Recent Progress in Treatment for HER2-Positive Advanced Gastric Cancer
Simple Summary
Abstract
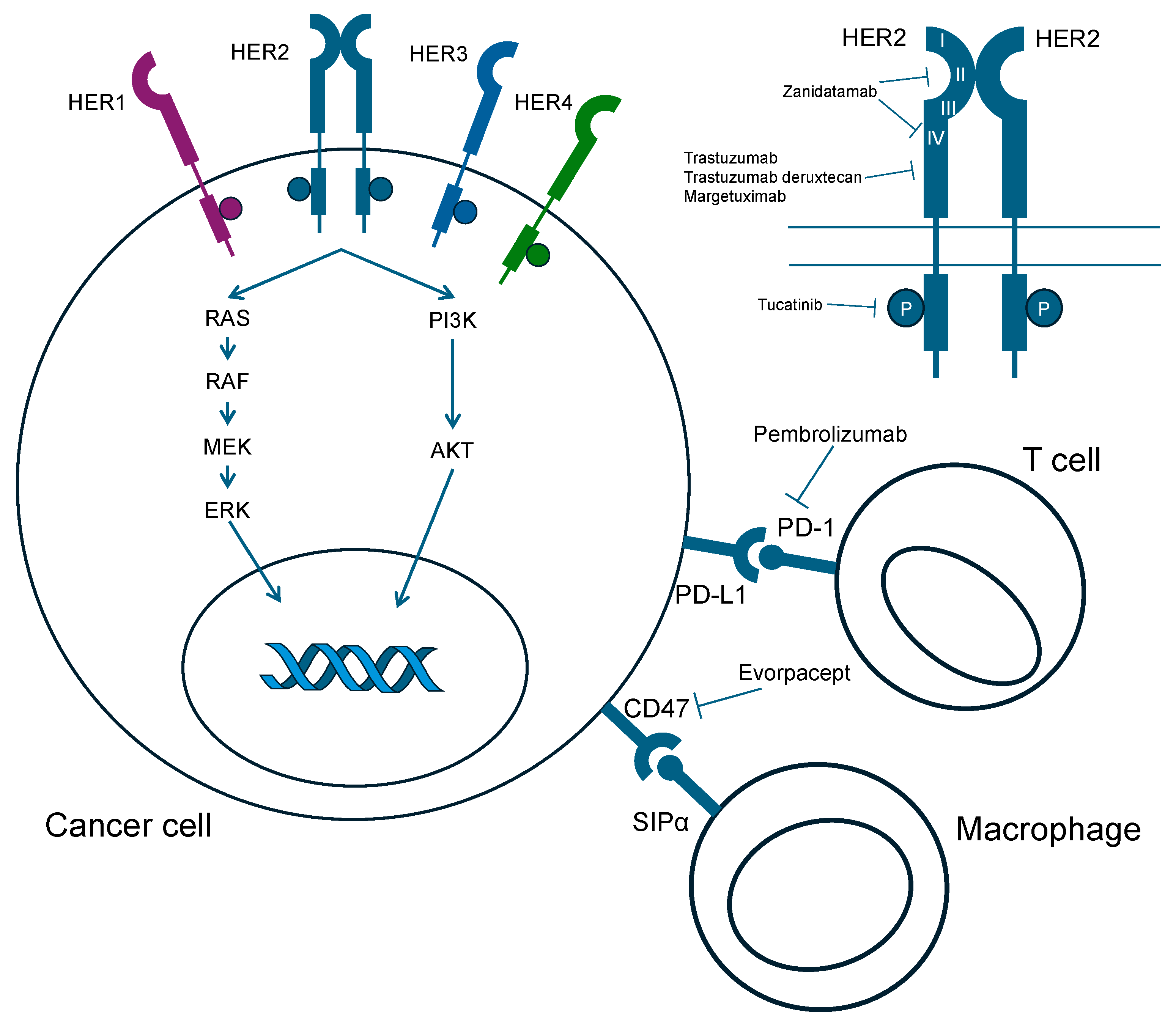
1. Introduction
2. Trastuzumab
2.1. First-Line
2.2. Previously Treated with a Trastuzumab-Containing Regimen after Second-Line Treatment
3. Trastuzumab Deruxtecan
4. Zanidatamab
5. Margetuximab
6. Tucatinib
7. Conclusions and Future Directions
Author Contributions
Funding
Conflicts of Interest
References
- Sakai, K.; Mori, S.; Kawamoto, T.; Taniguchi, S.; Kobori, O.; Morioka, Y.; Kuroki, T.; Kano, K. Expression of Epidermal Growth Factor Receptors on Normal Human Gastric Epithelia and Gastric Carcinomas. J. Natl. Cancer Inst. 1986, 77, 1047–1052. [Google Scholar] [PubMed]
- Yarden, Y.; Sliwkowski, M.X. Untangling the ErbB Signalling Network. Nat. Rev. Mol. Cell Biol. 2001, 2, 127–137. [Google Scholar] [CrossRef] [PubMed]
- Bartley, A.N.; Washington, M.K.; Colasacco, C.; Ventura, C.B.; Ismaila, N.; Benson, A.B.; Carrato, A.; Gulley, M.L.; Jain, D.; Kakar, S.; et al. HER2 Testing and Clinical Decision Making in Gastroesophageal Adenocarcinoma: Guideline from the College of American Pathologists, American Society for Clinical Pathology, and the American Society of Clinical Oncology. J. Clin. Oncol. 2017, 35, 446–464. [Google Scholar] [CrossRef] [PubMed]
- Aizawa, M.; Nagatsuma, A.K.; Kitada, K.; Kuwata, T.; Fujii, S.; Kinoshita, T.; Ochiai, A. Evaluation of HER2-Based Biology in 1,006 Cases of Gastric Cancer in a Japanese Population. Gastric Cancer 2014, 17, 34–42. [Google Scholar] [CrossRef] [PubMed]
- Fuse, N.; Kuboki, Y.; Kuwata, T.; Nishina, T.; Kadowaki, S.; Shinozaki, E.; Machida, N.; Yuki, S.; Ooki, A.; Kajiura, S.; et al. Prognostic Impact of HER2, EGFR, and c-MET Status on Overall Survival of Advanced Gastric Cancer Patients. Gastric Cancer 2016, 19, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Bang, Y.J.; Van Cutsem, E.; Feyereislova, A.; Chung, H.C.; Shen, L.; Sawaki, A.; Lordick, F.; Ohtsu, A.; Omuro, Y.; Satoh, T.; et al. Trastuzumab in Combination with Chemotherapy versus Chemotherapy Alone for Treatment of HER2-Positive Advanced Gastric or Gastro-Oesophageal Junction Cancer (ToGA): A Phase 3, Open-Label, Randomised Controlled Trial. Lancet 2010, 376, 687–697. [Google Scholar] [CrossRef] [PubMed]
- Janjigian, Y.Y.; Kawazoe, A.; Bai, Y.; Xu, J.; Lonardi, S.; Metges, J.P.; Yanez, P.; Wyrwicz, L.S.; Shen, L.; Ostapenko, Y.; et al. Pembrolizumab plus Trastuzumab and Chemotherapy for HER2-Positive Gastric or Gastro-Oesophageal Junction Adenocarcinoma: Interim Analyses from the Phase 3 KEYNOTE-811 Randomised Placebo-Controlled Trial. Lancet 2023, 402, 2197–2208. [Google Scholar] [CrossRef] [PubMed]
