A Combined Cyto- and Histopathological Diagnostic Approach Reduces Time to Diagnosis and Time to Therapy in First Manifestation of Metastatic Spinal Disease: A Cohort Study
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Patient Characteristics
3.2. Feasibility of Simultaneous Cytology from the Spinal Lesion and Bone Marrow
3.3. Diagnostic Accuracy of Cytology and Concordance with Histology
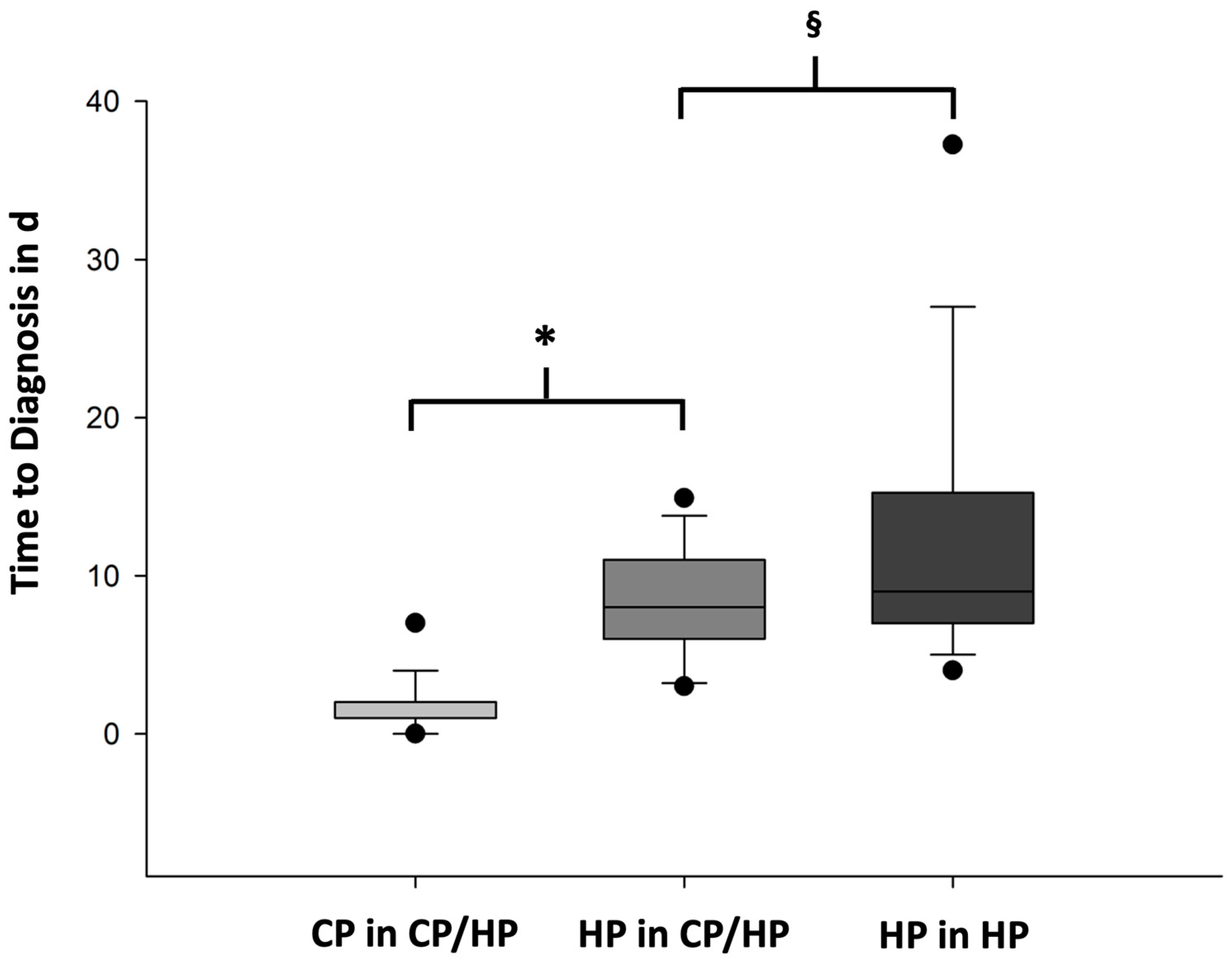
3.4. Time to Diagnosis (TTD) for CP/HP and HP
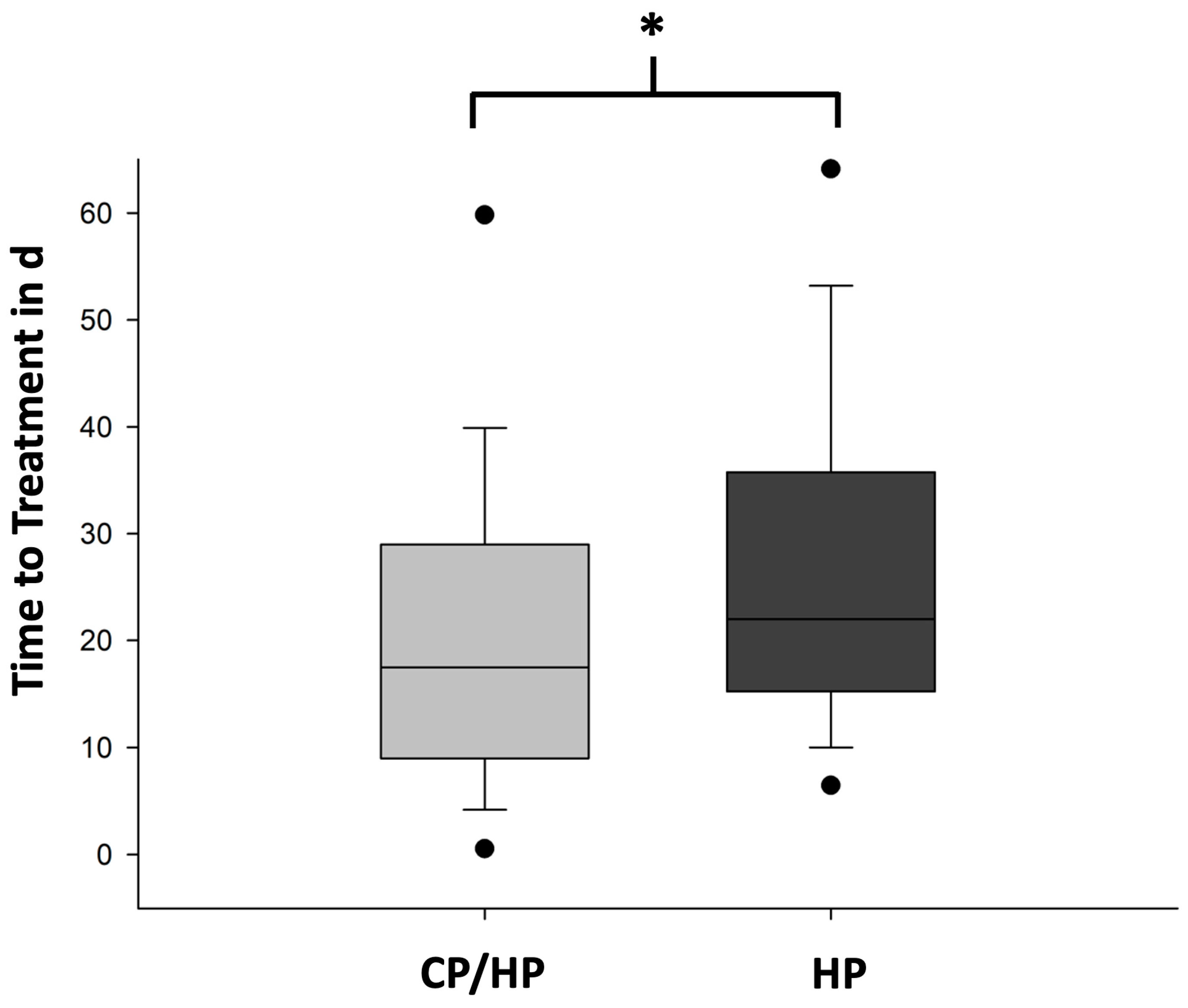
3.5. TTT in the CP/HP Group Compared to the HP Group
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Coleman, R.E. Clinical features of metastatic bone disease and risk of skeletal morbidity. Clin. Cancer Res. 2006, 12, 6243s–6249s. [Google Scholar] [CrossRef] [PubMed]
- Destombe, C.; Botton, E.; Le Gal, G.; Roudaut, A.; Jousse-Joulin, S.; Devauchelle-Pensec, V.; Saraux, A. Investigations for bone metastasis from an unknown primary. Jt. Bone Spine 2007, 74, 85–89. [Google Scholar] [CrossRef] [PubMed]
- Baron, M.G.; de la Gandara, I.; Espinosa, E.; de Paredes, M.L.; Zamora, P.; Mondejar, J.L. Bone metastases as the first manifestation of a tumour. Int. Orthop. 1991, 15, 373–376. [Google Scholar] [CrossRef] [PubMed]
- Kyle, R.A.; Gertz, M.A.; Witzig, T.E.; Lust, J.A.; Lacy, M.Q.; Dispenzieri, A.; Fonseca, R.; Rajkumar, S.V.; Offord, J.R.; Larson, D.R.; et al. Review of 1027 patients with newly diagnosed multiple myeloma. Mayo Clin. Proc. 2003, 78, 21–33. [Google Scholar] [CrossRef] [PubMed]
- Lote, K.; Walloe, A.; Bjersand, A. Bone metastasis. Prognosis, diagnosis and treatment. Acta Radiol. Oncol. 1986, 25, 227–232. [Google Scholar] [CrossRef] [PubMed]
- Park, S.B.; Park, J.M.; Moon, S.H.; Cho, Y.S.; Sun, J.M.; Kim, B.T.; Lee, K.H. Role of 18F-FDG PET/CT in patients without known primary malignancy with skeletal lesions suspicious for cancer metastasis. PLoS ONE 2018, 13, e0196808. [Google Scholar] [CrossRef] [PubMed]
- Vandecandelaere, M.; Flipo, R.M.; Cortet, B.; Catanzariti, L.; Duquesnoy, B.; Delcambre, B. Bone metastases revealing primary tumors. Comparison of two series separated by 30 years. Jt. Bone Spine 2004, 71, 224–229. [Google Scholar] [CrossRef] [PubMed]
