Effectiveness of the Korean National Cancer Screening Program in Reducing Colorectal Cancer Mortality
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
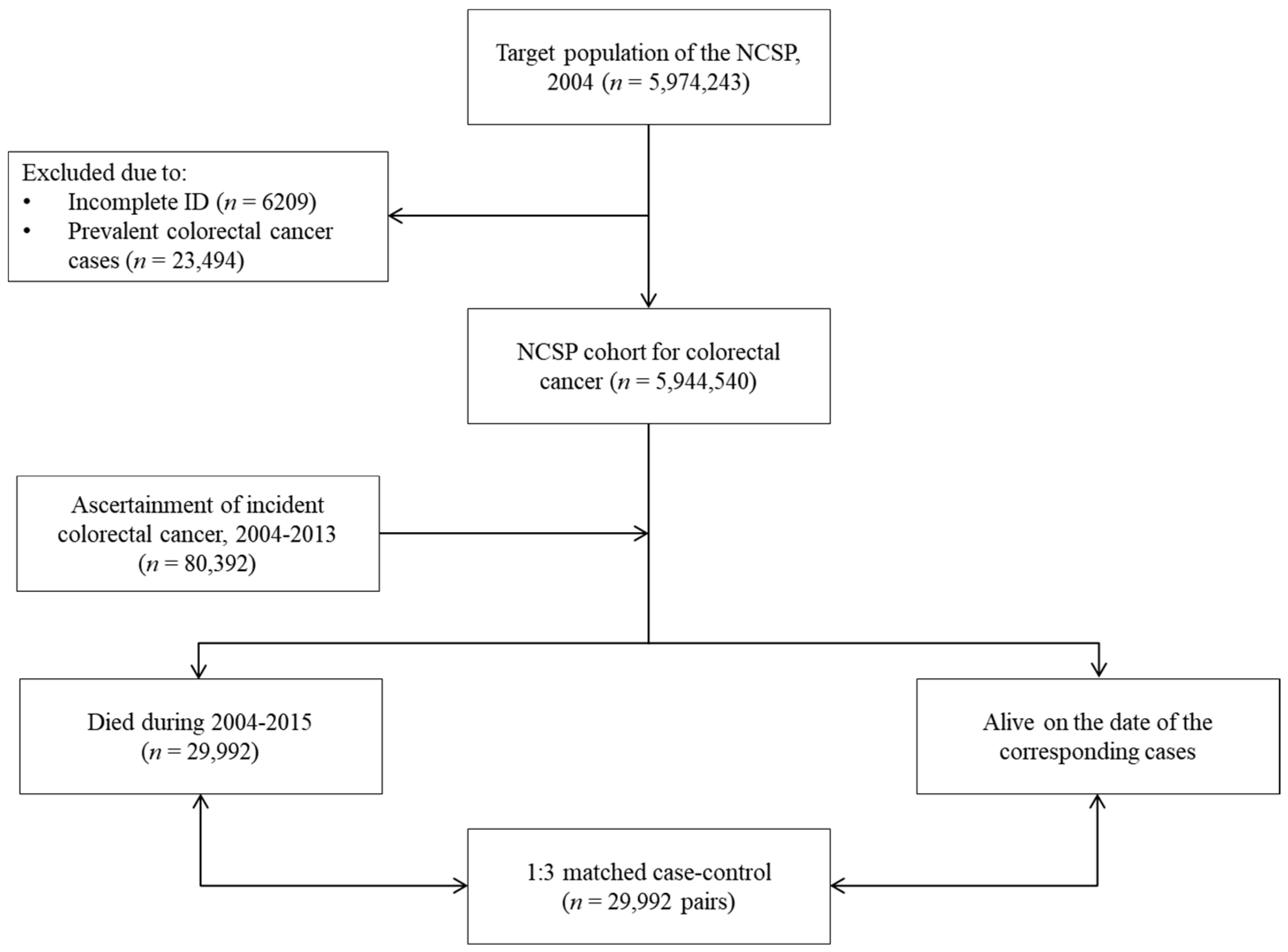
2.2. Study Population
2.3. Measurements
2.4. Statistical Analysis
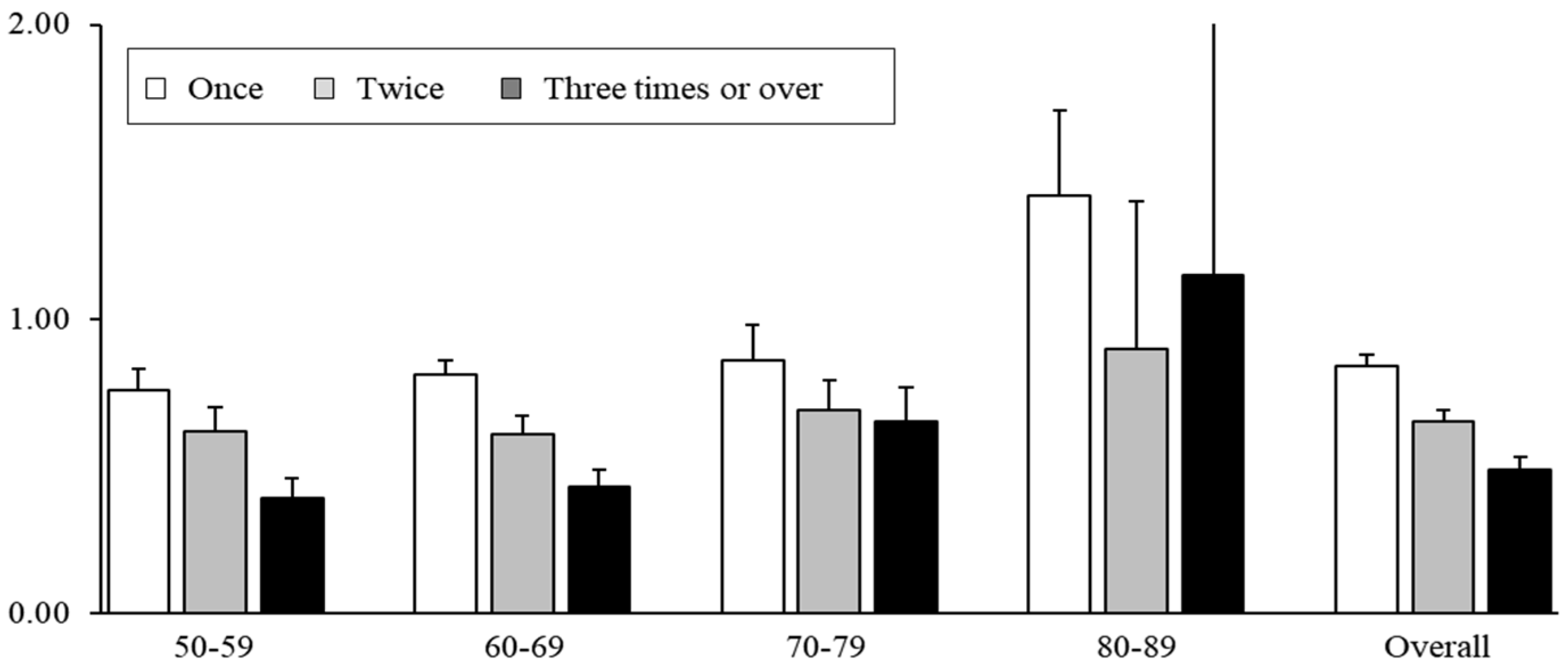
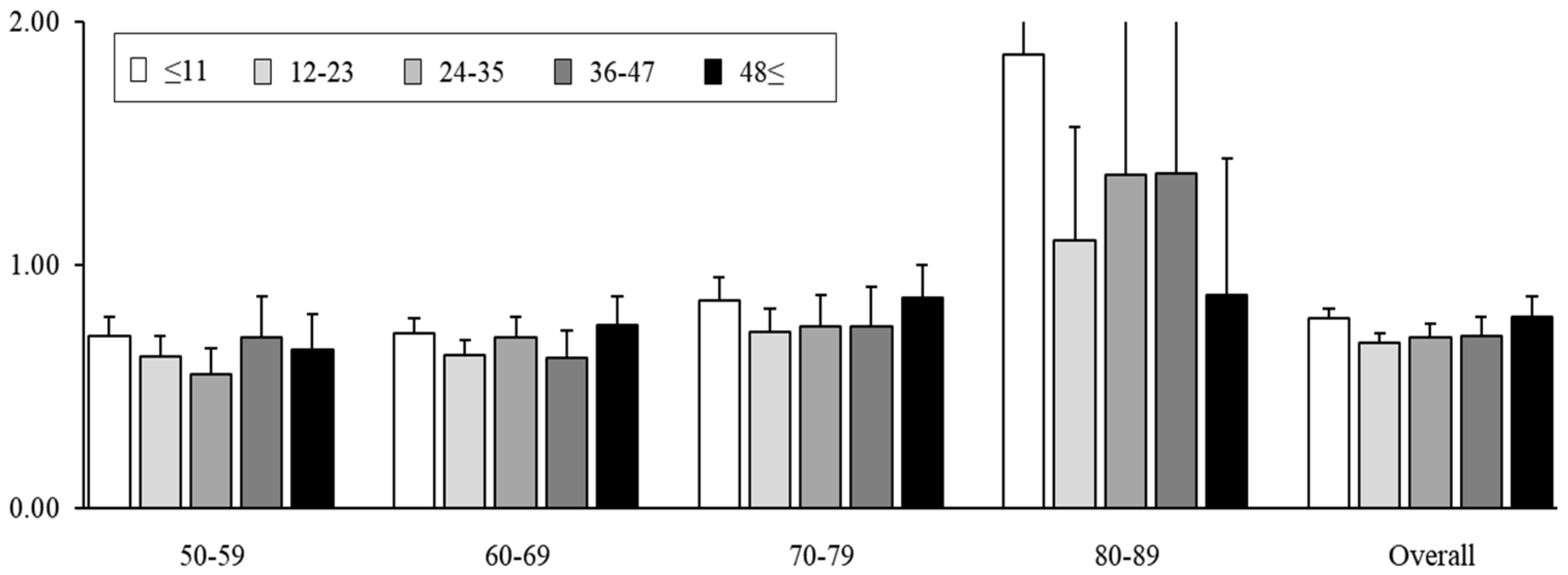
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Kang, M.J.; Jung, K.-W.; Bang, S.H.; Choi, S.H.; Park, E.H.; Yun, E.H.; Kim, H.-J.; Kong, H.-J.; Im, J.-S.; Seo, H.G. Cancer statistics in Korea: Incidence, mortality, survival, and prevalence in 2020. Cancer Res. Treat. 2023, 55, 385–399. [Google Scholar] [CrossRef] [PubMed]
- Morgan, E.; Arnold, M.; Gini, A.; Lorenzoni, V.; Cabasag, C.; Laversanne, M.; Vignat, J.; Ferlay, J.; Murphy, N.; Bray, F. Global burden of colorectal cancer in 2020 and 2040: Incidence and mortality estimates from GLOBOCAN. Gut 2023, 72, 338–344. [Google Scholar] [CrossRef] [PubMed]
- Winawer, S.J. Natural history of colorectal cancer. Am. J. Med. 1999, 106, 3–6. [Google Scholar] [CrossRef]
- Zheng, S.; Schrijvers, J.J.; Greuter, M.J.; Kats-Ugurlu, G.; Lu, W.; de Bock, G.H. Effectiveness of Colorectal Cancer (CRC) Screening on All-Cause and CRC-Specific Mortality Reduction: A Systematic Review and Meta-Analysis. Cancers 2023, 15, 1948. [Google Scholar] [CrossRef]
- Levin, T.R.; Corley, D.A.; Jensen, C.D.; Schottinger, J.E.; Quinn, V.P.; Zauber, A.G.; Lee, J.K.; Zhao, W.K.; Udaltsova, N.; Ghai, N.R. Effects of organized colorectal cancer screening on cancer incidence and mortality in a large community-based population. Gastroenterology 2018, 155, 1383–1391.e1385. [Google Scholar] [CrossRef]
- Lauby-Secretan, B.; Vilahur, N.; Bianchini, F.; Guha, N.; Straif, K. The IARC perspective on colorectal cancer screening. N. Engl. J. Med. 2018, 378, 1734–1740. [Google Scholar] [CrossRef]
- Guo, F.; Chen, C.; Holleczek, B.; Schöttker, B.; Hoffmeister, M.; Brenner, H. Strong reduction of colorectal cancer incidence and mortality after screening colonoscopy: Prospective cohort study from Germany. Am. J. Gastroenterol. 2021, 116, 967–975. [Google Scholar] [CrossRef]
