Systematic Review of Preoperative Prognostic Biomarkers in Perihilar Cholangiocarcinoma
Abstract
Simple Summary
Abstract
1. Introduction
2. Methods
2.1. Search Strategy
2.2. Study Selection
2.3. Data Extraction
3. Results
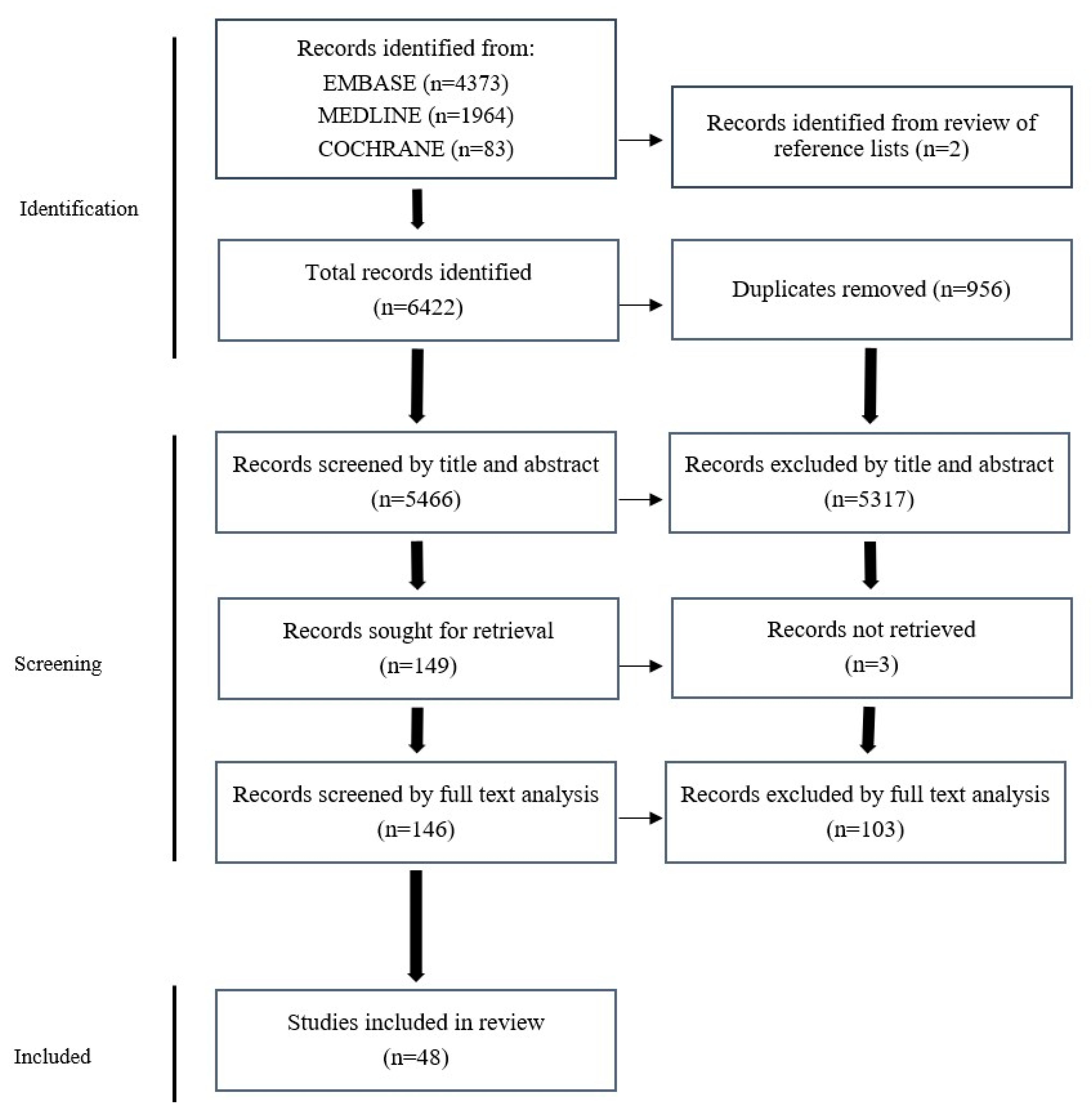
3.1. Study Selection
3.2. Adherence to REMARK Guidelines
3.3. Biomarkers Evaluated
3.4. Serum CA19-9
3.5. Serum Bilirubin
3.6. Serum Albumin
3.7. Serum CEA
3.8. Neutrophil-to-Lymphocyte Ratio (NLR)
3.9. Platelet-to-Lymphocyte Ratio (PLR)
3.10. Tumour Matrix Metalloproteinase-9 (MMP9)
3.11. Molecular Biomarkers Evaluated by Single Studies
3.12. High Mobility Group AT-Hook 2 (HMGA2)
3.13. Mucin 5AC and 6 (MUC5AC and MUC6)
3.14. Isocitrate Dehydrogenase 1 (IDH1)
3.15. PIWI-like-Protein 2 (PIWIL2)
3.16. DNA Index
3.17. Ribosomal Protein L34 (RPL34)
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Appendix A. Keywords and MeSH Terms Used in Embase Search
| 1. | exp bile duct/ |
| 2. | biliary tra*.mp. |
| 3. | bile duct*.mp. |
| 4. | cholang*.mp. |
| 5. | 1 or 2 or 3 or 4 |
| 6. | exp malignant neoplasm/ |
| 7. | (cancer* or tum?r or carcinoma* or adenocarcinoma* or cholangiocarcinoma*).mp. |
| 8. | malignan*.mp. |
| 9. | 6 or 7 or 8 |
| 10. | surgery/or surgery.mp. or cancer surgery/ |
| 11. | resect*.mp. |
| 12. | hepatectomy.mp. or liver resection/ |
| 13. | (pancreaticoduodenectomy or pancreatoduodenectomy).mp. or pancreaticoduodenectomy/ |
| 14. | (whipple* or hepatopancreaticoduodenectomy* or hepatopancreatoduodenectomy).mp. |
| 15. | 10 or 11 or 12 or 13 or 14 |
| 16. | biomarker*.mp. or biological marker/ |
| 17. | (blood test* or plasma* or serum*).mp. |
| 18. | urin*.mp. |
| 19. | urine sampling/ |
| 20. | immunohistochemistry/or immunohistoch*.mp. |
| 21. | protein expression/or immunofluorescence/or immunofluoresc*.mp. |
| 22. | 16 or 17 or 18 or 19 or 20 or 21 |
| 23. | recurren*.mp. |
| 24. | recurrent disease/ |
| 25. | exp survival/ |
| 26. | surviv*.mp. |
| 27. | prognosis/or cancer prognosis/or prognos*.mp. |
| 28. | 23 or 24 or 25 or 26 or 27 |
| 29. | 5 and 9 and 15 and 22 and 28 |
Appendix B. Modified REMARK Criteria Used to Evaluate Study Quality
| 1 | Cohort Overview: The cohort of the study is well-defined with regard to how the cohort was recruited and details regarding the diagnosis and treatment of the patients. |
| 2 | Clinical Data: Basic clinical data are provided, including the age, gender, clinical stage, and histopathologic grade of the cohort. |
| 3 | Test Protocol: For biomarkers not commonly tested in a hospital setting, a detailed protocol for testing the biomarker is provided or referred to. |
| 4 | Prognostic Endpoints: The endpoints used for prognostic analysis, such as overall survival or recurrence-free survival, are clearly stated. |
| 5 | Statistics: Appropriate statistical analysis is performed to adjust the estimation of the effect of the biomarker for known prognostic factors. |
| 6 | Classical Prognostic Factors: The prognostic impact of classical prognostic factors is reported, and the relationship between the evaluated and classical factors is described. |
References
- Banales, J.M.; Marin, J.J.G.; Lamarca, A.; Rodrigues, P.M.; Khan, S.A.; Roberts, L.R.; Cardinale, V.; Carpino, G.; Andersen, J.B.; Braconi, C.; et al. Cholangiocarcinoma 2020: The next horizon in mechanisms and management. Nat. Rev. Gastroenterol. Hepatol. 2020, 17, 557–588. [Google Scholar] [CrossRef] [PubMed]
- Nooijen, L.E.; Swijnenburg, R.J.; Klümpen, H.J.; Verheij, J.; Kazemier, G.; van Gulik, T.M.; Erdmann, J.I. Surgical Therapy for Perihilar Cholangiocarcinoma: State of the Art. Visc. Med. 2021, 37, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, P.M.; Vogel, A.; Arrese, M.; Balderramo, D.C.; Valle, J.W.; Banales, J.M. Next-Generation Biomarkers for Cholangiocarcinoma. Cancers 2021, 13, 3222. [Google Scholar] [CrossRef]
- Tian, Y.; Wen, N.; Li, B.; Lu, J.; Wang, Y.; Wang, S.; Cheng, N. A meta-analysis of prognostic factors for early recurrence in perihilar cholangiocarcinoma after curative-intent resection. Eur. J. Surg. Oncol. 2023, 49, 106982. [Google Scholar] [CrossRef] [PubMed]
- Takahara, N.; Nakai, Y.; Isayama, H.; Sasaki, T.; Saito, K.; Noguchi, K.; Suzuki, T.; Nakamura, T.; Sato, T.; Ishigaki, K.; et al. CA19-9 kinetics during systemic chemotherapy in patients with advanced or recurrent biliary tract cancer. Cancer Chemother. Pharmacol. 2017, 80, 1105–1112. [Google Scholar] [CrossRef] [PubMed]
- Doğan, Ü.B.; Gümürdülü, Y.; Gölge, N.; Kara, B. Relationship of CA 19-9 with choledocholithiasis and cholangitis. Turk. J. Gastroenterol. 2011, 22, 171–177. [Google Scholar] [CrossRef] [PubMed]
- Ruys, A.T.M.D.P.; Groot Koerkamp, B.M.D.P.; Wiggers, J.K.M.D.; Klümpen, H.-j.M.D.P.; Ten Kate, F.J.M.D.P.; van Gulik, T.M.M.D.P. Prognostic Biomarkers in Patients with Resected Cholangiocarcinoma: A Systematic Review and Meta-analysis. Ann. Surg. Oncol. 2014, 21, 487–500. [Google Scholar] [CrossRef]
- Pavicevic, S.; Reichelt, S.; Uluk, D.; Lurje, I.; Engelmann, C.; Modest, D.P.; Pelzer, U.; Krenzien, F.; Raschzok, N.; Benzing, C.; et al. Prognostic and Predictive Molecular Markers in Cholangiocarcinoma. Cancers 2022, 14, 1026. [Google Scholar] [CrossRef]
- Altman, D.G.; McShane, L.M.; Sauerbrei, W.; Taube, S.E. Reporting Recommendations for Tumor Marker Prognostic Studies (REMARK): Explanation and elaboration. PLoS Med. 2012, 9, e1001216. [Google Scholar] [CrossRef]
- Almangush, A.; Heikkinen, I.; Mäkitie, A.A.; Coletta, R.D.; Läärä, E.; Leivo, I.; Salo, T. Prognostic biomarkers for oral tongue squamous cell carcinoma: A systematic review and meta-analysis. Br. J. Cancer 2017, 117, 856–866. [Google Scholar] [CrossRef]