- Cronin, K.A.; Scott, S.; Firth, A.U.; Sung, H.; Henley, S.J.; Sherman, R.L.; Siegel, R.L.; Anderson, R.N.; Kohler, B.A.; Benard, V.B.; et al. Annual report to the nation on the status of cancer, part 1: National cancer statistics. Cancer 2022, 128, 4251–4284. [Google Scholar] [CrossRef]
- Guo, H.; Li, H.; Zhu, L.; Feng, J.; Huang, X.; Baak, J.P.A. “How Long Have I Got?” in Stage IV NSCLC Patients with at Least 3 Months Up to 10 Years Survival, Accuracy of Long-, Intermediate-, and Short-Term Survival Prediction Is Not Good Enough to Answer This Question. Front. Oncol. 2021, 11, 761042. [Google Scholar] [CrossRef]
- Hanna, T.P.; King, W.D.; Thibodeau, S.; Jalink, M.; Paulin, G.A.; Harvey-Jones, E.; O’Sullivan, D.E.; Booth, C.M.; Sullivan, R.; Aggarwal, A. Mortality due to cancer treatment delay: Systematic review and meta-analysis. BMJ 2020, 371, m4087. [Google Scholar] [CrossRef]
- Bochtler, T.; Loffler, H.; Kramer, A. Diagnosis and management of metastatic neoplasms with unknown primary. Semin. Diagn. Pathol. 2018, 35, 199–206. [Google Scholar] [CrossRef] [PubMed]
- Caldarella, A.; Crocetti, E.; Taddei, G.L.; Paci, E. Cytopathological diagnosis in a cancer registry: A useful diagnostic tool? Cancer 2007, 111, 99–105. [Google Scholar] [CrossRef]
- Varadhachary, G.R.; Abbruzzese, J.L.; Lenzi, R. Diagnostic strategies for unknown primary cancer. Cancer 2004, 100, 1776–1785. [Google Scholar] [CrossRef] [PubMed]
- Sailer, V.; Schiffman, M.H.; Kossai, M.; Cyrta, J.; Beg, S.; Sullivan, B.; Pua, B.B.; Lee, K.S.; Talenfeld, A.D.; Nanus, D.M.; et al. Bone biopsy protocol for advanced prostate cancer in the era of precision medicine. Cancer 2018, 124, 1008–1015. [Google Scholar] [CrossRef] [PubMed]
- Abdo, M.; Belloum, Y.; Heigener, D.; Welker, L.; von Weihe, S.; Schmidt, M.; Heuer-Olewinski, N.; Watermann, I.; Szewczyk, M.; Kropidlowski, J.; et al. Comparative evaluation of PD-L1 expression in cytology imprints, circulating tumour cells and tumour tissue in non-small cell lung cancer patients. Mol. Oncol. 2023, 17, 737–746. [Google Scholar] [CrossRef] [PubMed]
