Improved Accuracy and Sensitivity in Diagnosis and Staging of Lung Cancer with Systematic and Combined Endobronchial and Endoscopic Ultrasound (EBUS-EUS): Experience from a Tertiary Center
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Subjects
2.2. Procedures
2.3. Statistical Analysis
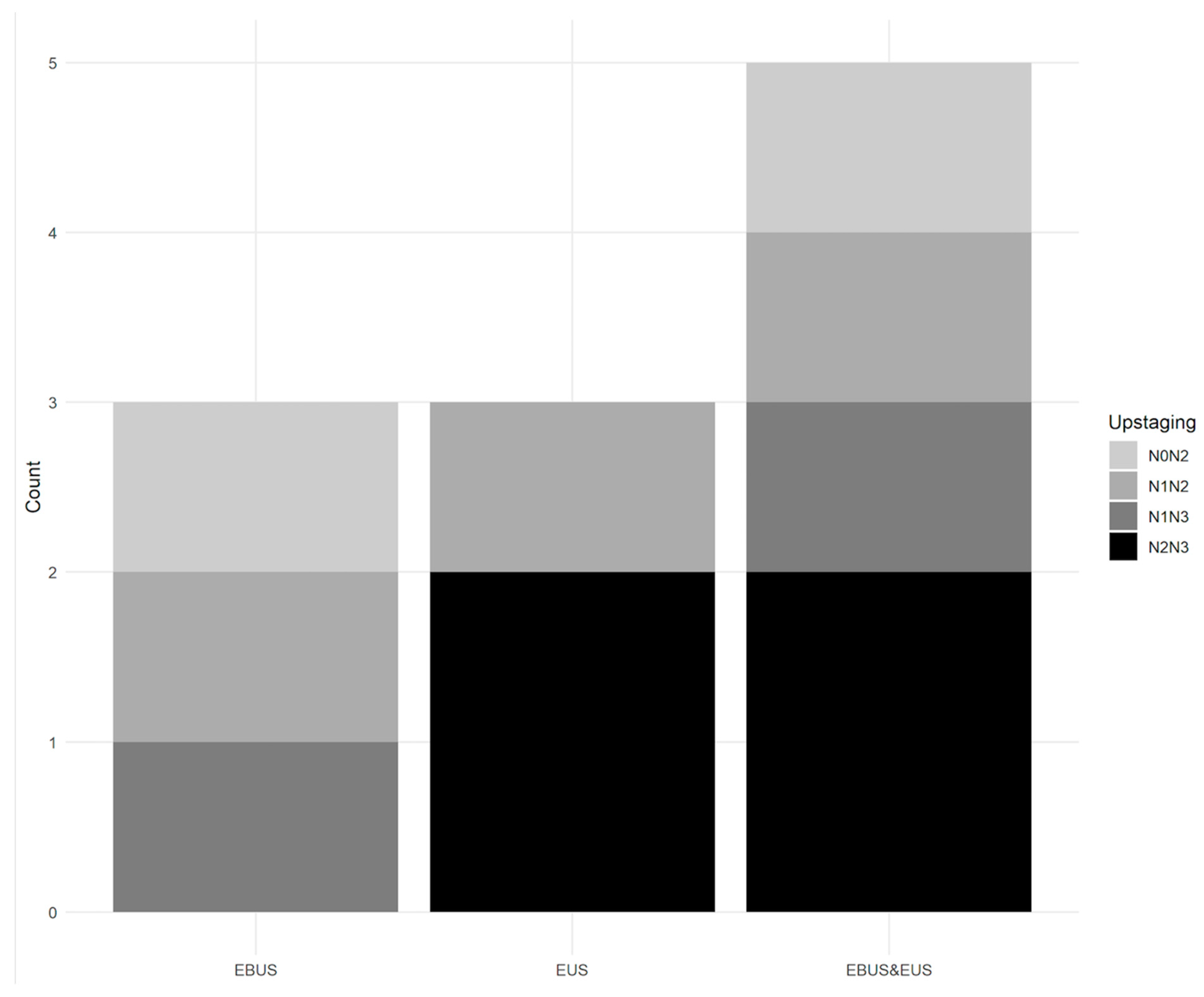
3. Results
4. Discussion
- Both techniques underestimate the N stage in case of malignant supraclavicular LNs (three patients in our series).
