Analysis of Swallowing Functional Preservation by Surgical Versus CRT After Induction Chemotherapy for Oropharyngeal Cancer
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Surgery After Induction Chemotherapy (IC–Surgery)
2.2. Chemoradiation Therapy After Induction Chemotherapy (IC-CRT)
Subgroup Analysis in Advanced Oropharyngeal Cancer
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vigneswaran, N.; Williams, M.D. Epidemiologic trends in head and neck cancer and aids in diagnosis. Oral Maxillofac. Surg. Clin. N. Am. 2014, 26, 123–141. [Google Scholar] [CrossRef] [PubMed]
- Tshering Vogel, D.W.; Zbaeren, P.; Thoeny, H.C. Cancer of the oral cavity and oropharynx. Cancer Imaging 2010, 10, 62–72. [Google Scholar] [CrossRef] [PubMed]
- Herrero, R.; Castellsagué, X.; Pawlita, M.; Lissowska, J.; Kee, F.; Balaram, P.; Rajkumar, T.; Sridhar, H.; Rose, B.; Pintos, J.; et al. Human papillomavirus and oral cancer: The International Agency for Research on Cancer multicenter study. J. Natl. Cancer Inst. 2003, 95, 1772–1783. [Google Scholar] [CrossRef] [PubMed]
- Shiboski, C.H.; Schmidt, B.L.; Jordan, R.C. Tongue and tonsil carcinoma: Increasing trends in the U.S. population ages 20–44 years. Cancer 2005, 103, 1843–1849. [Google Scholar] [CrossRef] [PubMed]
- Abnet, C.C.; Arnold, M.; Wei, W.Q. Epidemiology of esophageal squamous cell carcinoma. Gastroenterology 2018, 154, 360–373. [Google Scholar] [CrossRef]
- Skoretz, S.A.; Anger, N.; Wellman, L.; Takai, O.; Empey, A. A systematic review of tracheostomy modifications and swallowing in adults. Dysphagia 2020, 35, 935–947. [Google Scholar] [CrossRef]
- de Bruijn, M.J.; ten Bosch, L.; Kuik, D.J.; Quené, H.; Langendijk, J.A.; Leemans, C.R.; Verdonck-de Leeuw, I.M. Objective acoustic-phonetic speech analysis in patients treated for oral or oropharyngeal cancer. Folia Phoniatr. Logop. 2009, 61, 180–187. [Google Scholar] [CrossRef]