- Jain, D.; Nambirajan, A.; Borczuk, A.; Chen, G.; Minami, Y.; Moreira, A.L.; Motoi, N.; Papotti, M.; Rekhtman, N.; Russell, P.A.; et al. Immunocytochemistry for predictive biomarker testing in lung cancer cytology. Cancer Cytopathol. 2019, 127, 325–339. [Google Scholar] [CrossRef]
- Pisapia, P.; Pepe, F.; Sgariglia, R.; Nacchio, M.; Russo, G.; Conticelli, F.; Girolami, I.; Eccher, A.; Bellevicine, C.; Vigliar, E.; et al. Next generation sequencing in cytology. Cytopathology 2021, 32, 588–595. [Google Scholar] [CrossRef]
- Koepke, L.G.; Heuer, A.; Stangenberg, M.; Dreimann, M.; Welker, L.; Bokemeyer, C.; Strahl, A.; Asemissen, A.M.; Viezens, L. Surgical Site Cytology to Diagnose Spinal Lesions. Diagnostics 2022, 12, 310. [Google Scholar] [CrossRef]
- Caers, J.; Garderet, L.; Kortum, K.M.; O’Dwyer, M.E.; van de Donk, N.; Binder, M.; Dold, S.M.; Gay, F.; Corre, J.; Beguin, Y.; et al. European Myeloma Network recommendations on tools for the diagnosis and monitoring of multiple myeloma: What to use and when. Haematologica 2018, 103, 1772–1784. [Google Scholar] [CrossRef]
- Crothers, B.A. Cytologic-histologic correlation: Where are we now, and where are we going? Cancer Cytopathol. 2018, 126, 301–308. [Google Scholar] [CrossRef]
- Asaturova, A.; Dobrovolskaya, D.; Magnaeva, A.; Tregubova, A.; Bayramova, G.; Sukhikh, G. Cervical Cytology-Histology Correlation Based on the American Society of Cytopathology Guideline (2017) at the Russian National Medical Research Center for Obstetrics, Gynecology, and Perinatology. Diagnostics 2022, 12, 210. [Google Scholar] [CrossRef] [PubMed]
- El Chamieh, C.; Vielh, P.; Chevret, S. Statistical methods for evaluating the fine needle aspiration cytology procedure in breast cancer diagnosis. BMC Med. Res. Methodol. 2022, 22, 40. [Google Scholar] [CrossRef] [PubMed]
- Biancosino, C.; Kruger, M.; Vollmer, E.; Welker, L. Intraoperative fine needle aspirations—Diagnosis and typing of lung cancer in small biopsies: Challenges and limitations. Diagn. Pathol. 2016, 11, 59. [Google Scholar] [CrossRef] [PubMed]
- Botticella, M.A.; De Summa, S.; Cisternino, L.; Tommasi, S.; Pastena, M.I.; Schirosi, L.; Mangia, A.; Mele, F.; Lozupone, A.; Scattone, A.; et al. The role of rapid on site evaluation on touch imprint cytology and brushing during conventional bronchoscopy. Diagn. Cytopathol. 2021, 49, 832–837. [Google Scholar] [CrossRef] [PubMed]
