Real-World Cardiotoxicity in Metastatic Melanoma Patients Treated with Encorafenib and Binimetinib
Abstract
Simple Summary
Abstract
1. Introduction
2. Methods
2.1. Study Population
2.2. Assessment of Cardiac Function
2.3. Cardiotoxicity
2.4. Statistical Analysis
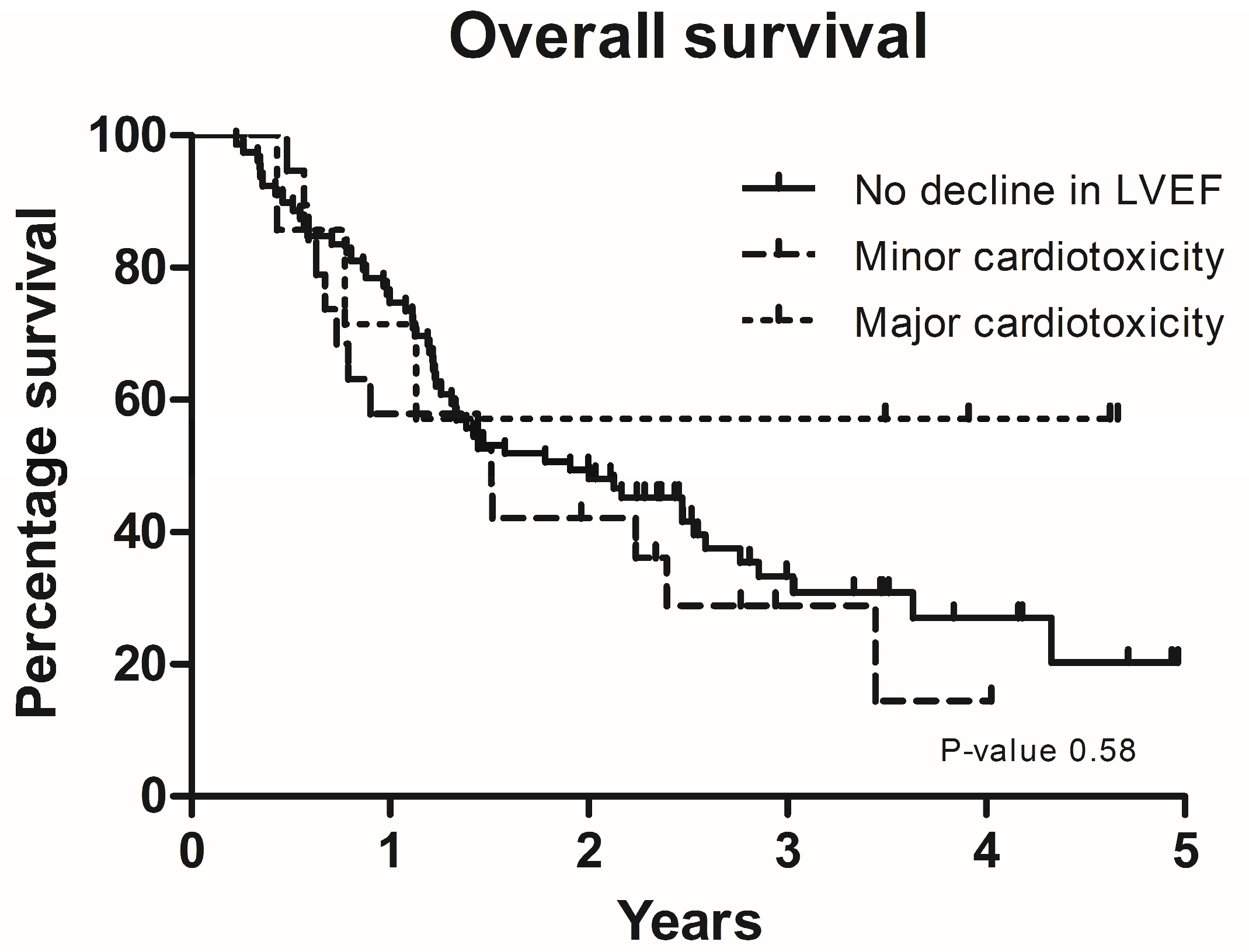
3. Results
3.1. Study Population
3.2. Cardiotoxicity
3.3. Minor Cardiotoxicity
3.4. Major Cardiotoxicity
3.5. LVEF <50% at Baseline
3.6. Time to Cardiotoxicity
3.7. Changes in Paraclinical Values
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dummer, R.; Flaherty, K.T.; Robert, C.; Arance, A.; De Groot, J.W.B.; Garbe, C.; Gogas, H.J.; Gutzmer, R.; Krajsová, I.; Liszkay, G.; et al. COLUMBUS 5-Year Update: A Randomized, Open-Label, Phase III Trial of Encorafenib Plus Binimetinib versus Vemurafenib or Encorafenib in Patients with BRAF V600-Mutant Melanoma. J. Clin. Oncol. 2022, 40, 4178–4188. [Google Scholar] [CrossRef] [PubMed]
- Wolchok, J.D.; Chiarion-Sileni, V.; Gonzalez, R.; Grob, J.J.; Rutkowski, P.; Lao, C.D.; Cowey, C.L.; Schadendorf, D.; Wagstaff, J.; Dummer, R.; et al. Long-Term Outcomes with Nivolumab Plus Ipilimumab or Nivolumab Alone versus Ipilimumab in Patients with Advanced Melanoma. J. Clin. Oncol. 2022, 40, 127–137. [Google Scholar] [CrossRef] [PubMed]
- Robert, C.; Grob, J.J.; Stroyakovskiy, D.; Karaszewska, B.; Hauschild, A.; Levchenko, E.; Chiarion Sileni, V.; Schachter, J.; Garbe, C.; Bondarenko, I.; et al. Five-Year Outcomes with Dabrafenib plus Trametinib in Metastatic Melanoma. N. Engl. J. Med. 2019, 381, 626–636. [Google Scholar] [CrossRef] [PubMed]
- Davies, H.; Bignell, G.R.; Cox, C.; Stephens, P.; Edkins, S.; Clegg, S.; Teague, J.; Woffendin, H.; Garnett, M.J.; Bottomley, W.; et al. Mutations of the BRAF Gene in Human Cancer. Nature 2002, 417, 949–954. [Google Scholar] [CrossRef]
- Spagnolo, F.; Ghiorzo, P.; Orgiano, L.; Pastorino, L.; Picasso, V.; Tornari, E.; Ottaviano, V.; Queirolo, P. BRAF-Mutant Melanoma: Treatment Approaches, Resistance Mechanisms, and Diagnostic Strategies. OncoTargets Ther. 2015, 8, 157–168. [Google Scholar] [CrossRef]
- Long, G.V.; Flaherty, K.T.; Stroyakovskiy, D.; Gogas, H.; Levchenko, E.; de Braud, F.; Larkin, J.; Garbe, C.; Jouary, T.; Hauschild, A.; et al. Dabrafenib plus Trametinib versus Dabrafenib Monotherapy in Patients with Metastatic BRAF V600E/ K-Mutant Melanoma: Long-Term Survival and Safety Analysis of a Phase 3 Study. Ann. Oncol. 2017, 28, 1631–1639. [Google Scholar] [CrossRef]
