Biomarkers in the Diagnosis of Endometrial Precancers. Molecular Characteristics, Candidate Immunohistochemical Markers, and Promising Results of Three-Marker Panel: Current Status and Future Directions
Abstract
Simple Summary
Abstract
1. Introduction
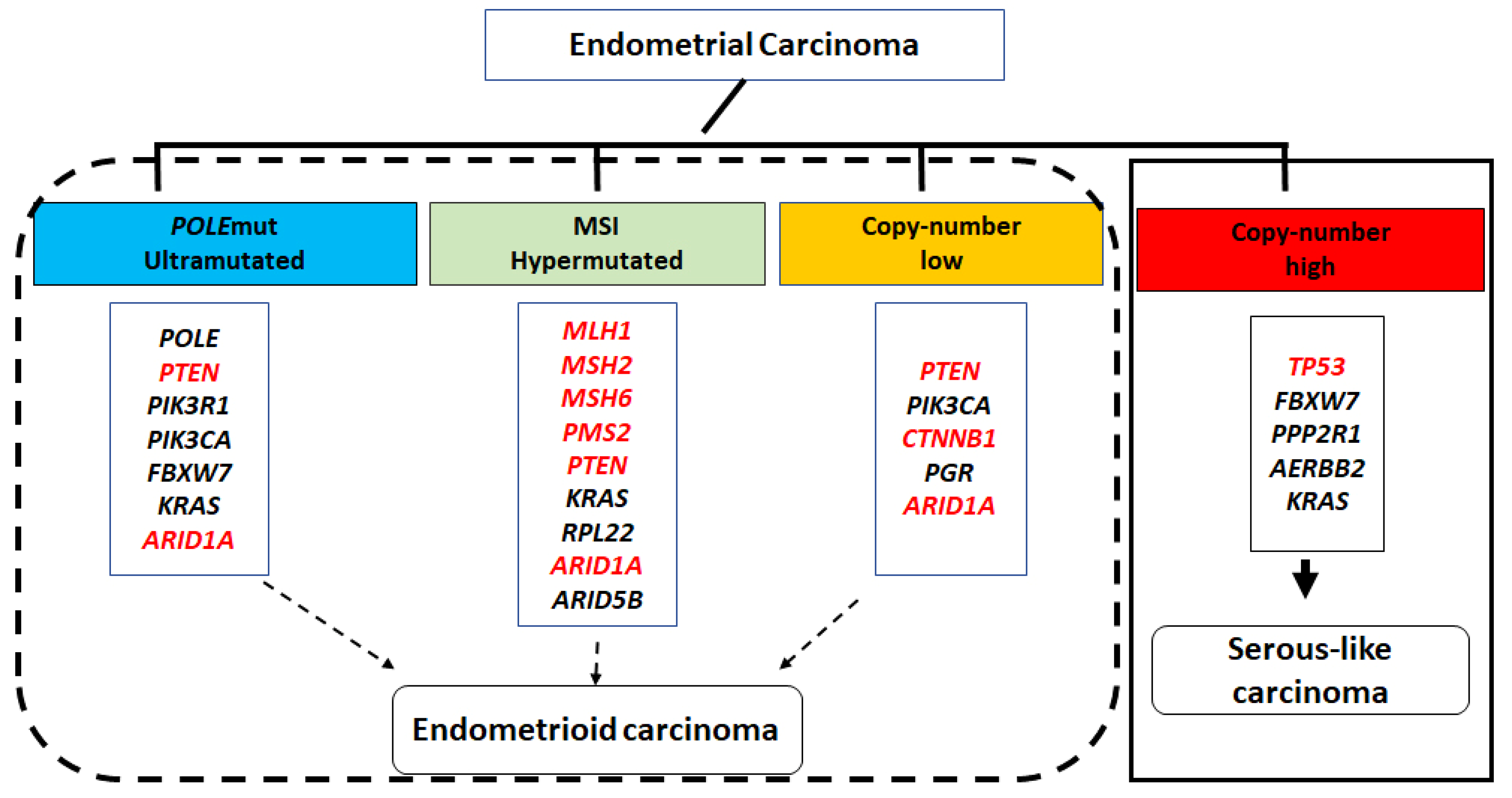
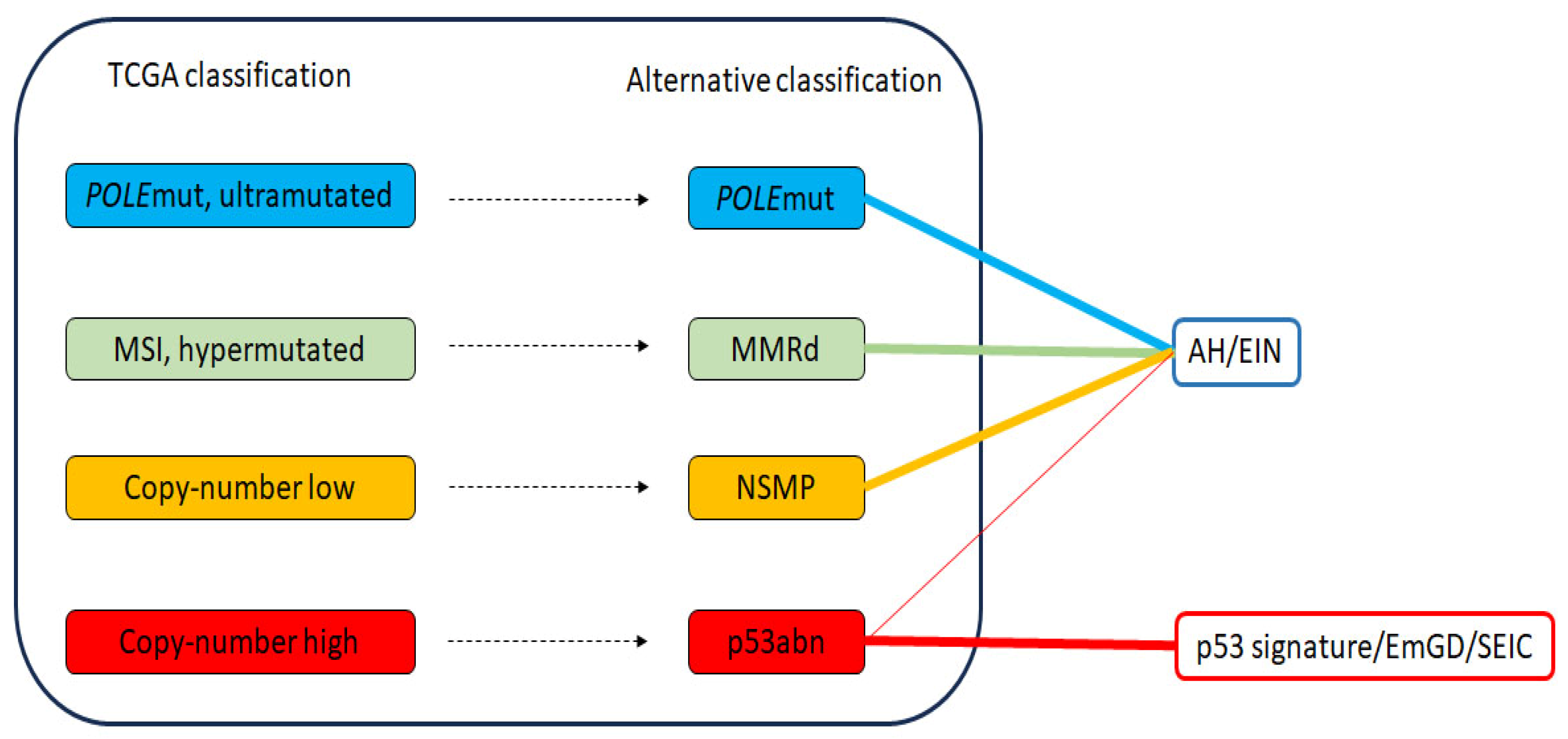
2. Molecular Classification of Endometrial Carcinoma
3. Diagnostic System of the Precancers of Endometrial Adenocarcinoma
4. Genetic Characteristics of AH/EIN and Its Association with Carcinoma
5. Candidate Immunohistochemical Biomarkers for Diagnosing AH/EIN
5.1. PAX2
5.2. PTEN
5.3. β-Catenin
5.4. Mismatch Repair (MMR) Proteins
5.5. ARID1A
5.6. p53
6. Multi-Marker Panels for Identifying AH/EIN
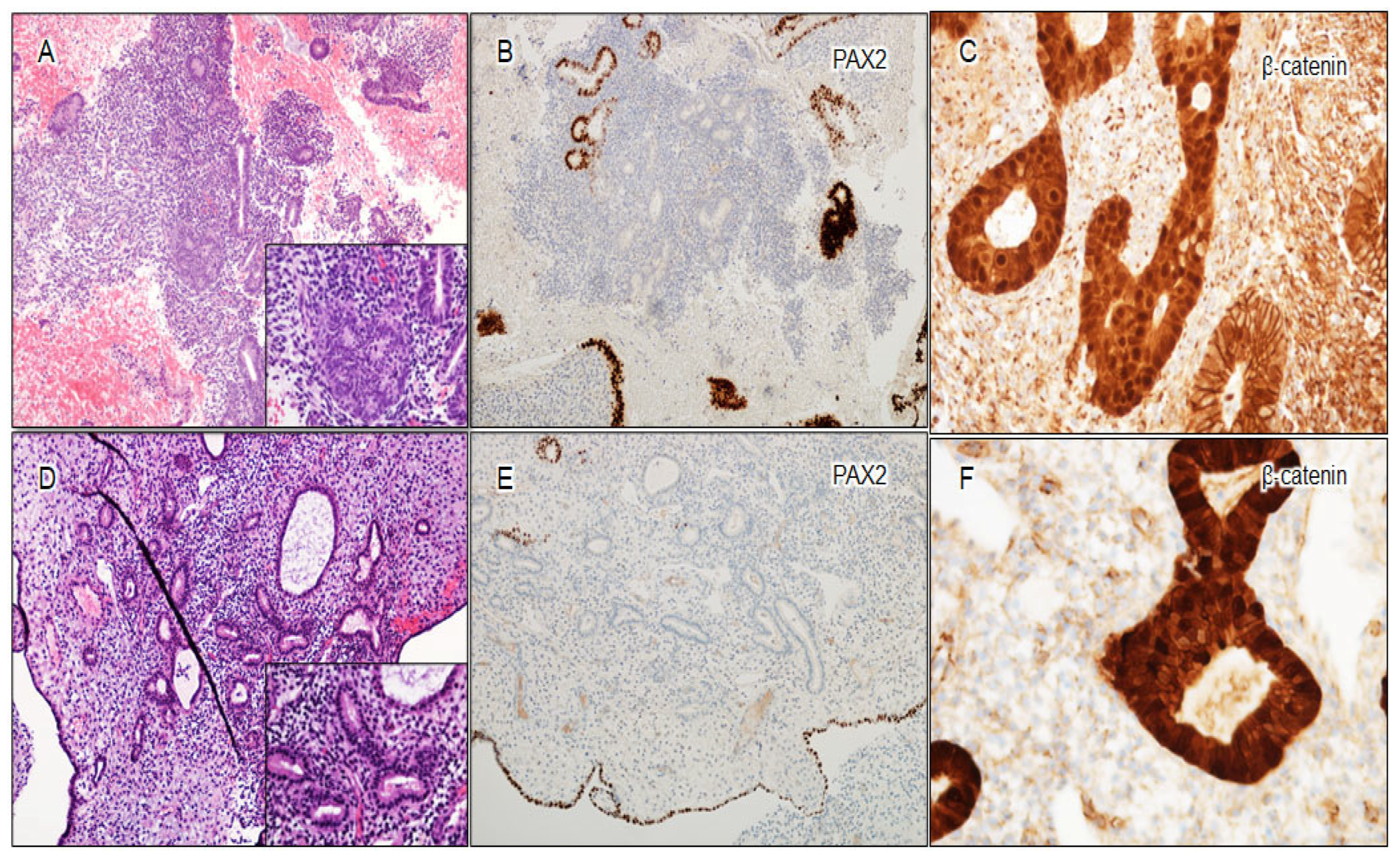
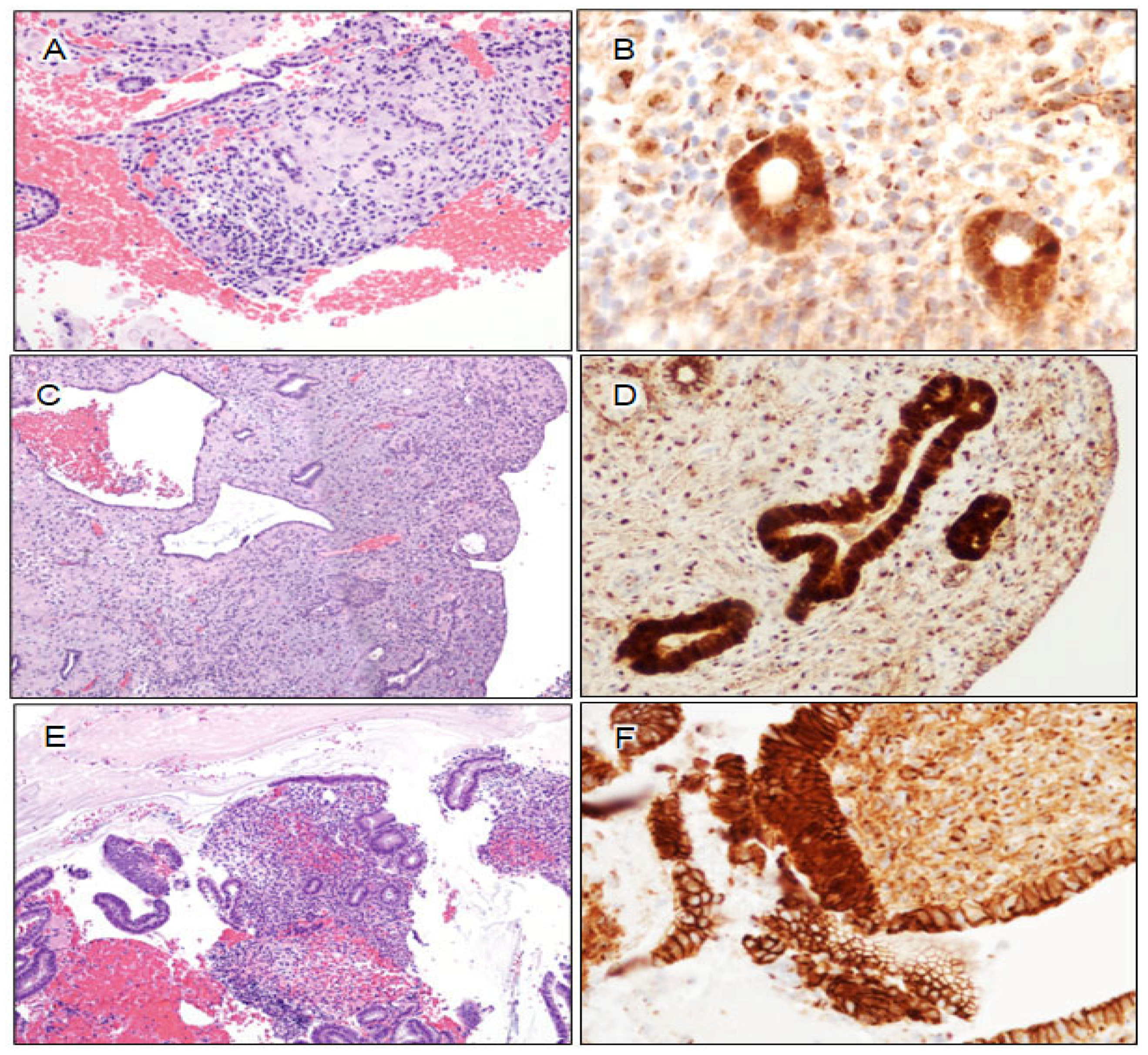
6.1. Morules as Surrogate Markers for β-Catenin Mutation
6.2. Utility of Three-Marker Panel Plus Morules in Diagnosis of Challenging AH/EIN
6.2.1. Utility of Three-Marker Panel Plus Morules in AH/EIN in Polyps
6.2.2. Utility of Three-Marker Panel Plus Morules in Secretory AH/EIN
6.2.3. Utility of Three-Marker Panel in Small-Sized AH/EIN
6.2.4. Utility of Three-Marker Panel Plus Morules in the Identification of Residual Lesion in Progestin-Treated AH/EIN
6.2.5. Utility of Three-Marker Panel in Other Putative Endometrial Precancers
7. Limitations of Three-Marker Panel
7.1. Detection Ceiling of Marker Panel
7.2. Resolution Ceiling of PAX2 and PTEN
7.3. Potential Advantages of an Expanded Panel
8. Unresolved Issues and Future Directions
8.1. Uncertain Significance of β-Catenin Aberrancy and Isolated Morules in Seemingly Normal Endometrial Glands during or after the Cessation of Progestin Therapy
8.2. Discordance between Morphology and Marker Aberrancy
9. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2019. CA Cancer J. Clin. 2019, 69, 7–34. [Google Scholar] [CrossRef]
- Constantine, G.D.; Kessler, G.; Graham, S.; Goldstein, S.R. Increased Incidence of Endometrial Cancer Following the Women’s Health Initiative: An Assessment of Risk Factors. J. Womens Health 2019, 28, 237–243. [Google Scholar] [CrossRef]
- Mutter, G.L.; Lax, S.F. Endometrial atypical hyperplasia/endometrioid intraepithelial neoplasia. In Female Genital Tumours, WHO Classification of Tumours Series, 5th ed.; WHO Classification of Tumours Editorial Board, Ed.; International Agency for Research on Cancer: Lyon, France, 2020; Volume 4, pp. 250–251. [Google Scholar]
- Leon-Castillo, A.; de Boer, S.M.; Powell, M.E.; Mileshkin, L.R.; Mackay, H.J.; Leary, A.; Nijman, H.W.; Singh, N.; Pollock, P.M.; Bessette, P.; et al. Molecular Classification of the PORTEC-3 Trial for High-Risk Endometrial Cancer: Impact on Prognosis and Benefit from Adjuvant Therapy. J. Clin. Oncol. 2020, 38, 3388–3397. [Google Scholar] [CrossRef] [PubMed]
- Piulats, J.M.; Guerra, E.; Gil-Martin, M.; Roman-Canal, B.; Gatius, S.; Sanz-Pamplona, R.; Velasco, A.; Vidal, A.; Matias-Guiu, X. Molecular approaches for classifying endometrial carcinoma. Gynecol. Oncol. 2017, 145, 200–207. [Google Scholar] [CrossRef]
- Talhouk, A.; McConechy, M.K.; Leung, S.; Li-Chang, H.H.; Kwon, J.S.; Melnyk, N.; Yang, W.; Senz, J.; Boyd, N.; Karnezis, A.N.; et al. A clinically applicable molecular-based classification for endometrial cancers. Br. J. Cancer 2015, 113, 299–310. [Google Scholar] [CrossRef] [PubMed]
- Levine, D.A.; The Cancer Genome Atlas Research Network. Integrated genomic characterization of endometrial carcinoma. Nature 2013, 497, 67–73. [Google Scholar] [CrossRef]
- Stelloo, E.; Nout, R.A.; Osse, E.M.; Jurgenliemk-Schulz, I.J.; Jobsen, J.J.; Lutgens, L.C.; van der Steen-Banasik, E.M.; Nijman, H.W.; Putter, H.; Bosse, T.; et al. Improved Risk Assessment by Integrating Molecular and Clinicopathological Factors in Early-stage Endometrial Cancer-Combined Analysis of the PORTEC Cohorts. Clin. Cancer Res. 2016, 22, 4215–4224. [Google Scholar] [CrossRef]