- Hecht, J.R.; Bang, Y.J.; Qin, S.K.; Chung, H.C.; Xu, J.M.; Park, J.O.; Jeziorski, K.; Shparyk, Y.; Hoff, P.M.; Sobrero, A.; et al. Lapatinib in Combination with Capecitabine plus Oxaliplatin in Human Epidermal Growth Factor Receptor 2-Positive Advanced or Metastatic Gastric, Esophageal, or Gastroesophageal Adenocarcinoma: TRIO-013/LOGiC—A Randomized Phase III Trial. J. Clin. Oncol. 2016, 34, 443–451. [Google Scholar] [CrossRef] [PubMed]
- Tabernero, J.; Hoff, P.M.; Shen, L.; Ohtsu, A.; Shah, M.A.; Cheng, K.; Song, C.; Wu, H.; Eng-Wong, J.; Kim, K.; et al. Pertuzumab plus Trastuzumab and Chemotherapy for HER2-Positive Metastatic Gastric or Gastro-Oesophageal Junction Cancer (JACOB): Final Analysis of a Double-Blind, Randomised, Placebo-Controlled Phase 3 Study. Lancet Oncol. 2018, 19, 1372–1384. [Google Scholar] [CrossRef] [PubMed]
- Satoh, T.; Doi, T.; Ohtsu, A.; Tsuji, A.; Omuro, Y.; Mukaiyama, A.; Kobayashi, M.; Miwa, H.; Xu, R.H.; Sun, G.P.; et al. Lapatinib plus Paclitaxel versus Paclitaxel Alone in the Second-Line Treatment of HER2-Amplified Advanced Gastric Cancer in Asian Populations: TyTAN—A Randomized, Phase III Study. J. Clin. Oncol. 2014, 32, 2039–2049. [Google Scholar] [CrossRef]
- Thuss-Patience, P.C.; Shah, M.A.; Ohtsu, A.; Van Cutsem, E.; Ajani, J.A.; Castro, H.; Mansoor, W.; Chung, H.C.; Bodoky, G.; Shitara, K.; et al. Trastuzumab Emtansine versus Taxane Use for Previously Treated HER2-Positive Locally Advanced or Metastatic Gastric or Gastro-Oesophageal Junction Adenocarcinoma (GATSBY): An International Randomised, Open-Label, Adaptive, Phase 2/3 Study. Lancet Oncol. 2017, 18, 640–653. [Google Scholar] [CrossRef]
- Makiyama, A.; Sukawa, Y.; Kashiwada, T.; Kawada, J.; Hosokawa, A.; Horie, Y.; Tsuji, A.; Moriwaki, T.; Tanioka, H.; Shinozaki, K.; et al. Randomized, Phase II Study of Trastuzumab beyond Progression in Patients with HER2-Positive Advanced Gastric or Gastroesophageal Junction Cancer: WJOG7112G (T-ACT Study). J. Clin. Oncol. 2020, 38, 1919–1927. [Google Scholar] [CrossRef] [PubMed]
- Shitara, K.; Bang, Y.-J.; Iwasa, S.; Sugimoto, N.; Ryu, M.-H.; Sakai, D.; Chung, H.-C.; Kawakami, H.; Yabusaki, H.; Lee, J.; et al. Trastuzumab Deruxtecan in Previously Treated HER2-Positive Gastric Cancer. N. Engl. J. Med. 2020, 382, 2419–2430. [Google Scholar] [CrossRef]
- Nakamura, Y.; Kawazoe, A.; Lordick, F.; Janjigian, Y.Y.; Shitara, K. Biomarker-Targeted Therapies for Advanced-Stage Gastric and Gastro-Oesophageal Junction Cancers: An Emerging Paradigm. Nat. Rev. Clin. Oncol. 2021, 18, 473–487. [Google Scholar] [CrossRef] [PubMed]
- Seo, S.; Ryu, M.H.; Park, Y.S.; Ahn, J.Y.; Park, Y.; Park, S.R.; Ryoo, B.Y.; Lee, G.H.; Jung, H.Y.; Kang, Y.K. Loss of HER2 Positivity after Anti-HER2 Chemotherapy in HER2-Positive Gastric Cancer Patients: Results of the GASTric Cancer HER2 Reassessment Study 3 (GASTHER3). Gastric Cancer 2019, 22, 527–535. [Google Scholar] [CrossRef] [PubMed]