- Abdel Wahab, M.; Fathy, O.; Elghwalby, N.; Sultan, A.; Elebidy, E.; Abdalla, T.; Elshobary, M.; Mostafa, M.; Foad, A.; Kandeel, T.; et al. Resectability and prognostic factors after resection of hilar cholangiocarcinoma. Hepato-Gastroenterology 2006, 53, 5–10. [Google Scholar]
- Atanasov, G.; Hau, H.M.; Dietel, C.; Benzing, C.; Krenzien, F.; Brandl, A.; Wiltberger, G.; Matia, I.; Prager, I.; Schierle, K.; et al. Prognostic significance of macrophage invasion in hilar cholangiocarcinoma. BMC Cancer 2015, 15, 790. [Google Scholar] [CrossRef]
- Atanasov, G.; Hau, H.M.; Dietel, C.; Benzing, C.; Krenzien, F.; Brandl, A.; Englisch, J.P.; Wiltberger, G.; Schierle, K.; Robson, S.C.; et al. Prognostic significance of TIE2-expressing monocytes in hilar cholangiocarcinoma. J. Surg. Oncol. 2016, 114, 91–98. [Google Scholar] [CrossRef]
- Atanasov, G.; Dietel, C.; Feldbrugge, L.; Benzing, C.; Krenzien, F.; Brandl, A.; Katou, S.; Schierle, K.; Robson, S.C.; Splith, K.; et al. Angiogenic miRNAs, the angiopoietin axis and related TIE2- expressing monocytes affect outcomes in cholangiocarcinoma. Oncotarget 2018, 9, 29921–29933. [Google Scholar] [CrossRef]
- Bird, N.T.E.; Manu, N.; Quinn, L.; Needham, A.; Jones, R.; Fenwick, S.; Poston, G.; Palmer, D.; Malik, H. Evaluation of the utility of prognostic models for patients with resected hilar cholangiocarcinoma. HPB Off. J. Int. Hepato Pancreato Biliary Assoc. 2019, 21, 1376–1384. [Google Scholar] [CrossRef]
- Cai, W.K.; Lin, J.J.; He, G.H.; Wang, H.; Lu, J.H.; Yang, G.S. Preoperative serum CA19-9 levels is an independent prognostic factor in patients with resected hilar cholangiocarcinoma. Int. J. Clin. Exp. Pathol. 2014, 7, 7890–7898. [Google Scholar]
- Chen, P.; Li, B.; Zhu, Y.; Chen, W.; Liu, X.; Li, M.; Duan, X.; Yi, B.; Wang, J.; Liu, C.; et al. Establishment and validation of a prognostic nomogram for patients with resectable perihilar cholangiocarcinoma. Oncotarget 2016, 7, 37319–37330. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Huang, L.; Liang, J.; Cai, J.; Lei, Y.; Lai, J.; Liang, L.; Zhang, K. Characterizing the activation of the Wnt signaling pathway in hilar cholangiocarcinoma using a tissue microarray approach. Eur. J. Histochem. 2016, 60, 2536. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.J.; Xiong, X.F.; Wen, S.Q.; Tian, L.; Cheng, W.L.; Qi, Y.Q. Expression and clinical significance of PIWIL2 in hilar cholangiocarcinoma tissues and cell lines. Genet. Mol. Res. 2015, 14, 7053–7061. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Q.; Luo, X.; Zhang, B.; Jiang, X.; Yi, B.; Wu, M. Predictive factors for prognosis of hilar cholangiocarcinoma: Postresection radiotherapy improves survival. Eur. J. Surg. Oncol. 2007, 33, 202–207. [Google Scholar] [CrossRef] [PubMed]
- Dumitrascu, T.; Chirita, D.; Ionescu, M.; Popescu, I. Resection for hilar cholangiocarcinoma: Analysis of prognostic factors and the impact of systemic inflammation on long-term outcome. J. Gastrointest. Surg. 2013, 17, 913–924. [Google Scholar] [CrossRef] [PubMed]
- Fang, Z.; Lu, L.; Tian, Z.; Luo, K. Overexpression of phosphorylated 4E-binding protein 1 predicts lymph node metastasis and poor prognosis of Chinese patients with hilar cholangiocarcinoma. Med. Oncol. 2014, 31, 940. [Google Scholar] [CrossRef] [PubMed]
- Feng, F.; Wu, X.; Shi, X.; Gao, Q.; Wu, Y.; Yu, Y.; Cheng, Q.; Li, B.; Yi, B.; Liu, C.; et al. Comprehensive analysis of genomic alterations of Chinese hilar cholangiocarcinoma patients. Int. J. Clin. Oncol. 2021, 26, 717–727. [Google Scholar] [CrossRef] [PubMed]
- Hu, H.-J.; Mao, H.; Shrestha, A.; Tan, Y.-Q.; Ma, W.-J.; Yang, Q.; Wang, J.-K.; Cheng, N.-S.; Li, F.-Y. Prognostic factors and long-term outcomes of hilar cholangiocarcinoma: A single-institution experience in China. World J. Gastroenterol. 2016, 22, 2601–2610. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Chen, W.; Liang, P.; Hu, W.; Zhang, K.; Shen, S.; Chen, J.; Zhang, Z.; Chen, B.; Han, Y.; et al. Serum CYFRA 21-1 in Biliary Tract Cancers: A Reliable Biomarker for Gallbladder Carcinoma and Intrahepatic Cholangiocarcinoma. Dig. Dis. Sci. 2015, 60, 1273–1283. [Google Scholar] [CrossRef]
- Ishida, K.; Osakabe, M.; Eizuka, M.; Tai, S.; Sugimoto, R.; Fujita, Y.; Katagiri, H.; Takahara, T.; Uesugi, N.; Nitta, H.; et al. The expression of gastrointestinal differentiation markers in extrahepatic cholangiocarcinoma: Clinicopathological significance based on tumor location. Hum. Pathol. 2019, 92, 91–100. [Google Scholar] [CrossRef]
- Jun, S.Y.; An, S.; Huh, T.; Chung, J.Y.; Hong, S.M. Clinicopathological significance of olfactomedin-4 in extrahepatic bile duct carcinoma. Pathol. Res. Pract. 2020, 216, 152940. [Google Scholar] [CrossRef]
- Kamphues, C.; Al-Abadi, N.; Bova, R.; Rademacher, S.; Al-Abadi, H.; Klauschen, F.; Bahra, M.; Neuhaus, P.; Pratschke, J.; Seehofer, D. The DNA index as a prognostic tool in hilar cholangiocarcinoma. J. Surg. Oncol. 2015, 112, 214–218. [Google Scholar] [CrossRef]
- Kriegsmann, M.; Roessler, S.; Kriegsmann, K.; Renner, M.; Longuespee, R.; Albrecht, T.; Loeffler, M.; Singer, S.; Mehrabi, A.; Vogel, M.N.; et al. Programmed cell death ligand 1 (PD-L1, CD274) in cholangiocarcinoma—Correlation with clinicopathological data and comparison of antibodies. BMC Cancer 2019, 19, 72. [Google Scholar] [CrossRef]
- Kuriyama, N.; Usui, M.; Gyoten, K.; Hayasaki, A.; Fujii, T.; Iizawa, Y.; Kato, H.; Murata, Y.; Tanemura, A.; Kishiwada, M.; et al. Neoadjuvant chemotherapy followed by curative-intent surgery for perihilar cholangiocarcinoma based on its anatomical resectability classification and lymph node status. BMC Cancer 2020, 20, 405. [Google Scholar] [CrossRef]