- Talhouk, A.; McConechy, M.K.; Leung, S.; Yang, W.; Lum, A.; Senz, J.; Boyd, N.; Pike, J.; Anglesio, M.; Kwon, J.S.; et al. Confirmation of ProMisE: A simple, genomics-based clinical classifier for endometrial cancer. Cancer 2017, 123, 802–813. [Google Scholar] [CrossRef] [PubMed]
- Vermij, L.; Smit, V.; Nout, R.; Bosse, T. Incorporation of molecular characteristics into endometrial cancer management. Histopathology 2020, 76, 52–63. [Google Scholar] [CrossRef]
- Devereaux, K.A.; Weiel, J.J.; Pors, J.; Steiner, D.F.; Ho, C.; Charu, V.; Suarez, C.J.; Renz, M.; Diver, E.; Karam, A.; et al. Prospective molecular classification of endometrial carcinomas: Institutional implementation, practice, and clinical experience. Mod. Pathol. 2022, 35, 688–696. [Google Scholar] [CrossRef]
- Vermij, L.; Léon-Castillo, A.; Singh, N.; Powell, M.E.; Edmondson, R.J.; Genestie, C.; Khaw, P.; Pyman, J.; McLachlin, C.M.; Ghatage, P.; et al. p53 immunohistochemistry in endometrial cancer: Clinical and molecular correlates in the PORTEC-3 trial. Mod. Pathol. 2022, 35, 1475–1483. [Google Scholar] [CrossRef]
- Mutter, G.L. Endometrial intraepithelial neoplasia (EIN): Will it bring order to chaos? The Endometrial Collaborative Group. Gynecol. Oncol. 2000, 76, 287–290. [Google Scholar] [CrossRef]
- Jarboe, E.A.; Mutter, G.L. Endometrial intraepithelial neoplasia. Semin. Diagn. Pathol. 2010, 27, 215–225. [Google Scholar] [CrossRef]
- Baak, J.P.; Mutter, G.L. EIN and WHO94. J. Clin. Pathol. 2005, 58, 1–6. [Google Scholar] [CrossRef]
- Hou, J.Y.; McAndrew, T.C.; Goldberg, G.L.; Whitney, K.; Shahabi, S. A clinical and pathologic comparison between stage-matched endometrial intraepithelial carcinoma and uterine serous carcinoma: Is there a difference? Reprod. Sci. 2014, 21, 532–537. [Google Scholar] [CrossRef] [PubMed]
- Soslow, R.A.; Pirog, E.; Isacson, C. Endometrial intraepithelial carcinoma with associated peritoneal carcinomatosis. Am. J. Surg. Pathol. 2000, 24, 726–732. [Google Scholar] [CrossRef] [PubMed]
- Zheng, W.; Xiang, L.; Fadare, O.; Kong, B. A proposed model for endometrial serous carcinogenesis. Am. J. Surg. Pathol. 2011, 35, e1–e14. [Google Scholar] [CrossRef]
- Fadare, O.; Zheng, W. Insights into endometrial serous carcinogenesis and progression. Int. J. Clin. Exp. Pathol. 2009, 2, 411–432. [Google Scholar] [PubMed]
- Li, L.; Yue, P.; Song, Q.; Yen, T.T.; Asaka, S.; Wang, T.L.; Beavis, A.L.; Fader, A.N.; Jiao, Y.; Yuan, G.; et al. Genome-wide mutation analysis in precancerous lesions of endometrial carcinoma. J. Pathol. 2021, 253, 119–128. [Google Scholar] [CrossRef] [PubMed]
- Russo, M.; Broach, J.; Sheldon, K.; Houser, K.R.; Liu, D.J.; Kesterson, J.; Phaeton, R.; Hossler, C.; Hempel, N.; Baker, M.; et al. Clonal evolution in paired endometrial intraepithelial neoplasia/atypical hyperplasia and endometrioid adenocarcinoma. Hum. Pathol. 2017, 67, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Chapel, D.B.; Patil, S.A.; Plagov, A.; Puranik, R.; Mendybaeva, A.; Steinhardt, G.; Wanjari, P.; Lastra, R.R.; Kadri, S.; Segal, J.P.; et al. Quantitative next-generation sequencing-based analysis indicates progressive accumulation of microsatellite instability between atypical hyperplasia/endometrial intraepithelial neoplasia and paired endometrioid endometrial carcinoma. Mod. Pathol. 2019, 32, 1508–1520. [Google Scholar] [CrossRef] [PubMed]
- Aguilar, M.; Zhang, H.; Zhang, M.; Cantarell, B.; Sahoo, S.S.; Li, H.D.; Cuevas, I.C.; Lea, J.; Miller, D.S.; Chen, H.; et al. Serial genomic analysis of endometrium supports the existence of histologically indistinct endometrial cancer precursors. J. Pathol. 2021, 254, 20–30. [Google Scholar] [CrossRef] [PubMed]
