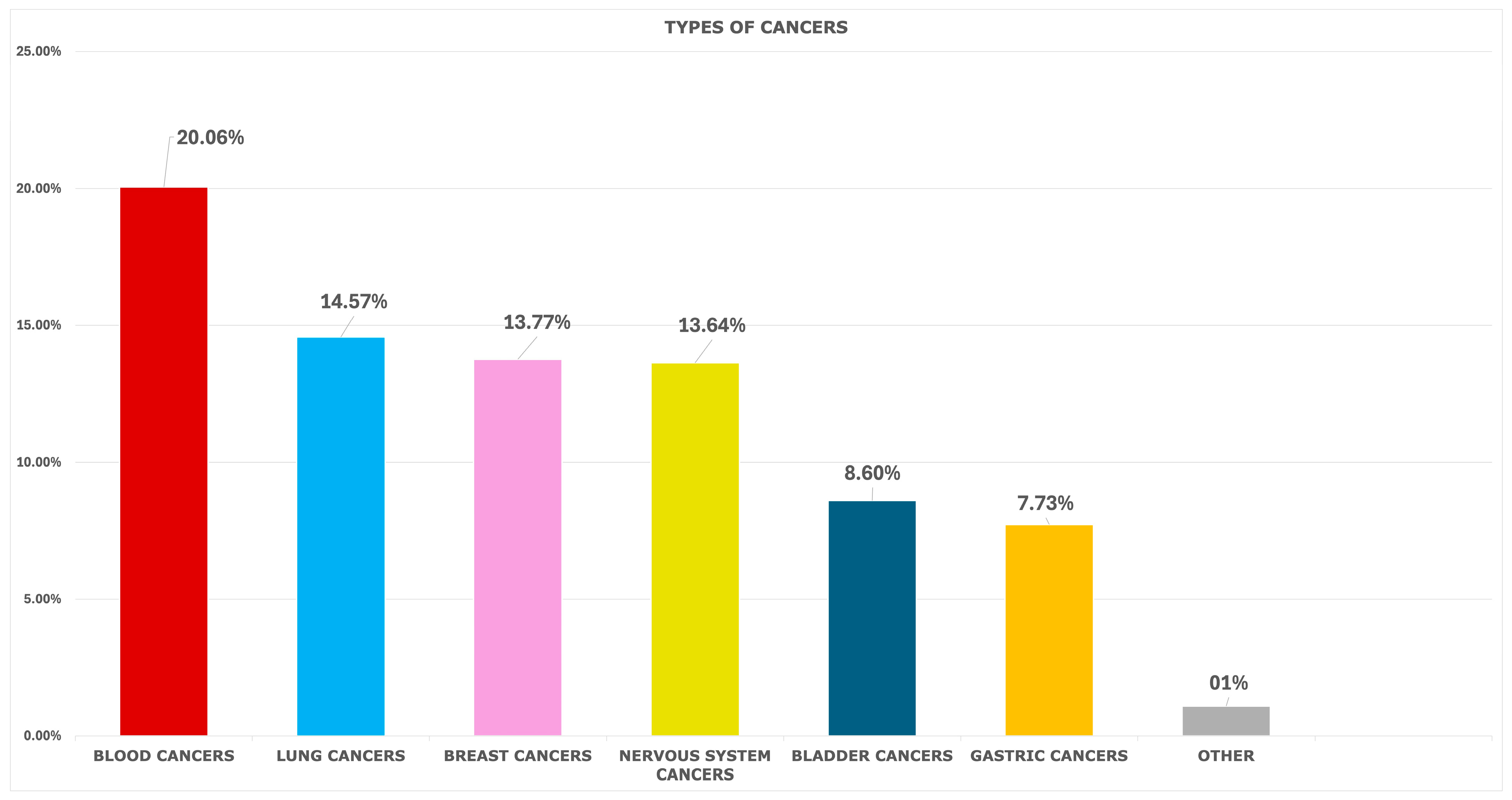
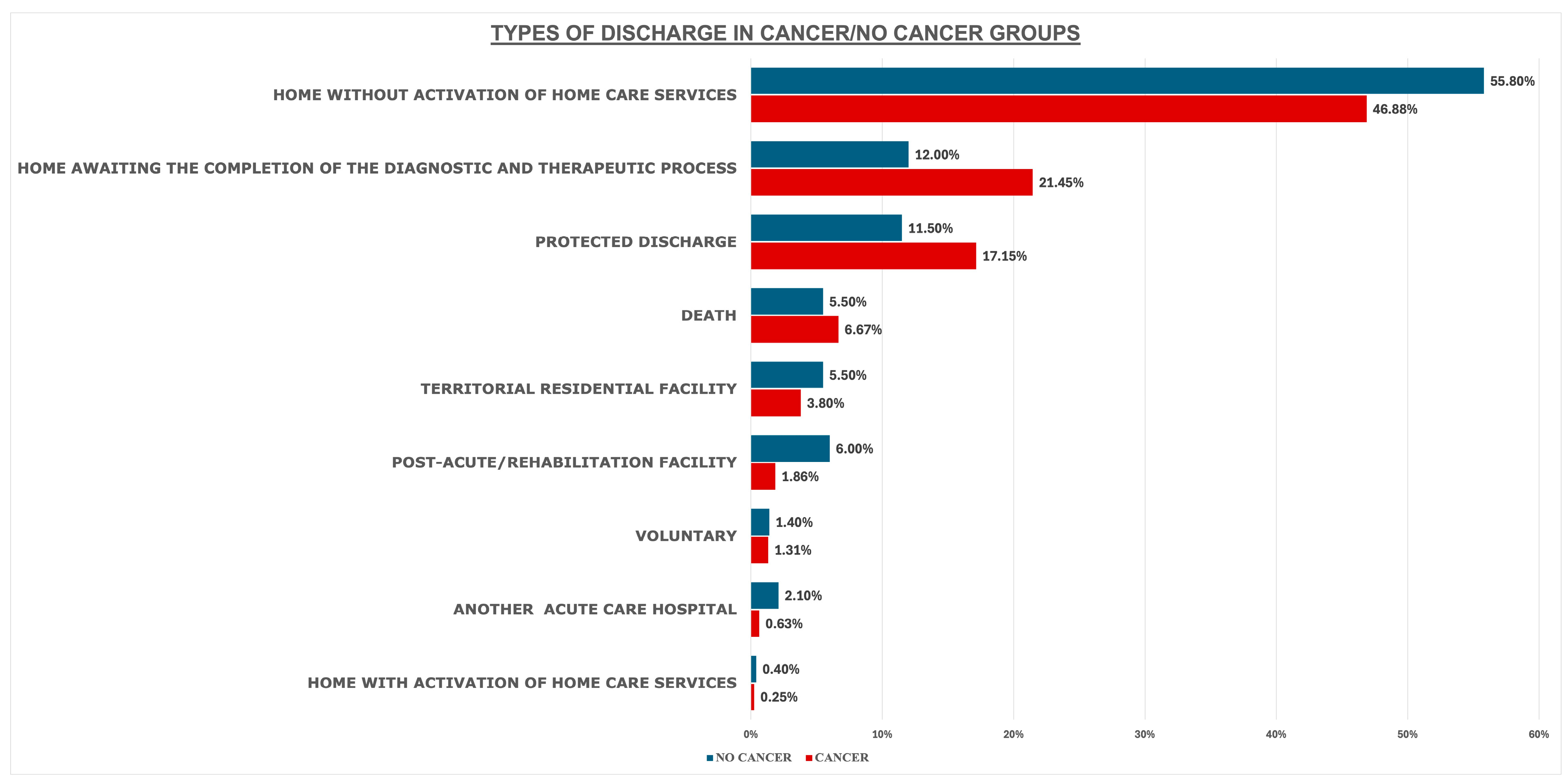
3. Results
4. Discussion
4.1. Summary of Key Findings
4.2. Implications of These Findings on Care Delivery
4.3. The Way Forward
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AOR | Adjusted Odds Ratio |
| CEI | Independent Ethics Committee |
| CI | Confidence Intervals |
| DRGs | Diagnosis-Related Groups |
| GDP | Gross domestic product |
| ICD-9 | International Classification of Diseases, 9th revision |
| LOS | Length of stay |
| NHF | National Health Fund |
| OR | Odds Ratio |
| PTV | Policlinico Tor Vergata |
| SDO | Scheda di Dimissione Ospedaliera |
| SPSS | Statistical Package for the Social Sciences |
References
- World Health Organization. Cancer. Available online: https://www.who.int/news-room/fact-sheets/detail/cancer (accessed on 10 March 2025).