- Li, B.; Lu, J.; Peng, D.Z.; Zhang, X.Y.; You, Z. Elevated platelet distribution width predicts poor prognosis in hilar cholangiocarcinoma. Medicine 2020, 99, e19400. [Google Scholar] [CrossRef] [PubMed]
- Li, O.; Yi, W.; Yang, P.; Guo, C.; Peng, C. Relationship between serum MMP-9 level and prognosis after radical resection for Hilar cholangiocarcinoma patients. Acta Cir. Bras. 2019, 34, e201900409. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Sun, R.; Zhang, X.; Qiu, B.; Chen, T.; Li, Z.; Xu, Y.; Zhang, Z. Transcription factor 7 promotes the progression of perihilar cholangiocarcinoma by inducing the transcription of c-Myc and FOS-like antigen 1. eBioMedicine 2019, 45, 181–191. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.F.; Zhao, R.; Guo, S.; Wang, X.Q.; Lian, P.L.; Chen, Y.G.; Xu, K.S. Expression and clinical significance of hepatoma-derived growth factor as a prognostic factor in human hilar cholangiocarcinoma. Ann. Surg. Oncol. 2011, 18, 872–879. [Google Scholar] [CrossRef] [PubMed]
- Nair, A.; Ingram, N.; Verghese, E.T.; Wijetunga, I.; Markham, A.F.; Wyatt, J.; Prasad, K.R.; Coletta, P.L. Neutrophil gelatinase-associated lipocalin as a theragnostic marker in perihilar cholangiocarcinoma. Anticancer Res. 2018, 38, 6737–6744. [Google Scholar] [CrossRef] [PubMed]
- Ning, S.; Guo, S.; Xie, J.; Xu, Y.; Lu, X.; Chen, Y. TROP2 correlates with microvessel density and poor prognosis in hilar cholangiocarcinoma. J. Gastrointest. Surg. 2013, 17, 360–368. [Google Scholar] [CrossRef]
- Okuno, M.; Ebata, T.; Yokoyama, Y.; Igami, T.; Sugawara, G.; Mizuno, T.; Yamaguchi, J.; Nagino, M. Evaluation of inflammation-based prognostic scores in patients undergoing hepatobiliary resection for perihilar cholangiocarcinoma. J. Gastroenterol. 2016, 51, 153–161. [Google Scholar] [CrossRef]
- Park, H.J.; Kim, K.; Paik, J.H.; Chie, E.K.; Kim, S.; Jang, J.Y.; Kim, S.W.; Han, S.W.; Oh, D.Y.; Im, S.A.; et al. Is c-Met oncoprotein expression an adverse prognosticator in extrahepatic bile duct cancer treated with curative resection followed by adjuvant chemoradiotherapy? Clin. Transl. Oncol. 2016, 18, 625–631. [Google Scholar] [CrossRef]
- Park, K.W.; Jung, E.S.; Kim, D.G.; Yoo, Y.K.; Hong, T.H.; Lee, I.S.; Koh, Y.H.; Kim, J.H.; Lee, M.A. ERCC1 can be a prognostic factor in hilar cholangiocarcinoma and extrahepatic bile duct cancer, but not in intrahepatic cholangiocarcinoma. Cancer Res. Treat. 2013, 45, 63–69. [Google Scholar] [CrossRef]
- Peng, D.; Lu, J.; Hu, H.; Li, B.; Ye, X.; Cheng, N. Lymphocyte to Monocyte Ratio Predicts Resectability and Early Recurrence of Bismuth-Corlette Type IV Hilar Cholangiocarcinoma. J. Gastrointest. Surg. 2020, 24, 330–340. [Google Scholar] [CrossRef] [PubMed]
- Qian, J.; Xu, L.; Yu, W.; Gu, X.; Zuo, Y.; Chen, Y.; Xie, F.; Wei, L. Ribosomal protein L34 is a potential prognostic biomarker and therapeutic target in hilar cholangiocarcinoma. Cell Biosci. 2020, 10, 100. [Google Scholar] [CrossRef]
- Ramacciato, G.; Nigri, G.; Bellagamba, R.; Petrucciani, N.; Ravaioli, M.; Cescon, M.; Del Gaudio, M.; Ercolani, G.; Di Benedetto, F.; Cautero, N.; et al. Univariate and multivariate analysis of prognostic factors in the surgical treatment of hilar cholangiocarcinoma. Am. Surg. 2010, 76, 1260–1268. [Google Scholar] [CrossRef]
- Ruzzenente, A.; Fassan, M.; Conci, S.; Simbolo, M.; Lawlor, R.T.; Pedrazzani, C.; Capelli, P.; D’Onofrio, M.; Iacono, C.; Scarpa, A.; et al. Cholangiocarcinoma Heterogeneity Revealed by Multigene Mutational Profiling: Clinical and Prognostic Relevance in Surgically Resected Patients. Ann. Surg. Oncol. 2016, 23, 1699–1707. [Google Scholar] [CrossRef] [PubMed]
- Saito, H.; Noji, T.; Okamura, K.; Tsuchikawa, T.; Shichinohe, T.; Hirano, S. A new prognostic scoring system using factors available preoperatively to predict survival after operative resection of perihilar cholangiocarcinoma. Surgery 2016, 159, 842–851. [Google Scholar] [CrossRef]
- Shimura, T.; Kofunato, Y.; Okada, R.; Yashima, R.; Koyama, Y.; Araki, K.; Kuwano, H.; Takenoshita, S. Intranuclear accumulation of galectin-3 is an independent prognostic factor for patients with distal cholangiocarcinoma. Oncol. Lett. 2017, 14, 819–829. [Google Scholar] [CrossRef][Green Version]
- Su, C.H.; Tsay, S.H.; Wu, C.C.; Shyr, Y.M.; King, K.L.; Lee, C.H.; Lui, W.Y.; Liu, T.J.; P’Eng, F.K. Factors influencing postoperative morbidity, mortality, and survival after resection for hilar cholangiocarcinoma. Ann. Surg. 1996, 223, 384–394. [Google Scholar] [CrossRef]
- Sun, Q.; Zhao, C.; Xia, L.; He, Z.; Lu, Z.; Liu, C.; Jia, M.; Wang, J.; Niu, J. High expression of matrix metalloproteinase-9 indicates poor prognosis in human hilar cholangiocarcinoma. Int. J. Clin. Exp. Pathol. 2014, 7, 6157–6164. [Google Scholar] [PubMed]
- Sun, Q.; Li, F.; Sun, F.; Niu, J. Interleukin-8 is a prognostic indicator in human hilar cholangiocarcinoma. Int. J. Clin. Exp. Pathol. 2015, 8, 8376–8384. [Google Scholar] [PubMed]
- Sun, Q.; Li, F.; Yu, S.; Zhang, X.; Shi, F.; She, J. Pontin Acts as a Potential Biomarker for Poor Clinical Outcome and Promotes Tumor Invasion in Hilar Cholangiocarcinoma. BioMed Res. Int. 2018, 2018, 6135016. [Google Scholar] [CrossRef] [PubMed]
- Sun, R.; Liu, Z.; Qiu, B.; Chen, T.; Li, Z.; Zhang, X.; Xu, Y.; Zhang, Z. Annexin10 promotes extrahepatic cholangiocarcinoma metastasis by facilitating EMT via PLA2G4A/PGE2/STAT3 pathway. eBioMedicine 2019, 47, 142–155. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.; Feng, Y.; Liu, H.; Shen, F.; Xiao, J.; Kang, X.; Zhao, Y.; Xiao, H.; Zhao, W.; Hu, X.; et al. Analysis of treatment methods and prognostic factors in 354 cases of hilar cholangiocarcinoma: A cohort study. J. Cancer Res. Ther. 2020, 16, 230–237. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, T.; Kawaji, H.; Murakawa, Y.; Hayashizaki, Y.; Murakami, T.; Yabushita, Y.; Homma, Y.; Kumamoto, T.; Matsuyama, R.; Endo, I. Significance of HMGA2 expression as independent poor prognostic marker in perihilar and distal cholangiocarcinoma resected with curative intent. Eur. J. Surg. Oncol. 2021, 47, 394–400. [Google Scholar] [CrossRef] [PubMed]