- Russo, M.; Newell, J.M.; Budurlean, L.; Houser, K.R.; Sheldon, K.; Kesterson, J.; Phaeton, R.; Hossler, C.; Rosenberg, J.; DeGraff, D.; et al. Mutational profile of endometrial hyperplasia and risk of progression to endometrioid adenocarcinoma. Cancer 2020, 126, 2775–2783. [Google Scholar] [CrossRef]
- Aguilar, M.; Chen, H.; Rivera-Colon, G.; Niu, S.; Carrick, K.; Gwin, K.; Cuevas, I.C.; Sahoo, S.S.; Li, H.D.; Zhang, S.; et al. Reliable Identification of Endometrial Precancers Through Combined Pax2, β-Catenin, and Pten Immunohistochemistry. Am. J. Surg. Pathol. 2022, 46, 404–414. [Google Scholar] [CrossRef]
- Lucas, E.; Chen, H.; Molberg, K.; Castrillon, D.H.; Rivera Colon, G.; Li, L.; Hinson, S.; Thibodeaux, J.; Lea, J.; Miller, D.S.; et al. Mismatch Repair Protein Expression in Endometrioid Intraepithelial Neoplasia/Atypical Hyperplasia: Should We Screen for Lynch Syndrome in Precancerous Lesions? Int. J. Gynecol. Pathol. 2019, 38, 533–542. [Google Scholar] [CrossRef]
- Casey, L.; Singh, N. POLE, MMR, and MSI Testing in Endometrial Cancer: Proceedings of the ISGyP Companion Society Session at the USCAP 2020 Annual Meeting. Int. J. Gynecol. Pathol. 2021, 40, 5–16. [Google Scholar] [CrossRef]
- Chen, H.; Strickland, A.L.; Castrillon, D.H. Histopathologic diagnosis of endometrial precancers: Updates and future directions. Semin. Diagn. Pathol. 2022, 39, 137–147. [Google Scholar] [CrossRef]
- Tong, G.X.; Chiriboga, L.; Hamele-Bena, D.; Borczuk, A.C. Expression of PAX2 in papillary serous carcinoma of the ovary: Immunohistochemical evidence of fallopian tube or secondary Mullerian system origin? Mod. Pathol. 2007, 20, 856–863. [Google Scholar] [CrossRef]
- Monte, N.M.; Webster, K.A.; Neuberg, D.; Dressler, G.R.; Mutter, G.L. Joint loss of PAX2 and PTEN expression in endometrial precancers and cancer. Cancer Res. 2010, 70, 6225–6232. [Google Scholar] [CrossRef]
- Jovanovic, A.S.; Boynton, K.A.; Mutter, G.L. Uteri of women with endometrial carcinoma contain a histopathological spectrum of monoclonal putative precancers, some with microsatellite instability. Cancer Res. 1996, 56, 1917–1921. [Google Scholar] [PubMed]
- Mutter, G.L.; Ince, T.A.; Baak, J.P.; Kust, G.A.; Zhou, X.P.; Eng, C. Molecular identification of latent precancers in histologically normal endometrium. Cancer Res. 2001, 61, 4311–4314. [Google Scholar] [PubMed]
- Moreno-Bueno, G.; Hardisson, D.; Sarrio, D.; Sanchez, C.; Cassia, R.; Prat, J.; Herman, J.G.; Esteller, M.; Matias-Guiu, X.; Palacios, J. Abnormalities of E- and P-cadherin and catenin (β-, γ-catenin, and p120ctn) expression in endometrial cancer and endometrial atypical hyperplasia. J. Pathol. 2003, 199, 471–478. [Google Scholar] [CrossRef] [PubMed]
- Levine, R.L.; Cargile, C.B.; Blazes, M.S.; van Rees, B.; Kurman, R.J.; Ellenson, L.H. PTEN mutations and microsatellite instability in complex atypical hyperplasia, a precursor lesion to uterine endometrioid carcinoma. Cancer Res. 1998, 58, 3254–3258. [Google Scholar] [PubMed]
- Maxwell, G.L.; Risinger, J.I.; Gumbs, C.; Shaw, H.; Bentley, R.C.; Barrett, J.C.; Berchuck, A.; Futreal, P.A. Mutation of the PTEN tumor suppressor gene in endometrial hyperplasias. Cancer Res. 1998, 58, 2500–2503. [Google Scholar]
- Duggan, B.D.; Felix, J.C.; Muderspach, L.I.; Tsao, J.L.; Shibata, D.K. Early mutational activation of the c-Ki-ras oncogene in endometrial carcinoma. Cancer Res. 1994, 54, 1604–1607. [Google Scholar]
- Mutter, G.L.; Wada, H.; Faquin, W.C.; Enomoto, T. K-ras mutations appear in the premalignant phase of both microsatellite stable and unstable endometrial carcinogenesis. Mol. Pathol. 1999, 52, 257–262. [Google Scholar] [CrossRef]