- Saeki, H.; Oki, E.; Kashiwada, T.; Arigami, T.; Makiyama, A.; Iwatsuki, M.; Narita, Y.; Satake, H.; Matsuda, Y.; Sonoda, H.; et al. Re-Evaluation of HER2 Status in Patients with HER2-Positive Advanced or Recurrent Gastric Cancer Refractory to Trastuzumab (KSCC1604). Eur. J. Cancer 2018, 105, 41–49. [Google Scholar] [CrossRef] [PubMed]
- Satoh, T.; Bang, Y.-J.; Gotovkin, E.A.; Hamamoto, Y.; Kang, Y.-K.; Moiseyenko, V.M.; Ohtsu, A.; Van Cutsem, E.; Al-Sakaff, N.; Urspruch, A.; et al. Quality of Life in the Trastuzumab for Gastric Cancer Trial. Oncologist 2014, 19, 712–719. [Google Scholar] [CrossRef] [PubMed]
- Gelmon, K.A.; Boyle, F.M.; Kaufman, B.; Huntsman, D.G.; Manikhas, A.; Di Leo, A.; Martin, M.; Schwartzberg, L.S.; Lemieux, J.; Aparicio, S.; et al. Lapatinib or Trastuzumab plus Taxane Therapy for Human Epidermal Growth Factor Receptor 2-Positive Advanced Breast Cancer: Final Results of NCIC CTG MA.31. J. Clin. Oncol. 2015, 33, 1574–1583. [Google Scholar] [CrossRef] [PubMed]
- Galluzzi, L.; Buqué, A.; Kepp, O.; Zitvogel, L.; Kroemer, G. Immunological Effects of Conventional Chemotherapy and Targeted Anticancer Agents. Cancer Cell 2015, 28, 690–714. [Google Scholar] [CrossRef] [PubMed]
- Janjigian, Y.Y.; Shitara, K.; Moehler, M.; Garrido, M.; Salman, P.; Shen, L.; Wyrwicz, L.; Yamaguchi, K.; Skoczylas, T.; Campos Bragagnoli, A.; et al. First-Line Nivolumab plus Chemotherapy versus Chemotherapy Alone for Advanced Gastric, Gastro-Oesophageal Junction, and Oesophageal Adenocarcinoma (CheckMate 649): A Randomised, Open-Label, Phase 3 Trial. Lancet 2021, 398, 27–40. [Google Scholar] [CrossRef] [PubMed]
- Kang, Y.K.; Chen, L.T.; Ryu, M.H.; Oh, D.Y.; Oh, S.C.; Chung, H.C.; Lee, K.W.; Omori, T.; Shitara, K.; Sakuramoto, S.; et al. Nivolumab plus Chemotherapy versus Placebo plus Chemotherapy in Patients with HER2-Negative, Untreated, Unresectable Advanced or Recurrent Gastric or Gastro-Oesophageal Junction Cancer (ATTRACTION-4): A Randomised, Multicentre, Double-Blind, Placebo-Contr. Lancet Oncol. 2022, 23, 234–247. [Google Scholar] [CrossRef] [PubMed]
- Gall, V.A.; Philips, A.V.; Qiao, N.; Clise-Dwyer, K.; Perakis, A.A.; Zhang, M.; Clifton, G.T.; Sukhumalchandra, P.; Ma, Q.; Reddy, S.M.; et al. Trastuzumab Increases HER2 Uptake and Cross-Presentation by Dendritic Cells. Cancer Res. 2017, 77, 5374–5383. [Google Scholar] [CrossRef] [PubMed]
- Chaganty, B.K.R.; Qiu, S.; Gest, A.; Lu, Y.; Ivan, C.; Calin, G.A.; Weiner, L.M.; Fan, Z. Trastuzumab Upregulates PD-L1 as a Potential Mechanism of Trastuzumab Resistance through Engagement of Immune Effector Cells and Stimulation of IFNγ Secretion. Cancer Lett. 2018, 430, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Janjigian, Y.Y.; Maron, S.B.; Chatila, W.K.; Millang, B.; Chavan, S.S.; Alterman, C.; Chou, J.F.; Segal, M.F.; Simmons, M.Z.; Momtaz, P.; et al. First-Line Pembrolizumab and Trastuzumab in HER2-Positive Oesophageal, Gastric, or Gastro-Oesophageal Junction Cancer: An Open-Label, Single-Arm, Phase 2 Trial. Lancet Oncol. 2020, 21, 821–831. [Google Scholar] [CrossRef] [PubMed]