- As mentioned above, stations 2R and 4R are not routinely punctured with EUS-TA owing to their right and anterior locations with the interposition of the trachea, except when LNs are above 20 mm in size. In our series, we reached LNs in the 4R station with EUS-TA in nine patients, with diagnosis and staging obtained in eight patients. In one patient with an LN in the 2R station which measured more than 20 mm and was punctured with EUS-TA, the diagnosis obtained was confirmed by mediastinoscopy, but the staging was established with EBUS-TBNA and could not be obtained with EUS-TA because it was an 11R station (right interlobar station) specific to EBUS-TBNA. LNs in the 2R and 4R stations were reached, whatever the size, with EBUS-TBNA in 6 and 64 patients, respectively (Table 2).
- Optimal EUS-TA including fanning was not feasible for the 2R (one patient) and 4R (nine patients) stations, since there is an interposition of the trachea and, therefore, the path of the needle passes along the right edge of the trachea to reach these anterior mediastinal stations. In two series, the MLN in the 2R and 4R stations were only ones accessed with EUS-TA in one patient [13,14]. In another series of 110 patients, EUS-TA was carried out in 2R and 4R stations in 10 and 12 patients, respectively [11]. However, no details on the size of the MLNs, the constraints of EUS-TA in these stations, or their consequences on the diagnosis and staging were mentioned [11,12,13,14].
- In our series, EUS staging was, however, clearly disadvantaged when compared with EBUS staging in this population, since they were mostly patients with right pulmonary lesions and N2 statuses corresponding to a majority of right and anterior MLNs that were not easily accessible by EUS-TA (in 40 patients with N2 disease, 27 had a right pulmonary lesion) (Table 1).
- Other stations are not easy or impossible to access by EUS or EBUS, such as stations 5 (sub-aortic, pulmonary-aortic window) and 6 (para-aortic), owing to the anatomical constraints of the aortic arch. In our study, EUS-TA was performed in station 5 in two patients without traversing the aorta, but not in station 6. These stations are better accessed with video-assisted thoracic surgery (VATS), which can reach almost every mediastinal LN station, especially stations 5 and 6, by means of left VATS. LNs in stations 5 and 6 cannot be reached by routine mediastinoscopy. Some authors have described transaortic puncture of LNs in station 6 in patients without serious complications [17,18]. Molina et al. described transvascular EBUS or EUS puncture through the aorta and the pulmonary artery to reach inaccessible mediastinal and hilar LNs and lung lesions, with an overall sensitivity of 71.5% and accuracy of 74.5% for diagnosing malignancy [19]. One can reasonably wonder about the risk of hematogenous tumor seeding [17,18,19]. Another report by Liberman et al. showed an EUS technique to puncture LNs in station 6 without traversing the aorta and without complications [20]. We did not use this technique because it is not a routine procedure.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bade, B.C.; Dela Cruz, C.S. Lung Cancer 2020: Epidemiology, Etiology, and Prevention. Clin. Chest Med. 2020, 41, 1–24. [Google Scholar] [CrossRef] [PubMed]