- Almog, R.; Ezra, G.; Lavi, I.; Rennert, G.; Hagoel, L. The public prefers fecal occult blood test over colonoscopy for colorectal cancer screening. Eur. J. Cancer Prev. 2008, 17, 430–437. [Google Scholar] [CrossRef]
- Sobhani, I.; Alzahouri, K.; Ghout, I.; Charles, D.J.; Durand-Zaleski, I. Cost-effectiveness of mass screening for colorectal cancer: Choice of fecal occult blood test and screening strategy. Dis. Colon Rectum 2011, 54, 876–886. [Google Scholar] [CrossRef]
- Lopes, G.; Stern, M.C.; Temin, S.; Sharara, A.I.; Cervantes, A.; Costas-Chavarri, A.; Engineer, R.; Hamashima, C.; Ho, G.F.; Huitzil, F.D. Early detection for colorectal cancer: ASCO resource-stratified guideline. J. Glob. Oncol. 2019, 5, 1–22. [Google Scholar] [PubMed]
- Clark, G.; Strachan, J.A.; Carey, F.A.; Godfrey, T.; Irvine, A.; McPherson, A.; Brand, J.; Anderson, A.S.; Fraser, C.G.; Steele, R.J. Transition to quantitative faecal immunochemical testing from guaiac faecal occult blood testing in a fully rolled-out population-based national bowel screening programme. Gut 2021, 70, 106–113. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, J.A.; Bobo, J.K.; Church, T.R.; Rex, D.K.; Chovnick, G.; Thompson, T.D.; Zauber, A.G.; Lieberman, D.; Levin, T.R.; Joseph, D.A. A comparison of fecal immunochemical and high-sensitivity guaiac tests for colorectal cancer screening. Am. J. Gastroenterol. 2017, 112, 1728–1735. [Google Scholar] [CrossRef]
- Tinmouth, J.; Lansdorp-Vogelaar, I.; Allison, J.E. Faecal immunochemical tests versus guaiac faecal occult blood tests: What clinicians and colorectal cancer screening programme organisers need to know. Gut 2015, 64, 1327–1337. [Google Scholar] [CrossRef]
- Levi, Z.; Birkenfeld, S.; Vilkin, A.; Bar-Chana, M.; Lifshitz, I.; Chared, M.; Maoz, E.; Niv, Y. A higher detection rate for colorectal cancer and advanced adenomatous polyp for screening with immunochemical fecal occult blood test than guaiac fecal occult blood test, despite lower compliance rate. A prospective, controlled, feasibility study. Int. J. Cancer 2011, 128, 2415–2424. [Google Scholar] [CrossRef]