- Numico, G.; Zanelli, C.; Ippoliti, R.; Rossi, M.; Traverso, E.; Antonuzzo, A.; Bellini, R. The hospital care of patients with cancer: A retrospective analysis of the characteristics of their hospital stay in comparison with other medical conditions. Eur. J. Cancer 2020, 139, 99–106. [Google Scholar] [CrossRef] [PubMed]
- Luengo-Fernandez, R.; Leal, J.; Gray, A.; Sullivan, R. Economic burden of cancer across the European Union: A population-based cost analysis. Lancet Oncol. 2013, 14, 1165–1174. [Google Scholar] [CrossRef]
- Sullivan, R.; Peppercorn, J.; Sikora, K.; Zalcberg, J.; Meropol, N.J.; Amir, E.; Khayat, D.; Boyle, P.; Autier, P.; Tannock, I.F.; et al. Delivering affordable cancer care in high-income countries. Lancet Oncol. 2011, 12, 933–980. [Google Scholar] [CrossRef]
- Statista Research Department. Percentage of Elderly Population in Italy from 2009 to 2024. Available online: https://www.statista.com/statistics/785104/elderly-population-in-italy/ (accessed on 10 March 2025).
- Longo, F.; Locatelli, F.; Del Vecchio, M.; Di Giulio, P.; Giordano, S.; Odone, A.; Ranieri, V.M.; Vineis, P. Tackling the crisis of the Italian National Health Fund. Lancet Public Health 2024, 9, e6–e7. [Google Scholar] [CrossRef]
- Eurostat. Hospital Discharges and Length of Stay Statistics. Available online: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Hospital_discharges_and_length_of_stay_statistics&oldid=540628 (accessed on 10 March 2025).
- Stone, K.; Zwiggelaar, R.; Jones, P.; Mac Parthaláin, N. A systematic review of the prediction of hospital length of stay: Towards a unified framework. PLoS Digit. Health 2022, 14, e0000017. [Google Scholar] [CrossRef] [PubMed]
- Trevisan, C.; Noale, M.; Zatti, G.; Vetrano, D.L.; Maggi, S.; Sergi, G. Hospital length of stay and 30-day readmissions in older people: Their association in a 20-year cohort study in Italy. BMC Geriatr. 2023, 23, 154. [Google Scholar] [CrossRef]
- Carestia, M.; Andreoni, M.; Buonomo, E.; Ciccacci, F.; De Angelis, L.; De Carolis, G.; De Filippis, P.; Di Giovanni, D.; Emberti Gialloreti, L.; Fontana, C.; et al. A novel, integrated approach for understanding and investigating Healthcare Associated Infections: A risk factors constellation analysis. PLoS ONE 2023, 18, e0282019. [Google Scholar] [CrossRef]
- Giraldi, G.; Montesano, M.; Napoli, C.; Frati, P.; La Russa, R.; Santurro, A.; Scopetti, M.; Orsi, G.B. Healthcare-Associated Infections Due to Multidrug-Resistant Organisms: A Surveillance Study on Extra Hospital Stay and Direct Costs. Curr. Pharm. Biotechnol. 2019, 20, 643–652. [Google Scholar] [CrossRef] [PubMed]
- Ministero Della Salute. Rapporto Annuale Sull’attività di Ricovero Ospedaliero: Dati SDO 2019. Available online: https://www.salute.gov.it/imgs/C_17_pubblicazioni_3002_allegato.pdf (accessed on 10 March 2025).
- FADOI. Ospedali, Anziani Dimessi 7 Giorni più Tardi. Oltre 2 Giornate di Degenza Improprie. L’indagine FADOI. Available online: https://www.fadoi.org/press-room/ospedali-anziani-dimessi-7-giorni-piu-tardi-oltre-2-giornate-di-degenza-improprie-lindagine-fadoi/?_gl=1*1sb1iyz*_up*MQ..*_ga*MTk0MzYzMDg5Ni4xNzE4NjYwOTg3*_ga_CBP79GC2JJ*MTcxODY2MDk4Ny4xLjEuMTcxODY2MTE1Mi4wLjAuMA (accessed on 10 March 2025).