- Vilmann, P.; Clementsen, P.F.; Colella, S.; Siemsen, M.; De Leyn, P.; Dumonceau, J.M.; Herth, F.J.; Larghi, A.; Vazquez-Sequeiros, E.; Hassan, C.; et al. Combined endobronchial and oesophageal endosonography for the diagnosis and staging of lung cancer. European Society of Gastrointestinal Endoscopy (ESGE) Guideline, in cooperation with the European Respiratory Society (ERS) and the European Society of Thoracic Surgeons (ESTS). Eur. Respir. J. 2015, 46, 40–60. [Google Scholar] [CrossRef] [PubMed]
- Vilmann, P.; Clementsen, P.F.; Colella, S.; Siemsen, M.; De Leyn, P.; Dumonceau, J.M.; Herth, F.J.; Larghi, A.; Vazquez-Sequeiros, E.; Hassan, C.; et al. Combined endobronchial and esophageal endosonography for the diagnosis and staging of lung cancer: European Society of Gastrointestinal Endoscopy (ESGE) Guideline, in cooperation with the European Respiratory Society (ERS) and the European Society of Thoracic Surgeons (ESTS). Endoscopy 2015, 47, c1. [Google Scholar] [CrossRef] [PubMed]
- Annema, J.T.; van Meerbeeck, J.P.; Rintoul, R.C.; Dooms, C.; Deschepper, E.; Dekkers, O.M.; De Leyn, P.; Braun, J.; Carroll, N.R.; Praet, M.; et al. Mediastinoscopy vs endosonography for mediastinal nodal staging of lung cancer: A randomized trial. JAMA 2010, 304, 2245–2252. [Google Scholar] [CrossRef] [PubMed]
- Annema, J.T.; Versteegh, M.I.; Veselic, M.; Welker, L.; Mauad, T.; Sont, J.K.; Willems, L.N.; Rabe, K.F. Endoscopic ultrasound added to mediastinoscopy for preoperative staging of patients with lung cancer. JAMA 2005, 294, 931–936. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; van Beek, E.J.; Murchison, J.T.; Marin, A.; Mirsadraee, S. The International Association for the Study of Lung Cancer Lymph Node Map: A Radiologic Atlas and Review. Tuberc. Respir. Dis. 2015, 78, 180–189. [Google Scholar] [CrossRef] [PubMed]
- Mountain, C.F.; Dresler, C.M. Regional lymph node classification for lung cancer staging. Chest 1997, 111, 1718–1723. [Google Scholar] [CrossRef] [PubMed]
- Rusch, V.W.; Asamura, H.; Watanabe, H.; Giroux, D.J.; Rami-Porta, R.; Goldstraw, P.; Members of I.S.C. The IASLC lung cancer staging project: A proposal for a new international lymph node map in the forthcoming seventh edition of the TNM classification for lung cancer. J. Thorac. Oncol. 2009, 4, 568–577. [Google Scholar] [CrossRef]
- De Leyn, P.; Dooms, C.; Kuzdzal, J.; Lardinois, D.; Passlick, B.; Rami-Porta, R.; Turna, A.; Van Schil, P.; Venuta, F.; Waller, D.; et al. Revised ESTS guidelines for preoperative mediastinal lymph node staging for non-small-cell lung cancer. Eur. J. Cardiothorac. Surg. 2014, 45, 787–798. [Google Scholar] [CrossRef]
- Wallace, M.B.; Pascual, J.M.; Raimondo, M.; Woodward, T.A.; McComb, B.L.; Crook, J.E.; Johnson, M.M.; Al-Haddad, M.A.; Gross, S.A.; Pungpapong, S.; et al. Minimally invasive endoscopic staging of suspected lung cancer. JAMA 2008, 299, 540–546. [Google Scholar] [CrossRef]
- Ohnishi, R.; Yasuda, I.; Kato, T.; Tanaka, T.; Kaneko, Y.; Suzuki, T.; Yasuda, S.; Sano, K.; Doi, S.; Nakashima, M.; et al. Combined endobronchial and endoscopic ultrasound-guided fine needle aspiration for mediastinal nodal staging of lung cancer. Endoscopy 2011, 43, 1082–1089. [Google Scholar] [CrossRef] [PubMed]
