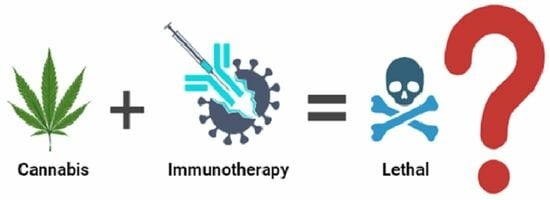
Immunotherapy and Cannabis: A Harmful Drug Interaction or Reefer Madness?
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Taha et al. The Oncologist 2019;24:549–554 [8]
3.2. Bar-Sela et al. Cancers 2020:12:2447 [9]
3.3. Correction to Bar-Sela et al. Cancers 2020:12:2447 [9]
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- National Academies of Sciences; Medicine Division; Board on Population Health; Public Health Practice; Committee on the Health Effects of Marijuana; An Evidence Review; Research Agenda. The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research; National Academies Press (US): Washington, DC, USA, 2017.
- The Editors of Mayo Clinic. Mayo Clinic Medical Marijuana; Mayo Clinic: Rochester, MI, USA, 2023. [Google Scholar]
- Haynes, B.F.; Soderberg, K.A.; Fauci, A.S. Mechanisms of Regulation and Dysregulation of the Immune System; McGraw-Hill Education: New York, NY, USA, 2022; Volume 350. [Google Scholar]
- Liu, C.; Yang, M.; Zhang, D.; Chen, M.; Zhu, D. Clinical cancer immunotherapy: Current progress and prospects. Front. Immunol. 2022, 13, 961805. [Google Scholar] [CrossRef]
- Eno, J. Immunotherapy through the years. J. Adv. Pract. Oncol. 2017, 8, 747–753. [Google Scholar]
- Buchbinder, E.I.; Desai, A. CTLA-4 and PD-1 pathways: Similarities, differences, and implications of their inhibition. Am. J. Clin. Oncol. 2016, 39, 98–106. [Google Scholar] [CrossRef] [PubMed]
- ACA American Cancer Society. Immune Checkpoint Inhibitors and Their Side Effects; American Cancer Society: Atlanta, GA, USA, 2022. [Google Scholar]
- Taha, T.; Meiri, D.; Talhamy, S.; Wollner, M.; Peer, A.; Bar-Sela, G. Cannabis impacts tumor response rate to nivolumab in patients with advanced malignancies. Oncologist 2019, 24, 549–554. [Google Scholar] [CrossRef]
- Bar-Sela, G.; Cohen, I.; Campisi-Pinto, S.; Lewitus, G.M.; Oz-Ari, L.; Jehassi, A.; Peer, A.; Turgeman, I.; Vernicova, O.; Berman, P.; et al. Cannabis consumption used by cancer patients during immunotherapy correlates with poor clinical outcome. Cancers 2020, 12, 2447, Erratum in Cancers 2022, 14, 1957. [Google Scholar] [CrossRef] [PubMed]
- Alderman, B.; Hui, D.; Mukhopadhyay, S.; Bouleuc, C.; Case, A.A.; Amano, K.; Crawford, G.B.; de Feo, G.; Sbrana, A.; Tanco, K.; et al. Multinational Association of Supportive Care in Cancer (MASCC) expert opinion/consensus guidance on the use of cannabinoids for gastrointestinal symptoms in patients with cancer. Support. Care Cancer 2022, 31, 39. [Google Scholar] [CrossRef] [PubMed]
- To, J.; Davis, M.; Sbrana, A.; Alderman, B.; Hui, D.; Mukhopadhyay, S.; Bouleuc, C.; Case, A.A.; Amano, K.; Crawford, G.B.; et al. MASCC guideline: Cannabis for cancer-related pain and risk of harms and adverse events. Support. Care Cancer 2023, 31, 202. [Google Scholar] [CrossRef]
- National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General; Centers for Disease Control and Prevention (US): Atlanta, GA, USA, 2014.