- Al-Hajeili, M.; Alqassas, M.; Alomran, A.; Batarfi, B.; Basunaid, B.; Alshail, R.; Alaydarous, S.; Bokhary, R.; Mosli, M. The Diagnostic Accuracy of Cytology for the Diagnosis of Hepatobiliary and Pancreatic Cancers. Acta Cytol. 2018, 62, 311–316. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.D.; Wani, F.A.; Bhardwaj, S. Diagnostic accuracy of FNAC and cyto-histopathological correlation in testicular and paratesticular mass lesions. Cytopathology 2017, 28, 542–548. [Google Scholar] [CrossRef] [PubMed]
- Mayooran, N.; Waters, P.S.; Kaim Khani, T.Y.; Kerin, M.J.; Quill, D. FNAC and frozen section correlations with definitive histology in thyroid diseases. Eur. Arch. Otorhinolaryngol. 2016, 273, 2181–2184. [Google Scholar] [CrossRef] [PubMed]
- Kuempers, C.; van der Linde, L.I.S.; Reischl, M.; Vogel, W.; Stellmacher, F.; Reck, M.; Heigener, D.; Rabe, K.F.; Kirfel, J.; Perner, S.; et al. Comparison of PD-L1 expression between paired cytologic and histologic specimens from non-small cell lung cancer patients. Virchows Arch. 2020, 476, 261–271. [Google Scholar] [CrossRef] [PubMed]
- Roy-Chowdhuri, S.; Stewart, J. Preanalytic Variables in Cytology: Lessons Learned From Next-Generation Sequencing-The MD Anderson Experience. Arch. Pathol. Lab. Med. 2016, 140, 1191–1199. [Google Scholar] [CrossRef]
- Dimopoulos, M.A.; Moreau, P.; Terpos, E.; Mateos, M.V.; Zweegman, S.; Cook, G.; Delforge, M.; Hajek, R.; Schjesvold, F.; Cavo, M.; et al. Multiple myeloma: EHA-ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up(dagger). Ann. Oncol. 2021, 32, 309–322. [Google Scholar] [CrossRef]
| CP/HP Group | HP Group | |
|---|---|---|
| Number of patients | 61 | 139 |
| Sex | 37.7% female | 36.9% female |
| Age | 65 (20–86) years | 67 (21–85) years |
| Anatomic region | ||
| • Cervical spine | 3 | 35 |
| • Thoracic spine | 31 | 74 |
| • Lumbar spine | 23 | 44 |
| • Pelvis | 7 | 8 |
| Diagnosis | N (CP/HP Group) | N (HP Group) |
|---|---|---|
| Multiple myeloma | 14 | 28 |
| Breast cancer | 9 | 11 |
| Bronchopulmonal adenocarcinoma | 8 | 21 |
| Prostate cancer | 5 | 10 |
| Undifferentiated carcinoma | 3 | 10 |
| Small cellular lung cancer | 3 | 5 |
| Hepatocellular carcinoma | 3 | 0 |