- Wang, R.C.; Wang, Z. Precision Medicine: Disease Subtyping and Tailored Treatment. Cancers 2023, 15, 3837. [Google Scholar] [CrossRef]
- Greenberg, J.A.; David, M.Z.; Pitrak, D.L.; Hall, J.B.; Kress, J.P. Prior infections are associated with increased mortality from subsequent blood-stream infections among patients with hematological malignancies. Eur. J. Clin. Microbiol. Infect Dis. 2014, 33, 1615–1621. [Google Scholar] [CrossRef]
- Waguia, R.; Wang, T.Y.; Mehta, V.A.; Ramirez, L.; McCray, E.; Pennington, Z.; Price, M.; Dalton, T.; Baëta, C.; Sciubba, D.M.; et al. Risk factors for prolonged length of stay in patients undergoing surgery for intramedullary spinal cord tumors. J. Clin. Neurosci. 2021, 91, 396–401. [Google Scholar] [CrossRef]
- Regione Lazio. DE G16239 del 24.12.2020 Rete e PDTA Mammella. 2020. Available online: https://www.regione.lazio.it/sites/default/files/documentazione/2024/DE%20G16239%20del%2024.12.2020%20Rete%20e%20PDTA%20Mammella.pdf (accessed on 10 March 2025).
- Pîslaru, A.I.; Albișteanu, S.-M.; Ilie, A.C.; Ștefaniu, R.; Mârza, A.; Moscaliuc, Ș.; Nicoară, M.; Turcu, A.-M.; Grigoraș, G.; Alexa, I.D. Lung Cancer: New Directions in Senior Patients Assessment. Geriatrics 2024, 9, 101. [Google Scholar] [CrossRef] [PubMed]
- Higuera, O.; Ghanem, I.; Nasimi, R.; Prieto, I.; Koren, L.; Feliu, J. Management of pancreatic cancer in the elderly. World J. Gastroenterol. 2016, 22, 764–775. [Google Scholar] [CrossRef]
- Cho, E.; Cho, H.A.; Jun, C.H.; Kim, H.J.; Cho, S.B.; Choi, S.K. A Review of Hepatocellular Carcinoma in Elderly Patients Focused on Management and Outcomes. In Vivo 2019, 33, 1411–1420. [Google Scholar] [CrossRef]
- Gentile, L.; Scaramella, M.; Liotta, G.; Magrini, A.; Mulas, M.F.; Quintavalle, G.; Palombi, L. Limitations and consequences of public health models centred on hospitals and lacking connections with territorial and home-based social and health services. Int. J. Emerg. Med. 2024, 17, 66. [Google Scholar] [CrossRef] [PubMed]
- Legramante, J.M.; Morciano, L.; Lucaroni, F.; Gilardi, F.; Caredda, E.; Pesaresi, A.; Coscia, M.; Orlando, S.; Brandi, A.; Giovagnoli, G.; et al. Frequent Use of Emergency Departments by the Elderly Population When Continuing Care Is Not Well Established. PLoS ONE 2016, 11, e0165939. [Google Scholar] [CrossRef] [PubMed]
- Gigantesco, A.; de Girolamo, G.; Santone, G.; Miglio, R.; Picardi, A.; PROGRES-Acute group. Long-stay in short-stay inpatient facilities: Risk factors and barriers to discharge. BMC Public Health 2009, 9, 306. [Google Scholar] [CrossRef]
- Hoogervorst-Schilp, J.; Langelaan, M.; Spreeuwenberg, P.; de Bruijne, M.C.; Wagner, C. Excess length of stay and economic consequences of adverse events in Dutch hospital patients. BMC Health Serv. Res. 2015, 15, 531. [Google Scholar] [CrossRef]
- Glasziou, P.; Straus, S.; Brownlee, S.; Trevena, L.; Dans, L.; Guyatt, G.; Elshaug, A.G.; Janett, R.; Saini, V. Evidence for underuse of effective medical services around the world. Lancet 2017, 390, 169–177. [Google Scholar] [CrossRef]
- Mennini, F.S.; Marcellusi, A.; Sciattella, P.; Scortichini, M.; Ragonese, A.; Cattel, F.; D’Antona, R.; Del Mastro, L.; Gori, S.; Perrone, G.; et al. Burden of Disease of Breast Cancer in Italy: A Real-World Data Analysis. Pharmacoecon Open 2025, 9, 283–290. [Google Scholar] [CrossRef]
- Hanan, T.; Mullen, L.; Laffoy, M.; O’Toole, E.; Richmond, J.; Wynne, M. Delivering care to oncology patients in the community: An innovative integrated approach. Br. J. Community Nurs. 2014, 19, 382–387. [Google Scholar] [CrossRef] [PubMed]
- Liljas, A.E.M.; Brattström, F.; Burström, B.; Schön, P.; Agerholm, J. Impact of Integrated Care on Patient-Related Outcomes Among Older People—A Systematic Review. Int. J. Integr. Care 2019, 19, 6. [Google Scholar] [CrossRef] [PubMed]
- Damery, S.; Flanagan, S.; Combes, G. Does integrated care reduce hospital activity for patients with chronic diseases? An umbrella review of systematic reviews. BMJ Open 2016, 6, e011952. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Regional Office for the Eastern Mediterranean. The Growing Need for Home Health Care for the Elderly. Available online: https://iris.who.int/bitstream/handle/10665/326801/EMROPUB_2015_EN_1901.pdf?sequence=1&isAllowed=y (accessed on 10 March 2025).