- Mousavinezhad, M.; Majdzadeh, R.; Sari, A.A.; Delavari, A.; Mohtasham, F. The effectiveness of FOBT vs. FIT: A meta-analysis on colorectal cancer screening test. Med. J. Islam. Repub. Iran 2016, 30, 366. [Google Scholar]
- Allison, J.E.; Tekawa, I.S.; Ransom, L.J.; Adrain, A.L. A comparison of fecal occult-blood tests for colorectal-cancer screening. N. Engl. J. Med. 1996, 334, 155–160. [Google Scholar] [CrossRef]
- Meklin, J.; Syrjänen, K.; Eskelinen, M. Fecal occult blood tests in colorectal cancer screening: Systematic review and meta-analysis of traditional and new-generation fecal immunochemical tests. Anticancer Res. 2020, 40, 3591–3604. [Google Scholar] [CrossRef]
- Park, B.; Her, E.Y.; Lee, K.; Nari, F.; Jun, J.K.; Choi, K.S.; Suh, M. Overview of the National Cancer Screening Program for Colorectal Cancer in Korea over 14 Years (2004–2017). Cancer Res. Treat. 2023, 55, 910–917. [Google Scholar] [CrossRef]
- Sohn, D.K.; Kim, M.J.; Park, Y.; Suh, M.; Shin, A.; Lee, H.Y.; Im, J.P.; Cho, H.-M.; Hong, S.P.; Kim, B.-h.; et al. The Korean guideline for colorectal cancer screening. JKMA J. Korean Med. Assoc. 2015, 58, 420–432. [Google Scholar] [CrossRef]
- Shin, A.; Choi, K.S.; Jun, J.K.; Noh, D.K.; Suh, M.; Jung, K.-W.; Kim, B.C.; Oh, J.H.; Park, E.-C. Validity of fecal occult blood test in the national cancer screening program, Korea. PLoS ONE 2013, 8, e79292. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Park, B.; Lee, Y.Y.; Song, S.Y.; Shin, H.Y.; Suh, M.; Choi, K.S.; Jun, J.K. Trends of colorectal cancer screening rates in Korea: Korean national cancer screening survey 2005–2020. Gut Liver 2022, 16, 930. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.H.; Jeong, S.Y. Korean national recommendation guidelines on screening and surveillance for early detection of colorectal cancers. J. Korean Med. Assoc. 2002, 45, 981–991. [Google Scholar] [CrossRef]