| Renal cell carcinoma | 2 | 7 |
| Malignant melanoma | 2 | 1 |
| Squamous cell carcinoma of the lung | 1 | 7 |
| Cholangiocellular carcinoma | 1 | 3 |
| Malignant fibrous tumor | 1 | 1 |
| Epithelioid angiosarcoma | 1 | 1 |
| B-cell lymphoma | 1 | 8 |
| Dedifferentiated liposarcoma | 1 | 0 |
| Undifferentiated squamous cell carcinoma | 0 | 9 |
| Gastrointestinal adenocarcinoma | 0 | 8 |
| Thyroid cancer | 0 | 1 |
| Urothelial carcinoma | 0 | 4 |
| Ewing sarcoma | 0 | 4 |
| Non-malignant | 6 | 0 |
| Histopathology | ||||||
|---|---|---|---|---|---|---|
| Myeloma | Solid | Lymphoma | Non-Malignant | Total | ||
| Myeloma | 9 | 0 | 0 | 1 | 10 | |
| Cytopathology | Solid | 0 | 39 | 0 | 0 | 39 |
| Lymphoma | 0 | 0 | 1 | 0 | 1 | |
| Non-malignant | 1 | 1 | 0 | 5 | 7 | |
| Total | 10 | 40 | 1 | 6 | 57 |
| TTT in d | T before HP in d | Diagnose | Type of T | Relevant Biomarkers |
|---|---|---|---|---|
| 0 | 6 | Prostate cancer | Anti-androgen therapy | Total PSA: 4257.22 µg/L Free PSA: 14.07 µg/L |
| 1 | 12 | Prostate cancer | Anti-androgen therapy | Total PSA: 2625.07 µg/L Free PSA: 320.91 µg/L |
| 7 | 1 | Prostate cancer | Anti-androgen therapy | Total PSA: 248.86 µg/L Free PSA: 21.23 µg/L |
| 6 | 7 | Prostate cancer | Anti-androgen therapy | Total PSA: 1345.52 µg/L Free PSA: n.a. |
| 0 | 9 | Multiple myeloma | Chemo-, biological, steroid therapy | M gradient: 39.4 Clonal protein: 43.7 g/L IgG: 57.55 g/L IgA: <0.15 g/L IgM: 0.13 g/L Free light chain kappa: 4.92 g/L Free light chain lambda: 0.12 g/L Free light chain quotient: 41.00 g/L |
| 4 | 7 | Multiple myeloma | Steroid therapy | M gradient: 37.3 Clonal protein: 27.2 g/L IgG: 32.40 g/L IgA: 0.41 g/L IgM: 0.22 g/L Free light chain kappa: 0.017 g/L Free light chain lambda: 0.66 g/L Free light chain quotient: 0.03 g/L |
| 4 | 3 | Multiple myeloma | Anti-CD38 antibody | M gradient: 53.4 Clonal protein: 53.9 g/L IgG: 58.68 g/L IgA: 0.68 g/L IgM: 0.12 g/L Free light chain kappa: 0.5 g/L Free light chain lambda: 15.80 g/L Free light chain quotient: 0.03 g/L |
| 7 | 2 | Multiple myeloma | Anti-CD38 antibody | M gradient: n.a. Clonal protein: n.a. IgG: n.a. IgA: n.a. IgM: n.a. Free light chain kappa: 0.51 g/L Free light chain lambda: 1.39 g/L Free light chain quotient: 0.36 g/L |