- Takahari, D.; Shoji, H.; Minashi, K.; Hara, H.; Chin, K.; Oki, A.; Ogura, M.; Nakayama, I.; Kato, K.; Iwasa, S.; et al. Safety and Early Efficacy Results of a Phase Ib Study of Nivolumab plus Trastuzumab with S-1/Capecitabine plus Oxaliplatin for HER2-Positive Advanced Gastric Cancer (Ni-HIGH Study). J. Clin. Oncol. 2022, 40 (Suppl. S4), 276. [Google Scholar] [CrossRef]
- Lee, C.K.; Rha, S.Y.; Kim, H.S.; Jung, M.; Kang, B.; Che, J.; Kwon, W.S.; Park, S.; Bae, W.K.; Koo, D.H.; et al. A Single Arm Phase Ib/II Trial of First-Line Pembrolizumab, Trastuzumab and Chemotherapy for Advanced HER2-Positive Gastric Cancer. Nat. Commun. 2022, 13, 6002. [Google Scholar] [CrossRef]
- Stein, A.; Paschold, L.; Tintelnot, J.; Goekkurt, E.; Henkes, S.S.; Simnica, D.; Schultheiss, C.; Willscher, E.; Bauer, M.; Wickenhauser, C.; et al. Efficacy of Ipilimumab vs FOLFOX in Combination with Nivolumab and Trastuzumab in Patients with Previously Untreated ERBB2-Positive Esophagogastric Adenocarcinoma: The AIO INTEGA Randomized Clinical Trial. JAMA Oncol. 2022, 8, 1150–1158. [Google Scholar] [CrossRef] [PubMed]
- Shah, M.A.; Kang, Y.K.; Thuss-Patience, P.C.; Ohtsu, A.; Ajani, J.A.; Van Cutsem, E.; Hoersch, S.; Harle-Yge, M.L.; de Haas, S.L. Biomarker Analysis of the GATSBY Study of Trastuzumab Emtansine versus a Taxane in Previously Treated HER2-Positive Advanced Gastric/Gastroesophageal Junction Cancer. Gastric Cancer 2019, 22, 803–816. [Google Scholar] [CrossRef] [PubMed]
- Alameddine, R.S.; Otrock, Z.K.; Awada, A.; Shamseddine, A. Crosstalk between HER2 Signaling and Angiogenesis in Breast Cancer: Molecular Basis, Clinical Applications and Challenges. Curr. Opin. Oncol. 2013, 25, 313–324. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.G.; Jung, M.; Kim, H.S.; Lee, C.; Jeung, H.-C.; Koo, D.-H.; Bae, W.K.; Zang, D.Y.; Kim, B.J.; Kim, H.; et al. Trastuzumab Combined with Ramucirumab and Paclitaxel in Patients with Previously Treated Human Epidermal Growth Factor Receptor 2–Positive Advanced Gastric or Gastroesophageal Junction Cancer. J. Clin. Oncol. 2023, 41, 4394–4405. [Google Scholar] [CrossRef] [PubMed]
- Oldenborg, P.-A. CD47: A Cell Surface Glycoprotein Which Regulates Multiple Functions of Hematopoietic Cells in Health and Disease. ISRN Hematol. 2013, 2013, 614619. [Google Scholar] [CrossRef] [PubMed]
- Lakhani, N.J.; Chow, L.Q.M.; Gainor, J.F.; LoRusso, P.; Lee, K.W.; Chung, H.C.; Lee, J.; Bang, Y.J.; Hodi, F.S.; Kim, W.S.; et al. Evorpacept Alone and in Combination with Pembrolizumab or Trastuzumab in Patients with Advanced Solid Tumours (ASPEN-01): A First-in-Human, Open-Label, Multicentre, Phase 1 Dose-Escalation and Dose-Expansion Study. Lancet Oncol. 2021, 22, 1740–1751. [Google Scholar] [CrossRef] [PubMed]