- Pubpeer. Available online: https://pubpeer.com/publications/5AFA302155D8AE02603134F556A085 (accessed on 13 March 2024).
- Pubpeer. Available online: https://pubpeer.com/publications/366C4360C23B9E177F00CA965630F3 (accessed on 13 March 2024).
- Pubpeer. Available online: https://pubpeer.com/publications/85A8F34A338C7E670E8086BBAA31F4 (accessed on 13 March 2024).
- Kandel, D.; Kandel, E. The gateway hypothesis of substance abuse: Developmental, biological and societal perspectives. Acta Pediatr. 2015, 104, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Franke, T.M.; Ho, T.; Christie, C.A. The chi-square test: Often used and more often misinterpreted. Am. J. Eval. 2012, 33, 448–458. [Google Scholar] [CrossRef]
- Yates, F. Contingency tables involving small numbers and the χ2 test. Suppl. J. R. Stat. Soc. 1934, 1, 217–235. [Google Scholar] [CrossRef]
- Campbell, I. Chi-squared and Fisher–Irwin tests of two-by-two tables with small sample recommendations. Stat. Med. 2007, 26, 3661–3675. [Google Scholar] [CrossRef]
- BMJ 8. The Chi Squared Tests|The BMJ.com. BMJ 2019. Available online: https://www.bmj.com/about-bmj/resources-readers/publications/statistics-square-one/8-chi-squared-tests (accessed on 13 March 2024).
- Midthun, D.E. Overview of the Initial Treatment and Prognosis of Lung Cancer; UpToDate: Waltham, MA, USA, 2023. [Google Scholar]
- Clark, J.W.; Sanoff, H.K. Initial Systemic Therapy for Metastatic Colorectal Cancer; UpToDate: Waltham, MA, USA, 2024. [Google Scholar]
- Sosman, J.A. Overview of the Management of Advanced Cutaneous Melanoma; UpToDate: Waltham, MA, USA, 2023. [Google Scholar]
- George, D.; Jonasch, E. Systemic Therapy for Advanced and Metastatic Clear Cell Renal Carcinoma; UpToDate: Waltham, MA, USA, 2014. [Google Scholar]
- GraphPad Prism QuickCalcs. Analyze a 2 × 2 Contingency Table. Available online: https://www.graphpad.com/quickcalcs/contingency1/ (accessed on 13 March 2024).
- Social Science Statistics. Chi Square Calculator 2 × 2. Available online: https://www.socscistatistics.com/tests/chisquare/default2.aspx (accessed on 13 March 2024).
- GraphPad QuickCalcs: T-Test Calculator. Available online: https://www.graphpad.com/quickcalcs/ttest1/ (accessed on 13 March 2024).
- Rodgman, A.; Perfetti, T.A. The Chemical Components of Tobacco and Tobacco Smoke; CRC Press: Boca Raton, FL, USA, 2008. [Google Scholar]
- Centers for Disease Control and Prevention (US); National Center for Chronic Disease Prevention and Health Promotion (US); Office on Smoking and Health (US). How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease: A Report of the Surgeon General; Centers for Disease Control and Prevention (US): Atlanta, GA, USA, 2010; Volume 5.
- CDC. Centers for Disease Control and Prevention. 2019. Cancer and Tobacco Use. Available online: https://www.cdc.gov/vitalsigns/cancerandtobacco/index.html (accessed on 7 March 2024).