| 11 | 3 | Small cellular lung cancer | Radiation, chemotherapy, checkpoint inhibitor | Total PSA: 0.88 µg/L Free PSA: 0.21 µg/L NSE: 97.1 µg/L |
| 14 | 1 | Small cellular lung cancer | Radiation, chemotherapy, checkpoint inhibitor | NSE: 14.5 µg/L |
| 11 | 4 | Melanoma | Dual checkpointinhibitors | n.a. |
| 9 | 3 | Breast cancer | Anti-hormone therapy | CA15-3: 458.9 kU/L CEA: 86.0 kU/L |
| 9 | 1 | Biliopancreatic carcinoma | Radiation | CA19-9: 48.1 kU/L CA125: 0.8 kU/L |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leonhardt, L.-G.; Heuer, A.; Stangenberg, M.; Schroeder, M.; Schmidt, G.; Welker, L.; von Amsberg, G.; Strahl, A.; Krüger, L.; Dreimann, M.; et al. A Combined Cyto- and Histopathological Diagnostic Approach Reduces Time to Diagnosis and Time to Therapy in First Manifestation of Metastatic Spinal Disease: A Cohort Study. Cancers 2024, 16, 1659. https://doi.org/10.3390/cancers16091659
Leonhardt L-G, Heuer A, Stangenberg M, Schroeder M, Schmidt G, Welker L, von Amsberg G, Strahl A, Krüger L, Dreimann M, et al. A Combined Cyto- and Histopathological Diagnostic Approach Reduces Time to Diagnosis and Time to Therapy in First Manifestation of Metastatic Spinal Disease: A Cohort Study. Cancers. 2024; 16(9):1659. https://doi.org/10.3390/cancers16091659
Chicago/Turabian StyleLeonhardt, Leon-Gordian, Annika Heuer, Martin Stangenberg, Malte Schroeder, Gabriel Schmidt, Lutz Welker, Gunhild von Amsberg, André Strahl, Lara Krüger, Marc Dreimann, and et al. 2024. "A Combined Cyto- and Histopathological Diagnostic Approach Reduces Time to Diagnosis and Time to Therapy in First Manifestation of Metastatic Spinal Disease: A Cohort Study" Cancers 16, no. 9: 1659. https://doi.org/10.3390/cancers16091659
APA StyleLeonhardt, L.-G., Heuer, A., Stangenberg, M., Schroeder, M., Schmidt, G., Welker, L., von Amsberg, G., Strahl, A., Krüger, L., Dreimann, M., Bokemeyer, C., Viezens, L., & Asemissen, A. M. (2024). A Combined Cyto- and Histopathological Diagnostic Approach Reduces Time to Diagnosis and Time to Therapy in First Manifestation of Metastatic Spinal Disease: A Cohort Study. Cancers, 16(9), 1659. https://doi.org/10.3390/cancers16091659