- Sasaki, H.; Nishii, H.; Takahashi, H.; Tada, A.; Furusato, M.; Terashima, Y.; Siegal, G.P.; Parker, S.L.; Kohler, M.F.; Berchuck, A.; et al. Mutation of the Ki-ras protooncogene in human endometrial hyperplasia and carcinoma. Cancer Res. 1993, 53, 1906–1910. [Google Scholar]
- Werner, H.M.; Berg, A.; Wik, E.; Birkeland, E.; Krakstad, C.; Kusonmano, K.; Petersen, K.; Kalland, K.H.; Oyan, A.M.; Akslen, L.A.; et al. ARID1A loss is prevalent in endometrial hyperplasia with atypia and low-grade endometrioid carcinomas. Mod. Pathol. 2013, 26, 428–434. [Google Scholar] [CrossRef]
- Wu, H.; Chen, Y.; Liang, J.; Shi, B.; Wu, G.; Zhang, Y.; Wang, D.; Li, R.; Yi, X.; Zhang, H.; et al. Hypomethylation-linked activation of PAX2 mediates tamoxifen-stimulated endometrial carcinogenesis. Nature 2005, 438, 981–987. [Google Scholar] [CrossRef] [PubMed]
- Patricio, P.; Ramalho-Carvalho, J.; Costa-Pinheiro, P.; Almeida, M.; Barros-Silva, J.D.; Vieira, J.; Dias, P.C.; Lobo, F.; Oliveira, J.; Teixeira, M.R.; et al. Deregulation of PAX2 expression in renal cell tumours: Mechanisms and potential use in differential diagnosis. J. Cell. Mol. Med. 2013, 17, 1048–1058. [Google Scholar] [CrossRef]
- Joiner, A.K.; Quick, C.M.; Jeffus, S.K. Pax2 expression in simultaneously diagnosed WHO and EIN classification systems. Int. J. Gynecol. Pathol. 2015, 34, 40–46. [Google Scholar] [CrossRef]
- Owings, R.A.; Quick, C.M. Endometrial intraepithelial neoplasia. Arch. Pathol. Lab. Med. 2014, 138, 484–491. [Google Scholar] [CrossRef]
- Quick, C.M.; Laury, A.R.; Monte, N.M.; Mutter, G.L. Utility of PAX2 as a marker for diagnosis of endometrial intraepithelial neoplasia. Am. J. Clin. Pathol. 2012, 138, 678–684. [Google Scholar] [CrossRef]
- Strickland, A.L.; Rivera, G.; Lucas, E.; John, G.; Cuevas, I.; Castrillon, D.H. PI3K Pathway Effectors pAKT and FOXO1 as Novel Markers of Endometrioid Intraepithelial Neoplasia. Int. J. Gynecol. Pathol. 2018, 38, 503–513. [Google Scholar] [CrossRef]
- Lucas, E.; Niu, S.; Aguilar, M.; Molberg, K.; Carrick, K.; Rivera-Colon, G.; Gwin, K.; Wang, Y.; Zheng, W.; Castrillon, D.H.; et al. Utility of a PAX2, PTEN, and β-catenin Panel in the Diagnosis of Atypical Hyperplasia/Endometrioid Intraepithelial Neoplasia in Endometrial Polyps. Am. J. Surg. Pathol. 2023, 47, 1019–1026. [Google Scholar] [CrossRef] [PubMed]
- Sahoo, S.S.; Aguilar, M.; Xu, Y.; Lucas, E.; Miller, V.; Chen, H.; Zheng, W.; Cuevas, I.C.; Li, H.D.; Hitrys, D.; et al. Endometrial polyps are non-neoplastic but harbor epithelial mutations in endometrial cancer drivers at low allelic frequencies. Mod. Pathol. 2022, 35, 1702–1712. [Google Scholar] [CrossRef] [PubMed]
- Raffone, A.; Travaglino, A.; Saccone, G.; Mascolo, M.; Insabato, L.; Mollo, A.; De Placido, G.; Zullo, F. PAX2 in endometrial carcinogenesis and in differential diagnosis of endometrial hyperplasia: A systematic review and meta-analysis of diagnostic accuracy. Acta Obstet. Gynecol. Scand. 2019, 98, 287–299. [Google Scholar] [CrossRef]
- Chen, H.; Lucas, E.; Strickland, A.L.; Carrick, K.; Gwin, K.; Castrillon, D.H.; Rivera-Colon, G.; Niu, S.; Molberg, K.H.; Zheng, W. Specific Biomarker Expression Patterns in the Diagnosis of Residual and Recurrent Endometrial Precancers after Progestin Treatment: A Longitudinal Study. Am. J. Surg. Pathol. 2020, 44, 1429–1439. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.; Wang, Y.; Wang, Y.; Chan, A.M. Multifaceted Regulation of PTEN Subcellular Distributions and Biological Functions. Cancers 2019, 11, 1247. [Google Scholar] [CrossRef]
- Cheung, L.W.; Hennessy, B.T.; Li, J.; Yu, S.; Myers, A.P.; Djordjevic, B.; Lu, Y.; Stemke-Hale, K.; Dyer, M.D.; Zhang, F.; et al. High frequency of PIK3R1 and PIK3R2 mutations in endometrial cancer elucidates a novel mechanism for regulation of PTEN protein stability. Cancer Discov. 2011, 1, 170–185. [Google Scholar] [CrossRef]