- Lowy, D.R.; Fiore, M.C.; Willis, G.; Mangold, K.N.; Bloch, M.H.; Baker, T.B. Treating smoking in cancer patients: An essential component of cancer care—The New National Cancer Institute Tobacco Control Monograph. JCO Oncol. Pract. 2022, 18, e1971–e1976. [Google Scholar] [CrossRef]
- Ban, W.H.; Yeo, C.D.; Han, S.; Kang, H.S.; Park, C.K.; Kim, J.S.; Kim, J.W.; Kim, S.J.; Lee, S.H.; Kim, S.K. Impact of smoking amount on clinicopathological features and survival in non-small cell lung cancer. BMC Cancer 2020, 20, 848. [Google Scholar] [CrossRef]
- Li, Z.; Wang, Z.; Yu, Y.; Zhang, H.; Chen, L. Smoking is inversely related to cutaneous malignant melanoma: Results of a meta-analysis. Br. J. Dermatol. 2015, 173, 1540–1543. [Google Scholar] [CrossRef]
- Sondermeijer, L.; Lamboo, L.G.E.; de Waal, A.C.; Galesloot, T.E.; Kiemeney, L.A.L.M.; van Rossum, M.; Aben, K.H. Cigarette smoking and the risk of cutaneous melanoma: A case-control study. Dermatology 2020, 236, 228–236. [Google Scholar] [CrossRef]
- Gibson, J.G.; Dobbs, T.D.; Griffiths, R.; Song, J.; Akbari, A.; Whitaker, A.; Langan, S.M.; Hutchings, H.A.; Lyons, R.A.; Whitaker, I.S.; et al. The association of smoking and socioeconomic status on cutaneous melanoma: A population-based, data-linkage, case-control study. Br. J. Dermatol. 2020, 182, 1136–1147. [Google Scholar] [CrossRef] [PubMed]
- Jackson, K.M.; Jones, P.C.; Fluke, L.M.; Fischer, T.D.; Thompson, J.F.; Cochran, A.J.; Stern, S.L.; Faries, M.B.; Hoon, D.S.B.; Foshag, L.J. Smoking status and survival in patients with early-stage primary cutaneous melanoma. JAMA Netw. Open 2024, 7, e2354751. [Google Scholar] [CrossRef] [PubMed]
- Hunt, J.D.; Van Der Hel, O.L.; McMillan, G.P.; Boffetta, P.; Brennan, P. Renal cell carcinoma in relation to cigarette smoking: Meta-analysis of 24 studies. Int. J. Cancer 2005, 114, 101–108. [Google Scholar] [CrossRef]
- Xu, Y.; Qi, Y.; Zhang, J.; Lu, Y.; Song, J.; Dong, B.; Xue, W.; Huang, Y. The impact of smoking on survival in renal cell carcinoma: A systematic review and meta-analysis. Tumour. Biol. 2014, 35, 6633–6640. [Google Scholar] [CrossRef] [PubMed]
- Hardwicke, T.E.; Goodman, S.N. How often do leading biomedical journals use statistical experts to evaluate statistical methods? The results of a survey. PLoS ONE 2020, 15, e0239598. [Google Scholar] [CrossRef] [PubMed]
- Nuijten, M.B.; Hartgerink, C.H.; van Assen, M.A.; Epskamp, S.; Wicherts, J.M. The prevalence of statistical reporting errors in psychology (1985–2013). Behav. Res. Methods 2016, 48, 1205–1226. [Google Scholar] [CrossRef] [PubMed]
- Nuijten, M.B.; Polanin, J.R. “Statcheck”: Automatically detect statistical reporting inconsistencies to increase reproducibility of meta-analyses. Res. Synth. Methods 2020, 11, 574–579. [Google Scholar] [CrossRef]
- Waissengrin, B.; Leshem, Y.; Taya, M.; Meiri, D.; Merimsky, O.; Shamai, S.; Wolf, I.; Rubinek, T. The use of medical cannabis concomitantly with immune checkpoint inhibitors in non-small cell lung cancer: A sigh of relief? Eur. J. Cancer 2023, 180, 52–61. [Google Scholar] [CrossRef] [PubMed]
- Wakefield, A.J.; Murch, S.H.; Anthony, A.; Linnell, J.; Casson, D.M.; Malik, M.; Berelowitz, M.; Dhillon, A.P.; Thomson, M.A.; Harvey, P.; et al. Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children. Lancet 1998, 351, 637–641, Erratum in Lancet 2004, 363, 750. [Google Scholar] [CrossRef] [PubMed]
- Wakefield, A.J.; Murch, S.H.; Anthony, A.; Linnell, J.; Casson, D.M.; Malik, M.; Berelowitz, M.; Dhillon, A.P.; Thomson, M.A.; Harvey, P.; et al. Retraction: Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children. Lancet 2010, 375, 445. [Google Scholar]
- Cancers MDPI. Open Access and Article Processing Charge (APC). Available online: https://www.mdpi.com/journal/cancers/apc#:~:text=All%20articles%20published%20in%20Cancers,papers%20accepted%20after%20peer%20review (accessed on 14 March 2024).
