Prealbumin Prognostic Score: A Novel Prognostic Indicator After Radical Gastrectomy in Patients with Gastric Cancer
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Definitions
2.3. Study Endopoints
2.4. Perioperative Treatment
2.5. Statistical Analysis
3. Results
3.1. Characteristics of the Patients
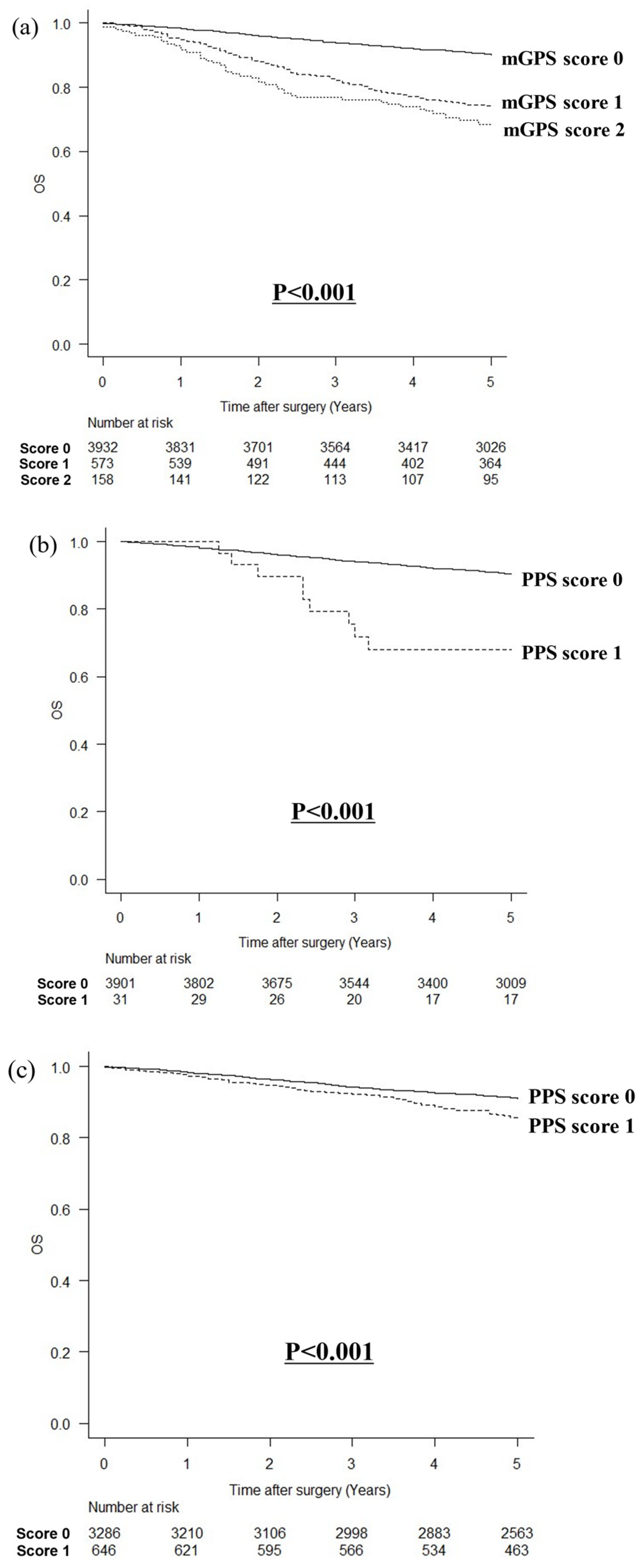
3.2. Comparison of OS
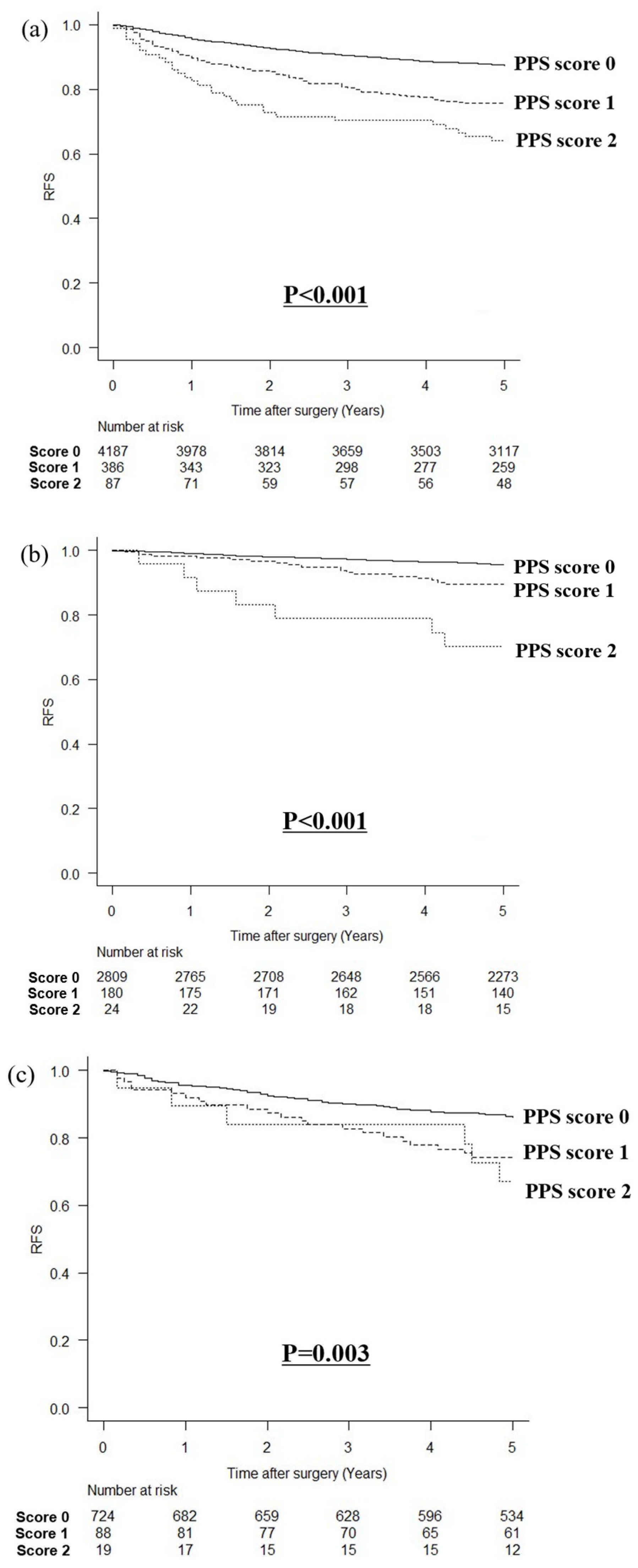
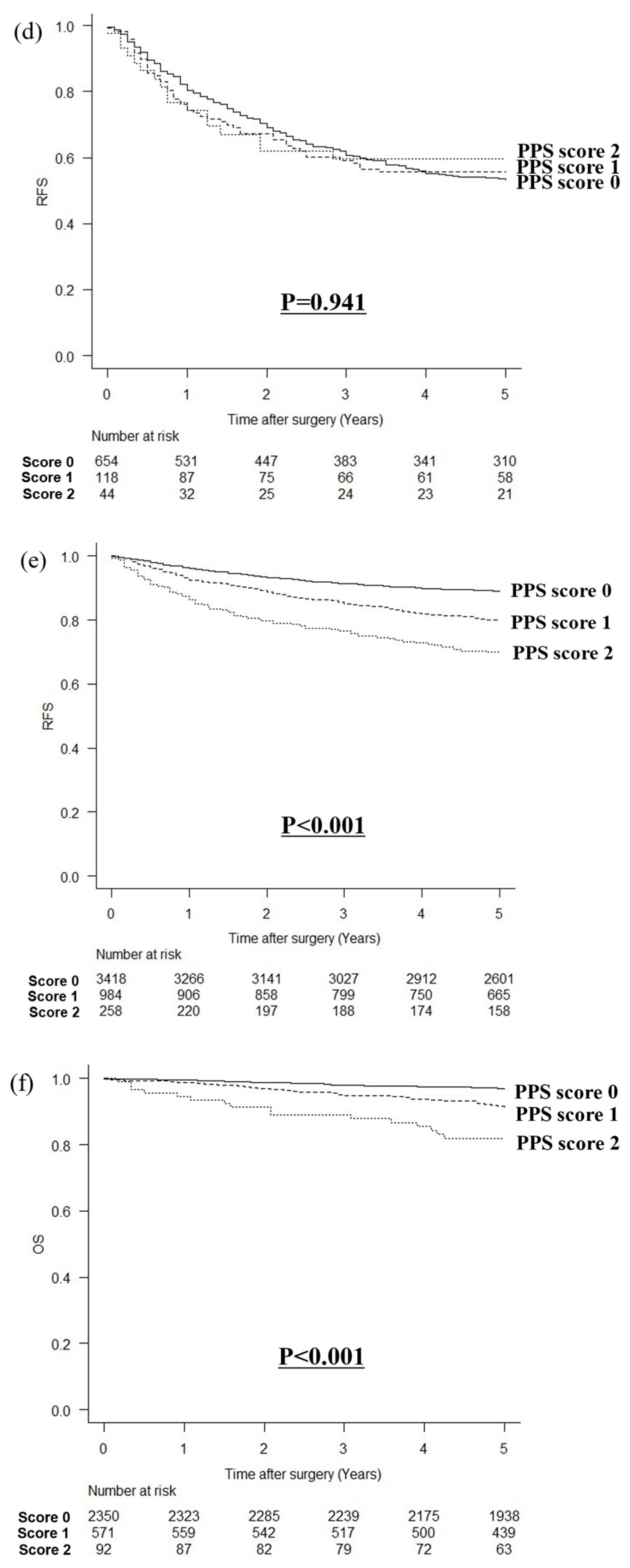
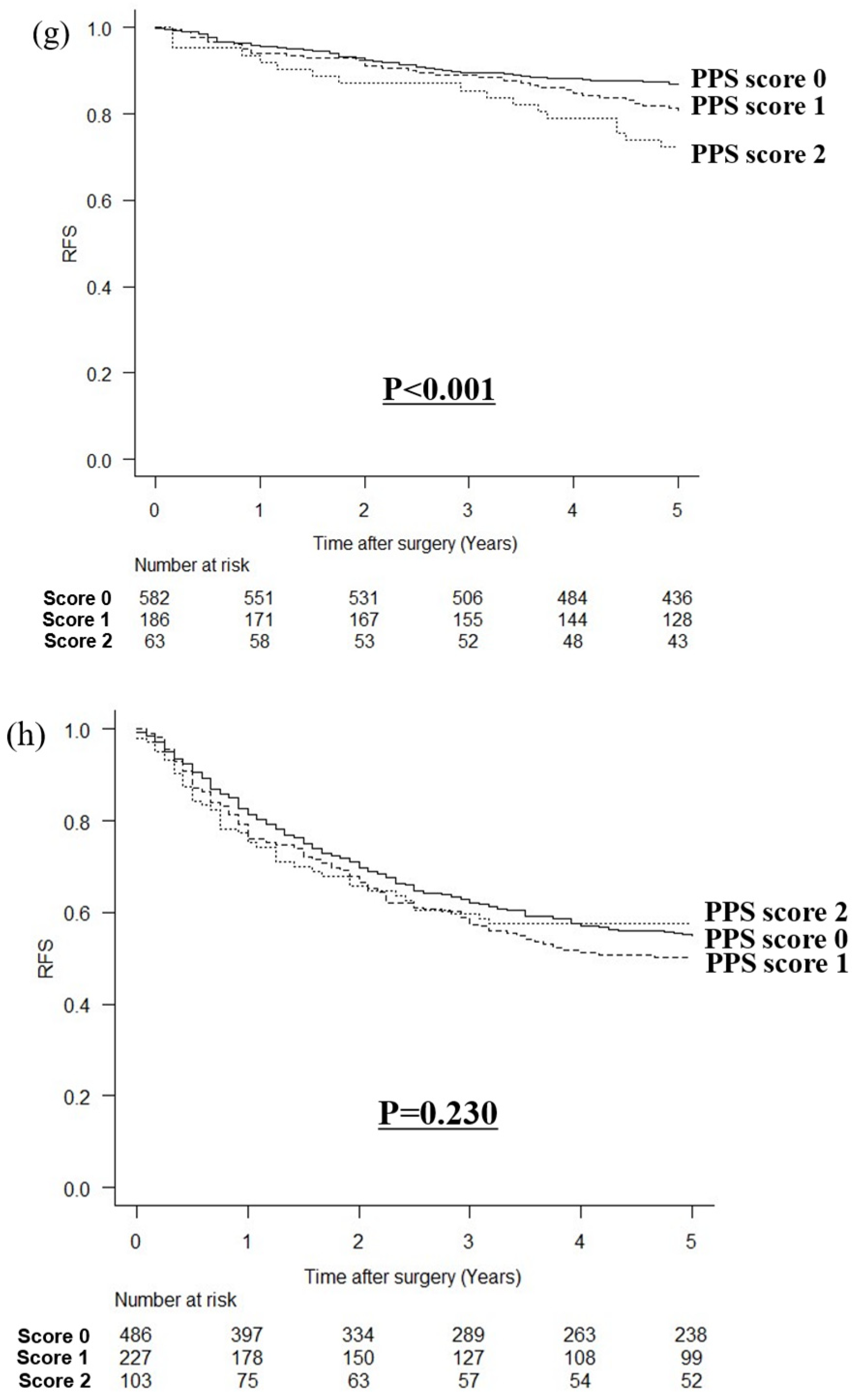
3.3. Comparison of RFS
3.4. Prognostic Factors by Multivariate Analysis
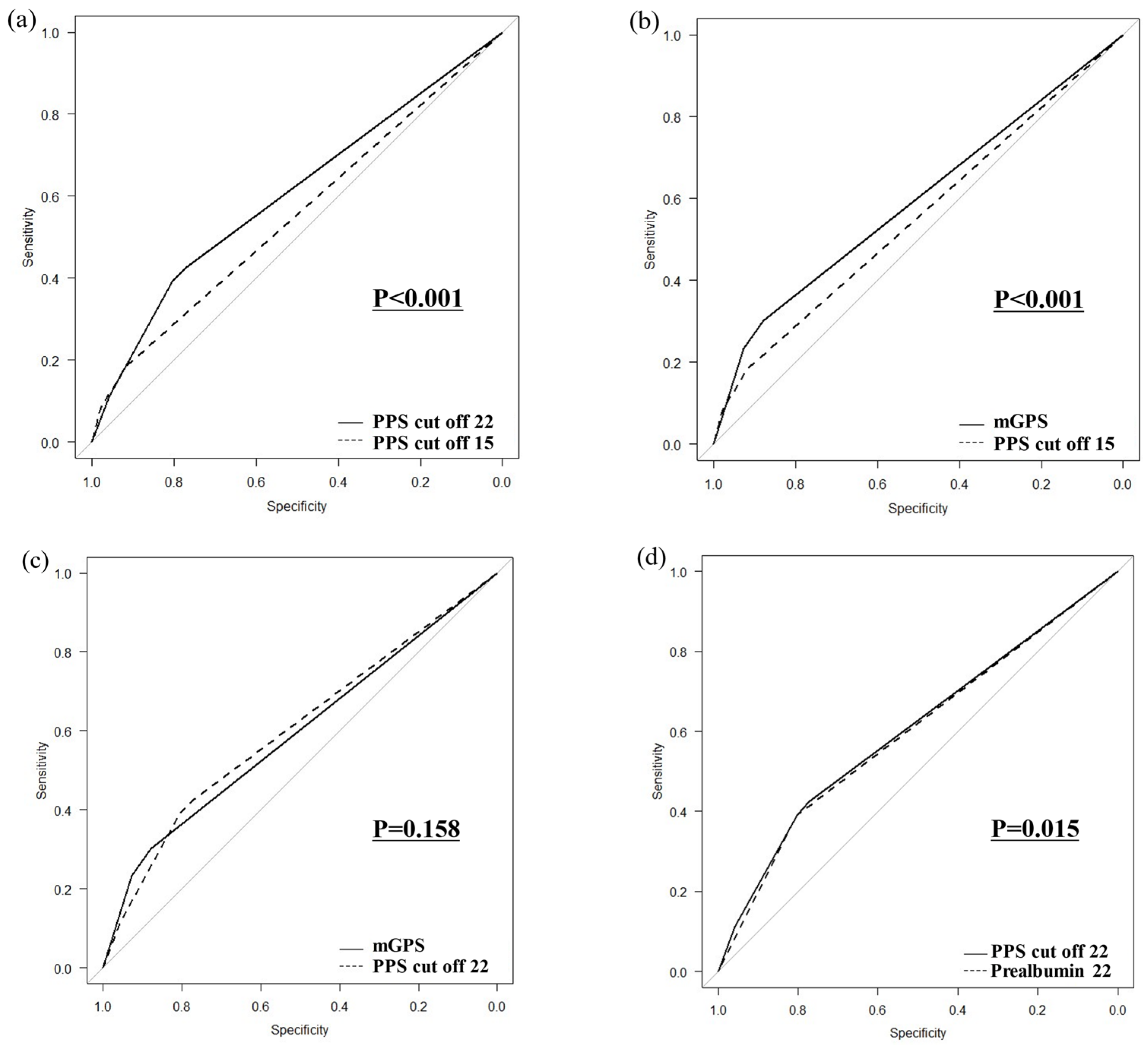
3.5. Comparison of ROC Curves
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Shimoda, Y.; Fujikawa, H.; Komori, K.; Watanabe, H.; Takahashi, K.; Kano, K.; Yamada, T.; Shiozawa, M.; Morinaga, S.; Katsumata, K.; et al. The Glasgow Prognostic Score Before Curative Resection May Predict Postoperative Complications in Patients with Gastric Cancer. J. Gastrointest. Cancer 2022, 53, 908–914. [Google Scholar] [CrossRef] [PubMed]
- Jiang, X.; Hiki, N.; Nunobe, S.; Kumagai, K.; Kubota, T.; Aikou, S.; Sano, T.; Yamaguchi, T. Prognostic importance of the inflammation-based Glasgow prognostic score in patients with gastric cancer. Br. J. Cancer 2012, 107, 275–279. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.-S.; Ren, C.; Qiu, M.-Z.; Luo, H.-Y.; Wang, Z.-Q.; Zhang, D.-S.; Wang, F.-H.; Li, Y.-H.; Xu, R.-H. Comparison of the prognostic value of various preoperative inflammation-based factors in patients with stage III gastric cancer. Tumour Biol. 2012, 33, 749–756. [Google Scholar] [CrossRef] [PubMed]
- Dutta, S.; Crumley, A.B.; Fullarton, G.M.; Horgan, P.G.; McMillan, D.C. Comparison of the prognostic value of tumour and patient related factors in patients undergoing potentially curative resection of gastric cancer. Am. J. Surg. 2012, 204, 294–299. [Google Scholar] [CrossRef] [PubMed]
- Forrest, L.M.; McMillan, D.C.; McArdle, C.S.; Angerson, W.J.; Dunlop, D.J. Evaluation of cumulative prognostic scores based on the systemic inflammatory response in patients with inoperable non-small-cell lung cancer. Br. J. Cancer 2003, 89, 1028–1030. [Google Scholar] [CrossRef] [PubMed]
- Toiyama, Y.; Miki, C.; Inoue, Y.; Tanaka, K.; Mohri, Y.; Kusunoki, M. Evaluation of an inflammation-based prognostic score for the identification of patients requiring postoperative adjuvant chemotherapy for stage II colorectal cancer. Exp. Ther. Med. 2011, 2, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Matsui, R.; Ida, S.; Ri, M.; Makuuchi, R.; Hayami, M.; Kumagai, K.; Ohashi, M.; Sano, T.; Nunobe, S. Impact of preoperative prealbumin levels on long-term prognosis in patients with gastric cancer after gastrectomy: A retrospective cohort study. Gastric Cancer 2024, 27, 611–621. [Google Scholar] [CrossRef] [PubMed]