- Bettstetter, M.; Berezowska, S.; Keller, G.; Walch, A.; Feuchtinger, A.; Slotta-Huspenina, J.; Feith, M.; Drecoll, E.; Hofler, H.; Langer, R. Epidermal growth factor receptor, phosphatidylinositol-3-kinase catalytic subunit/PTEN, and KRAS/NRAS/BRAF in primary resected esophageal adenocarcinomas: Loss of PTEN is associated with worse clinical outcome. Hum. Pathol. 2013, 44, 829–836. [Google Scholar] [CrossRef]
- Carnero, A.; Blanco-Aparicio, C.; Renner, O.; Link, W.; Leal, J.F. The PTEN/PI3K/AKT signalling pathway in cancer, therapeutic implications. Curr. Cancer Drug Targets 2008, 8, 187–198. [Google Scholar] [CrossRef]
- Bell, D.W.; Ellenson, L.H. Molecular Genetics of Endometrial Carcinoma. Annu. Rev. Pathol. 2019, 14, 339–367. [Google Scholar] [CrossRef]
- Mutter, G.L.; Lin, M.C.; Fitzgerald, J.T.; Kum, J.B.; Baak, J.P.; Lees, J.A.; Weng, L.P.; Eng, C. Altered PTEN expression as a diagnostic marker for the earliest endometrial precancers. J. Natl. Cancer Inst. 2000, 92, 924–930. [Google Scholar] [CrossRef]
- Nucci, M.R.; Castrillon, D.H.; Bai, H.; Quade, B.J.; Ince, T.A.; Genest, D.R.; Lee, K.R.; Mutter, G.L.; Crum, C.P. Biomarkers in diagnostic obstetric and gynecologic pathology: A review. Adv. Anat. Pathol. 2003, 10, 55–68. [Google Scholar] [CrossRef]
- Nagase, S.; Sato, S.; Tezuka, F.; Wada, Y.; Yajima, A.; Horii, A. Deletion mapping on chromosome 10q25-q26 in human endometrial cancer. Br. J. Cancer 1996, 74, 1979–1983. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Salvesen, H.B.; MacDonald, N.; Ryan, A.; Jacobs, I.J.; Lynch, E.D.; Akslen, L.A.; Das, S. PTEN methylation is associated with advanced stage and microsatellite instability in endometrial carcinoma. Int. J. Cancer 2001, 91, 22–26. [Google Scholar] [CrossRef] [PubMed]
- Villacorte, M.; Suzuki, K.; Hirasawa, A.; Ohkawa, Y.; Suyama, M.; Maruyama, T.; Aoki, D.; Ogino, Y.; Miyagawa, S.; Terabayashi, T.; et al. β-Catenin signaling regulates Foxa2 expression during endometrial hyperplasia formation. Oncogene 2013, 32, 3477–3482. [Google Scholar] [CrossRef] [PubMed]
- Morin, P.J. β-catenin signaling and cancer. Bioessays 1999, 21, 1021–1030. [Google Scholar] [CrossRef]
- Gao, C.; Wang, Y.; Broaddus, R.; Sun, L.; Xue, F.; Zhang, W. Exon 3 mutations of CTNNB1 drive tumorigenesis: A review. Oncotarget 2018, 9, 5492–5508. [Google Scholar] [CrossRef]
- Costigan, D.C.; Dong, F.; Nucci, M.R.; Howitt, B.E. Clinicopathologic and Immunohistochemical Correlates of CTNNB1 Mutated Endometrial Endometrioid Carcinoma. Int. J. Gynecol. Pathol. 2020, 39, 119–127. [Google Scholar] [CrossRef]
- Kim, G.; Kurnit, K.C.; Djordjevic, B.; Singh, C.; Munsell, M.F.; Wang, W.L.; Lazar, A.J.; Zhang, W.; Broaddus, R. Nuclear β-catenin localization and mutation of the CTNNB1 gene: A context-dependent association. Mod. Pathol. 2018, 31, 1553–1559. [Google Scholar] [CrossRef]
- Kurnit, K.C.; Kim, G.N.; Fellman, B.M.; Urbauer, D.L.; Mills, G.B.; Zhang, W.; Broaddus, R.R. CTNNB1 (β-catenin) mutation identifies low grade, early stage endometrial cancer patients at increased risk of recurrence. Mod. Pathol. 2017, 30, 1032–1041. [Google Scholar] [CrossRef] [PubMed]
- Xiong, Y.; Xiong, Y.Y.; Zhou, Y.F. Expression and significance of β-catenin, Glut-1 and PTEN in proliferative endometrium, endometrial intraepithelial neoplasia and endometrioid adenocarcinoma. Eur. J. Gynaecol. Oncol. 2010, 31, 160–164. [Google Scholar] [PubMed]
- Norimatsu, Y.; Moriya, T.; Kobayashi, T.K.; Sakurai, T.; Shimizu, K.; Tsukayama, C.; Ohno, E. Immunohistochemical expression of PTEN and β-catenin for endometrial intraepithelial neoplasia in Japanese women. Ann. Diagn. Pathol. 2007, 11, 103–108. [Google Scholar] [CrossRef]