- Takihata, Y.; Einama, T.; Kobayashi, K.; Suzuki, T.; Yonamine, N.; Fujinuma, I.; Tsunenari, T.; Yamagishi, Y.; Iwasaki, T.; Miyata, Y.; et al. Different role of MSLN and CA125 co-expression as a prognostic predictor between perihilar and distal bile duct carcinoma. Oncol. Lett. 2021, 21, 414. [Google Scholar] [CrossRef] [PubMed]
- Thelen, A.; Scholz, A.; Benckert, C.; Schroder, M.; Weichert, W.; Wiedenmann, B.; Neuhaus, P.; Jonas, S. Microvessel density correlates with lymph node metastases and prognosis in hilar cholangiocarcinoma. J. Gastroenterol. 2008, 43, 959–966. [Google Scholar] [CrossRef] [PubMed]
- Urabe, K.; Murakami, Y.; Kondo, N.; Uemura, K.; Hashimoto, Y.; Nakagawa, N.; Sasaki, H.; Hiyama, E.; Takahashi, S.; Sueda, T. Nerve Growth Factor Expression Is Not Associated with Perineural Invasion in Extrahepatic Cholangiocarcinoma. Dig. Dis. Sci. 2016, 61, 774–784. [Google Scholar] [CrossRef] [PubMed]
- Wang, A.; He, Z.; Cong, P.; Qu, Y.; Hu, T.; Cai, Y.; Sun, B.; Chen, H.; Fu, W.; Peng, Y. Controlling Nutritional Status (CONUT) Score as a New Indicator of Prognosis in Patients With Hilar Cholangiocarcinoma Is Superior to NLR and PNI: A Single-Center Retrospective Study. Front. Oncol. 2020, 10, 593452. [Google Scholar] [CrossRef] [PubMed]
- Yoo, J.; Kim, J.H.; Bae, J.S.; Kang, H.J. Prediction of prognosis and resectability using MR imaging, clinical, and histopathological findings in patients with perihilar cholangiocarcinoma. Abdom. Radiol. 2021, 46, 4159–4169. [Google Scholar] [CrossRef]
- Zhao, J.; Zhang, W.; Zhang, J.; Chen, Y.T.; Ma, W.J.; Liu, S.Y.; Li, F.Y.; Song, B. Independent Risk Factors of Early Recurrence After Curative Resection for Perihilar Cholangiocarcinoma: Adjuvant Chemotherapy May Be Beneficial in Early Recurrence Subgroup. Cancer Manag. Res. 2020, 12, 13111–13123. [Google Scholar] [CrossRef]
- Liu, Y.; Lv, G.; Bai, J.; Song, L.; Ding, E.; Liu, L.; Tian, Y.; Chen, Q.; Li, K.; Liu, X.; et al. Effects of HMGA2 on the epithelial-mesenchymal transition-related genes in ACHN renal cell carcinoma cells-derived xenografts in nude mice. BMC Cancer 2022, 22, 421. [Google Scholar] [CrossRef]
- Babu, S.D.; Jayanthi, V.; Devaraj, N.; Reis, C.A.; Devaraj, H. Expression profile of mucins (MUC2, MUC5AC and MUC6) in Helicobacter pylori infected pre-neoplastic and neoplastic human gastric epithelium. Mol. Cancer 2006, 5, 10. [Google Scholar] [CrossRef]
- Yang, H.; Ye, D.; Guan, K.L.; Xiong, Y. IDH1 and IDH2 mutations in tumorigenesis: Mechanistic insights and clinical perspectives. Clin. Cancer Res. 2012, 18, 5562–5571. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Xu, L.; Bao, Z.; Xu, P.; Chang, H.; Wu, J.; Bei, Y.; Xia, L.; Wu, P.; Cui, G. High expression of PIWIL2 promotes tumor cell proliferation, migration and predicts a poor prognosis in glioma. Oncol. Rep. 2017, 38, 183–192. [Google Scholar] [CrossRef]
- Dey, P. Aneuploidy and malignancy: An unsolved equation. J. Clin. Pathol. 2004, 57, 1245–1249. [Google Scholar] [CrossRef] [PubMed]
- Luo, S.; Zhao, J.; Fowdur, M.; Wang, K.; Jiang, T.; He, M. Highly expressed ribosomal protein L34 indicates poor prognosis in osteosarcoma and its knockdown suppresses osteosarcoma proliferation probably through translational control. Sci. Rep. 2016, 6, 37690. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.; Teng, T.Z.J.; Shelat, V.G. Carbohydrate antigen 19-9—Tumor marker: Past, present, and future. World J. Gastrointest. Surg. 2020, 12, 468–490. [Google Scholar] [CrossRef]
- Juntermanns, B.; Radunz, S.; Heuer, M.; Hertel, S.; Reis, H.; Neuhaus, J.; Vernadakis, S.; Trarbach, T.; Paul, A.; Kaiser, G.M. Tumor markers as a diagnostic key for hilar cholangiocarcinoma. Eur. J. Med. Res. 2010, 15, 357–361. [Google Scholar] [CrossRef]
- Fang, T.; Wang, H.; Wang, Y.; Lin, X.; Cui, Y.; Wang, Z. Clinical Significance of Preoperative Serum CEA, CA125, and CA19-9 Levels in Predicting the Resectability of Cholangiocarcinoma. Dis. Markers 2019, 2019, 6016931. [Google Scholar] [CrossRef] [PubMed]
- Xiang, S.; Lau, W.Y.; Chen, X.P. Hilar cholangiocarcinoma: Controversies on the extent of surgical resection aiming at cure. Int. J. Color. Dis. 2015, 30, 159–171. [Google Scholar] [CrossRef]
- Marrelli, D.; Caruso, S.; Pedrazzani, C.; Neri, A.; Fernandes, E.; Marini, M.; Pinto, E.; Roviello, F. CA19-9 serum levels in obstructive jaundice: Clinical value in benign and malignant conditions. Am. J. Surg. 2009, 198, 333–339. [Google Scholar] [CrossRef]
- Yin, X.; Wu, L.; Yang, H.; Yang, H. Prognostic significance of neutrophil-lymphocyte ratio (NLR) in patients with ovarian cancer: A systematic review and meta-analysis. Medicine 2019, 98, e17475. [Google Scholar] [CrossRef]
- Zhou, X.; Du, Y.; Huang, Z.; Xu, J.; Qiu, T.; Wang, J.; Wang, T.; Zhu, W.; Liu, P. Prognostic value of PLR in various cancers: A meta-analysis. PLoS ONE 2014, 9, e101119. [Google Scholar] [CrossRef]
- Nahm, C.B.; Turchini, J.; Jamieson, N.; Moon, E.; Sioson, L.; Itchins, M.; Arena, J.; Colvin, E.; Howell, V.M.; Pavlakis, N.; et al. Biomarker panel predicts survival after resection in pancreatic ductal adenocarcinoma: A multi-institutional cohort study. Eur. J. Surg. Oncol. 2019, 45, 218–224. [Google Scholar] [CrossRef] [PubMed]