- Luu, X.Q.; Lee, K.; Jun, J.K.; Suh, M.; Jung, K.W.; Choi, K.S. Effect of colorectal cancer screening on long-term survival of colorectal cancer patients: Results of the Korea National Cancer Screening Program. Int. J. Cancer 2022, 150, 1958–1967. [Google Scholar] [CrossRef]
- Ahn, E. Introducing big data analysis using data from National Health Insurance Service. Korean J. Anesthesiol. 2020, 73, 205–211. [Google Scholar] [CrossRef]
- Zappa, M.; Castiglione, G.; Grazzini, G.; Falini, P.; Giorgi, D.; Paci, E.; Ciatto, S. Effect of faecal occult blood testing on colorectal mortality: Results of a population-based case-control study in the district of Florence, Italy. Int. J. Cancer 1997, 73, 208–210. [Google Scholar] [CrossRef]
- Gini, A.; Jansen, E.E.; Zielonke, N.; Meester, R.G.; Senore, C.; Anttila, A.; Segnan, N.; Mlakar, D.N.; de Koning, H.J.; Lansdorp-Vogelaar, I. Impact of colorectal cancer screening on cancer-specific mortality in Europe: A systematic review. Eur. J. Cancer 2020, 127, 224–235. [Google Scholar] [CrossRef]
- Rossi, P.G.; Vicentini, M.; Sacchettini, C.; Di Felice, E.; Caroli, S.; Ferrari, F.; Mangone, L.; Pezzarossi, A.; Roncaglia, F.; Campari, C. Impact of screening program on incidence of colorectal cancer: A cohort study in Italy. Am. J. Gastroenterol. 2015, 110, 1359–1366. [Google Scholar] [CrossRef]
- Chiu, H.M.; Chen, S.L.S.; Yen, A.M.F.; Chiu, S.Y.H.; Fann, J.C.Y.; Lee, Y.C.; Pan, S.L.; Wu, M.S.; Liao, C.S.; Chen, H.H. Effectiveness of fecal immunochemical testing in reducing colorectal cancer mortality from the One Million Taiwanese Screening Program. Cancer 2015, 121, 3221–3229. [Google Scholar] [CrossRef]
- Hewitson, P.; Glasziou, P.; Watson, E.; Towler, B.; Irwig, L. Cochrane systematic review of colorectal cancer screening using the fecal occult blood test (hemoccult): An update. Am. J. Gastroenterol. 2008, 103, 1541–1549. [Google Scholar] [CrossRef]
- Zorzi, M.; Fedeli, U.; Schievano, E.; Bovo, E.; Guzzinati, S.; Baracco, S.; Fedato, C.; Saugo, M.; Dei Tos, A.P. Impact on colorectal cancer mortality of screening programmes based on the faecal immunochemical test. Gut 2015, 64, 784–790. [Google Scholar] [CrossRef] [PubMed]