- Evans, D.C.; Corkins, M.R.; Malone, A.; Miller, S.; Mogensen, K.M.; Guenter, P.; Jensen, G.L.; The ASPEN Malnutrition Committee. The Use of Visceral Proteins as Nutrition Markers: An ASPEN Position Paper. Nutr. Clin. Pract. 2021, 36, 22–28. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, T.; Hojo, Y.; Kumamoto, T.; Kurahashi, Y.; Ishida, Y.; Shinohara, H. History of the lymph node numbering system in the Japanese Classification of Gastric Carcinoma since 1962. Surg. Today 2022, 52, 1515–1523. [Google Scholar] [CrossRef] [PubMed]
- Katayama, H.; Kurokawa, Y.; Nakamura, K.; Ito, H.; Kanemitsu, Y.; Masuda, N.; Tsubosa, Y.; Satoh, T.; Yokomizo, A.; Fukuda, H.; et al. Extended Clavien-Dindo classification of surgical complications: Japan Clinical Oncology Group postoperative complications criteria. Surg. Today 2016, 46, 668–685. [Google Scholar] [CrossRef] [PubMed]
- Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer 2017, 20, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2018 (5th edition). Gastric Cancer 2021, 24, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Forrest, L.M.; McMillan, D.C.; McArdle, C.S.; Angerson, W.J.; Dunlop, D.J. Comparison of an inflammation-based prognostic score (GPS) with performance status (ECOG) in patients receiving platinum-based chemotherapy for inoperable non-small-cell lung cancer. Br. J. Cancer 2004, 90, 1704–1706. [Google Scholar] [CrossRef] [PubMed]
- Inoue, Y.; Iwata, T.; Okugawa, Y.; Kawamoto, A.; Hiro, J.; Toiyama, Y.; Tanaka, K.; Uchida, K.; Mohri, Y.; Miki, C.; et al. Prognostic significance of a systemic inflammatory response in patients undergoing multimodality therapy for advanced colorectal cancer. Oncology 2013, 84, 100–107. [Google Scholar] [CrossRef] [PubMed]
- McMillan, D.C. Systemic inflammation, nutritional status and survival in patients with cancer. Curr. Opin. Clin. Nutr. Metab. Care 2009, 12, 223–226. [Google Scholar] [CrossRef] [PubMed]
- McMillan, D.C. An inflammation-based prognostic score and its role in the nutrition-based management of patients with cancer. Proc. Nutr. Soc. 2008, 67, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Maruyama, S.; Okamura, A.; Kanie, Y.; Sakamoto, K.; Fujiwara, D.; Kanamori, J.; Imamura, Y.; Kumagai, K.; Watanabe, M. C-reactive protein to prealbumin ratio: A useful inflammatory and nutritional index for predicting prognosis after curative resection in esophageal squamous cell carcinoma patients. Langenbeck’s Arch. Surg. 2022, 407, 1901–1909. [Google Scholar] [CrossRef] [PubMed]
- Aoyama, T.; Hashimoto, I.; Maezawa, Y.; Hara, K.; Komori, K.; Otani, K.; Kazama, K.; Sawazaki, S.; Numata, M.; Kamiya, N.; et al. The C-reactive Protein to Prealbumin Ratio is an Independent Prognostic Factor for Patients with Gastric Cancer Who Receive Curative Surgery. Anticancer Res. 2023, 43, 5181–5187. [Google Scholar] [CrossRef] [PubMed]