- Ogitani, Y.; Aida, T.; Hagihara, K.; Yamaguchi, J.; Ishii, C.; Harada, N.; Soma, M.; Okamoto, H.; Oitate, M.; Arakawa, S.; et al. DS-8201a, a Novel HER2-Targeting ADC with a Novel DNA Topoisomerase I Inhibitor, Demonstrates a Promising Antitumor Efficacy with Differentiation from T-DM1. Clin. Cancer Res. 2016, 22, 5097–5108. [Google Scholar] [CrossRef]
- Powell, C.A.; Modi, S.; Iwata, H.; Takahashi, S.; Smit, E.F.; Siena, S.; Chang, D.Y.; Macpherson, E.; Qin, A.; Singh, J.; et al. Pooled Analysis of Drug-Related Interstitial Lung Disease and/or Pneumonitis in Nine Trastuzumab Deruxtecan Monotherapy Studies. ESMO Open 2022, 7, 100554. [Google Scholar] [CrossRef] [PubMed]
- Berger, M.J.; Agarwal, R.; Anand, S.; Bagegni, N.A.; Barbour, S.; Bowman, C.; Lurie, R.H.; Brown, G.E.; Dow-Hillgartner, E. NCCN Guidelines Version 2.2023 Antiemesis Continue. 2023. Available online: https://www.nccn.org/ (accessed on 1 December 2023).
- Yamaguchi, K.; Bang, Y.-J.; Satoru, I.; Sugimoto, N.; Ryu, M.-H.; Sakai, D.; Chung, H.C.; Kawakami, H.; Yabusaki, H.; Lee, J.; et al. Trastuzumab Deruxtecan in Anti-Human Epidermal Growth Factor Receptor 2 Treatment-Naive Patients with Human Epidermal Growth Factor Receptor 2-Low Gastric or Gastroesophageal Junction Adenocarcinoma: Exploratory Cohort Results in a Phase II Trial. J. Clin. Oncol. 2022, 41, 816–825. [Google Scholar] [CrossRef] [PubMed]
- Nakayama, I.; Takahari, D.; Chin, K.; Wakatsuki, T.; Takamatsu, M.; Yamamoto, N.; Ogura, M.; Ooki, A.; Fukuda, K.; Osumi, H.; et al. Incidence, Clinicopathological Features, and Clinical Outcomes of Low HER2 Expressed, Inoperable, Advanced, or Recurrent Gastric/Gastroesophageal Junction Adenocarcinoma. ESMO Open 2023, 8, 101582. [Google Scholar] [CrossRef] [PubMed]
- Van Cutsem, E.; di Bartolomeo, M.; Smyth, E.; Chau, I.; Park, H.; Siena, S.; Lonardi, S.; Wainberg, Z.A.; Ajani, J.; Chao, J.; et al. Trastuzumab Deruxtecan in Patients in the USA and Europe with HER2-Positive Advanced Gastric or Gastroesophageal Junction Cancer with Disease Progression on or after a Trastuzumab-Containing Regimen (DESTINY-Gastric02): Primary and Updated Analyses from a Single-Arm, Phase 2 Study. Lancet Oncol. 2023, 24, 744–756. [Google Scholar]
- Tabernero, J.; Shen, L.; Elimova, E.; Ku, G.; Liu, T.; Shitara, K.; Lin, X.; Boyken, L.; Li, H.; Grim, J.; et al. HERIZON-GEA-01: Zanidatamab + Chemo ± Tislelizumab for 1L Treatment of HER2-Positive Gastroesophageal Adenocarcinoma. Future Oncol. 2022, 18, 3255–3266. [Google Scholar] [CrossRef] [PubMed]
- Meric-Bernstam, F.; Beeram, M.; Hamilton, E.; Oh, D.Y.; Hanna, D.L.; Kang, Y.K.; Elimova, E.; Chaves, J.; Goodwin, R.; Lee, J.; et al. Zanidatamab, a Novel Bispecific Antibody, for the Treatment of Locally Advanced or Metastatic HER2-Expressing or HER2-Amplified Cancers: A Phase 1, Dose-Escalation and Expansion Study. Lancet Oncol. 2022, 23, 1558–1570. [Google Scholar] [CrossRef] [PubMed]