- Murphy, C.C.; Sen, A.; Watson, B.; Gupta, S.; Mayo, H.; Singal, A.G. A systematic review of repeat fecal occult blood tests for colorectal cancer screening. Cancer Epidemiol. Biomark. 2020, 29, 278–287. [Google Scholar] [CrossRef] [PubMed]
- Holme, Ø.; Bretthauer, M.; Fretheim, A.; Odgaard-Jensen, J.; Hoff, G. Flexible sigmoidoscopy versus faecal occult blood testing for colorectal cancer screening in asymptomatic individuals. Cochrane Database Syst. Rev. 2013, 2014, CD009259. [Google Scholar] [CrossRef] [PubMed]
- Hassan, C.; Rossi, P.G.; Camilloni, L.; Rex, D.; Jimenez-Cendales, B.; Ferroni, E.; Borgia, P.; Zullo, A.; Guasticchi, G.; Group, H. Meta-analysis: Adherence to colorectal cancer screening and the detection rate for advanced neoplasia, according to the type of screening test. Aliment. Pharmacol. Ther. 2012, 36, 929–940. [Google Scholar] [CrossRef] [PubMed]
- Bénard, F.; Barkun, A.N.; Martel, M.; von Renteln, D. Systematic review of colorectal cancer screening guidelines for average-risk adults: Summarizing the current global recommendations. World J. Gastroenterol. 2018, 24, 124–138. [Google Scholar] [CrossRef]
- Hong, S.; Lee, Y.Y.; Lee, J.; Kim, Y.; Choi, K.S.; Jun, J.K.; Suh, M. Trends in cancer screening rates among Korean men and women: Results of the Korean National Cancer Screening Survey, 2004–2018. Cancer Res. Treat. 2021, 53, 330–338. [Google Scholar] [CrossRef]
- Shaukat, A.; Dostal, A.; Menk, J.; Church, T.R. BMI is a risk factor for colorectal cancer mortality. Dig. Dis. Sci. 2017, 62, 2511–2517. [Google Scholar] [CrossRef]
- Murphy, T.K.; Calle, E.E.; Rodriguez, C.; Kahn, H.S.; Thun, M.J. Body mass index and colon cancer mortality in a large prospective study. Am. J. Epidemiol. 2000, 152, 847–854. [Google Scholar] [CrossRef]
- Chao, A.; Thun, M.J.; Jacobs, E.J.; Henley, S.J.; Rodriguez, C.; Calle, E.E. Cigarette smoking and colorectal cancer mortality in the cancer prevention study II. J. Natl. Cancer Inst. 2000, 92, 1888–1896. [Google Scholar] [CrossRef]