- Lu, J.; Xu, B.-B.; Zheng, Z.-F.; Xie, J.-W.; Wang, J.-B.; Lin, J.-X.; Chen, Q.-Y.; Cao, L.-L.; Lin, M.; Tu, R.-H.; et al. CRP/prealbumin, a novel inflammatory index for predicting recurrence after radical resection in gastric cancer patients: Post hoc analysis of a randomized phase III trial. Gastric Cancer 2019, 22, 536–545. [Google Scholar] [CrossRef] [PubMed]




| mGPS | PPS: Cut Off 15mg/dL | PPS: Cut Off 15mg/dL | |
|---|---|---|---|
| Score 0 | Alb ≥ 3.5g/dL and CRP ≤ 0.5mg/dL | Prealbumin ≥ 15 mg/dL and CRP ≤ 0.5mg/dL | Prealbumin ≥ 22 mg/dL and CRP ≤ 0.5mg/dL |
| Score 1 | Alb < 3.5g/dL or CRP > 0.5mg/dL | Prealbumin < 15 mg/dL or CRP > 0.5mg/dL | Prealbumin < 22 mg/dL or CRP > 0.5mg/dL |
| Score 2 | Alb < 3.5g/dL and CRP > 0.5mg/dL | Prealbumin < 15 mg/dL and CRP > 0.5mg/dL | Prealbumin < 22 mg/dL and CRP > 0.5mg/dL |
| Prealbumin Prognostic Score (Prealbumin Cutoff Value: 15 mg/dL) | PPS Score 0 N = 4190 | PPS Score 1 N = 386 | PPS Score 2 N = 87 | p Value |
|---|---|---|---|---|
| Age (years), Median (IQR) | 64.0 (56.0, 72.0) | 68.5 (60.3, 76.0) | 71.0 (65.0, 79.0) | <0.001 |
| Sex | 0.378 | |||
| Male | 2687 (64.1%) | 256 (66.3%) | 51 (58.6%) | |
| Female | 1503 (35.9%) | 130 (33.7%) | 36 (41.4%) | |
| Body mass index, Median (IQR) | 22.5 (20.5, 24.6) | 22.7 (20.2, 25.0) | 21.0 (19.3, 22.8) | <0.001 |
| Comorbidity | ||||
| Chronic kidney disease | 548 (13.1%) | 72 (18.7%) | 18 (20.7%) | 0.002 |
| Diabetes | 350 (8.4%) | 53 (13.7%) | 11 (12.6%) | 0.001 |
| CRP (mg/dL), Median (IQR) | 0.08 (0.03, 0.10) | 0.78 (0.51, 1.40) | 2.10 (1.13, 4.75) | <0.001 |
| Prealbumin (mg/dL), Median (IQR) | 26.7 (23.1, 30.7) | 20.3 (16.3, 24.4) | 13.2 (10.9, 14.2) | <0.001 |
| >22.0 | 3450 (82.3%) | 146 (37.8%) | 0 (0%) | |
| 15.0–22.0 | 740 (17.7%) | 171 (44.3%) | 0 (0%) | <0.001 |
| <15.0 | 0 (0%) | 69 (17.9%) | 87 (100%) | |
| Clinical stage | ||||
| I | 3108 (74.2%) | 194 (50.3%) | 25 (28.7%) | <0.001 |
| II | 512 (12.2%) | 69 (17.9%) | 10 (11.5%) | |
| III | 539 (12.9%) | 117 (30.3%) | 44 (50.6%) | |
| IVA | 31 (0.7%) | 6 (1.6%) | 8 (9.2%) | |
| Surgical approach | ||||
| Laparoscopic surgery | 2605 (62.2%) | 145 (37.6%) | 14 (16.1%) | <0.001 |
| Open surgery | 1585 (37.8%) | 241 (62.4%) | 73 (83.9%) | |
| Surgical procedure | ||||
| Distal gastrectomy | 2396 (57.2%) | 224 (58.0%) | 55 (63.2%) | <0.001 |
| Total gastrectomy | 840 (20.0%) | 118 (30.6%) | 29 (33.3%) | |
| Proximal gastrectomy | 195 (4.7%) | 7 (1.8%) | 1 (1.1%) | |
| Pylorus-preserving gastrectomy | 759 (18.1%) | 37 (9.6%) | 2 (2.3%) | |
| Lymph node dissection | ||||
| D1+ | 2408 (57.5%) | 145 (37.6%) | 20 (23.0%) | <0.001 |
| D2 | 1782 (42.5%) | 241 (62.4%) | 67 (77.0%) | |
| Serosal invasion | 667 (15.9%) | 153 (39.6%) | 53 (60.9%) | <0.001 |
| Lymph node metastasis | ||||
| N1 | 544 (13.0%) | 64 (16.6%) | 17 (19.5%) | <0.001 |
| N2 | 369 (8.8%) | 51 (13.2%) | 19 (21.8%) | |
| N3 | 328 (7.8%) | 62 (16.1%) | 13 (14.9%) | |
| Pathological stage | ||||
| I | 2809 (67.0%) | 180 (46.6%) | 24 (27.6%) | <0.001 |