- Allan, S.; Roland, D.; Malisauskaite, G.; Jones, K.; Baxter, K.; Gridley, K.; Birks, Y. The influence of home care supply on delayed discharges from hospital in England. BMC Health Serv. Res. 2021, 21, 1297. [Google Scholar] [CrossRef]
- NHS England and NHS Improvement. Building Strong Integrated Care Systems Everywhere ICS Implementation Guidance on Working with People and Communities London, England. 2021. Available online: https://www.england.nhs.uk/wp-content/uploads/2021/06/B0661-ics-working-with-people-and-communities.pdf (accessed on 28 April 2025).
- Wiernik, A.; Rogado, A.; O’Mahony, D.; Abdul Razak, A.R. Elevating Cancer Care Standards Worldwide: An Analysis of Global Initiatives and Progress. JCO Glob. Oncol. 2024, 10, e2400199. [Google Scholar] [CrossRef]
- Mariotti, S.; Minuti, G.; Landi, L.; Bria, E.; Carlucci, G.; Di Salvatore, M.; Giusti, R.; Iurato, A.; Ramella, S.; Ricciotti, M.A.; et al. Simultaneous care provision to patients with small cell lung cancer in Lazio region: Practical recommendations of a multidisciplinary group. Heliyon 2024, 10, e39324. [Google Scholar] [CrossRef]
- OECD/European Commission. EU Country Cancer Profile: Italy 2025, EU Country Cancer Profiles; OECD Publishing: Paris, France, 2025. [Google Scholar] [CrossRef]
- Bidoli, C.; Pegoraro, V.; Dal Mas, F.; Bagnoli, C.; Cordiano, C.; Minto, G.; Zantedeschi, M.; Stocco, P.; Bonin, M.; Pilerci, C.; et al. Virtual hospital: Il futuro del sistema sociosanitario? Un approccio basato su un expert consensus all’interno della Regione Veneto. Politiche Sanit. 2022, 23, 133–148. [Google Scholar] [CrossRef]
- Wong, A.; Cooper, C.; Evans, C.J.; Rawle, M.J.; Walters, K.; Conroy, S.P.; Davies, N. Supporting older people through Hospital at Home care: A systematic review of patient, carer and healthcare professionals’ perspectives. Age Ageing 2025, 54, afaf033. [Google Scholar] [CrossRef]
- Dambha-Miller, H.; Simpson, G.; Hobson, L.; Olaniyan, D.; Hodgson, S.; Roderick, P.; Fraser, S.D.; Little, P.; Everitt, H.; Santer, M. Integrating primary care and social services for older adults with multimorbidity: A qualitative study. Br. J. Gen. Pract. 2021, 71, e753–e761. [Google Scholar] [CrossRef]
- Istituto Superiore di Sanità. EpiCentro—L’epidemiologia per la Sanità Pubblica. Ricoveri Ospedalieri in Italia: Il Rapporto SDO. 2023. Available online: https://www.epicentro.iss.it/sdo/rapporto-sdo-2023 (accessed on 14 April 2025).