- Elimova, E.; Ajani, A.J.; Burris III, A.H.; Denlinger, S.C.S.; Iqbal, S.; Kang, Y.-K.; Kim, Y.H.H.; Lee, K.-W.; Lin, B.; Mehta, R. Zanidatamab + Chemotherapy as First-Line Treatment for HER2-Expressing Metastatic Gastroesophageal Adenocarcinoma (mGEA). J. Clin. Oncol. 2023, 41, 347. [Google Scholar] [CrossRef]
- Musolino, A.; Gradishar, W.J.; Rugo, H.S.; Nordstrom, J.L.; Rock, E.P.; Arnaldez, F.; Pegram, M.D. Role of Fcγreceptors in HER2-Targeted Breast Cancer Therapy. J. Immunother. Cancer 2022, 10, e003171. [Google Scholar] [CrossRef] [PubMed]
- Nordstrom, J.L.; Gorlatov, S.; Zhang, W.; Yang, Y.; Huang, L.; Burke, S.; Li, H.; Ciccarone, V.; Zhang, T.; Stavenhagen, J.; et al. Anti-Tumor Activity and Toxicokinetics Analysis of MGAH22, an Anti-HER2 Monoclonal Antibody with Enhanced Fcγ Receptor Binding Properties. Breast Cancer Res. 2011, 13, R123. [Google Scholar] [CrossRef] [PubMed]
- Catenacci, D.V.T.; Rosales, M.; Chung, H.C.; Yoon, H.H.; Shen, L.; Moehler, M.; Kang, Y.K. MAHOGANY: Margetuximab Combination in HER2+ Unresectable/Metastatic Gastric/Gastroesophageal Junction Adenocarcinoma. Future Oncol. 2021, 17, 1155–1164. [Google Scholar] [CrossRef] [PubMed]
- Bang, Y.J.; Giaccone, G.; Im, S.A.; Oh, D.Y.; Bauer, T.M.; Nordstrom, J.L.; Li, H.; Chichili, G.R.; Moore, P.A.; Hong, S.; et al. First-in-Human Phase 1 Study of Margetuximab (MGAH22), an Fc-Modified Chimeric Monoclonal Antibody, in Patients with HER2-Positive Advanced Solid Tumors. Ann. Oncol. 2017, 28, 855–861. [Google Scholar] [CrossRef] [PubMed]
- Catenacci, D.V.T.; Kang, Y.K.; Park, H.; Uronis, H.E.; Lee, K.W.; Ng, M.C.H.; Enzinger, P.C.; Park, S.H.; Gold, P.J.; Lacy, J.; et al. Margetuximab plus Pembrolizumab in Patients with Previously Treated, HER2-Positive Gastro-Oesophageal Adenocarcinoma (CP-MGAH22–05): A Single-Arm, Phase 1b–2 Trial. Lancet Oncol. 2020, 21, 1066–1076. [Google Scholar] [CrossRef] [PubMed]
- Waugh, K.A.; Leach, S.M.; Moore, B.L.; Bruno, T.C.; Buhrman, J.D.; Slansky, J.E. Molecular Profile of Tumor-Specific CD8+ T Cell Hypofunction in a Transplantable Murine Cancer Model. J. Immunol. 2016, 197, 1477–1488. [Google Scholar] [CrossRef]
- Woo, S.R.; Turnis, M.E.; Goldberg, M.V.; Bankoti, J.; Selby, M.; Nirschl, C.J.; Bettini, M.L.; Gravano, D.M.; Vogel, P.; Liu, C.L.; et al. Immune Inhibitory Molecules LAG-3 and PD-1 Synergistically Regulate T-Cell Function to Promote Tumoral Immune Escape. Cancer Res. 2012, 72, 917–927. [Google Scholar] [CrossRef] [PubMed]
- Tawbi, H.A.; Schadendorf, D.; Lipson, E.J.; Ascierto, P.A.; Matamala, L.; Castillo Gutiérrez, E.; Rutkowski, P.; Gogas, H.J.; Lao, C.D.; De Menezes, J.J.; et al. Relatlimab and Nivolumab versus Nivolumab in Untreated Advanced Melanoma. N. Engl. J. Med. 2022, 386, 24–34. [Google Scholar] [CrossRef] [PubMed]
- Catenacci, D.V.T.; Kang, Y.K.; Yoon, H.H.; Shim, B.Y.; Kim, S.T.; Oh, D.Y.; Spira, A.I.; Ulahannan, S.V.; Avery, E.J.; Boland, P.M.; et al. Margetuximab with Retifanlimab as First-Line Therapy in HER2+/PD-L1+ Unresectable or Metastatic Gastroesophageal Adenocarcinoma: MAHOGANY Cohort A. ESMO Open 2022, 7, 100563. [Google Scholar] [CrossRef] [PubMed]