| II | 724 (17.3%) | 88 (22.8%) | 19 (21.8%) | |
| III | 657 (15.7%) | 118 (30.6%) | 44 (50.6%) | |
| Histological type | ||||
| Differentiated | 1841 (43.9%) | 179 (46.4%) | 38 (43.7%) | 0.651 |
| Undifferentiated | 2349 (56.1%) | 207 (53.6%) | 49 (56.3%) | |
| Postoperative complications | ||||
| Overall complications | 820 (19.6%) | 97 (25.1%) | 20 (23.0%) | 0.026 |
| Severe complications | 284 (6.8%) | 30 (7.8%) | 11 (12.6%) | 0.085 |
| Adjuvant chemotherapy | 787 (18.8%) | 110 (28.5%) | 34 (39.1%) | <0.001 |
| Prealbumin Prognostic Score (Prealbumin Cutoff Value: 22 mg/dL) | PPS Score 0 N = 3421 | PPS Score 1 N = 984 | PPS Score 2 N = 258 | p Value |
|---|---|---|---|---|
| Age (years), Median (IQR) | 64.0 (56.0, 71.0) | 68.0 (57.0, 76.0) | 70.0 (64.0, 78.0) | <0.001 |
| Sex | <0.001 | |||
| Male | 2377 (69.5%) | 458 (46.5%) | 159 (61.6%) | |
| Female | 1044 (30.5%) | 526 (53.5%) | 99 (38.4%) | |
| Body mass index, Median (IQR) | 22.7 (20.7, 24.7) | 21.6 (19.4, 24.3) | 21.5 (19.8, 24.1) | <0.001 |
| Comorbidity | ||||
| Chronic kidney disease | 449 (13.1%) | 138 (14.0%) | 51 (19.8%) | 0.011 |
| Diabetes | 257 (7.5%) | 120 (12.2%) | 37 (14.3%) | <0.001 |
| CRP (mg/dL), Median (IQR) | 0.08 (0.03, 0.10) | 0.10 (0.05, 0.30) | 1.30 (0.74, 2.28) | <0.001 |
| Prealbumin (mg/dL), Median (IQR) | 28.1 (25.2, 31.5) | 20.3 (18.1, 21.6) | 17.1 (14.2, 19.8) | <0.001 |
| >22.0 | 3421 (100.0%) | 175 (17.8%) | 0 (0%) | |
| 15.0–22.0 | 0 (0%) | 740 (75.2%) | 171 (66.3%) | <0.001 |
| <15.0 | 0 (0%) | 69 (7.0%) | 87 (33.7%) | |
| Clinical stage | ||||
| I | 2599 (76.0%) | 630 (64.0%) | 98 (38.0%) | <0.001 |
| II | 406 (11.9%) | 139 (14.1%) | 46 (17.8%) | |
| III | 397 (11.6%) | 199 (20.2%) | 104 (40.3%) | |
| IVA | 19 (0.6%) | 16 (1.6%) | 10 (3.9%) | |
| Surgical approach | ||||
| Laparoscopic surgery | 2198 (64.3%) | 496 (50.4%) | 70 (27.1%) | <0.001 |
| Open surgery | 1223 (35.7%) | 488 (49.6%) | 188 (72.9%) | |
| Surgical procedure | ||||
| Distal gastrectomy | 1929 (56.4%) | 593 (60.3%) | 153 (59.3%) | <0.001 |
| Total gastrectomy | 679 (19.8%) | 220 (22.4%) | 88 (34.1%) | |
| Proximal gastrectomy | 166 (4.9%) | 33 (3.4%) | 4 (1.6%) | |
| Pylorus-preserving gastrectomy | 647 (18.9%) | 138 (14.0%) | 13 (5.0%) | |
| Lymph node dissection | ||||
| D1+ | 2009 (58.7%) | 491 (49.9%) | 73 (28.3%) | <0.001 |
| D2 | 1412 (41.3%) | 493 (50.1%) | 185 (71.7%) | |
| Serosal invasion | 477 (13.9%) | 266 (27.0%) | 130 (50.4%) | <0.001 |
| Lymph node metastasis | ||||
| N1 | 433 (12.7%) | 137 (13.9%) | 55 (21.3%) | <0.001 |
| N2 | 289 (8.4%) | 108 (11.0%) | 42 (16.3%) | |
| N3 | 236 (6.9%) | 125 (12.7%) | 42 (16.3%) | |
| Pathological stage | ||||
| I | 2350 (68.7%) | 571 (58.0%) | 92 (35.7%) | <0.001 |
| II | 582 (17.0%) | 186 (18.9%) | 63 (24.4%) | |
| III | 489 (14.3%) | 227 (23.1%) | 103 (39.9%) | |
| Histological type | ||||
| Differentiated | 1507 (44.1%) | 431 (43.8%) | 120 (46.5%) | 0.724 |