| Characteristics at Admissions | Total Ordinary Admissions n = 14,451 | Non-Cancer Patients n = 12,083 | Cancer Patients n =2368 | p-Value |
|---|---|---|---|---|
| Gender, n. (%) | <0.001 * | |||
| Male | 8212 (56.8%) | 6982 (57.8%) | 1230 (51.9%) | |
| Female | 6239 (43.2%) | 5101 (42.2%) | 1138 (48.1%) | |
| Age | ||||
| Age range (min–max) | 18–101 | 18–101 | 18–94 | |
| Mean age (years ± SD) | 64.6 ± 16.6 | 64.5 ± 17.2 | 65.2 ± 13.6 | 0.060 # |
| Age ≤ 65 n. (%) | 6395 (44.3%) | 5369 (44.4%) | 1026 (43.3%) | 0.321 * |
| Age > 65 n. (%) | 8056 (55.7%) | 6714 (55.6%) | 1342 (56.7%) | |
| Between 65 and 75 years | 3474 (24%) | 2771 (22.9%) | 703 (29.7%) | 0.001 * |
| Between 75 and 85 years | 3251 (22.5%) | 2725 (22.6%) | 526 (22.2%) | 0.718 * |
| Over 85 years | 1331 (9.2%) | 1218 (10.8%) | 113 (4.8%) | 0.001 * |
| Type of admission, n. (%) | 0.001 * | |||
| Transfer from Another hospital | 271 (1.9%) | 244 (2.0%) | 26 (1.1%) | |
| Emergency Department (ED) | 8524 (59.0%) | 7621 (63.1%) | 903 (38.1%) | |
| Planned by a specialist | 5656 (39.1%) | 4218 (34.9%) | 1439 (60.8%) | |
| Length of stay LOS, mean days ± SD | ||||
| LOS for total admission | 9.3 ±13.1 | 9.0 ±13.0 | 11.0 ±13.2 | 0.001 # |
| LOS outlier over DRG threshold (n = 725) | 15.6 ± 24.0 | 16.2 ± 25.4 | 12.9 ± 14.7 | 0.153 # |
| LOS outlier > 65 years old (n = 472) | 14.6 ± 21.5 | 15.0 ± 22.4 | 12.4 ± 15.2 | 0.363 # |
| Type of Cancer | n° | Variable | Univariate OR (95% CI) | p Value | Multivariate AOR (95% CI) * | p-Value |
|---|---|---|---|---|---|---|
| Blood cancers | 475 | LOS outlier | 2.658 (1.990–3.551) | <0.001 | 2.031 (1.499–2.753) | <0.001 |
| Age ≥ 65 years | 0.664 (0.553–0.798) | <0.001 | 0.590 (0.489–0.711) | <0.001 | ||
| Infections | 2.435 (1.988–2.983) | <0.001 | 2.368 (1.911–2.933) | <0.001 | ||
| Secondary diagnosis | 1.310 (1.246–1.377) | <0.001 | 1.302 (1.176–1.858) | <0.001 | ||
| Breast cancers | 326 | LOS outlier | 0.290 (0.120–0.704) | 0.006 | NS | |
| Age ≥ 65 years | 0.479 (0.382–0.601) | <0.001 | 0.516 (0.412–0.648) | <0.001 | ||
| Infections | 0.156 (0.080–0.303) | <0.001 | 0.173 (0.089–0.336) | <0.001 | ||
| Secondary diagnosis | 0.667 (0.620–0.717) | <0.001 | 0.716 (0.662–0.773) | <0.001 | ||
| Nervous system cancers | 323 | LOS outlier | 1.537 (1.007–2.346) | 0.046 | 1.940 (1.255–2.998) | 0.003 |
| Age ≥ 65 years | 0.691 (0.554–0.862) | 0.001 | 0.711 (0.570–0.889) | 0.003 | ||
| Infections | 0.547 (0.373–0.803) | 0.002 | 0.517 (0.348–0.768) | 0.001 | ||
| Secondary diagnosis | 0.857 (0.828–0.932) | <0.001 | 0.906 (0.848–0.967) | 0.003 | ||
| Gastric cancers | 183 | LOS outlier | 1.705 (1.000–2.907) | 0.050 | NS | |
| Age ≥ 65 years | 1.813 (1.322–2.487) | <0.001 | 1.673 (1.216–2.301) | 0.002 | ||
| Infections | 2.382 (1.728–3.283) | <0.001 | 2.216 (1.603–3.062) | <0.001 | ||
| Secondary diagnosis | 1.637 (1.486–1.802) | <0.001 | 1.637 (1.486–1.802) | <0.001 | ||
| Hepatopancreatic cancers | 487 | LOS outlier | 0.479 (0.263–0.837) | 0.010 | 0.460 (0.258–0.820) | 0.008 |
| Age ≥ 65 years | 1.228 (1.021–1.477) | 0.029 | 1.241 (1.032–1.494) | 0.022 | ||
| Infections | NS | NS | ||||