- Kulukian, A.; Lee, P.; Taylor, J.; Rosler, R.; De Vries, P.; Watson, D.; Forero-Torres, A.; Peterson, S. Preclinical Activity of HER2-Selective Tyrosine Kinase Inhibitor Tucatinib as a Single Agent or in Combination with Trastuzumab or Docetaxel in Solid Tumor Models. Mol. Cancer Ther. 2020, 19, 976–987. [Google Scholar] [CrossRef]
- Murthy, R.K.; Loi, S.; Okines, A.; Paplomata, E.; Hamilton, E.; Hurvitz, S.A.; Lin, N.U.; Borges, V.; Abramson, V.; Anders, C.; et al. Tucatinib, Trastuzumab, and Capecitabine for HER2-Positive Metastatic Breast Cancer. N. Engl. J. Med. 2020, 382, 597–609. [Google Scholar] [CrossRef] [PubMed]
- Strickler, J.H.; Cercek, A.; Siena, S.; André, T.; Ng, K.; Van Cutsem, E.; Wu, C.; Paulson, A.S.; Hubbard, J.M.; Coveler, A.L.; et al. Tucatinib plus Trastuzumab for Chemotherapy-Refractory, HER2-Positive, RAS Wild-Type Unresectable or Metastatic Colorectal Cancer (MOUNTAINEER): A Multicentre, Open-Label, Phase 2 Study. Lancet Oncol. 2023, 24, 496–508. [Google Scholar] [CrossRef] [PubMed]
| Trial Name | Phase | Regimen | Overall Survival (months) | Progression-Free Survival (months) | Overall Response Rate (%) |
|---|---|---|---|---|---|
| First-line | |||||
| ToGA [6] | 3 | XP/FP + Tmab vs. XP/FP | 13.8 vs. 11.1 (HR: 0.74; 95% CI: 0.60–0.91; p = 0.0046) | 6.7 vs. 5.5 (HR: 0.71; 95% CI: 0.59–0.85; p = 0.0002) | 47 vs. 35 (p = 0.0017) |
| TRIO-013/LoGIC [8] | 3 | XELOX + lapatinib vs. XELOX | 12.2 vs. 11.1 (HR: 0.91; 95% CI: 0.73–1.12; p = 0.3492) | 6.0 vs. 5.4 (HR: 0.82; 95% CI: 0.67–1.00; p = 0.0381) | 53 vs. 39 (p = 0.0031) |
| JACOB [9] | 3 | CT + Tmab + pertuzumab vs. CT + Tmab | 17.5 vs. 14.2 (HR: 0.84; 95% CI: 0.71–1.00; p = 0.057) | 8.5 vs. 7.0 (HR: 0.73; 95% CI: 0.62–0.86; p = 0.0001) | 56.7 vs. 48.3 (p = 0.026) |
| KN–811 [7] | 3 | CT + Tmab vs. CT + Tmab + pembrolizumab | 10.0 vs. 8.1; HR: 0.72; 95% CI: 0.60–0.87; p = 0.0002 | 20.0 vs. 16.9; HR: 0.87; 95% CI: 0.72–1.06; p = 0.084 | 72.6 vs. 59.8 |
| Previously treated with a Tmab-containing regimen | |||||
| TyTAN [10] | 3 | PTX + lapatinib vs. PTX | 11.0 vs. 8.9 (HR: 0.84; 95% CI: 0.64–1.11; p = 0.1044) | 5.4 vs. 4.4 (HR: 0.85; 95% CI: 0.63–1.13; p = 0.2441) | 27 vs. 9 (p < 0.001) |
| GATSBY [11] | 2/3 | PTX vs. T-DM1 | 8.6 vs. 7.9 (HR: 1.15; 95% CI: 0.87–1.51; p = 0.86) | 2.9 vs. 2.7 (HR: 0.84; 95% CI: 0.64–1.11; p = 0.1044) | 19.6 vs. 20.6 (p = 0.8406) |
| T-ACT [12] | rP2 | PTX vs. PTX + Tmab | 10.0 vs. 10.2 (HR: 1.23; 95% CI: 0.76–1.99; p = 0.20) | 3.2 vs. 3.7 (HR: 1.15; 95% CI: 0.87–1.51; p = 0.86) | 32 vs. 33 (p = 1.00) |
| DESTINY-Gastric01 [13] | rP2 | T-DXd vs. Physician’s choice (PTX or IRI) | 12.5 vs. 8.4 (HR: 0.59; 95% CI: 0.39–0.88; p = 0.01) | 5.6 vs. 3.5 (HR: 0.47; 95% CI: 0.31–0.71) | 51 vs. 14 (p < 0.001) |