- The Oncologist. Instructions to Authors. Available online: https://academic.oup.com/oncolo/pages/general-instructions (accessed on 14 March 2024).
- Cancers MDPI. Supplemental Materials. Available online: https://www.mdpi.com/journal/cancers/instructions#suppmaterials (accessed on 14 March 2024).
- Kovalchuk, O.; Kovalchuk, I. Cannabinoids as anticancer therapeutic agents. Cell Cycle 2020, 19, 961–989. [Google Scholar] [CrossRef]
- Laezza, C.; Pagano, C.; Navarra, G.; Pastorino, O.; Proto, M.C.; Fiore, D.; Piscopo, C.; Gazzerro, P.; Bifulco, M. The endocannabinoid system: A target for cancer treatment. Int. J. Mol. Sci. 2020, 21, 747. [Google Scholar] [CrossRef]
- Zaiachuk, M.; Pryimak, N.; Kovalchuk, O.; Kovalchuk, I. Cannabinoids, medical cannabis, and colorectal cancer immunotherapy. Front. Med. 2021, 8, 713153. [Google Scholar] [CrossRef]
- Sun, D.; Li, X.; Nie, S.; Liu, J.; Wang, S. Disorders of cancer metabolism: The therapeutic potential of cannabinoids. Biomed. Pharmacother. 2023, 157, 113993. [Google Scholar] [CrossRef] [PubMed]
- Stuart, H.; Hurlbert, R.; Levine; Jessica, U. Coup de Grâce for a tough old bull: “Statistically significant” expires. Am. Stat. 2019, 73, 352–357. [Google Scholar]
- Tanasescu, R.; Constantinescu, C.S. Cannabinoids and the immune system: An overview. Immunobiology 2010, 215, 588–597. [Google Scholar] [CrossRef] [PubMed]
- Besançon, L.; Peiffer-Smadja, N.; Segalas, C.; Jiang, H.; Masuzzo, P.; Smout, C.; Billy, E.; Deforet, M.; Leyrat, C. Open science saves lives: Lessons from the COVID-19 pandemic. BMC Med. Res. Methodol. 2021, 21, 117. [Google Scholar] [CrossRef] [PubMed]
- Ioannidis, J.P.A. Why most published research findings are false. PLoS Med. 2005, 2, e124. [Google Scholar] [CrossRef] [PubMed]
- Fernández, J.; Silván, B.; Entrialgo-Cadierno, R.; Villar, C.J.; Capasso, R.; Uranga, J.A.; Lombó, F.; Abalo, R. Antiproliferative and palliative activity of flavonoids in colorectal cancer. Biomed. Pharmacother. 2021, 143, 112241. [Google Scholar] [CrossRef] [PubMed]
- Şahin, T.Ö.; Yılmaz, B.; Yeşilyurt, N.; Cicia, D.; Szymanowska, A.; Amero, P.; Ağagündüz, D.; Capasso, R. Recent insights into the nutritional immunomodulation of cancer-related microRNAs. Phytother. Res. 2023, 37, 4375–4397. [Google Scholar] [CrossRef] [PubMed]
- Pagano, E.; Romano, B.; Cicia, D.; Iannotti, F.A.; Venneri, T.; Lucariello, G.; Nanì, M.F.; Cattaneo, F.; De Cicco, P.; D’Armiento, M.; et al. TRPM8 indicates poor prognosis in colorectal cancer patients and its pharmacological targeting reduces tumour growth in mice by inhibiting Wnt/β-catenin signalling. Br. J. Pharmacol. 2023, 180, 235–251. [Google Scholar] [CrossRef]