- Ascierto, P.A.; McArthur, G.A.; Dréno, B.; Atkinson, V.; Liszkay, G.; Di Giacomo, A.M.; Mandalà, M.; Demidov, L.; Stroyakovskiy, D.; Thomas, L.; et al. Cobimetinib Combined with Vemurafenib in Advanced BRAFV600-Mutant Melanoma (CoBRIM): Updated Efficacy Results from a Randomised, Double-Blind, Phase 3 Trial. Lancet Oncol. 2016, 17, 1248–1260. [Google Scholar] [CrossRef] [PubMed]
- Robert, C.; Karaszewska, B.; Schachter, J.; Rutkowski, P.; Mackiewicz, A.; Stroiakovski, D.; Lichinitser, M.; Dummer, R.; Grange, F.; Mortier, L.; et al. Improved Overall Survival in Melanoma with Combined Dabrafenib and Trametinib. N. Engl. J. Med. 2015, 372, 30–39. [Google Scholar] [CrossRef]
- Guha, A.; Jain, P.; Fradley, M.G.; Lenihan, D.; Gutierrez, J.M.; Jain, C.; de Lima, M.; Barnholtz-Sloan, J.S.; Oliveira, G.H.; Dowlati, A.; et al. Cardiovascular Adverse Events Associated with BRAF versus BRAF/MEK Inhibitor: Cross-Sectional and Longitudinal Analysis Using Two Large National Registries. Cancer Med. 2021, 10, 3862–3872. [Google Scholar] [CrossRef]
- Mezi, S.; Botticelli, A.; Scagnoli, S.; Pomati, G.; Fiscon, G.; De Galitiis, F.; Di Pietro, F.R.; Verkhovskaia, S.; Amirhassankhani, S.; Pisegna, S.; et al. The Impact of Drug–Drug Interactions on the Toxicity Profile of Combined Treatment with BRAF and MEK Inhibitors in Patients with BRAF-Mutated Metastatic Melanoma. Cancers 2023, 15, 4587. [Google Scholar] [CrossRef]
- Bronte, E.; Bronte, G.; Novo, G.; Rinaldi, G.; Bronte, F.; Passiglia, F.; Russo, A. Cardiotoxicity Mechanisms of the Combination of BRAF-Inhibitors and MEK-Inhibitors. Pharmacol. Ther. 2018, 192, 65–73. [Google Scholar] [CrossRef] [PubMed]
- Glen, C.; Adam, S.; McDowell, K.; Waterston, A.; Tan, Y.Y.; Petrie, M.C.; Coats, C.J.; Lang, N.N. Cardiotoxicity of BRAF/MEK Inhibitors: A Longitudinal Study Incorporating Contemporary Definitions and Risk Scores. JACC CardioOncol. 2023, 5, 628–637. [Google Scholar] [CrossRef]
- Dummer, R.; Ascierto, P.A.; Gogas, H.J.; Arance, A.; Mandala, M.; Liszkay, G.; Garbe, C.; Schadendorf, D.; Krajsova, I.; Gutzmer, R.; et al. Overall Survival in Patients with BRAF-Mutant Melanoma Receiving Encorafenib plus Binimetinib versus Vemurafenib or Encorafenib (COLUMBUS): A Multicentre, Open-Label, Randomised, Phase 3 Trial. Lancet Oncol. 2018, 19, 1315–1327. [Google Scholar] [CrossRef] [PubMed]