- Bressan, V.; Stevanin, S.; Bianchi, M.; Aleo, G.; Bagnasco, A.; Sasso, L. The effects of swallowing disorders, dysgeusia, oral mucositis and xerostomia on nutritional status, oral intake and weight loss in head and neck cancer patients: A systematic review. Cancer Treat. Rev. 2016, 45, 105–119. [Google Scholar] [CrossRef]
- Nguyen, N.P.; Moltz, C.C.; Frank, C.; Vos, P.; Smith, H.J.; Karlsson, U.; Dutta, S.; Midyett, F.A.; Barloon, J.; Sallah, S. Dysphagia following chemoradiation for locally advanced head and neck cancer. Ann. Oncol. 2004, 15, 383–388. [Google Scholar] [CrossRef]
- Caudell, J.J.; Schaner, P.E.; Meredith, R.F.; Locher, J.L.; Nabell, L.M.; Carroll, W.R.; Magnuson, J.S.; Spencer, S.A.; Bonner, J.A. Factors associated with long-term dysphagia after definitive radiotherapy for locally advanced head-and-neck cancer. Int. J. Radiat. Oncol. Biol. Phys. 2009, 73, 410–415. [Google Scholar] [CrossRef]
- Maniaci, A.; Hao, S.P.; Cancemi, F.; Giardini, D.; Checcoli, E.; Soprani, F.; Iannella, G.; Vicini, C.; Cocuzza, S.; La Mantia, I.; et al. Surgical treatment for advanced oropharyngeal cancer: A narrative review. Medicina 2023, 59, 304. [Google Scholar] [CrossRef] [PubMed]
- Carmignani, I.; Locatello, L.G.; Desideri, I.; Bonomo, P.; Olmetto, E.; Livi, L.; Le Saec, O.; Coscarelli, S.; Mannelli, G. Analysis of dysphagia in advanced-stage head-and-neck cancer patients: Impact on quality of life and development of a preventive swallowing treatment. Eur. Arch. Otorhinolaryngol. 2018, 275, 2159–2167. [Google Scholar] [CrossRef] [PubMed]
- Kreeft, A.M.; van der Molen, L.; Hilgers, F.J.; Balm, A.J. Speech and swallowing after surgical treatment of advanced oral and oropharyngeal carcinoma: A systematic review of the literature. Eur. Arch. Otorhinolaryngol. 2009, 266, 1687–1698. [Google Scholar] [CrossRef] [PubMed]