- Zhang, R.; Ying, K.; Shi, L.; Zhang, L.; Zhou, L. Combined endobronchial and endoscopic ultrasound-guided fine needle aspiration for mediastinal lymph node staging of lung cancer: A meta-analysis. Eur. J. Cancer 2013, 49, 1860–1867. [Google Scholar] [CrossRef] [PubMed]
- Oki, M.; Saka, H.; Ando, M.; Kitagawa, C.; Kogure, Y.; Seki, Y. Endoscopic ultrasound-guided fine needle aspiration and endobronchial ultrasound-guided transbronchial needle aspiration: Are two better than one in mediastinal staging of non-small cell lung cancer? J. Thorac. Cardiovasc. Surg. 2014, 148, 1169–1177. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lee, K.J.; Suh, G.Y.; Chung, M.P.; Kim, H.; Kwon, O.J.; Han, J.; Um, S.W. Combined endobronchial and transesophageal approach of an ultrasound bronchoscope for mediastinal staging of lung cancer. PLoS ONE 2014, 9, e91893. [Google Scholar] [CrossRef] [PubMed]
- Crombag, L.M.M.; Dooms, C.; Stigt, J.A.; Tournoy, K.G.; Schuurbiers, O.C.J.; Ninaber, M.K.; Buikhuisen, W.A.; Hashemi, S.M.S.; Bonta, P.I.; Korevaar, D.A.; et al. Systematic and combined endosonographic staging of lung cancer (SCORE study). Eur. Respir. J. 2019, 53, 1800800. [Google Scholar] [CrossRef] [PubMed]
- Nagula, S.; Pourmand, K.; Aslanian, H.; Bucobo, J.C.; Gonda, T.A.; Gonzalez, S.; Goodman, A.; Gross, S.A.; Ho, S.; DiMaio, C.J.; et al. Comparison of Endoscopic Ultrasound-Fine-Needle Aspiration and Endoscopic Ultrasound-Fine-Needle Biopsy for Solid Lesions in a Multicenter, Randomized Trial. Clin. Gastroenterol. Hepatol. 2018, 16, 1307–1313.e1301. [Google Scholar] [CrossRef] [PubMed]
- von Bartheld, M.B.; Rabe, K.F.; Annema, J.T. Transaortic EUS-guided FNA in the diagnosis of lung tumors and lymph nodes. Gastrointest. Endosc. 2009, 69, 345–349. [Google Scholar] [CrossRef]
- Wallace, M.B.; Woodward, T.A.; Raimondo, M.; Al-Haddad, M.; Odell, J.A. Transaortic fine-needle aspiration of centrally located lung cancer under endoscopic ultrasound guidance: The final frontier. Ann. Thorac. Surg. 2007, 84, 1019–1021. [Google Scholar] [CrossRef]
- Molina, J.C.; Chaudry, F.; Menezes, V.; Ferraro, P.; Lafontaine, E.; Martin, J.; Nasir, B.; Liberman, M. Transvascular endosonographic-guided needle biopsy of intrathoracic lesions. J. Thorac. Cardiovasc. Surg. 2020, 159, 2057–2065. [Google Scholar] [CrossRef]
- Liberman, M.; Duranceau, A.; Grunenwald, E.; Martin, J.; Thiffault, V.; Khereba, M.; Ferraro, P. New technique performed by using EUS access for biopsy of para-aortic (station 6) mediastinal lymph nodes without traversing the aorta (with video). Gastrointest. Endosc. 2011, 73, 1048–1051. [Google Scholar] [CrossRef]
- Pai, K.R.; Page, R.D. Mediastinitis after EUS-guided FNA biopsy of a posterior mediastinal metastatic teratoma. Gastrointest. Endosc. 2005, 62, 980–981. [Google Scholar] [CrossRef]
- Wildi, S.M.; Hoda, R.S.; Fickling, W.; Schmulewitz, N.; Varadarajulu, S.; Roberts, S.S.; Ferguson, B.; Hoffman, B.J.; Hawes, R.H.; Wallace, M.B. Diagnosis of benign cysts of the mediastinum: The role and risks of EUS and FNA. Gastrointest. Endosc. 2003, 58, 362–368. [Google Scholar] [CrossRef]
- von Bartheld, M.B.; Annema, J.T. Endosonography-related mortality and morbidity for pulmonary indications: A nationwide survey in the Netherlands. Gastrointest. Endosc. 2015, 82, 1009–1015. [Google Scholar] [CrossRef] [PubMed]