| Undifferentiated | 1914 (55.9%) | 553 (56.2%) | 138 (53.5%) | |
| Postoperative complications | ||||
| Overall complications | 682 (19.9%) | 194 (19.7%) | 61 (23.6%) | 0.339 |
| Severe complications | 233 (6.8%) | 67 (6.8%) | 25 (9.7%) | 0.210 |
| Adjuvant chemotherapy | 630 (18.4%) | 208 (21.1%) | 93 (36.0%) | <0.001 |
| Variables | Prealbumin Cutoff Value: 15 mg/dL | Prealbumin Cutoff Value: 22 mg/dL | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Univariate Analysis | Multivariate Analysis | Univariate Analysis | Multivariate Analysis | |||||||||
| HR | 95% CI | p Value | HR | 95% CI | p Value | HR | 95% CI | p Value | HR | 95% CI | p Value | |
| Sex | ||||||||||||
| Female | 1 | 1 | 1 | 1 | ||||||||
| Male | 1.463 | 1.266–1.691 | <0.001 | 1.482 | 1.279–1.719 | <0.001 | 1.463 | 1.266–1.691 | <0.001 | 1.582 | 1.362–1.838 | <0.001 |
| Age (years) | ||||||||||||
| <70 | 1 | 1 | 1 | 1 | ||||||||
| ≥70 | 2.988 | 2.619–3.408 | <0.001 | 2.701 | 2.353–3.100 | <0.001 | 2.988 | 2.619–3.408 | <0.001 | 2.552 | 2.219–2.935 | <0.001 |
| Surgical procedure | ||||||||||||
| Non-TG | 1 | 1 | 1 | 1 | ||||||||
| TG | 2.644 | 2.314–3.022 | <0.001 | 1.597 | 1.383–1.846 | <0.001 | 2.644 | 2.314–3.022 | <0.001 | 1.591 | 1.378–1.836 | <0.001 |
| Surgical approach | ||||||||||||
| Laparoscopy | 1 | 1 | 1 | 1 | ||||||||
| Open | 3.552 | 3.092–4.080 | <0.001 | 2.323 | 1.844–2.926 | <0.001 | 3.552 | 3.092–4.080 | <0.001 | 2.164 | 1.719–2.723 | <0.001 |
| Lymph node dissection | ||||||||||||
| D1+ | 1 | 1 | 1 | 1 | ||||||||
| D2 | 2.454 | 2.143–2.809 | <0.001 | 0.693 | 0.553–0.868 | 0.001 | 2.454 | 2.143–2.809 | <0.001 | 0.711 | 0.568–0.889 | 0.003 |
| pStage | ||||||||||||
| I, II | 1 | 1 | 1 | 1 | ||||||||
| III | 4.747 | 4.157–5.419 | <0.001 | 3.300 | 2.737–3.977 | <0.001 | 4.747 | 4.157–5.419 | <0.001 | 3.228 | 2.676–3.893 | <0.001 |
| Histological type | ||||||||||||
| Differentiated | 1 | 1 | 1 | 1 | ||||||||
| Undifferentiated | 0.856 | 0.751–0.975 | 0.019 | 0.988 | 0.861–1.134 | 0.866 | 0.856 | 0.751–0.975 | 0.019 | 0.990 | 0.863–1.136 | 0.884 |
| Score | ||||||||||||
| 0 | 1 | 1 | 1 | 1 | ||||||||
| 1 | 1.893 | 1.567–2.286 | <0.001 | 1.113 | 0.916–1.353 | 0.283 | 1.905 | 1.656–2.192 | <0.001 | 1.603 | 1.378–1.866 | <0.001 |
| 2 | 3.087 | 2.256–4.224 | <0.001 | 1.396 | 1.010–1.928 | 0.043 | 2.407 | 1.957–2.960 | <0.001 | 1.322 | 1.055–1.656 | 0.015 |
| Postoperative complication | ||||||||||||
| Absent | 1 | 1 | 1 | 1 | ||||||||
| Overall complications | 1.603 | 1.385–1.856 | <0.001 | 1.603 | 1.385–1.856 | <0.001 | ||||||
| Severe complications | 1.698 | 1.365–2.111 | <0.001 | 1.268 | 1.016–1.583 | 0.036 | 1.698 | 1.365–2.111 | <0.001 | 1.272 | 1.019–1.588 | 0.033 |
| Adjuvant chemotherapy | ||||||||||||
| Absent | 1 | 1 | 1 | 1 | ||||||||
| Present | 2.354 | 2.050–2.702 | <0.001 | 0.894 | 0.747–1.069 | 0.218 | 2.354 | 2.050–2.702 | <0.001 | 0.917 | 0.766–1.098 | 0.346 |