- Gillespie, M.B.; Brodsky, M.B.; Day, T.A.; Sharma, A.K.; Lee, F.S.; Martin-Harris, B. Laryngeal penetration and aspiration during swallowing after the treatment of advanced oropharyngeal cancer. Arch. Otolaryngol. Head. Neck Surg. 2005, 131, 615–619. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Høxbroe Michaelsen, S.; Grønhøj, C.; Høxbroe Michaelsen, J.; Friborg, J.; von Buchwald, C. Quality of life in survivors of oropharyngeal cancer: A systematic review and meta-analysis of 1366 patients. Eur. J. Cancer 2017, 78, 91–102. [Google Scholar] [CrossRef]
- Huang, S.H.; O’Sullivan, B.; Waldron, J. Current indications for postoperative radiation therapy for head and neck cancer. JAMA Otolaryngol. Head. Neck Surg. 2018, 144, 167–174. [Google Scholar]
- Mirghani, H.; Blanchard, P. Treatment de-escalation for HPV-driven oropharyngeal cancer: Where do we stand? Clin. Transl. Radiat. Oncol. 2017, 2, 6–13. [Google Scholar] [CrossRef]
- Zanoni, D.K.; Patel, S.G.; Shah, J.P. Changes in the 8th Edition of the American Joint Committee on Cancer (AJCC) Staging of Head and Neck Cancer: Rationale and Implications. Curr. Oncol. Rep. 2019, 21, 52. [Google Scholar] [CrossRef]
- Woods, R.S.; O’Regan, E.M.; Kennedy, S.; Martin, C.; O’Leary, J.J.; Timon, C. Role of human papillomavirus in oropharyngeal squamous cell carcinoma: A review. World J. Clin. Cases 2014, 2, 172–193. [Google Scholar] [CrossRef]
- Mahal, B.A.; Catalano, P.J.; Haddad, R.I.; Hanna, G.J.; Kass, J.I.; Schoenfeld, J.D.; Tishler, R.B.; Margalit, D.N. Incidence and demographic burden of HPV-associated oropharyngeal head and neck cancers in the United States. Cancer Epidemiol. Biomark. Prev. 2019, 28, 1660–1667. [Google Scholar] [CrossRef]
- Vidal, L.; Gillison, M.L. Human papillomavirus in HNSCC: Recognition of a distinct disease type. Hematol. Oncol. Clin. N. Am. 2008, 22, 1125–1142. [Google Scholar] [CrossRef] [PubMed]