- Ağagündüz, D.; Cocozza, E.; Cemali, Ö.; Bayazıt, A.D.; Nanì, M.F.; Cerqua, I.; Morgillo, F.; Saygılı, S.K.; Canani, R.B.; Amero, P.; et al. Understanding the role of the gut microbiome in gastrointestinal cancer: A review. Front. Pharmacol. 2023, 14, 1130562. [Google Scholar] [CrossRef]
- Zeng, H.; Lazarova, D.L.; Bordonaro, M. Mechanisms linking dietary fiber, gut microbiota and colon cancer prevention. World J. Gastrointest. Oncol. 2014, 6, 41–51. [Google Scholar] [CrossRef]
- Bodine, M.; Kemp, A.K. Medical Cannabis Use in Oncology. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar]
- Ramer, R.; Wendt, F.; Wittig, F.; Schäfer, M.; Boeckmann, L.; Emmert, S.; Hinz, B. Impact of Cannabinoid Compounds on Skin Cancer. Cancers 2022, 14, 1769. [Google Scholar] [CrossRef]
- Abrams, D.I.; Velasco, G.; Twelves, C.; Ganju, R.K.; Bar-Sela, G. Cancer Treatment: Preclinical & Clinical. J. Natl. Cancer Inst. Monogr. 2021, 2021, 107–113. [Google Scholar] [CrossRef]
- Nugent, S.M.; Meghani, S.H.; Rogal, S.S.; Merlin, J.S. Medical Cannabis Use among Individuals with Cancer: An Unresolved and Timely Issue. Cancer 2020, 126, 1832–1836. [Google Scholar] [CrossRef]
- Creanga-Murariu, I.; Filipiuc, L.E.; Cuciureanu, M.; Tamba, B.-I.; Alexa-Stratulat, T. Should Oncologists Trust Cannabinoids? Front. Pharmacol. 2023, 14, 1211506. [Google Scholar] [CrossRef] [PubMed]
- Nahler, G. Cannabidiol and Other Phytocannabinoids as Cancer Therapeutics. Pharmaceut. Med. 2022, 36, 99–129. [Google Scholar] [CrossRef]
- Abu-Amna, M.; Salti, T.; Khoury, M.; Cohen, I.; Bar-Sela, G. Medical Cannabis in Oncology: A Valuable Unappreciated Remedy or an Undesirable Risk? Curr. Treat. Options Oncol. 2021, 22, 16. [Google Scholar] [CrossRef] [PubMed]
- Sarsembayeva, A.; Schicho, R. Cannabinoids and the Endocannabinoid System in Immunotherapy: Helpful or Harmful? Front. Oncol. 2023, 13, 1296906. [Google Scholar] [CrossRef] [PubMed]
- Hinz, B.; Ramer, R. Cannabinoids as Anticancer Drugs: Current Status of Preclinical Research. Br. J. Cancer 2022, 127, 1–13. [Google Scholar] [CrossRef]

| Variable | Smallest Cell N Observed (Expected) | BMJ Statistic | Reported p | Calculated p | Interpretation |
|---|---|---|---|---|---|
| Gender | 10 (10.67) | chi-square | 0.9399 C or F | 0.9399 Y | Misreported |
| ECOG | 10 (7.67) | chi-square | 0.3568 C or F | 0.3568 Y | Misreported |
| Chronic diseases = 0 Chronic diseases = 1 Chronic diseases = 2+ | 13 (11.67) 7 (7.67) 14 (14.67) | chi-square chi-square chi-square | 0.7124 C or F 0.9332 C or F 0.9437 C or F | 0.7124 Y 0.9332 Y 0.9437 Y | Misreported Misreported Misreported |