| Variables | CRP < 0.5 mg/dL | CRP ≥ 0.5 mg/dL | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Univariate Analysis | Multivariate Analysis | Univariate Analysis | Multivariate Analysis | |||||||||
| HR | 95% CI | p Value | HR | 95% CI | p Value | HR | 95% CI | p Value | HR | 95% CI | p Value | |
| Sex | ||||||||||||
| Female | 1 | 1 | 1 | 1 | ||||||||
| Male | 1.399 | 1.198–1.634 | <0.001 | 1.541 | 1.310–1.812 | <0.001 | 1.963 | 1.303–2.958 | 0.001 | 2.454 | 1.598–3.770 | <0.001 |
| Age (years) | ||||||||||||
| <70 | 1 | 1 | 1 | 1 | ||||||||
| ≥70 | 2.998 | 2.601–3.455 | <0.001 | 2.705 | 2.325–3.148 | <0.001 | 2.316 | 1.622–3.309 | <0.001 | 1.794 | 1.235–2.606 | 0.002 |
| Surgical procedure | ||||||||||||
| Non-TG | 1 | 1 | 1 | 1 | ||||||||
| TG | 2.671 | 2.311–3.087 | <0.001 | 1.653 | 1.415–1.930 | <0.001 | 2.071 | 1.466–2.927 | <0.001 | 1.616 | 1.087–2.404 | 0.018 |
| Surgical approach | ||||||||||||
| Laparoscopy | 1 | 1 | 1 | 1 | ||||||||
| Open | 3.570 | 3.079–4.139 | <0.001 | 1.966 | 1.534–2.519 | <0.001 | 2.443 | 1.608–3.712 | <0.001 | 2.458 | 1.317–4.588 | 0.005 |
| Lymph node dissection | ||||||||||||
| D1+ | 1 | 1 | 1 | 1 | ||||||||
| D2 | 2.531 | 2.189–2.927 | <0.001 | 0.757 | 0.594–0.964 | 0.024 | 1.443 | 0.994–2.095 | 0.054 | 0.536 | 0.308–0.936 | 0.028 |
| pStage | ||||||||||||
| I, II | 1 | 1 | 1 | 1 | ||||||||
| III | 5.176 | 4.484–5.975 | <0.001 | 3.464 | 2.823–4.251 | <0.001 | 2.284 | 1.614–3.232 | <0.001 | 1.816 | 1.147–2.877 | 0.011 |
| Histological type | ||||||||||||
| Differentiated | 1 | 1 | 1 | 1 | ||||||||
| Undifferentiated | 0.862 | 0.749–0.992 | 0.038 | 0.986 | 0.849–1.146 | 0.857 | 0.831 | 0.590–1.172 | 0.291 | 0.949 | 0.661–1.362 | 0.777 |
| Prealbumin (mg/dL) | ||||||||||||
| High | 1 | 1 | 1 | 1 | ||||||||
| Moderate | 2.075 | 1.774–2.429 | <0.001 | 1.672 | 1.414–1.976 | <0.001 | 1.147 | 0.813–1.618 | 0.434 | 1.602 | 0.992–2.588 | 0.054 |
| Low | 3.756 | 2.676–5.273 | <0.001 | 1.806 | 1.266–2.576 | 0.001 | 2.073 | 1.428–3.008 | <0.001 | 2.589 | 1.520–4.409 | <0.001 |
| Postoperative complication | ||||||||||||
| Absent | 1 | 1 | 1 | 1 | ||||||||
| Overall complications | 1.656 | 1.414–1.940 | <0.001 | 1.169 | 0.791–1.729 | 0.434 | ||||||
| Severe complications | 1.698 | 1.340–2.152 | <0.001 | 1.242 | 0.976–1.581 | 0.078 | 1.645 | 0.941–2.875 | 0.081 | 1.424 | 0.798–2.540 | 0.231 |
| Adjuvant chemotherapy | ||||||||||||
| Absent | 1 | 1 | 1 | 1 | ||||||||
| Present | 2.512 | 2.163–2.916 | <0.001 | 1.027 | 0.844–1.250 | 0.790 | 1.273 | 0.888–1.825 | 0.189 | 0.624 | 0.391–0.997 | 0.049 |
| Variables | pStage I, II | pStage III | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Univariate Analysis | Multivariate Analysis | Univariate Analysis | Multivariate Analysis | |||||||||
| HR | 95% CI | p Value | HR | 95% CI | p Value | HR | 95% CI | p Value | HR | 95% CI | p Value | |
| Sex | ||||||||||||
| Female | 1 | 1 | 1 | 1 | ||||||||