- Dowthwaite, S.A.; Franklin, J.H.; Palma, D.A.; Fung, K.; Yoo, J.; Nichols, A.C. The role of transoral robotic surgery in the management of oropharyngeal cancer: A review of the literature. ISRN Oncol. 2012, 2012, 945162. [Google Scholar] [CrossRef] [PubMed]
- Haughey, B.H.; Hinni, M.L.; Salassa, J.R.; Hayden, R.E.; Grant, D.G.; Rich, J.T.; Milov, S.; Lewis, J.S., Jr.; Krishna, M. Transoral laser microsurgery as primary treatment for advanced-stage oropharyngeal cancer: A United States multicenter study. Head. Neck 2011, 33, 1683–1694. [Google Scholar] [CrossRef] [PubMed]
- Perez, C.A.; Patel, M.M.; Chao, K.S.; Simpson, J.R.; Sessions, D.; Spector, G.J.; Haughey, B.; Lockett, M.A. Carcinoma of the tonsillar fossa: Prognostic factors and long-term therapy outcome. Int. J. Radiat. Oncol. Biol. Phys. 1998, 42, 1077–1084. [Google Scholar] [CrossRef] [PubMed]
- Gomes, C.A., Jr.; Andriolo, R.B.; Bennett, C.; Lustosa, S.A.; Matos, D.; Waisberg, D.R.; Waisberg, J. Percutaneous endoscopic gastrostomy versus nasogastric tube feeding for adults with swallowing disturbances. Cochrane Database Syst. Rev. 2015, 2015, CD008096. [Google Scholar] [CrossRef]
- Corry, J.; Poon, W.; McPhee, N.; Milner, A.D.; Cruickshank, D.; Porceddu, S.V.; Rischin, D.; Peters, L.J. Randomized study of percutaneous endoscopic gastrostomy versus nasogastric tubes for enteral feeding in head and neck cancer patients treated with (chemo)radiation. J. Med. Imaging Radiat. Oncol. 2008, 52, 503–510. [Google Scholar] [CrossRef]
- Zaherah Mohamed Shah, F.; Suraiya, H.S.; Poi, P.J.; Tan, K.S.; Lai, P.S.; Ramakrishnan, K.; Mahadeva, S. Long-term nasogastric tube feeding in elderly stroke patients: An assessment of nutritional adequacy and attitudes to gastrostomy feeding in Asians. J. Nutr. Health Aging 2012, 16, 701–706. [Google Scholar] [CrossRef]