- van Keulen, A.M.; Olthof, P.B.; Cescon, M.; Guglielmi, A.; Jarnagin, W.R.; Nadalin, S.; Pratschke, J.; Ratti, F.; Troisi, R.I.; Groot Koerkamp, B.; et al. Actual 10-Year Survival after Resection of Perihilar Cholangiocarcinoma: What Factors Preclude a Chance for Cure? Cancers 2021, 13, 6260. [Google Scholar] [CrossRef]
- Tojima, Y.; Nagino, M.; Ebata, T.; Uesaka, K.; Kamiya, J.; Nimura, Y. Immunohistochemically demonstrated lymph node micrometastasis and prognosis in patients with otherwise node-negative hilar cholangiocarcinoma. Ann. Surg. 2003, 237, 201–207. [Google Scholar] [CrossRef]
- Nakamura, H.; Arai, Y.; Totoki, Y.; Shirota, T.; Elzawahry, A.; Kato, M.; Hama, N.; Hosoda, F.; Urushidate, T.; Ohashi, S.; et al. Genomic spectra of biliary tract cancer. Nat. Genet. 2015, 47, 1003–1010. [Google Scholar] [CrossRef] [PubMed]
- Chantrill, L.A.; Nagrial, A.M.; Watson, C.; Johns, A.L.; Martyn-Smith, M.; Simpson, S.; Mead, S.; Jones, M.D.; Samra, J.S.; Gill, A.J.; et al. Precision Medicine for Advanced Pancreas Cancer: The Individualized Molecular Pancreatic Cancer Therapy (IMPaCT) Trial. Clin. Cancer Res. 2015, 21, 2029–2037. [Google Scholar] [CrossRef]
- Gradishar, W.J.; Moran, M.S.; Abraham, J.; Abramson, V.; Aft, R.; Agnese, D.; Allison, K.H.; Anderson, B.; Burstein, H.J.; Chew, H.; et al. NCCN Guidelines® Insights: Breast Cancer, Version 4.2023. J. Natl. Compr. Cancer Netw. 2023, 21, 594–608. [Google Scholar] [CrossRef] [PubMed]
- Nahm, C.B.; Turchini, J.; Sahni, S.; Moon, E.; Itchins, M.; Arena, J.; Chou, A.; Colvin, E.K.; Howell, V.M.; Pavlakis, N.; et al. The Right Treatment Strategy for the Right Patient: A Biomarker-Driven Approach to Neoadjuvant vs. Surgery-First Management of Resectable and Borderline Resectable Pancreatic Cancer. Cancers 2022, 14, 3620. [Google Scholar] [CrossRef]
- D’Amico, A.V.; Chen, M.H.; Roehl, K.A.; Catalona, W.J. Preoperative PSA velocity and the risk of death from prostate cancer after radical prostatectomy. N. Engl. J. Med. 2004, 351, 125–135. [Google Scholar] [CrossRef]
| Authors | Biomarker | Cutoff | Detection Site | Detection Method | Total Participants with pCCA | Participants with Positive Biomarker | REMARK Score | Prognostic Significance (N/U/M) |
|---|---|---|---|---|---|---|---|---|
| Abdel Wahab et al., 2016 [11] | Albumin | not specified | Serum | not specified | 234 | not specified | 3/6 | N |
| Bilirubin | not specified | Serum | not specified | 234 | not specified | N | ||
| CA19-9 | not specified | Serum | not specified | 234 | not specified | M (OS) | ||
| Atanasov et al., 2016 [12] | TAM | >25% cell density | Tumour | IHC | 45 | 12 | 6/6 | U (OS) M (RFS) |
| Atanasov et al., 2016 [13] | TEM | expression score 2 | Tumour | IHC | 45 | 11 | 6/6 | M (OS) |
| Atanasov et al. 2018 [14] | miR-126 | not specified | Tumour | qPCR | 45 | 18 | 5/6 | U (OS) |
| Bird et al., 2019 [15] | CA19-9 | >46 U/ml | Serum | not specified | 56 | 22 | 5/6 | M (OS) |
| MLR | ≥3 | Serum | not specified | 56 | 31 | N | ||
| NLR | ≥3 | Serum | not specified | 56 | 23 | N | ||
| Cai et al., 2014 [16] | CA19-9 | >150 U/ml | Serum | not specified | 168 | 74 | 5/6 | M (OS) |
| Bilirubin | >10 mg/dL | Serum | not specified | 168 | 96 | N | ||
| Chen P et al., 2016 [17] | CA19-9 | 73.5–325 U/mL | Serum | not specified | 235 | 78 | 5/6 | M (OS) |
| CA19-9 | >325 U/ml | Serum | not specified | 235 | 79 | M (OS) | ||
| Chen W et al., 2015 [18] | Complete vs. partial Wnt pathway activation | Wnt2+/3+ and b-catenin + and TCF4+ vs. Wnt2+/3+ and b-catenin + or TCF4+ | Tumour | IHC | 129 | 101 | 4/6 | M (OS) |
| Chen YJ et al., 2015 [19] | PIWIL2 | expression score ≥ 4 | Tumour | IHC | 41 | 33 | 5/6 | M (OS + RFS) |
| Cheng et al., 2007 [20] | Bilirubin | >10 mg/dL | Serum | not specified | 75 | not specified | 5/6 | M (OS) |
| Dumitrascu et al., 2013 [21] | Albumin | >4 g/dL | Serum | not specified | 90 | not specified | 4/6 | U (OS + RFS) |
| Bilirubin | >10.4 mg/dl | Serum | not specified | 90 | not specified | U (OS + RFS) | ||
| CA19-9 | >200 U/mL | Serum | not specified | 90 | not specified | U (OS + RFS) | ||
| Haemoglobin | >12.5 mg/dL | Serum | not specified | 90 | not specified | U (OS + RFS) | ||
| Leukocyte count | >8000/mmc | Serum | not specified | 90 | not specified | U (OS + RFS) | ||
| NLR | >3.3 | Serum | not specified | 90 | not specified | U (OS) M (RFS) | ||
| TLR | >184 | Serum | not specified | 90 | not specified | U (OS + RFS) | ||
| Platelets | >312,000/mmc | Serum | not specified | 90 | not specified | U (OS + RFS) | ||
| Fang et al., 2014 [22] | P-4E-BP1 | >25% positive cells | Tumour | IHC | 61 | 31 | 5/6 | U (OS + RFS) |
| Feng et al., 2021 [23] | ARID1B | n/a | Tumour | NGS | 63 | 58 | 5/6 | M (RFS) |
| RBM10 | n/a | Tumour | NGS | 63 | 58 | N | ||
| Hu et al., 2016 [24] | CA19-9 | >100 U/mL | Serum | Not specified | 381 | not specified | 5/6 | U (OS + RFS) |
| Huang et al., 2015 [25] | CYFRA21-1 | >2.27 ng/mL | Serum | ECL | 31 | 22 | 5/6 | U (OS + RFS) |
| Ishida et al., 2019 [26] | MUC5A and MUC6 | <25% expression | Tumour | IHC | 30 | 13 | 6/6 | M (OS) |
| Jun et al., 2020 [27] | OLFM4 | Tumour | IHC | 54 | 14 | 5/6 | N | |
| Kamphues et al., 2015 [28] | DNA index | >1.5 | Tumour | Image cytometry | 154 | 71 | 5/6 | M (OS) |
| Kriegsmann et al., 2019 [29] | PD-L1 | >5% positive cells | Tumour | IHC | 57 | 3 | 5/6 | N |
| Kuriyama et al., 2020 [30] | CA19-9 | ≥25 U/ml | Serum | not specified | 49 | 35 | 6/6 | N |
| CEA | ≥8.5 ng/mL | Serum | not specified | 49 | 7 | M (OS) | ||
| Li et al., 2020 [31] | Albumin | >35 g/L | Blood | not specified | 292 | not specified | 5/6 | U (OS) |
| Mean Platelet Volume | >13 | Blood | not specified | 292 | not specified | U (OS) | ||
| Platelet Distribution Width | >16.55 | Blood | not specified | 292 | 121 | M (OS) | ||