- Niu, S.; Lucas, E.; Molberg, K.; Strickland, A.; Wang, Y.; Carrick, K.; Rivera-Colon, G.; Gwin, K.; SoRelle, J.A.; Castrillon, D.H.; et al. Morules But Not Squamous Differentiation are a Reliable Indicator of CTNNB1 (β-catenin) Mutations in Endometrial Carcinoma and Precancers. Am. J. Surg. Pathol. 2022, 46, 1447–1455. [Google Scholar] [CrossRef] [PubMed]
- Li, H.D.; Lu, C.; Zhang, H.; Hu, Q.; Zhang, J.; Cuevas, I.C.; Sahoo, S.S.; Aguilar, M.; Maurais, E.G.; Zhang, S.; et al. A PoleP286R mouse model of endometrial cancer recapitulates high mutational burden and immunotherapy response. JCI Insight 2020, 5, e138829. [Google Scholar] [CrossRef]
- Hecht, J.L.; Mutter, G.L. Molecular and pathologic aspects of endometrial carcinogenesis. J. Clin. Oncol. 2006, 24, 4783–4791. [Google Scholar] [CrossRef]
- Zighelboim, I.; Goodfellow, P.J.; Gao, F.; Gibb, R.K.; Powell, M.A.; Rader, J.S.; Mutch, D.G. Microsatellite instability and epigenetic inactivation of MLH1 and outcome of patients with endometrial carcinomas of the endometrioid type. J. Clin. Oncol. 2007, 25, 2042–2048. [Google Scholar] [CrossRef]
- Simpkins, S.B.; Bocker, T.; Swisher, E.M.; Mutch, D.G.; Gersell, D.J.; Kovatich, A.J.; Palazzo, J.P.; Fishel, R.; Goodfellow, P.J. MLH1 promoter methylation and gene silencing is the primary cause of microsatellite instability in sporadic endometrial cancers. Hum. Mol. Genet. 1999, 8, 661–666. [Google Scholar] [CrossRef]
- Hampel, H.; Frankel, W.; Panescu, J.; Lockman, J.; Sotamaa, K.; Fix, D.; Comeras, I.; La Jeunesse, J.; Nakagawa, H.; Westman, J.A.; et al. Screening for Lynch syndrome (hereditary nonpolyposis colorectal cancer) among endometrial cancer patients. Cancer Res. 2006, 66, 7810–7817. [Google Scholar] [CrossRef] [PubMed]
- Okoye, E.I.; Bruegl, A.S.; Fellman, B.; Luthra, R.; Broaddus, R.R. Defective DNA Mismatch Repair Influences Expression of Endometrial Carcinoma Biomarkers. Int. J. Gynecol. Pathol. 2016, 35, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Lu, K.H.; Broaddus, R.R. Endometrial Cancer. N. Engl. J. Med. 2020, 383, 2053–2064. [Google Scholar] [CrossRef] [PubMed]
- Bartley, A.N.; Luthra, R.; Saraiya, D.S.; Urbauer, D.L.; Broaddus, R.R. Identification of cancer patients with Lynch syndrome: Clinically significant discordances and problems in tissue-based mismatch repair testing. Cancer Prev. Res. 2012, 5, 320–327. [Google Scholar] [CrossRef] [PubMed]
- Vierkoetter, K.R.; Kagami, L.A.; Ahn, H.J.; Shimizu, D.M.; Terada, K.Y. Loss of Mismatch Repair Protein Expression in Unselected Endometrial Adenocarcinoma Precursor Lesions. Int. J. Gynecol. Cancer 2016, 26, 228–232. [Google Scholar] [CrossRef] [PubMed]
- Aguilar, M.; Chen, H.; Sahoo, S.S.; Zheng, W.; Grubman, J.; SoRelle, J.A.; Lucas, E.; Castrillon, D.H. β-catenin, Pax2, and Pten Panel Identifies Precancers Among Histologically Subdiagnostic Endometrial Lesions. Am. J. Surg. Pathol. 2023, 47, 618–629. [Google Scholar] [CrossRef]
- Huvila, J.; Pors, J.; Thompson, E.F.; Gilks, C.B. Endometrial carcinoma: Molecular subtypes, precursors and the role of pathology in early diagnosis. J. Pathol. 2021, 253, 355–365. [Google Scholar] [CrossRef]
- Wiegand, K.C.; Lee, A.F.; Al-Agha, O.M.; Chow, C.; Kalloger, S.E.; Scott, D.W.; Steidl, C.; Wiseman, S.M.; Gascoyne, R.D.; Gilks, B.; et al. Loss of BAF250a (ARID1A) is frequent in high-grade endometrial carcinomas. J. Pathol. 2011, 224, 328–333. [Google Scholar] [CrossRef]
- Guan, B.; Mao, T.L.; Panuganti, P.K.; Kuhn, E.; Kurman, R.J.; Maeda, D.; Chen, E.; Jeng, Y.M.; Wang, T.L.; Shih, I.-M. Mutation and loss of expression of ARID1A in uterine low-grade endometrioid carcinoma. Am. J. Surg. Pathol. 2011, 35, 625–632. [Google Scholar] [CrossRef]
- Ayhan, A.; Mao, T.L.; Suryo Rahmanto, Y.; Zeppernick, F.; Ogawa, H.; Wu, R.C.; Wang, T.L.; Shih, I.-M. Increased proliferation in atypical hyperplasia/endometrioid intraepithelial neoplasia of the endometrium with concurrent inactivation of ARID1A and PTEN tumour suppressors. J. Pathol. Clin. Res. 2015, 1, 186–193. [Google Scholar] [CrossRef]