- Haxhija, E.Q.; Demiri, A.H.; Haxhija, D.H. Oropharyngeal dysphagia and head and neck cancer. J. Clin. Med. Res. 2014, 6, 329–335. [Google Scholar]
- Cohen, D.L.; Roffe, C.; Beavan, J.; Blackett, J.W. Dysphagia and quality of life after head and neck cancer treatment. Head. Neck 2019, 41, 778–783. [Google Scholar]
- Gaziano, J.E. Evaluation and management of oropharyngeal Dysphagia in head and neck cancer. Cancer Control 2002, 9, 400–409. [Google Scholar] [CrossRef]
- Groher, M.E. Mechanical disorders in swallowing. In Diagnosis and Management, 3rd ed.; Groher, M.E., Ed.; Dysphagia: Boston, MA, USA; Butterworth-Heinemann: Oxford, UK, 1997; pp. 73–106. [Google Scholar]
- Sessions, D.G.; Zill, R.; Schwartz, S.L. Deglutition after conservation surgery for cancer of the larynx and hypopharynx. Otolaryngol. Head. Neck Surg. 1979, 87, 779–796. [Google Scholar] [CrossRef] [PubMed]
| Items | Values (Total n =267) | Hazard Ratio (95% CI) | p-Value |
|---|---|---|---|
| Age | 54.55 ± 9.85 | 0.98 (0.97~1.02) | 0.94 |
| Male sex, no. (%) | 254 (95.13%) | 0.36 (0.15~0.62) | 0.01 * |
| Alcohol, no. (%) | 217 (81.27%) | 1.06 (0.64~1.74) | 0.81 |
| Betel nut, no. (%) | 205 (76.77%) | 1.08 (0.68~1.71) | 0.73 |
| Cigarette, no. (%) | 234 (87.64%) | 1.26 (0.71~2.23) | 0.42 |
| HPV-positive (%) | 81 (30.34%) | 0.54 (0.21~0.78) | 0.65 |
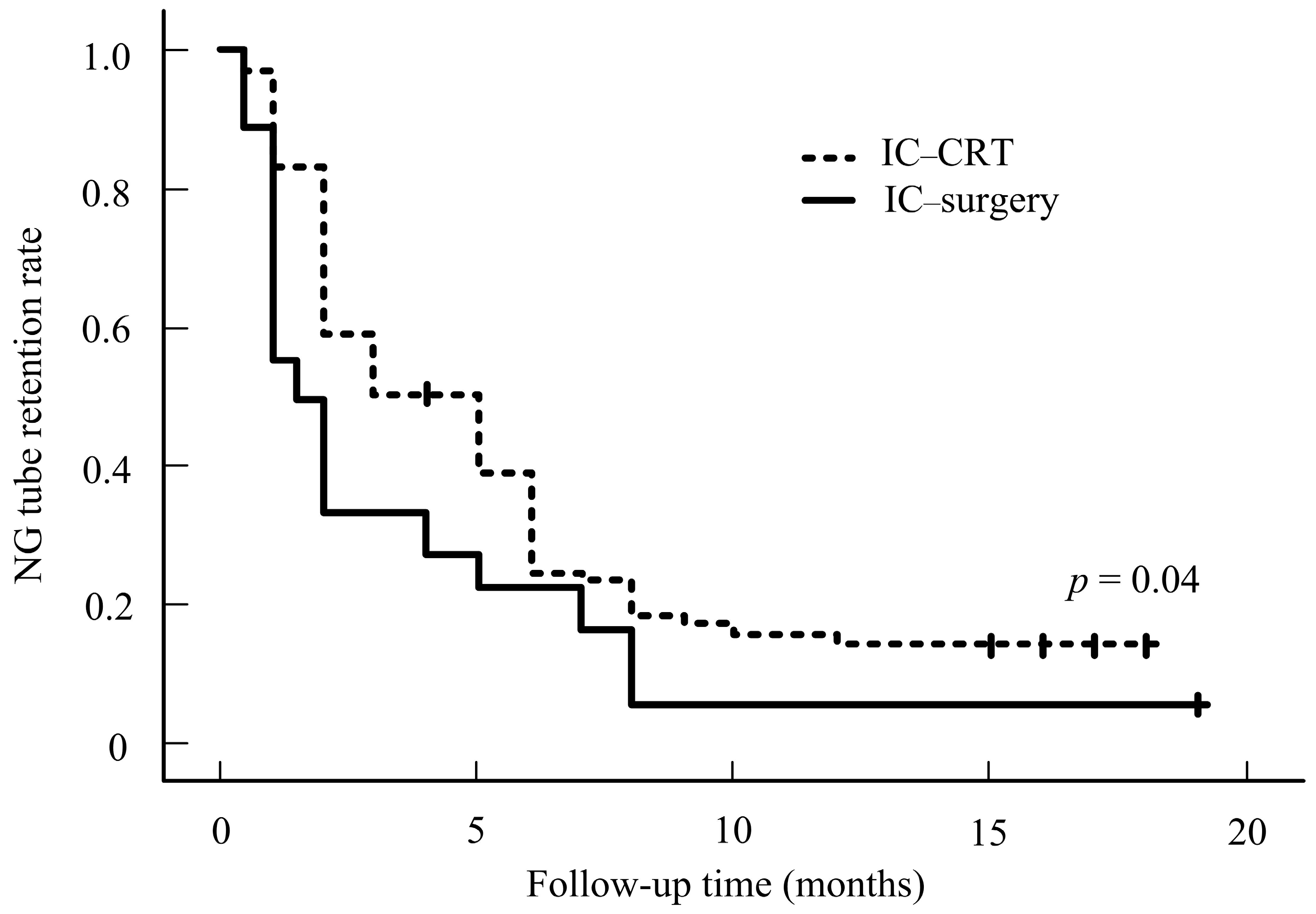
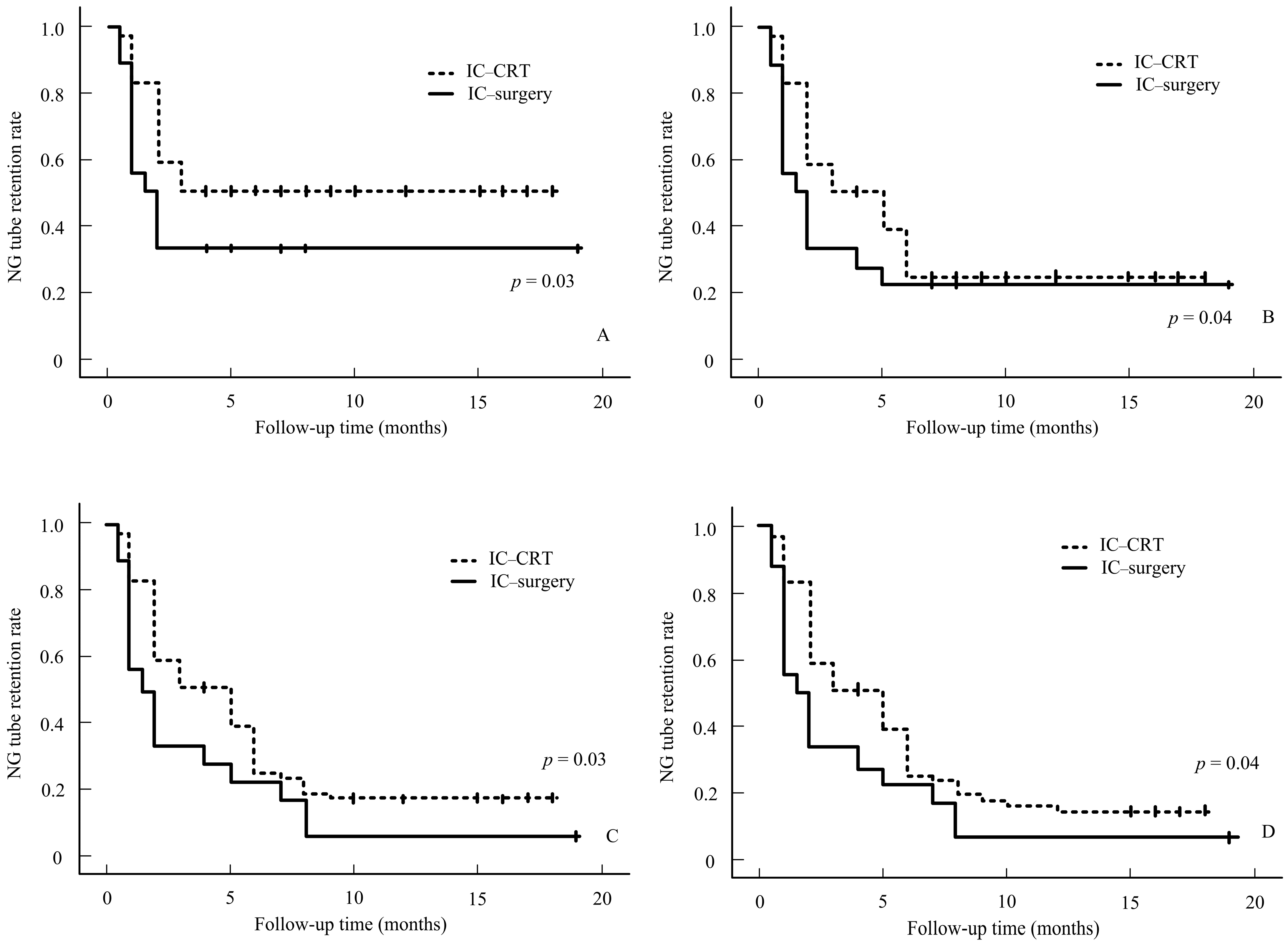
| IC–surgery | 171 (64.04%) | 0.23 (0.12~0.42) | 0.01 * |
| IC-CRT | 96 (35.95%) | 2.77 (1.82~4.22) | 0.01 * |
| Cancer stage | |||
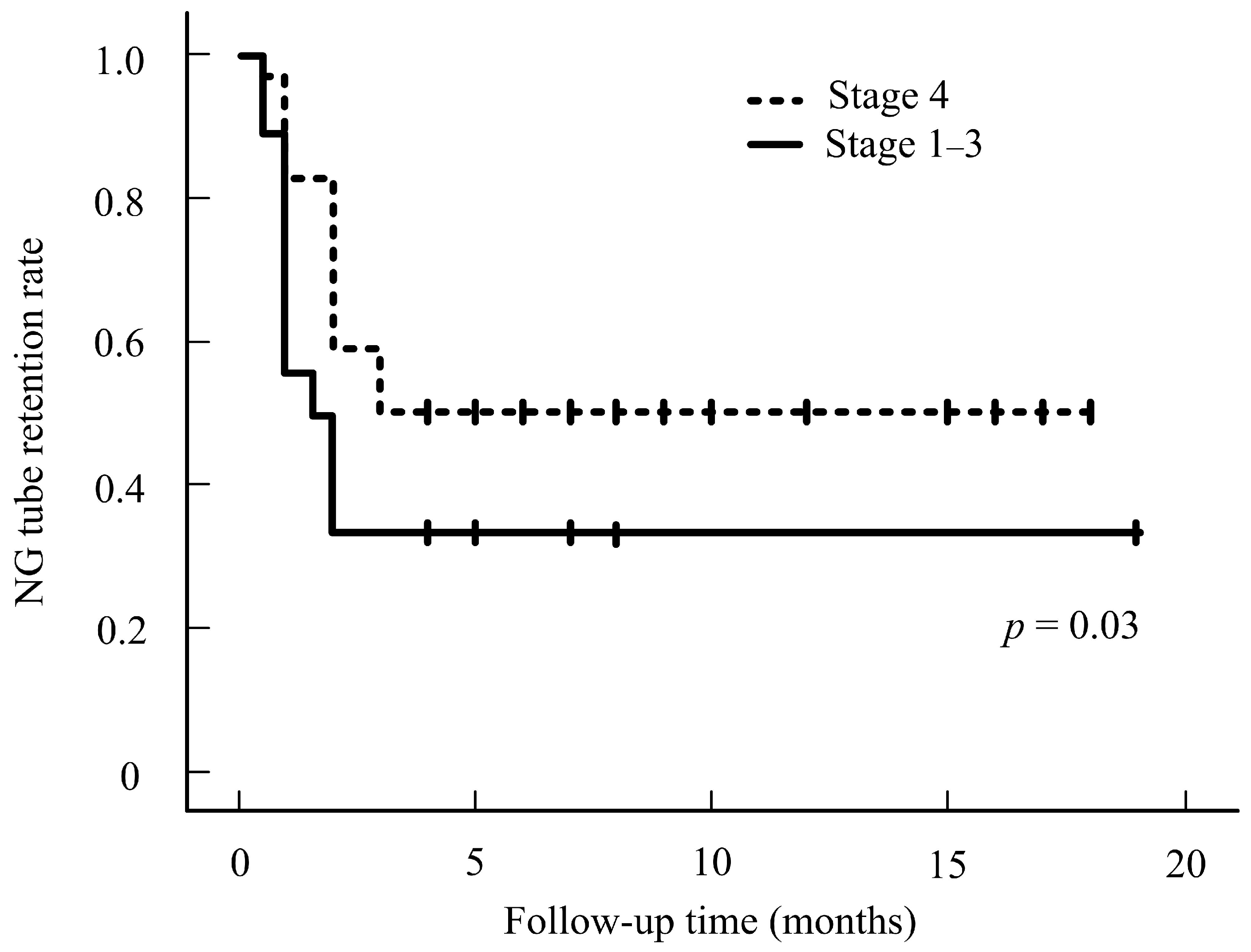
| Stage 1–3 vs. 4, no. | 201/66 | 0.53 (0.27~0.96) | 0.03 * |
| TNM stage | |||
| T stage (T0–2) vs. (T3–4), no. | 186/81 | 3.04 (2.01~4.60) | 0.01 * |
| N stage (N0–1) vs. (N2–3), no. | 119/148 | 0.78 (0.51~1.18) | 0.24 |
| M stage (M0) vs. (M1), no. | 258/9 | 0.33 (0.04~2.42) | 0.28 |
| Items | IC–Surgery (n =171) | IC-CRT (n = 96) | p-Value |
|---|---|---|---|