| Platelets | >300 × 109 | Blood | not specified | 292 | not specified | N | ||
| Li et al., 2019 [32] | Bilirubin | >100 mg/L | Blood | not specified | 181 | not specified | 5/6 | N |
| MMP9 | >201.93 ng/mL | Blood | ELISA | 181 | not specified | M (OS) | ||
| Liu et al., 2019 [33] | TCF7 | not specified. Comparison of low vs. high | Tumour | IHC | 160 | 76 | 5/6 | M (OS) |
| Liu et al., 2011 [34] | VEGF | >25% staining | Tumour | IHC | 58 | 42 | 5/6 | M (OS) |
| HDFG | HDGF labelling index > 166.91 | Tumour | IHC | 58 | 27 | U (OS) | ||
| Nair et al., 2018 [35] | NGAL | >345 Histoscore | Tumour | IHC | 54 | not specified | 5/6 | N |
| Ning et al., 2013 [36] | TROP2 | Score > 4 | Tumour | IHC | 70 | 43 | 6/6 | M (OS) |
| Okuno et al., 2016 [37] | mGPS | mGPS ≥ 1 | Serum | not specified | 534 | 112 | 5/6 | M (OS) |
| NLR | ≥3 | Serum | not specified | 534 | 158 | N | ||
| PLR | ≥150 | Serum | not specified | 534 | 359 | N | ||
| PNI | ≥40 | Serum | not specified | 534 | 362 | N | ||
| Park et al., 2015 [38] | C-met | Staining ≥ 30% | Tumour | IHC | 53 | 19 | 5/6 | N |
| EGFR | Staining ≥ 30% | Tumour | IHC | 53 | not specified | N | ||
| VEGF | Staining ≥ 30% | Tumour | IHC | 53 | not specified | N | ||
| Park et al., 2013 [39] | ERCC1 | Staining > 10% | Tumour | IHC | 41 | 9 | 5/6 | N |
| Survivin | Staining > 10% | Tumour | IHC | 41 | 14 | U (OS) | ||
| TP | Staining > 10% | Tumour | IHC | 41 | 25 | N | ||
| TP53 | Staining > 10% | Tumour | IHC | 41 | 18 | N | ||
| Cyclin D1 | Staining > 10% | Tumour | IHC | 41 | 8 | N | ||
| Peng et al., 2020 [40] | LMRc | Postop LMR > preop LMR | Serum | not specified | 254 | 125 | 6/6 | U (OS) M (RFS) |
| Qian et al., 2020 [41] | RPL34 | Expression ≥ 75 | Tumour | IHC | 121 | 94 | 5/6 | M (OS + RFS) |
| Ramacciato et al., 2010 [42] | Albumin | Low < 3 g/dL | Serum | not specified | 30 | 21 | 4/6 | N |
| Bilirubin | >3 mg/dL | Serum | not specified | 30 | 11 | N | ||
| CA19-9 | >400 ng/mL | Serum | not specified | 30 | 17 | N | ||
| CEA | >2 U/L | Serum | not specified | 30 | 18 | N | ||
| Ruzzenente et al., 2016 [43] | ALK | n/a | Tumour | NGS | 18 | 1 | 5/6 | U (OS) |
| BRAF | n/a | Tumour | NGS | 18 | 1 | N | ||
| IDH | n/a | Tumour | NGS | 18 | 2 | M (OS) | ||
| KRAS | n/a | Tumour | NGS | 18 | 12 | N | ||
| PIK3CA | n/a | Tumour | NGS | 18 | 3 | N | ||
| PBRM1 | n/a | Tumour | NGS | 18 | 3 | N | ||
| TP53 | n/a | Tumour | NGS | 18 | 11 | M (OS) | ||
| Saito et al., 2016 [44] | Albumin | <3.5 mg/dL | Serum | not specified | 121 | 26 | 6/6 | M (OS) |
| CRP | >0.5 mg/dL | Tumour | not specified | 121 | 56 | M (OS) | ||
| CA19-9 | >300 U/mL | Tumour | not specified | 121 | 17 | U (OS) | ||
| CEA | >7 ng/mL | Tumour | not specified | 121 | 14 | M (OS) | ||
| PLR | >150 | Tumour | not specified | 121 | 53 | U (OS) | ||
| Shimura et al., 2017 [45] | Gal-3 | >50% staining | Tumour | IHC | 21 | 11 | 6/6 | N |
| Intranuclear Gal-3 | >5% intranuclear staining | Tumour | IHC | 21 | not specified | N | ||
| Su et al., 1996 [46] | ALT | >120 U/L | Serum | not specified | 44 | 13 | 5/6 | N |
| Albumin | <30 mg/L | Serum | not specified | 44 | 45 | N | ||
| AST | >135 U/L | Serum | not specified | 44 | 6 | N | ||
| Bilirubin | >10 mg/dL | Serum | not specified | 44 | 17 | M (OS) | ||
| Sun et al., 2014 [47] | MMP9 | >50% staining | Tumour | IHC | 58 | 27 | 6/6 | M (OS) |
| Sun Q et al., 2015 [48] | IL8 | median score—not specified | Tumour | IHC | 62 | 35 | 6/6 | M (OS) |
| MMP9 | >50% staining | Tumour | IHC | 62 | 29 | M (OS) | ||
| Sun Q et al., 2018 [49] | Pontin | >5% staining | Tumour | IHC | 86 | 34 | 5/6 | M (OS) |
| Sun R et al., 2019 [50] | ANXA10 | >5% staining | Tumour | IHC | 128 | not specified | 5/6 | M (OS) |
| Sun Z et al., 2020 [51] | Albumin | <35 g/L | Serum | not specified | 110 | 173 | 5/6 | M (OS) |
| ALT | ≥80 U/L | Serum | not specified | 110 | 225 | N | ||
| AST | ≥70 U/L | Serum | not specified | 110 | 202 | N | ||
| GGT | ≥90 U/L | Serum | not specified | 110 | 288 | N | ||
| Bilirubin | ≥4 mg/Dl | Serum | not specified | 110 | 242 | M (OS) | ||
| CRP | ≥5 mg/L | Serum | not specified | 110 | 189 | N | ||
| CA19-9 | >0.001 U/mL | Serum | not specified | 110 | not specified | N | ||
| CEA | ≥5 ng/mL | Serum | not specified | 110 | 71 | N | ||
| Takahashi et al., 2021 [52] | HMGA2 | >50% staining | Tumour | IHC | 41 | 21 | 6/6 | M (OS) |
| Takihata et al., 2021 [53] | CA125 and MSLN coexpression | >50% staining | Tumour | IHC | 31 | 15 | 5/6 | U (OS) |
| Thelen et al., 2008 [54] | CD31 | Average count > 20 | Tumour | IHC | 60 | 38 | 5/6 | M (OS) U (RFS) |
| Urabe et al., 2016 [55] | NGF | >30% | Tumour | IHC | 59 | 35 | 5/6 | N |
| Wang et al., 2020 [56] | CA19-9 | >37 ng/ml | Serum | not specified | 94 | not specified | 5/6 | U (OS) |
| CEA | >5 ng/mL | Serum | not specified | 94 | not specified | N | ||
| NLR | >3.6 | Serum | not specified | 94 | 51 | M (OS + RFS) | ||
| PNI | >43.7 | Serum | not specified | 94 | 50 | M (OS + RFS) | ||
| CONUT Score | >3 | Serum | not specified | 94 | 31 | M (OS + RFS) | ||
| Yoo et al., 2021 [57] | ALT | >40 U/L | Serum | not specified | 196 | not specified | 5/6 | N |
| AST | ≥40 U/L | Serum | not specified | 196 | not specified | N | ||
| ALP | >115 U/L | Serum | not specified | 196 | not specified | N | ||
| CA19-9 | >37 U/mL | Serum | not specified | 196 | not specified | M (OS) | ||
| CEA | >5 ng/ml | Serum | not specified | 196 | not specified | N | ||
| Zhao et al., 2020 [58] | Bilirubin | ≥142.4 µmol/L | Serum | not specified | 335 | 168 | 4/6 | M (OS) |
| CA19-9 | ≥1000 U/mL | Serum | not specified | 335 | 68 | U (OS) M (RFS) | ||
| CEA | ≥3.0 ng/mL | Serum | not specified | 335 | 168 | U (RFS) |