- Mao, T.L.; Ardighieri, L.; Ayhan, A.; Kuo, K.T.; Wu, C.H.; Wang, T.L.; Shih, I.-M. Loss of ARID1A expression correlates with stages of tumor progression in uterine endometrioid carcinoma. Am. J. Surg. Pathol. 2013, 37, 1342–1348. [Google Scholar] [CrossRef]
- Wang, Y.; Hoang, L.; Ji, J.X.; Huntsman, D.G. SWI/SNF Complex Mutations in Gynecologic Cancers: Molecular Mechanisms and Models. Annu. Rev. Pathol. 2020, 15, 467–492. [Google Scholar] [CrossRef]
- Raffone, A.; Travaglino, A.; Saccone, G.; Cieri, M.; Mascolo, M.; Mollo, A.; Insabato, L.; Zullo, F. Diagnostic and prognostic value of ARID1A in endometrial hyperplasia: A novel marker of occult cancer. APMIS 2019, 127, 597–606. [Google Scholar] [CrossRef]
- Georgescu, T.A.; Cirstoiu, M.; Costache, M.; Lazaroiu, A.; Dumitru, A.; Sajin, M. Histopathological, Immunohistochemical and Therapeutical Assessment of Premalignant Endometrial Lesions in a Hospital Based Series of Cases. Maedica 2016, 11, 115–121. [Google Scholar]
- Kobel, M.; Ronnett, B.M.; Singh, N.; Soslow, R.A.; Gilks, C.B.; McCluggage, W.G. Interpretation of P53 Immunohistochemistry in Endometrial Carcinomas: Toward Increased Reproducibility. Int. J. Gynecol. Pathol. 2019, 38 (Suppl. S1), S123–S131. [Google Scholar] [CrossRef] [PubMed]
- Deligdisch, L. Hormonal pathology of the endometrium. Mod. Pathol. 2000, 13, 285–294. [Google Scholar] [CrossRef] [PubMed]
- Baak, J.P.; Mutter, G.L.; Robboy, S.; van Diest, P.J.; Uyterlinde, A.M.; Orbo, A.; Palazzo, J.; Fiane, B.; Lovslett, K.; Burger, C.; et al. The molecular genetics and morphometry-based endometrial intraepithelial neoplasia classification system predicts disease progression in endometrial hyperplasia more accurately than the 1994 World Health Organization classification system. Cancer 2005, 103, 2304–2312. [Google Scholar] [CrossRef] [PubMed]
- Lucas, E.; Chen, H.; Sahoo, S.S.; Carrick, K.; Grubman, J.; Zheng, W.; Hecht, J.; Castrillon, D.H. β-Catenin, PAX2 and PTEN panel in the diagnosis of endometrial precancers: A case-based review. Diagn. Histopathol. 2023, 29, 468–482. [Google Scholar] [CrossRef]
- Wheeler, D.T.; Bristow, R.E.; Kurman, R.J. Histologic alterations in endometrial hyperplasia and well-differentiated carcinoma treated with progestins. Am. J. Surg. Pathol. 2007, 31, 988–998. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.R.; Ahn, H.J. Effects of Progesterone Treatment on the Squamous or Morular Metaplasia Associated with Endometrial Hyperplasia. J. Pathol. Transl. Med. 1996, 30, 680–686. [Google Scholar]
- Lin, M.C.; Lomo, L.; Baak, J.P.; Eng, C.; Ince, T.A.; Crum, C.P.; Mutter, G.L. Squamous morules are functionally inert elements of premalignant endometrial neoplasia. Mod. Pathol. 2009, 22, 167–174. [Google Scholar] [CrossRef]
- Nemejcova, K.; Kenny, S.L.; Laco, J.; Skapa, P.; Stanek, L.; Zikan, M.; Kleiblova, P.; McCluggage, W.G.; Dundr, P. Atypical Polypoid Adenomyoma of the Uterus: An Immunohistochemical and Molecular Study of 21 Cases. Am. J. Surg. Pathol. 2015, 39, 1148–1155. [Google Scholar] [CrossRef]
- Young, R.H.; Treger, T.; Scully, R.E. Atypical polypoid adenomyoma of the uterus. A report of 27 cases. Am. J. Clin. Pathol. 1986, 86, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Heatley, M.K. Atypical polypoid adenomyoma: A systematic review of the English literature. Histopathology 2006, 48, 609–610. [Google Scholar] [CrossRef] [PubMed]
- Biasioli, A.; Londero, A.P.; Orsaria, M.; Scrimin, F.; Mangino, F.P.; Bertozzi, S.; Mariuzzi, L.; Cagnacci, A. Atypical polypoid adenomyoma follow-up and management: Systematic review of case reports and series and meta-analysis. Medicine 2020, 99, e20491. [Google Scholar] [CrossRef] [PubMed]