- von Bartheld, M.B.; van Breda, A.; Annema, J.T. Complication rate of endosonography (endobronchial and endoscopic ultrasound): A systematic review. Respiration 2014, 87, 343–351. [Google Scholar] [CrossRef] [PubMed]
- Korevaar, D.A.; Colella, S.; Spijker, R.; Bossuyt, P.M.; Konge, L.; Clementsen, P.F.; Annema, J.T. Esophageal Endosonography for the Diagnosis of Intrapulmonary Tumors: A Systematic Review and Meta-Analysis. Respiration 2017, 93, 126–137. [Google Scholar] [CrossRef] [PubMed]
- Micames, C.G.; McCrory, D.C.; Pavey, D.A.; Jowell, P.S.; Gress, F.G. Endoscopic ultrasound-guided fine-needle aspiration for non-small cell lung cancer staging: A systematic review and metaanalysis. Chest 2007, 131, 539–548. [Google Scholar] [CrossRef] [PubMed]
- Caglayan, B.; Yilmaz, A.; Bilaceroglu, S.; Comert, S.S.; Demirci, N.Y.; Salepci, B. Complications of Convex-Probe Endobronchial Ultrasound-Guided Transbronchial Needle Aspiration: A Multi-Center Retrospective Study. Respir. Care 2016, 61, 243–248. [Google Scholar] [CrossRef] [PubMed]
- Hirdes, M.M.; Schwartz, M.P.; Tytgat, K.M.; Schlosser, N.J.; Sie-Go, D.M.; Brink, M.A.; Oldenburg, B.; Siersema, P.D.; Vleggaar, F.P. Performance of EUS-FNA for mediastinal lymphadenopathy: Impact on patient management and costs in low-volume EUS centers. Surg. Endosc. 2010, 24, 2260–2267. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Postmus, P.E.; Kerr, K.M.; Oudkerk, M.; Senan, S.; Waller, D.A.; Vansteenkiste, J.; Escriu, C.; Peters, S.; Committee, E.G. Early and locally advanced non-small-cell lung cancer (NSCLC): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2017, 28, iv1–iv21. [Google Scholar] [CrossRef] [PubMed]
- Ettinger, D.S.; Wood, D.E.; Aisner, D.L.; Akerley, W.; Bauman, J.R.; Bharat, A.; Bruno, D.S.; Chang, J.Y.; Chirieac, L.R.; D’Amico, T.A.; et al. Non-Small Cell Lung Cancer, Version 3.2022, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Canc Netw. 2022, 20, 497–530. [Google Scholar] [CrossRef]
- Zhong, W.Z.; Liu, S.Y.; Wu, Y.L. Numbers or Stations: From Systematic Sampling to Individualized Lymph Node Dissection in Non-Small-Cell Lung Cancer. J. Clin. Oncol. 2017, 35, 1143–1145. [Google Scholar] [CrossRef] [PubMed]
- Sharples, L.D.; Jackson, C.; Wheaton, E.; Griffith, G.; Annema, J.T.; Dooms, C.; Tournoy, K.G.; Deschepper, E.; Hughes, V.; Magee, L.; et al. Clinical effectiveness and cost-effectiveness of endobronchial and endoscopic ultrasound relative to surgical staging in potentially resectable lung cancer: Results from the ASTER randomised controlled trial. Health Technol. Assess. 2012, 16, 1–75, iii–iv. [Google Scholar] [CrossRef] [PubMed]

| Number of patients | 141 | ||
| Age, median (range), years | 66 (47–85) | ||
| Sex ratio M/F | 105/36 | ||
| Primary lesion location (including 6 patients with 2 pulmonary lesions) | |||
| Right upper lobe | 43 | ||
| Right middle lobe | 7 | ||
| Right lower lobe | 39 | ||
| Left upper lobe | 34 | ||
| Left lower lobe | 24 | ||
| Histological findings (combined EBUS-TBNA-EUS-TA) | |||
| NSCLC | 85 | ||
| Adenocarcinoma | 48 | ||
| Squamous cell carcinoma (SCC) | 29 | ||
| Indeterminate carcinoma | 8 | ||
| NOS | 4 | ||