| Trial Number | Phase | Experimental Arm | Control Arm | Primary Endpoint | Estimated Study Completion Date |
|---|---|---|---|---|---|
| First-line | |||||
| NCT05152147 | 3 | XELOX/FP + Zanidatamab, XELOX/FP + Zanidatamab + Tislelizumab | XELOX/FP + Tmab | PFS, OS | 1 July 2025 |
| NCT03929666 | 2 | Zanidatamab + FP/mFOLFOX6/XELOX | None | Part 1 Incidence of DLTs, AEs, lab abnormalities Part 2 ORR | 30 October 2026 |
| NCT05382364 | 1b/2 | Tucatinib + Tmab + FOLFOX/XELOX, Tucatinib + Tmab + Pembrolizumab + FOLFOX/XELOX, Tucatinib + Tmab + Pembrolizumab, Tucatinib + Tmab + FOLFOX/XELOX | None | Incidence of renal DLTs, AEs, laboratory abnormalities, DLTs, and dose alterations | 29 December 2025 |
| NCT04082364 | 2/3 | Margetuximab + Retifanlimab, Margetuximab + Retifanlimab + XELOX/mFOLFOX6, Margetuximab + Tebotelimab + XELOX/mFOLFOX6, Margetuximab + XELOX/mFOLFOX6 | Tmab + XELOX/mFOLFOX6 | AEs, ORR for non-MSI-H | March 2024 |
| NCT04379596 | 1/2 | Part 1 T-DXd + 5-FU, T-DXd + Cape, T-DXd + Durvalumab, T-DXd + XELOX, T-DXd + 5-FU + Durvalumab, T-DXd + Cape + Durvalumab. Part 2 T-DXd, T-DXd + 5-FU/Cape + Pembrolizumab, T-DXd + Pembrolizumab, T-DXd + 5-FU/Cape + Pembrolizumab. Part 3 T-DXd + 5-FU/Cape + MEDI5752 | Part 1 None Part 2 Tmab + 5-FU/Cape + Cisplatin/Oxaliplatin. Part 3 None | Part 1 Occurrence of AEs and SAEs, changes from baseline in laboratory parameters, vital signs, and ECG Parts 2 and 3 ORR | 30 July 2026 |
| After Second–line | |||||
| NCT04704934 | 3 | T-DXd | RAM + PTX | OS | 15 November 2024 |
| NCT05002127 | 2/3 | Evorpacept + Tmab + RAM + PTX | RAM + PTX | Phase 2 part ORR Phase 3 part OS | August 2028 |
| NCT04499924 | 2/3 | Tucatinib + Tmab + RAM + PTX, Tucatinib + RAM + PTX | RAM + PTX | Phase 2 part Incidence of DLTs, AEs, laboratory abnormalities, dose modifications. Phase 3 part OS, PFS | 31 March 2027 |
| NCT05190445 | 2 | Cinrebafusp alfa + RAM + PTX, Cinrebafusp + Tucatinib | None | ORR | 1 February 2023 |
| NCT04989816 | 2 | T-DXd | None | ORR | 28 February 2024 |
| NCT05270889 | 2 | Zanidatamab + Tislelizumab | None | ORR | June 2024 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kawakami, T.; Yamazaki, K. Recent Progress in Treatment for HER2-Positive Advanced Gastric Cancer. Cancers 2024, 16, 1747. https://doi.org/10.3390/cancers16091747
Kawakami T, Yamazaki K. Recent Progress in Treatment for HER2-Positive Advanced Gastric Cancer. Cancers. 2024; 16(9):1747. https://doi.org/10.3390/cancers16091747
Chicago/Turabian StyleKawakami, Takeshi, and Kentaro Yamazaki. 2024. "Recent Progress in Treatment for HER2-Positive Advanced Gastric Cancer" Cancers 16, no. 9: 1747. https://doi.org/10.3390/cancers16091747
APA StyleKawakami, T., & Yamazaki, K. (2024). Recent Progress in Treatment for HER2-Positive Advanced Gastric Cancer. Cancers, 16(9), 1747. https://doi.org/10.3390/cancers16091747