| Author, Year | Cutoff Value | No. of pCCA Resections | Endpoint | Univariable Analysis mOS Months, + vs. − or HR | Multivariable Analysis | Unfulfilled Modified REMARK Criteria |
|---|---|---|---|---|---|---|
| Serum CA19-9 | ||||||
| Abdel Wahab et al., 2016 [11] | CA 19-9 considered as continuous variable | 243 | OS | Significant (numbers not reported) | HR = 1.01 (1.01–1.02) p = 0.000 | 2: Clinical data 5: Statistics 6: Classical prognostic factors |
| Bird et al., 2019 [15] | >46 U/mL | 56 | OS | 41.3 vs. 66.0 mths p = 0.024 | HR = 3.24 (1.37–7.69) p = 0.007 | 2: Clinical data |
| Cai et al., 2014 [16] | >150 U/mL | 168 | OS | 22 vs. 44 mths p = 0.001 | HR = 2.23 (1.14–4.39) p = 0.020 | 2: Clinical data |
| Chen et al., 2016 [17] | >73.5 but <325 U/mL | 235 | OS | HR = 1.63 (1.14–2.32) p = 0.008 | (vs. <73.5 U/mL) HR = 1.70 (1.18–2.44) p = 0.004 | 2: Clinical data |
| ≥325 U/mL | 235 | OS | (vs. <73.5 U/mL) HR = 2.39 (1.68–3.41) p < 0.001 | HR = 2.30 (1.60–3.30) p < 0.001 | ||
| Dumitrascu et al., 2013 [21] | 200 U/mL | 90 | OS | 13 vs. 43 mths p < 0.001 | N | 2: Clinical data 6: Classical prognostic factors |
| RFS | 12 vs. 35 mths p = 0.004 | N | ||||
| Hu et al., 2016 [24] | 100 U/mL | 381 | OS | 23 vs. 39.7 mths p = 0.039 | N | 2: Clinical data |
| RFS | 16.7 vs. 23.6 mths p = 0.018 | N | ||||
| Kuriyama et al., 2020 [30] | 25 U/mL | 49 | OS | 49.4 mths vs. not reached p = 0.355 | NR | |
| Ramacciato et al., 2010 [42] | 400 ng/mL | 30 | OS | 16 vs. 19 mths p = 0.460 | NR | 2: Clinical data 5: Statistics |
| Saito et al., 2016 [44] | 300 U/mL | 121 | OS | 27.6 vs. 74.6 mths p = 0.003 | HR = 1.00 (0.46–2.17) p = 0.999 | |
| Sun Z et al., 2020 [51] | >0.001 U/L | 110 | OS | 12.1 vs. 13 mths p = 0.678 | NR | 2: Clinical data |
| Wang et al., 2020 [56] | 37 ng/mL | 94 | OS | HR = 2.02 (1.06–3.84) p = 0.032 | HR = 0.85 (0.39–1.87) p = 0.692 | 2: Clinical data |
| RFS | HR = 3.58 (1.69–7.59) p = 0.001 | HR = 1.75 (0.76–4.05) p = 0.189 | ||||
| Yoo et al., 2021 [57] | 37 U/mL | 196 | OS | HR = 2.16 (1.48–3.17) p < 0.001 | HR = 2.06 (1.37–3.10) p < 0.001 | 2: Clinical data |
| Zhao et al., 2020 [58] | >1000 U/mL | 335 | OS | 25 mths vs. 33 mths p = 0.002 | NR | 2: Clinical data 5: Statistics |
| RFS < 12 mths | OR = 1.662 (1.071–2.581) p = 0.024 | OR = 2.205 (1.208–4.026) p = 0.010 | ||||
| Serum bilirubin | ||||||
| Abdel Wahab et al., 2016 [11] | NR | 243 | OS | N | NR | 2: Clinical data 5: Statistics 6: Classical prognostic factors |
| Cai et al., 2014 [16] | >10 mg/dL | 168 | OS | 39 vs. 33 mths p = 0.436 | NR | 2: Clinical data |
| Cheng et al., 2007 [20] | >10 mg/dL | 75 | OS | Significant (numbers not reported) | HR = 2.0 (1.5–2.5) p = 0.04 | 2: Clinical data |
| Dumitrascu et al., 2013 [21] | >10.4 mg/dL | 90 | OS | 17 vs. 42 mths p = 0.010 | N | 2: Clinical data 6: Classical prognostic factors |
| RFS | 12 vs. 31 mths p = 0.011 | N | ||||
| Li et al., 2019 [32] | >10 mg/dL | 181 | OS | 41.6 vs. 40.7 mths p = 0.868 | NR | 2: Clinical data |
| Ramacciato et al., 2010 [42] | >3 mg/dL | 30 | OS | 18 vs. 16 mths p = 0.259 | NR | 2: Clinical data 5: Statistics |
| Su et al., 1996 [46] | >10 mg/dL | 44 | OS | 6 vs. 18 mths p = 0.006 | HR = 2.44 (1.01–5.88) p = 0.001 | 2: Clinical data |
| Sun Z et al., 2020 [51] | >4 mg/dL | 110 | OS | 12 vs. 15.3 mths p = 0.018 | HR = 1.63 (1.02–2.59) p = 0.040 | 2: Clinical data |
| Zhao et al., 2020 [58] | >142.4 µmol/L | 335 | RFS <12 mths | OR = 1.207 (0.780–1.868) p = 0.398 | NR | 2: Clinical data 5: Statistics |
| Serum albumin * | ||||||
| Abdel Wahab et al., 2016 [11] | NR | 243 | OS | N | NR | 2: Clinical data 5: Statistics 6: Classical prognostic factors |
| Dumitrascu et al., 2013 [21] | <4 g/dL | 90 | OS | 44 vs. 13 mths p < 0.001 | N | 2: Clinical data 6: Classical prognostic factors |
| RFS | 38 vs. 10 mths p < 0.001 | N | ||||
| Li et al., 2020 [31] | <3.5 g/dL | 292 | OS | HR 0.72 (0.52–0.99) p = 0.041 | NR | 2: Clinical data |
| Ramacciato et al., 2010 [42] | <3 g/dL | 30 | OS | 19 vs. 11 mths p = 0.691 | NR | 2: Clinical data 5: Statistics |
| Saito et al., 2016 [44] | <3.5 g/dL | 121 | OS | 88.1 vs. 34.6 mths p = 0.003 | HR = 0.44 (0.22–0.88) p = 0.020 | |
| Su et al., 1996 [46] | <3 g/dL | 44 | OS | N and NR | NR | 2: Clinical data |
| Sun Z et al., 2020 [51] | <3.5 g/dL | 110 | OS | 19.4 vs. 9.2 mths p < 0.001 | HR = 0.65 (0.45–0.94) p = 0.023 | 2: Clinical data |
| Serum CEA | ||||||
| Kuriyama et al., 2020 [30] | >8.5 ng/mL | 49 | OS | 21.2 mths vs. not reached 5 yr OS: 39.2% vs. 51.6% p < 0.001 | HR = 10.516 (2.213–49.971) p = 0.003 | |
| Ramacciato et al., 2010 [42] | >2 U/ml | 30 | OS | 11 mths vs. 19 mths p = 0.465 | NR | 2: Clinical data 5: Statistics |
| Saito et al., 2016 [44] | >7 ng/mL | 121 | OS | 20.5 mths vs. 88.1 mths p < 0.001 | HR = 5.033 (2.273–11.14) p <0.001 | |
| Sun Z et al., 2020 [51] | >5 ng/ml | 110 | OS | 11.4 mths vs. 12.1 mths p = 0.635 | NR | 2: Clinical data |
| Wang et al., 2020 [56] | RFS | HR = 1.30 (0.75–2.26) p = 0.348 | 2: Clinical data | |||
| Yoo et al., 2021 [57] | >5 ng/ml | 94 | OS | HR = 1.29 (0.73–2.29) p = 0.374 | NR | 2: Clinical data |
| Zhao et al., 2020 [58] | >5 ng/mL | 196 | OS | HR = 1.82 (0.97–3.40) p = 0.062 | NR | 2: Clinical data |
| >3 ng/mL | 335 | RFS < 12 mths | OR = 1.662 (1.071–2.581) p = 0.024 | OR = 1.279 (0.775–2.108) p = 0.336 | 2: Clinical data 5: Statistics | |
| Serum NLR | ||||||
| Bird et al., 2019 [15] | >3 | 56 | OS | 33.7 vs. 53.6 mths p = 0.42 | NR | 2: Clinical data |
| Dumitrascu et al., 2013 [21] | >3.3 | 90 | OS | 15 vs. 43 mths p < 0.001 | HR = 0.76 (0.57–1) p = 0.053 | 2: Clinical data |
| RFS | 11 vs. 38 mths p < 0.001 | HR = 0.78 (0.62–0.98) p = 0.036 | ||||