- Botteri, E.; Iodice, S.; Bagnardi, V.; Raimondi, S.; Lowenfels, A.B.; Maisonneuve, P. Smoking and colorectal cancer: A meta-analysis. JAMA 2008, 300, 2765–2778. [Google Scholar] [CrossRef]
| All-Cause Mortality | Colorectal Cancer-Specific Mortality | All-Cause Mortality Except from Colorectal Cancer | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Screened, % | Screened, % | Screened, % | |||||||||||||
| Pairs, n | Case | Control | OR | 95% CI | Pairs, n | Case | Control | OR | 95% CI | Pairs, n | Case | Control | OR | 95% CI | |
| Overall | 29,992 | 23.50 | 27.70 | 0.77 | 0.74–0.79 | 23,455 | 23.60 | 28.60 | 0.74 | 0.71–0.76 | 6537 | 23.10 | 24.80 | 0.90 | 0.83–0.96 |
| Sex | |||||||||||||||
| Male | 18,587 | 26.00 | 30.50 | 0.77 | 0.74–0.80 | 14,122 | 26.00 | 31.40 | 0.73 | 0.70–0.77 | 4465 | 26.00 | 27.60 | 0.91 | 0.83–0.99 |
| Female | 11,405 | 19.40 | 23.30 | 0.75 | 0.71–0.85 | 9333 | 19.90 | 24.30 | 0.73 | 0.69–0.78 | 2072 | 17.00 | 18.80 | 0.86 | 0.74–1.00 |
| 10-year age groups | |||||||||||||||
| 50–59 | 6072 | 27.80 | 24.80 | 0.68 | 0.64–0.73 | 5201 | 27.30 | 34.90 | 0.66 | 0.61–0.71 | 871 | 30.70 | 34.10 | 0.83 | 0.70–1.00 |
| 60–69 | 10,411 | 29.90 | 36.10 | 0.71 | 0.68–0.75 | 8013 | 30.20 | 37.30 | 0.69 | 0.65–0.73 | 2398 | 28.80 | 32.40 | 0.82 | 0.73–0.91 |
| 70–79 | 10,153 | 19.30 | 21.70 | 0.84 | 0.79–0.89 | 7631 | 19.20 | 22.50 | 0.79 | 0.74–0.85 | 2522 | 19.40 | 19.40 | 0.99 | 0.88–1.12 |
| 80+ | 3356 | 8.40 | 6.70 | 1.29 | 1.10–1.50 | 2610 | 8.40 | 6.60 | 1.31 | 1.10–1.55 | 746 | 8.60 | 7.10 | 1.22 | 0.88–1.68 |
| 5-year age groups | |||||||||||||||
| 50–54 | 3100 | 25.90 | 32.40 | 0.69 | 0.63–0.76 | 2723 | 26.20 | 32.50 | 0.70 | 0.63–0.78 | 377 | 23.90 | 31.80 | 0.63 | 0.47–0.84 |
| 55–59 | 2972 | 29.80 | 37.20 | 0.67 | 0.61–0.74 | 2478 | 28.60 | 37.50 | 0.62 | 0.55–0.69 | 494 | 35.80 | 35.90 | 1.00 | 0.80–1.25 |
| 60–64 | 5348 | 30.70 | 38.40 | 0.66 | 0.62–0.71 | 4186 | 30.70 | 39.20 | 0.64 | 0.59–0.69 | 1162 | 30.60 | 35.50 | 0.77 | 0.66–0.90 |
| 65–69 | 5063 | 29.10 | 33.70 | 0.77 | 0.71–0.83 | 3827 | 29.70 | 35.10 | 0.74 | 0.68–0.81 | 1236 | 27.10 | 29.50 | 0.87 | 0.74–1.02 |