| Age | 54.82 ± 9.81 | 53.98 ± 9.89 | 0.50 |
| Male sex, no. (%) | 167 (97.66%) | 87 (90.62%) | |
| Alcohol, no. (%) | 141 (82.45%) | 76 (79.16%) | |
| Betel nut, no. (%) | 130 (76.02%) | 75 (78.12%) | |
| Cigarette, no. (%) | 149 (87.13%) | 85 (88.54%) | |
| HPV-positive (%) | 51 (29.82%) | 30 (31.25%) | |
| Cancer stage | |||
| Stage 1–3 vs. 4, no. | 36/135 | 30/66 | 0.06 |
| TNM stage | |||
| T stage (T0–2) vs. (T3–4), no. | 118/53 | 67/29 | 0.89 |
| N stage (N0–1) vs. (N 2–3), no. | 84/87 | 35/61 | 0.05 |
| M stage (M0) vs. (M1), no. | 171/0 | 87/9 | N.S. |
| Overall survival Stages 1–2 Stages 3–4 | 73% 51% | 75% 48% | 0.73 |
| Tumor location | |||
| Tonsil | 35 (20.36%) | 16 (16.67%) | |
| Tongue base | 43 (25.14%) | 29 (30.20%) | |
| Tonsil + tongue base + adjacent tissue | 90 (52.63%) | 51 (53.12%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsou, Y.-A.; Chang, W.-D.; Meng, N.-H.; Hua, C.-H. Analysis of Swallowing Functional Preservation by Surgical Versus CRT After Induction Chemotherapy for Oropharyngeal Cancer. Cancers 2024, 16, 3658. https://doi.org/10.3390/cancers16213658
Tsou Y-A, Chang W-D, Meng N-H, Hua C-H. Analysis of Swallowing Functional Preservation by Surgical Versus CRT After Induction Chemotherapy for Oropharyngeal Cancer. Cancers. 2024; 16(21):3658. https://doi.org/10.3390/cancers16213658
Chicago/Turabian StyleTsou, Yung-An, Wen-Dien Chang, Nai-Hsin Meng, and Chun-Hung Hua. 2024. "Analysis of Swallowing Functional Preservation by Surgical Versus CRT After Induction Chemotherapy for Oropharyngeal Cancer" Cancers 16, no. 21: 3658. https://doi.org/10.3390/cancers16213658
APA StyleTsou, Y.-A., Chang, W.-D., Meng, N.-H., & Hua, C.-H. (2024). Analysis of Swallowing Functional Preservation by Surgical Versus CRT After Induction Chemotherapy for Oropharyngeal Cancer. Cancers, 16(21), 3658. https://doi.org/10.3390/cancers16213658