- Arangalage, D.; Degrauwe, N.; Michielin, O.; Monney, P.; Özdemir, B.C. Pathophysiology, Diagnosis and Management of Cardiac Toxicity Induced by Immune Checkpoint Inhibitors and BRAF and MEK Inhibitors. Cancer Treat. Rev. 2021, 100, 102282. [Google Scholar] [CrossRef]
- Beck, T.C.; Arhontoulis, D.C.; Morningstar, J.E.; Hyams, N.; Stoddard, A.; Springs, K.; Mukherjee, R.; Helke, K.; Guo, L.; Moore, K.; et al. Cellular and Molecular Mechanisms of MEK1 Inhibitor–Induced Cardiotoxicity. JACC CardioOncol. 2022, 4, 535–548. [Google Scholar] [CrossRef]
- Gilbert, C.J.; Longenecker, J.Z.; Accornero, F. ERK1/2: An Integrator of Signals That Alters Cardiac Homeostasis and Growth. Biology 2021, 10, 346. [Google Scholar] [CrossRef]
- Pedersen, S.; Larsen, K.O.; Christensen, A.H.; Svane, I.M.; Zerahn, B.; Ellebaek, E. Cardiotoxicity in Metastatic Melanoma Patients Treated with BRAF and MEK Inhibitors in a Real-World Setting. Acta Oncol. 2022, 61, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Ellebaek, E.; Svane, I.M.; Schmidt, H.; Haslund, C.A.; Donia, M.; Hoejberg, L.; Ruhlmann, C.; Guldbrandt, L.M.; Køhler, U.H.; Bastholt, L. The Danish Metastatic Melanoma Database (DAMMED): A Nation-Wide Platform for Quality Assurance and Research in Real-World Data on Medical Therapy in Danish Melanoma Patients. Cancer Epidemiol. 2021, 73, 101943. [Google Scholar] [CrossRef] [PubMed]
- Jensen, M.M.; Haase, C.; Zerahn, B. Interstudy Repeatability of Left and Right Ventricular Volume Estimations by Serial-Gated Tomographic Radionuclide Angiographies Using a Cadmium-Zinc-Telluride Detector Gamma Camera. Clin. Physiol. Funct. Imaging 2015, 35, 418–424. [Google Scholar] [CrossRef]
- Rydberg, J.; Andersen, J.; Haarmark, C.; Zerahn, B. The Influence of Anthropometric and Basic Circulatory Variables on Count Rate in Cadmium-Zinc-Telluride SPECT Gated Radionuclide Angiography. J. Nucl. Cardiol. 2019, 26, 1974–1980. [Google Scholar] [CrossRef]
- Hansen, N.L.; Haarmark, C.; Zerahn, B. Ventricular Peak Emptying and Filling Rates Measured by Gated Tomographic Radionuclide Angiography Using a Cadmium–Zinc–Telluride SPECT Camera in Chemotherapy-Naïve Cancer Patients. J. Nucl. Cardiol. 2020, 27, 1193–1201. [Google Scholar] [CrossRef] [PubMed]
- Khouri, M.G.; Douglas, P.S.; Mackey, J.R.; Martin, M.; Scott, J.M.; Scherrer-Crosbie, M.; Jones, L.W. Cancer Therapy-Induced Cardiac Toxicity in Early Breast Cancer Addressing the Unresolved Issues. Circulation 2012, 126, 2749–2763. [Google Scholar] [CrossRef] [PubMed]