| Little differentiated | 4 | ||
| SCLC | 17 | ||
| Composite lung cancer (SCC and SCLC) | 1 | ||
| Neuroendocrine tumor | 1 | ||
| Benign lesions | 37 | ||
| Final staging (n = 82 patients) | |||
| Combined EBUS-TBNA and EUS-TA | Mediastinoscopy/SLA/Follow-up | ||
| N0 | 35 | N0 | 26 |
| N1 | 2 | N1 | 2 |
| N2 | 34 | N2 | 40 |
| N3 | 11 | N3 | 14 |
| Proportion of right/left pulmonary lesions in N2 population | 27/13 | ||
| Stations | 2R | 2L | 3 | 4R | 4L | 5 | 7 | 8 | 9 | 10R | 10L | 11R | 11L | Lung Mass | LAG * | LL ** |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| EBUS-TBNA | 6 | 1 | 1 (3p) | 64 | 19 | 87 | 14 | 5 | 26 | 17 | 4 | |||||
| EUS-TA | 1 | 5 | 3 (3p) | 9 | 49 | 2 | 94 | 9 | 3 | 6 | 21 | 1 |
| Tests | EBUS-TBNA | EUS-TA | Combined EBUS-TBNA and EUS-TA |
|---|---|---|---|
| Sensitivity *, % (95% CI) | 75 [66–83] | 87 [79–93] | 93 [86–97] |
| Specificity, % (95% CI) | 100 [90–100] | 100 [91–100] | 100 [89–100] |
| Accuracy, % (95% CI) | 82 [74–88] | 91 [85–95] | 94 [89–98] |
| PPV, % (95% CI) | 100 [95–100] | 100 [96–100] | 100 [96–100] |
| NPV, % (95% CI) | 58 [45–70] | 75 [61–86] | 80 [64–91] |
| Tests | EBUS-TBNA | EUS-TA | Combined EBUS-TBNA and EUS-TA |
|---|---|---|---|
| Sensitivity *, % (95% CI) | 62 [49–75] | 54 [40–67] | 79 [66–88] |
| Specificity, % (95% CI) | 100 [87–100] | 100 [87–100] | 100 [87–100] |
| Accuracy, % (95% CI) | 74 [64–83] | 68 [57–78] | 85 [76–92] |
| PPV, % (95% CI) | 100 [90–100] | 100 [88–100] | 100 [92–100] |
| NPV, % (95% CI) | 55 [40–70] | 50 [36–64] | 68 [51–82] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Badaoui, A.; De Wergifosse, M.; Rondelet, B.; Deprez, P.H.; Stanciu-Pop, C.; Bairy, L.; Eucher, P.; Delos, M.; Ocak, S.; Gillain, C.; et al. Improved Accuracy and Sensitivity in Diagnosis and Staging of Lung Cancer with Systematic and Combined Endobronchial and Endoscopic Ultrasound (EBUS-EUS): Experience from a Tertiary Center. Cancers 2024, 16, 728. https://doi.org/10.3390/cancers16040728
Badaoui A, De Wergifosse M, Rondelet B, Deprez PH, Stanciu-Pop C, Bairy L, Eucher P, Delos M, Ocak S, Gillain C, et al. Improved Accuracy and Sensitivity in Diagnosis and Staging of Lung Cancer with Systematic and Combined Endobronchial and Endoscopic Ultrasound (EBUS-EUS): Experience from a Tertiary Center. Cancers. 2024; 16(4):728. https://doi.org/10.3390/cancers16040728
Chicago/Turabian StyleBadaoui, Abdenor, Marion De Wergifosse, Benoit Rondelet, Pierre H. Deprez, Claudia Stanciu-Pop, Laurent Bairy, Philippe Eucher, Monique Delos, Sebahat Ocak, Cédric Gillain, and et al. 2024. "Improved Accuracy and Sensitivity in Diagnosis and Staging of Lung Cancer with Systematic and Combined Endobronchial and Endoscopic Ultrasound (EBUS-EUS): Experience from a Tertiary Center" Cancers 16, no. 4: 728. https://doi.org/10.3390/cancers16040728
APA StyleBadaoui, A., De Wergifosse, M., Rondelet, B., Deprez, P. H., Stanciu-Pop, C., Bairy, L., Eucher, P., Delos, M., Ocak, S., Gillain, C., Duplaquet, F., & Pirard, L. (2024). Improved Accuracy and Sensitivity in Diagnosis and Staging of Lung Cancer with Systematic and Combined Endobronchial and Endoscopic Ultrasound (EBUS-EUS): Experience from a Tertiary Center. Cancers, 16(4), 728. https://doi.org/10.3390/cancers16040728