| Male | 1.731 | 1.419–2.111 | <0.001 | 1.929 | 1.567–2.376 | <0.001 | 1.236 | 0.998–1.532 | 0.053 | 1.252 | 1.006–1.558 | 0.044 |
| Age (years) | ||||||||||||
| <70 | 1 | 1 | 1 | 1 | ||||||||
| ≥70 | 4.859 | 4.059–5.817 | <0.001 | 4.159 | 3.444–5.024 | <0.001 | 1.432 | 1.165–1.759 | <0.001 | 1.206 | 0.963–1.509 | 0.103 |
| Surgical procedure | ||||||||||||
| Non-TG | 1 | 1 | 1 | 1 | ||||||||
| TG | 2.311 | 1.923–2.777 | <0.001 | 1.722 | 1.415–2.095 | <0.001 | 1.439 | 1.176–1.760 | <0.001 | 1.376 | 1.119–1.692 | 0.002 |
| Surgical approach | ||||||||||||
| Laparoscopy | 1 | 1 | 1 | 1 | ||||||||
| Open | 2.298 | 1.937–2.726 | <0.001 | 1.679 | 1.303–2.164 | <0.001 | 1.446 | 0.876–2.388 | 0.149 | 1.963 | 1.117–3.452 | 0.019 |
| Lymph node dissection | ||||||||||||
| D1+ | 1 | 1 | 1 | 1 | ||||||||
| D2 | 1.526 | 1.284–1.812 | <0.001 | 0.797 | 0.621–1.023 | 0.075 | 0.590 | 0.404–0.863 | 0.006 | 0.480 | 0.314–0.734 | <0.001 |
| Histological type | ||||||||||||
| Differentiated | 1 | 1 | 1 | 1 | ||||||||
| Undifferentiated | 0.594 | 0.499–0.707 | <0.001 | 0.957 | 0.780–1.147 | 0.631 | 0.972 | 0.783–1.205 | 0.794 | 1.140 | 0.913–1.423 | 0.249 |
| Score (Prealbumin cutoff: 15) | ||||||||||||
| 0 | 1 | 1 | 1 | 1 | ||||||||
| 1 | 2.086 | 1.737–2.506 | <0.001 | 2.027 | 1.664–2.469 | <0.001 | 1.258 | 1.010–1.565 | 0.040 | 1.212 | 0.957–1.534 | 0.110 |
| 2 | 3.000 | 2.269–3.967 | <0.001 | 2.535 | 1.879–3.420 | <0.001 | 0.981 | 0.720–1.335 | 0.902 | 0.962 | 0.692–1.337 | 0.817 |
| Postoperative complication | ||||||||||||
| Absent | 1 | 1 | 1 | 1 | ||||||||
| Overall complications | 1.480 | 1.212–1.808 | <0.001 | 1.250 | 1.006–1.553 | 0.044 | ||||||
| Severe complications | 1.535 | 1.128–2.091 | 0.006 | 1.194 | 0.873–1.632 | 0.267 | 1.444 | 1.061–1.966 | 0.020 | 1.269 | 0.923–1.746 | 0.143 |
| Adjuvant chemotherapy | ||||||||||||
| Absent | 1 | 1 | 1 | 1 | ||||||||
| Present | 1.848 | 1.454–2.349 | <0.001 | 1.706 | 1.313–2.217 | <0.001 | 0.520 | 0.423–0.640 | <0.001 | 0.564 | 0.453–0.701 | <0.001 |
| Variables | Prealbumin Cutoff Value: 15 mg/dL | Prealbumin Cutoff Value: 22 mg/dL | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Univariate Analysis | Multivariate Analysis | Univariate Analysis | Multivariate Analysis | |||||||||
| HR | 95% CI | p Value | HR | 95% CI | p Value | HR | 95% CI | p Value | HR | 95% CI | p Value | |
| Sex | ||||||||||||
| Female | 1 | 1 | 1 | 1 | ||||||||
| Male | 1.415 | 1.229–1.629 | <0.001 | 1.416 | 1.226–1.636 | <0.001 | 1.415 | 1.229–1.629 | <0.001 | 1.498 | 1.294–1.733 | <0.001 |
| Age (years) | ||||||||||||
| <70 | 1 | 1 | 1 | 1 | ||||||||
| ≥70 | 2.883 | 2.534–3.279 | <0.001 | 2.607 | 2.277–2.985 | <0.001 | 2.883 | 2.534–3.279 | <0.001 | 2.479 | 2.161–2.843 | <0.001 |
| Surgical procedure | ||||||||||||
| Non-TG | 1 | 1 | 1 | 1 | ||||||||
| TG | 2.662 | 2.336–3.035 | <0.001 | 1.542 | 1.339–1.776 | <0.001 | 2.662 | 2.336–3.035 | <0.001 | 1.542 | 1.339–1.775 | <0.001 |