- Haarmark, C.; Haase, C.; Jensen, M.M.; Zerahn, B. Pre-Chemotherapy Values for Left and Right Ventricular Volumes and Ejection Fraction by Gated Tomographic Radionuclide Angiography Using a Cadmium-Zinc-Telluride Detector Gamma Camera. J. Nucl. Cardiol. 2016, 23, 87–97. [Google Scholar] [CrossRef] [PubMed]
- Berger, M.; Amini-Adlé, M.; Maucort-Boulch, D.; Robinson, P.; Thomas, L.; Dalle, S.; Courand, P.Y. Left Ventricular Ejection Fraction Decrease Related to BRAF and/or MEK Inhibitors in Metastatic Melanoma Patients: A Retrospective Analysis. Cancer Med. 2020, 9, 2611–2620. [Google Scholar] [CrossRef] [PubMed]
| Baseline Characteristics | All Patients | Patients with No LVEF Decline | Patients with Minor Cardiotoxicity | Patients with Major Cardiotoxicity | Patients with LVEF <50% at Baseline |
|---|---|---|---|---|---|
| Number of patients | 108 | 79 | 19 | 7 | 3 |
| Sex, male | 66 (61) | 52 (66) | 9 (47) | 4 (57) | 1 (33) |
| Age (mean ± SD) | 63.4 ± 13.7 | 62.2 ± 13.4 | 63.9 ± 15.8 | 68.6 ± 13.1 | 53.6 ± 4.5 |
| BMI (mean ± SD) | 24.8 ± 4.1 | 24.9 ± 4.1 | 25.4 ± 4.8 | 22.7 ± 1.9 | 23.9 ± 3.2 |
| Performance status: | |||||
| 0–1 | 90 (83) | 67 (85) | 17 (90) | 4 (57) | 2 |
| ≥2 | 18 (17) | 12 (15) | 2 (11) | 3 (43) | 1 |
| Brain metastases | 42 (39) | 31 (39) | 5 (26) | 4 (57) | 2 |
| LDH | |||||
| <ULN | 53 (50) | 40 (51) | 8 (44) | 4 (57) | 1 |
| >ULN | 53 (50) | 38 (49) | 10 (56) | 3 (43) | 2 |
| Missing | 2 | 1 | 1 | 0 | – |
| BRAF/MEKi as 1. line treatment | 59 (55) | 43 (54) | 10 (53) | 4 (57) | 2 |
| ICI in later lines | 31 (53) | 24 (56) | 5 (50) | 0 | 2 (100) |
| BRAF/MEKi as 2. line or higher | 49 (45) | 36 (46) | 9 (47) | 3 (43) | 1 (33) |
| ICI in previous lines | 49 (100) | 36 (100) | 9 (100) | 3 (100) | 1 (100) |
| ICI in later lines | 20 (41) | 16 (44) | 3 (33) | 1 (33) | – |
| Comorbidities | |||||
| Hypertension | 23 (21) | 18 (23) | 4 (21) | 1 (14) | – |
| Ischemic heart disease | 4 (4) | 1 (1) | – | 3 (43) | – |
| Diabetes | 3 (3) | 2 (3) | – | 1 (14) | – |
| COLD | 10 (9) | 5 (6) | 3 (16) | 2 (29) | – |
| MUGA values (means ± SD) | |||||
| LVEF (%) | 70 ± 12 | 69 ± 10 | 82 ± 7 | 58 ± 6 | 40 ± 10 |
| LVEDV (mL) | 86 ± 24 | 88 ± 24 | 73 ± 16 | 90 ± 31 | 106 ± 28 |
| LVESV (mL) | 28 ± 16 | 29 ± 14 | 14 ± 6 | 39 ± 18 | 65 ± 27 |
| HR (beats per minute) | 73 ± 14 | 72 ± 14 | 78 ± 14 | 75 ± 19 | 68 ± 7 |
| Systolic BP (mmHg) | 126 ± 17 | 126 ± 18 | 125 ± 14 | 124 ± 16 | 130 ± 20 |