| Secondary diagnosis | 1.485 (1.407–1.568) | <0.001 | 0.382 (0.213–0.686) | <0.001 | ||
| Lung cancers | 345 | LOS outlier | NS | NS | ||
| Age ≥ 65 years | 1.814 (1.440–2.286) | <0.001 | 1.862 (1.476–2.348) | <0.001 | ||
| Infections | NS | 0.689 (0.495–0.959) | 0.027 | |||
| Secondary diagnosis | NS | NS | ||||
| Bladder Cancers | 203 | LOS outlier | NS | NS | ||
| Age ≥ 65 years | 2.827 (2.269–3.521) | <0.001 | 2.661 (2.133–3.319) | <0.001 | ||
| Infections | 2.156 (1.749–2.657) | <0.001 | 1.905 (1.543–2.352) | <0.001 | ||
| Secondary diagnosis | 1.129 (1.051–1.213) | 0.001 | NS |
| Type of Discharge | n° of Discharges | LOS in Days Mean ± SD | Univariate OR (95% CI) | p-Value | Multivariate AOR (95% CI) * | p-Value |
|---|---|---|---|---|---|---|
| Home without activation of home care services | 1110 | 12.3 ± 14.4 | 0.698 (0.639–0.762) | <0.001 | NS | |
| Home awaiting the completion of the diagnostic/therapeutic process | 508 | 5 ± 6.7 | 1.997 (1.785–2.235) | <0.001 | 2.150 (1.911–2.418) | <0.001 |
| Protected discharge | 406 | 8.2± 7.9 | 1.601 (1.419–1.806) | <0.001 | 1.805 (1.591–2.047) | <0.001 |
| Death | 158 | 18.5 ± 16.6 | 1.237 (1.034–1.481) | 0.020 | 1.472 (1.225–1.768) | <0.001 |
| Territory residential facility | 90 | 18.8 ± 13.7 | 0.685 (0.547–0.858) | 0.001 | NS | |
| Transfer to post-acute /rehabilitation facility | 44 | 22.6 ± 15.7 | 0.298 (0.219–0.405) | <0.001 | 0.375 (0.275–0.511) | <0.001 |
| Voluntary | 31 | 9.7 ± 11.2 | NS | 0.438 | ||
| Acute care hospital | 15 | 22.3 ± 22.6 | 0.297 (0.176–0.501) | <0.001 | 0.363 (0.215–0.613) | <0.001 |
| Home with activation of home care service | 6 | 34.3 ± 29.1 | NS | 0.724 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gentile, L.; Moramarco, S.; Carnevale, E.; Ciccacci, F.; Ippoliti, L.; Liotta, G.; Orlando, S.; Quintavalle, G.; Schittulli, F.; Palombi, L. Italian Oncology at the Crossroads: Between Hospital Bed Cuts and the Need for a Transition to Integrated Community-Based Simultaneous Care. Cancers 2025, 17, 1821. https://doi.org/10.3390/cancers17111821
Gentile L, Moramarco S, Carnevale E, Ciccacci F, Ippoliti L, Liotta G, Orlando S, Quintavalle G, Schittulli F, Palombi L. Italian Oncology at the Crossroads: Between Hospital Bed Cuts and the Need for a Transition to Integrated Community-Based Simultaneous Care. Cancers. 2025; 17(11):1821. https://doi.org/10.3390/cancers17111821
Chicago/Turabian StyleGentile, Lavinia, Stefania Moramarco, Edoardo Carnevale, Fausto Ciccacci, Lorenzo Ippoliti, Giuseppe Liotta, Stefano Orlando, Giuseppe Quintavalle, Francesco Schittulli, and Leonardo Palombi. 2025. "Italian Oncology at the Crossroads: Between Hospital Bed Cuts and the Need for a Transition to Integrated Community-Based Simultaneous Care" Cancers 17, no. 11: 1821. https://doi.org/10.3390/cancers17111821
APA StyleGentile, L., Moramarco, S., Carnevale, E., Ciccacci, F., Ippoliti, L., Liotta, G., Orlando, S., Quintavalle, G., Schittulli, F., & Palombi, L. (2025). Italian Oncology at the Crossroads: Between Hospital Bed Cuts and the Need for a Transition to Integrated Community-Based Simultaneous Care. Cancers, 17(11), 1821. https://doi.org/10.3390/cancers17111821