| 70–74 | 6491 | 21.60 | 25.00 | 0.80 | 0.74–0.86 | 4852 | 21.60 | 26.10 | 0.75 | 0.69–0.82 | 1639 | 21.50 | 21.70 | 0.98 | 0.85–1.14 |
| 75–79 | 3662 | 15.20 | 15.90 | 0.93 | 0.84–1.04 | 2779 | 15.10 | 16.20 | 0.91 | 0.80–1.03 | 883 | 15.60 | 15.20 | 1.02 | 0.82–1.27 |
| 80–84 | 2624 | 9.80 | 7.50 | 1.35 | 1.15–1.59 | 2048 | 9.60 | 7.40 | 1.38 | 1.15–1.65 | 576 | 10.20 | 8.00 | 1.27 | 0.90–1.79 |
| 85+ | 732 | 3.70 | 3.00 | 1.20 | 0.69–2.08 | 562 | 3.90 | 3.00 | 1.31 | 0.71–2.41 | 170 | 2.90 | 3.00 | 0.79 | 0.20–3.11 |
| Economic level | |||||||||||||||
| High | 16,187 | 20.60 | 25.60 | 0.70 | 0.67–0.74 | 12,556 | 20.90 | 26.30 | 0.69 | 0.65–0.72 | 3631 | 19.50 | 22.90 | 0.77 | 0.70–0.86 |
| Middle | 9227 | 27.50 | 32.10 | 0.77 | 0.73–0.82 | 7375 | 27.40 | 33.00 | 0.73 | 0.68–0.77 | 1852 | 28.00 | 28.50 | 0.98 | 0.86–1.11 |
| Low | 4578 | 25.80 | 26.60 | 0.96 | 0.88–1.04 | 3524 | 25.40 | 27.10 | 0.91 | 0.82–1.00 | 1054 | 27.00 | 24.50 | 1.15 | 0.97–1.37 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, H.J.; Lee, K.; Kim, B.C.; Jun, J.K.; Choi, K.S.; Suh, M. Effectiveness of the Korean National Cancer Screening Program in Reducing Colorectal Cancer Mortality. Cancers 2024, 16, 4278. https://doi.org/10.3390/cancers16244278
Lee HJ, Lee K, Kim BC, Jun JK, Choi KS, Suh M. Effectiveness of the Korean National Cancer Screening Program in Reducing Colorectal Cancer Mortality. Cancers. 2024; 16(24):4278. https://doi.org/10.3390/cancers16244278
Chicago/Turabian StyleLee, Hyeon Ji, Kyeongmin Lee, Byung Chang Kim, Jae Kwan Jun, Kui Son Choi, and Mina Suh. 2024. "Effectiveness of the Korean National Cancer Screening Program in Reducing Colorectal Cancer Mortality" Cancers 16, no. 24: 4278. https://doi.org/10.3390/cancers16244278
APA StyleLee, H. J., Lee, K., Kim, B. C., Jun, J. K., Choi, K. S., & Suh, M. (2024). Effectiveness of the Korean National Cancer Screening Program in Reducing Colorectal Cancer Mortality. Cancers, 16(24), 4278. https://doi.org/10.3390/cancers16244278