| Diastolic BP (mmHg) | 75 ± 10 | 76 ± 9 | 71 ± 11 | 75 ± 12 | 80 ± 11 |
| LVPER (mL/s) | −3.5 ± 1.1 | −3.4 ± 1.0 | −4.4 ± 0.9 | −2.6 ± 0.5 | −2.2 ± 0.8 |
| LVPFR (mL/s) | 2.9 ± 1.0 | 2.8 ± 0.8 | 3.8 ± 1.4 | 2.6 ± 0.7 | 2.0 ± 0.6 |
| LVPER adjusted (mL) | −4.7 ± 1.6 | −4.7 ± 1.7 | −5.7 ± 1.1 | −3.5 ± 0.6 | −3.3 ± 1.3 |
| LVPFR adjusted (mL) | 4.0 ± 0.9 | 3.9 ± 0.8 | 4.7 ± 1.0 | 3.5 ± 0.5 | 3.0 ± 1.0 |
| Patient Group | Mean Time to Decline in LVEF (Days) | Median Time to Decline in LVEF (Days) | Range (Days) |
|---|---|---|---|
| All patients with cardiotoxicity | 174 | 90 | 71–1246 |
| Minor cardiotoxicity | 179 | 78 | 71–1246 |
| Major cardiotoxicity | 160 | 134 | 76–377 |
| Patient Group | LVEF (%) | LVEDV (mL) | LVESV (mL) | LVPER (mL/s) | LVPFR (mL/s) | LVPER-Adj (mL) | LVPFR-Adj (mL) | HR s-1 |
|---|---|---|---|---|---|---|---|---|
| No LVEF decline (n = 76) | −6 ± 4.8 (−8%) | 6 ± 15.3 (10%) | 7 ± 6.7 (42%) | 1 ± 0.9 (−13%) | 0 ± 0.6 (−11%) | 0 ± 0.9 (−8%) | 0 ± 0.7 (−7%) | −4 ± 10.9 (−4%) |
| Minor cardiotoxicity (n = 22) | −19 ± 3.3 (−24%) | 7 ± 16.6 (12%) | 16 ± 6.9 (158%) | 1 ± 1 (−29%) | −1 ± 1 (−28%) | 1 ± 1.1 (−24%) | −1 ± 1 (−22%) | −6 ± 13.2 (−6%) |
| Major cardiotoxicity (n = 7) | −14 ± 3.8 (−24%) | 11 ± 15.6 (13%) | 17 ± 6.3 (49%) | 1 ± 0.5 (−22%) | −1 ± 0.6 (−24%) | 1 ± 0.7 (−17%) | −1 ± 0.6 (−22%) | −6 ± 15.5 (−4%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pedersen, S.; Nielsen, M.Ø.; Donia, M.; Svane, I.M.; Zerahn, B.; Ellebaek, E. Real-World Cardiotoxicity in Metastatic Melanoma Patients Treated with Encorafenib and Binimetinib. Cancers 2024, 16, 2945. https://doi.org/10.3390/cancers16172945
Pedersen S, Nielsen MØ, Donia M, Svane IM, Zerahn B, Ellebaek E. Real-World Cardiotoxicity in Metastatic Melanoma Patients Treated with Encorafenib and Binimetinib. Cancers. 2024; 16(17):2945. https://doi.org/10.3390/cancers16172945
Chicago/Turabian StylePedersen, Sidsel, Marc Østergaard Nielsen, Marco Donia, Inge Marie Svane, Bo Zerahn, and Eva Ellebaek. 2024. "Real-World Cardiotoxicity in Metastatic Melanoma Patients Treated with Encorafenib and Binimetinib" Cancers 16, no. 17: 2945. https://doi.org/10.3390/cancers16172945
APA StylePedersen, S., Nielsen, M. Ø., Donia, M., Svane, I. M., Zerahn, B., & Ellebaek, E. (2024). Real-World Cardiotoxicity in Metastatic Melanoma Patients Treated with Encorafenib and Binimetinib. Cancers, 16(17), 2945. https://doi.org/10.3390/cancers16172945