| Chronic heart disease | 5 (7.67) | chi-square | 0.2762 C or F | 0.2762 Y | Misreported |
| Diabetes | 6 (7.67) | chi-square | 0.5576 C or F | 0.5576 Y | Misreported |
| High blood pressure | 13 (15.67) | chi-square | 0.3612 C or F | 0.3612 Y | Misreported |
| COPD | 3 (4.00) | chi-square | 1 C or F | 0.5145 C, 0.7463 F, 0.7445 Y | Unverified |
| Hyperlipidemia | 7 (10.00) | chi-square | 0.2491 C or F | 0.2491 Y | Misreported |
| Other disease | 0 (-) | chi-square | 1 C or F | 0.3125 C, 0.5512 F, 0.8007 Y | Unverified |
| Non-small-cell LC | 14 (15.00) | chi-square | 0.8325 C or F | 0.8325 Y | Misreported |
| Melanoma | 9 (11.33) | chi-square | 0.414 C or F | 0.4140 Y | Misreported |
| Renal cell carcinoma | 2 (2.00) | chi-square | 1 C or F | 1.000 C,F,Y | Verified |
| Other malignancy | 3 (1.67) | chi-square | 1 C or F | 0.1946 C, 0.3300 F, 0.4175 Y | Unverified |
| Brain metastasis | 8 (6.67) | chi-square | 0.6593 C or F | 0.6593 Y | Misreported |
| Lungs metastasis | 11 (13.33) | chi-square | 0.4303 C or F | 0.4303 Y | Misreported |
| Liver metastasis | 11 (8.00) | chi-square | 0.2157 C or F | 0.2157 Y | Misreported |
| Immunotherapy 1st line | 8 (13.00) | chi-square | 0.05178 C or F | 0.0518 Y | Misreported |
| Pembrolizumab or nivo | 5 (8.67) | chi-square | 0.127 C or F | 0.1270 Y | Misreported |
| Ipilimumab and nivo | 4 (6.67) | chi-square | 0.2517 C or F | 0.2517 Y | Misreported |
| Durvalumab or atezo | 1 (2.00) | chi-square | 1 C or F | 0.3720 C, 0.6607 F, 0.6554 Y | Unverified |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Piper, B.J.; Tian, M.; Saini, P.; Higazy, A.; Graham, J.; Carbe, C.J.; Bordonaro, M. Immunotherapy and Cannabis: A Harmful Drug Interaction or Reefer Madness? Cancers 2024, 16, 1245. https://doi.org/10.3390/cancers16071245
Piper BJ, Tian M, Saini P, Higazy A, Graham J, Carbe CJ, Bordonaro M. Immunotherapy and Cannabis: A Harmful Drug Interaction or Reefer Madness? Cancers. 2024; 16(7):1245. https://doi.org/10.3390/cancers16071245
Chicago/Turabian StylePiper, Brian J., Maria Tian, Pragosh Saini, Ahmad Higazy, Jason Graham, Christian J. Carbe, and Michael Bordonaro. 2024. "Immunotherapy and Cannabis: A Harmful Drug Interaction or Reefer Madness?" Cancers 16, no. 7: 1245. https://doi.org/10.3390/cancers16071245
APA StylePiper, B. J., Tian, M., Saini, P., Higazy, A., Graham, J., Carbe, C. J., & Bordonaro, M. (2024). Immunotherapy and Cannabis: A Harmful Drug Interaction or Reefer Madness? Cancers, 16(7), 1245. https://doi.org/10.3390/cancers16071245