| Surgical approach | ||||||||||||
| Laparoscopy | 1 | 1 | 1 | 1 | ||||||||
| Open | 3.719 | 3.245–4.263 | <0.001 | 2.291 | 1.824–2.877 | <0.001 | 3.719 | 3.245–4.263 | <0.001 | 2.149 | 1.712–2.698 | <0.001 |
| Lymph node dissection | ||||||||||||
| D1+ | 1 | 1 | 1 | 1 | ||||||||
| D2 | 2.602 | 2.277–2.972 | <0.001 | 0.717 | 0.574–0.895 | 0.003 | 2.602 | 2.277–2.972 | <0.001 | 0.733 | 0.588–0.915 | 0.006 |
| pStage | ||||||||||||
| I, II | 1 | 1 | 1 | 1 | ||||||||
| III | 5.191 | 4.560–5.910 | <0.001 | 3.409 | 2.844–4.085 | <0.001 | 5.191 | 4.560–5.910 | <0.001 | 3.334 | 2.781–3.998 | <0.001 |
| Histological type | ||||||||||||
| Differentiated | 1 | 1 | 1 | 1 | ||||||||
| Undifferentiated | 0.861 | 0.758–0.979 | 0.022 | 0.959 | 0.838–1.098 | 0.543 | 0.861 | 0.758–0.979 | 0.022 | 0.961 | 0.840–1.100 | 0.565 |
| Score | ||||||||||||
| 0 | 1 | 1 | 1 | 1 | ||||||||
| 1 | 1.877 | 1.560–2.259 | <0.001 | 1.090 | 0.900–1.320 | 0.376 | 1.855 | 1.617–2.129 | <0.001 | 1.520 | 1.309–1.763 | <0.001 |
| 2 | 3.018 | 2.214–4.113 | <0.001 | 1.297 | 0.943–1.784 | 0.110 | 2.368 | 1.931–2.903 | <0.001 | 1.248 | 1.000–1.558 | 0.049 |
| Postoperative complication | ||||||||||||
| Absent | 1 | 1 | 1 | 1 | ||||||||
| Overall complications | 1.578 | 1.367–1.823 | <0.001 | 1.578 | 1.367–1.823 | <0.001 | ||||||
| Severe complications | 1.761 | 1.426–2.176 | <0.001 | 1.310 | 1.056–1.624 | 0.014 | 1.761 | 1.426–2.176 | <0.001 | 1.318 | 1.063–1.634 | 0.012 |
| Adjuvant chemotherapy | ||||||||||||
| Absent | 1 | 1 | 1 | 1 | ||||||||
| Present | 2.585 | 2.260–2.956 | <0.001 | 0.989 | 0.831–1.176 | 0.898 | 2.585 | 2.260–2.956 | <0.001 | 1.011 | 0.850–1.204 | 0.898 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matsui, R.; Nunobe, S.; Ri, M.; Makuuchi, R.; Irino, T.; Hayami, M.; Ohashi, M.; Sano, T. Prealbumin Prognostic Score: A Novel Prognostic Indicator After Radical Gastrectomy in Patients with Gastric Cancer. Cancers 2024, 16, 3889. https://doi.org/10.3390/cancers16223889
Matsui R, Nunobe S, Ri M, Makuuchi R, Irino T, Hayami M, Ohashi M, Sano T. Prealbumin Prognostic Score: A Novel Prognostic Indicator After Radical Gastrectomy in Patients with Gastric Cancer. Cancers. 2024; 16(22):3889. https://doi.org/10.3390/cancers16223889
Chicago/Turabian StyleMatsui, Ryota, Souya Nunobe, Motonari Ri, Rie Makuuchi, Tomoyuki Irino, Masaru Hayami, Manabu Ohashi, and Takeshi Sano. 2024. "Prealbumin Prognostic Score: A Novel Prognostic Indicator After Radical Gastrectomy in Patients with Gastric Cancer" Cancers 16, no. 22: 3889. https://doi.org/10.3390/cancers16223889
APA StyleMatsui, R., Nunobe, S., Ri, M., Makuuchi, R., Irino, T., Hayami, M., Ohashi, M., & Sano, T. (2024). Prealbumin Prognostic Score: A Novel Prognostic Indicator After Radical Gastrectomy in Patients with Gastric Cancer. Cancers, 16(22), 3889. https://doi.org/10.3390/cancers16223889