- Raffone, A.; Travaglino, A.; Saccone, G.; Alviggi, C.; Mascolo, M.; De Placido, G.; Insabato, L.; Mollo, A.; Zullo, F. Management of women with atypical polypoid adenomyoma of the uterus: A quantitative systematic review. Acta Obstet. Gynecol. Scand. 2019, 98, 842–855. [Google Scholar] [CrossRef] [PubMed]
- Yoo, S.H.; Park, B.H.; Choi, J.; Yoo, J.; Lee, S.W.; Kim, Y.M.; Kim, K.R. Papillary mucinous metaplasia of the endometrium as a possible precursor of endometrial mucinous adenocarcinoma. Mod. Pathol. 2012, 25, 1496–1507. [Google Scholar] [CrossRef]
- Alomari, A.; Abi-Raad, R.; Buza, N.; Hui, P. Frequent KRAS mutation in complex mucinous epithelial lesions of the endometrium. Mod. Pathol. 2014, 27, 675–680. [Google Scholar] [CrossRef] [PubMed]
- Turashvili, G.; Childs, T. Mucinous metaplasia of the endometrium: Current concepts. Gynecol. Oncol. 2015, 136, 389–393. [Google Scholar] [CrossRef]
- Yoo, S.H. Papillary mucinous metaplasia: A distinct precursor of mucinous adenocarcinoma of the endometrium. Int. J. Clin. Exp. Pathol. 2022, 15, 83–87. [Google Scholar] [PubMed]
- Mutter, G.L.; Zaino, R.J.; Baak, J.P.; Bentley, R.C.; Robboy, S.J. Benign endometrial hyperplasia sequence and endometrial intraepithelial neoplasia. Int. J. Gynecol. Pathol. 2007, 26, 103–114. [Google Scholar] [CrossRef] [PubMed]



| Staining Characteristics | |||
|---|---|---|---|
| Markers | Normal Pattern | Aberrant Patterns in AH/EIN | Prevalence of Marker Aberrancy in AH/EIN |
| PAX2 | Strong and uniform nuclear staining. Note: loss of nuclear staining in scattered glands is common in normal endometrium, typically in <5% of entire sample, except in cases of endometrial polyp, where approximately 10–20% of cases show significant PAX2 loss. |
| ~70–80% |
| PTEN | Mainly cytoplasmic staining. Loss of expression in scattered glands is common in normal endometrium, typically in <5% of entire sample. |
| ~40–50% |
| β-catenin | Ubiquitously membranous staining, except in some cases of interval phase endometrium, where weak nuclear localization can be seen. |
| ~50% |
| ARID1A | Ubiquitously nuclear staining. |
| ~10% |
| Mismatch repair (MMR) proteins | Ubiquitously nuclear staining. |
| <5% |
| p53 | Variable proportion of tumor cell nuclei staining with variable intensity. |
| <3% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Niu, S.; Molberg, K.; Castrillon, D.H.; Lucas, E.; Chen, H. Biomarkers in the Diagnosis of Endometrial Precancers. Molecular Characteristics, Candidate Immunohistochemical Markers, and Promising Results of Three-Marker Panel: Current Status and Future Directions. Cancers 2024, 16, 1159. https://doi.org/10.3390/cancers16061159
Niu S, Molberg K, Castrillon DH, Lucas E, Chen H. Biomarkers in the Diagnosis of Endometrial Precancers. Molecular Characteristics, Candidate Immunohistochemical Markers, and Promising Results of Three-Marker Panel: Current Status and Future Directions. Cancers. 2024; 16(6):1159. https://doi.org/10.3390/cancers16061159
Chicago/Turabian StyleNiu, Shuang, Kyle Molberg, Diego H. Castrillon, Elena Lucas, and Hao Chen. 2024. "Biomarkers in the Diagnosis of Endometrial Precancers. Molecular Characteristics, Candidate Immunohistochemical Markers, and Promising Results of Three-Marker Panel: Current Status and Future Directions" Cancers 16, no. 6: 1159. https://doi.org/10.3390/cancers16061159
APA StyleNiu, S., Molberg, K., Castrillon, D. H., Lucas, E., & Chen, H. (2024). Biomarkers in the Diagnosis of Endometrial Precancers. Molecular Characteristics, Candidate Immunohistochemical Markers, and Promising Results of Three-Marker Panel: Current Status and Future Directions. Cancers, 16(6), 1159. https://doi.org/10.3390/cancers16061159