| Okuno et al., 2015 [37] | >5 | 538 | OS | 39 vs. 28 mths p = 0.477 | NR | 1: Cohort overview |
| Saito et al., 2016 [44] | >2.5 | 121 | OS | 49.3 mths vs. 74.6 mths p = 0.225 | NR | |
| Wang et al., 2020 [56] | >3.6 | 94 | OS | HR = 2.78 (1.59–4.86) p < 0.001 | HR = 2.27 (1.22–4.24) p = 0.010 | 2: Clinical data |
| RFS | HR = 2.17 (1.29–3.66) p = 0.004 | HR = 1.83 (1.03–3.24) p = 0.038 | ||||
| Serum PLR | ||||||
| Dumitrascu et al., 2013 [21] | >184 | 90 | OS | 17 mths vs. 43 mths p = 0.002 | NR | 2: Clinical data 6: Classical prognostic factors |
| RFS | 12 mths vs. 35 mths p = 0.004 | NR | ||||
| Okuno et al., 2015 [37] | <150 ≥150 ≥300 | 534 | OS | 36 mths 44.4 mths 42 mths p = 0.409 | NR | 1: Cohort overview |
| Saito et al., 2016 [44] | >150 | 121 | OS | 49.3 mths 5 yr OS 43.8% vs. 62.4% p = 0.012 | HR = 2.207 (1.200–4.060) p = 0.011 | |
| Serum and Tumour MMP9 | ||||||
| Li et al., 2019 [32] | >201.93 ng/mL (Serum) | 181 | OS | 34.5 vs. 50.9 mths p < 0.001 | HR = 5.19 (CI NR) p < 0.01 | 2: Clinical data |
| Sun et al., 2014 [47] | >50% tumour expression | 58 | OS | 15 vs. >40 mths p < 0.001 | HR = 4.30 (1.49–12.43) p = 0.007 | |
| Sun et al., 2015 [48] | >50% tumour expression | 62 | OS | NR p < 0.022 | HR = 3.27 (1.22–6.94) p = 0.016 | |
| Author, Year | Biomarker | Detection | Univariable Analysis | Multivariable Analysis |
|---|---|---|---|---|
| Atanasov et al. 2018 [14] | miR-126 | Tumour IHC | mOS 8 vs. 24 mths p = 0.004 | NR |
| Atanasov et al., 2016 [13] | TEM | Tumour IHC | 5 yr OS 14.9% vs. 56.5% p = 0.026 | HR 2.90 (1.01–8.36) p = 0.045 |
| Atanasov et al., 2016 [12] | TAM | Tumour IHC | HR 0.32 (0.13–0.78) p = 0.013 | HR 0.856 (0.29–2.56) p = 0.78 |
| Chen et al., 2015 [19] | PIWIL2 | Tumour IHC | mOS 25.3 vs. 37.7 mths p = 0.013 | HR 0.253 (0.09–0.90) p = 0.026 |
| Dumitrascu et al., 2013 [21] | Haemoglobin | Blood | mOS 17 vs. 43 mths p = 0.015 | NR |
| Leukocyte count | Blood | mOS 17 vs. 43 mths p = 0.010 | NR | |
| Platelet count | Blood | mOS 14 vs. 44 mths p < 0.001 | NR | |
| Fang et al., 2014 [22] | P-4E-BP1 | Tumour IHC | mOS 19.5 vs. 29.9 mths p = 0.006 | NR |
| Huang et al., 2015 [25] | CYFRA21-1 | ECLiA | 5 yr OS 36.3% vs. 87.5% p < 0.01 | NR |
| Ishida et al., 2019 [26] | MUC5AC and MUC6 | Tumour IHC | HR 4.67 (1.42–17.98) p = 0.010 | HR 7.82 (1.29–66.97) p = 0.024 |
| Kamphues et al., 2015 [28] | DNA index | Tumour image cytometry | mOS 21.9 vs. 46.6 mths p = 0.010 | HR 0.61 (0.40–0.93) p = 0.021 |
| Li et al., 2020 [31] | MPV | Blood | HR 1.69 (1.23–2.31) p = 0.01 | HR 1.24 (0.89–1.74) p = 0.206 |
| PDW | Blood | HR 3.12 (2.33–4.19) p < 0.01 | HR 2.52 (1.83–3.47) p < 0.001 | |
| Liu et al., 2011 [34] | HDGF | Tumour IHC | Survival rate 35.7% vs. 73.3% p = 0.003 | HR 4.36 (1.45–13.10) p = 0.009 |
| VEGF | Tumour IHC | Survival rate 45.2% vs. 81.3% p = 0.018 | HR 3.913 (0.83–18.43) p = 0.084 | |
| Liu et al., 2019 [33] | TCF7 | Tumour IHC | 3 yr OS 59.0% vs. 23.0% p = 0.019 | HR 2.06 (CI NR) p = 0.024 |
| Ning et al., 2013 [36] | TROP2 | Tumour IHC | mOS 37 vs. >70 mths p = 0.001 | HR 3.26 (1.47–7.21) p = 0.004 |
| Okuno et al., 2016 [37] | mGPS | Blood | 5 yr OS 26.3% vs. 41.9% p < 0.001 | HR 1.58 (1.21–2.06) p = 0.001 |
| Peng et al., 2020 [40] | LMRc | Blood | mOS 20 vs. 36 mths p = 0.001 | NR |
| Qian et al., 2020 [41] | RPL34 | Tumour IHC | mOS 1.70 vs. 3.63 yrs p < 0.001 | HR 0.25 (0.12–0.54) p = 0.001 |
| Ruzzenente et al., 2016 [43] | ALK | Tumour PCR | mOS 5 vs. 34.9 mths p < 0.001 | NR |
| IDH1 | Tumour IHC | mOS 9.1 vs. 29.6 mths p = 0.043 | HR 17.84 (3.95–17.40) p = 0.004 | |
| P53 | Tumour PCR | mOS 15.4 vs. 32.5 mths p = 0.019 | HR 2.706 (1.11–8.21) p = 0.039 | |
| Saito et al., 2016 [44] | CRP | Blood | mOS 44.6 vs. >50 mths p < 0.001 | HR 3.29 (1.80–6.03) p < 0.001 |
| Sun Q et al., 2015 [48] | IL8 | Tumour IHC | mOS 17 vs. >42 mths p = 0.010 | HR 2.46 (0.92–8.54) p = 0.005 |
| Sun Q et al., 2018 [49] | Pontin | Tumour IHC | mOS 18 vs. > 40 mths p = 0.002 | HR 2.883 (1.26–6.72) p = 0.001 |
| Sun R et al., 2019 [50] | ANXA10 | Tumour IHC | 3 yr OS 13.1% vs. 52.0% p < 0.001 | HR 2.25 (1.34–3.84) p = 0.026 |
| Takahashi et al., 2021 [52] | HMGA2 | Tumour IHC | HR 3.05 (1.19–7.80) p = 0.015 | HR 5.23 (1.77–15.50) p = 0.003 |
| Wang et al., 2020 [56] | CONUT score | Blood | HR 3.77 (2.21–6.43) p < 0.001 | HR 4.01 (1.97–8.18) p < 0.001 |
| PNI | Blood | HR 0.36 (0.21–0.61) p < 0.001 | HR 0.26 (0.14–0.49) p < 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pawaskar, R.; Huang, K.Z.; Pham, H.; Nagrial, A.; Wong, M.; O’Neill, S.; Pleass, H.; Yuen, L.; Lam, V.W.T.; Richardson, A.; et al. Systematic Review of Preoperative Prognostic Biomarkers in Perihilar Cholangiocarcinoma. Cancers 2024, 16, 698. https://doi.org/10.3390/cancers16040698
Pawaskar R, Huang KZ, Pham H, Nagrial A, Wong M, O’Neill S, Pleass H, Yuen L, Lam VWT, Richardson A, et al. Systematic Review of Preoperative Prognostic Biomarkers in Perihilar Cholangiocarcinoma. Cancers. 2024; 16(4):698. https://doi.org/10.3390/cancers16040698
Chicago/Turabian StylePawaskar, Rishaan, Kevin Zhang Huang, Helen Pham, Adnan Nagrial, Mark Wong, Siobhan O’Neill, Henry Pleass, Lawrence Yuen, Vincent W. T. Lam, Arthur Richardson, and et al. 2024. "Systematic Review of Preoperative Prognostic Biomarkers in Perihilar Cholangiocarcinoma" Cancers 16, no. 4: 698. https://doi.org/10.3390/cancers16040698
APA StylePawaskar, R., Huang, K. Z., Pham, H., Nagrial, A., Wong, M., O’Neill, S., Pleass, H., Yuen, L., Lam, V. W. T., Richardson, A., Pang, T., & Nahm, C. B. (2024). Systematic Review of Preoperative Prognostic Biomarkers in Perihilar Cholangiocarcinoma. Cancers, 16(4), 698. https://doi.org/10.3390/cancers16040698







