Clinical Outcomes and Prognostic Factors in Nonmetastatic Castration-Resistant Prostate Cancer Treated with Androgen Receptor Signaling Inhibitors Therapy
Abstract
Simple Summary
Abstract
1. Introduction
2. Methods
2.1. Study Population
2.2. Treatment and Follow-Up Examination
2.3. Statistical Analysis
3. Results
3.1. Patient Characteristics
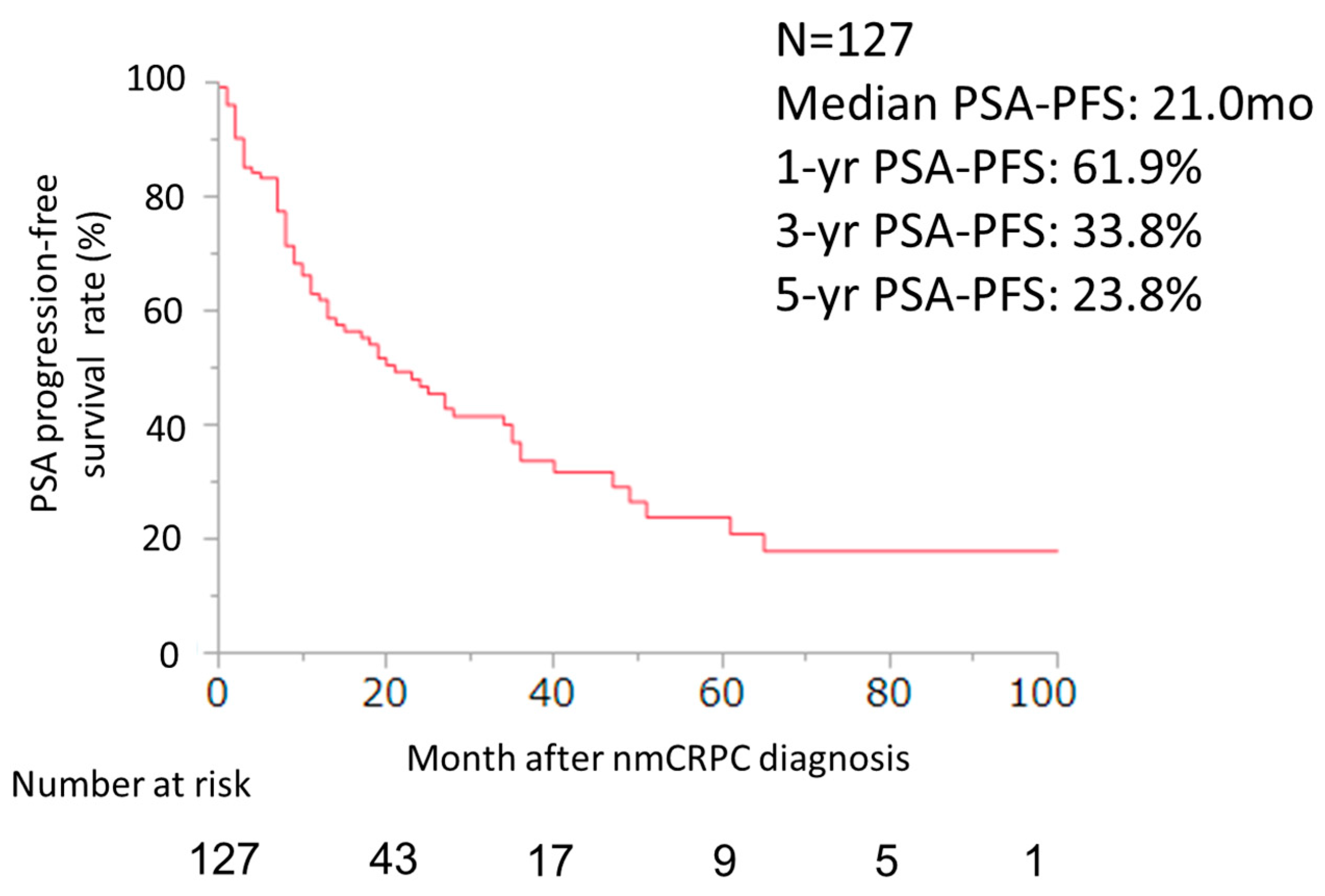
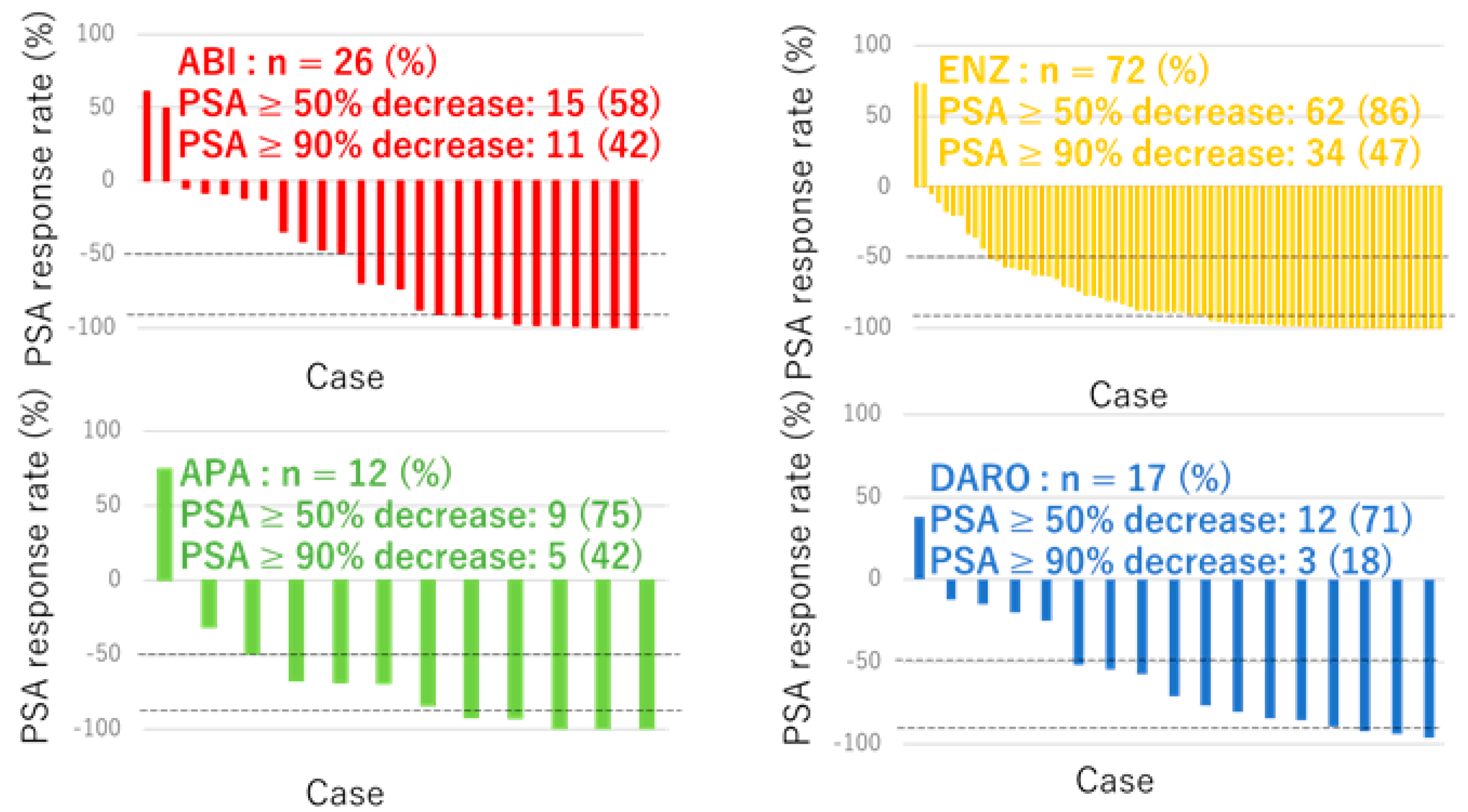
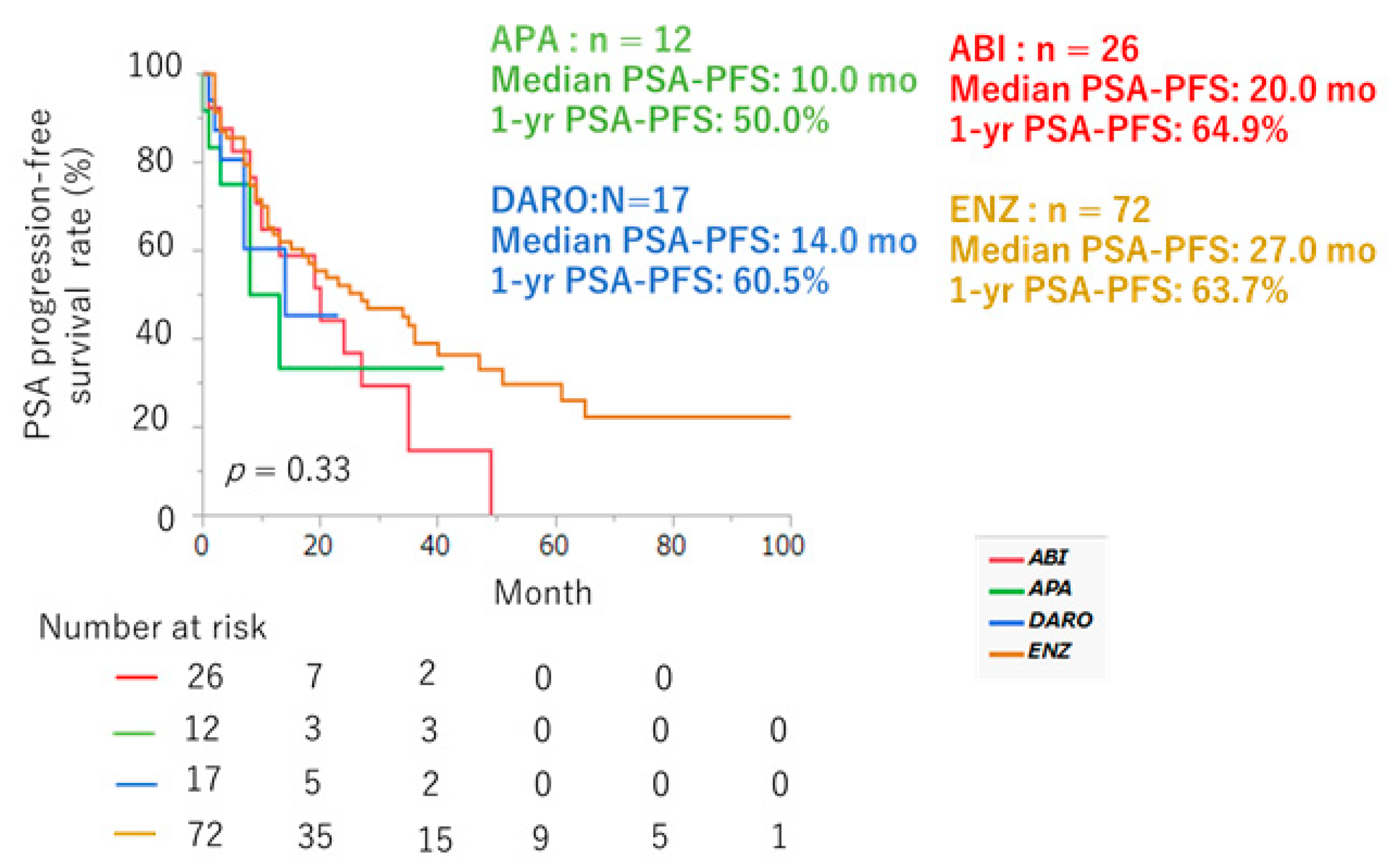
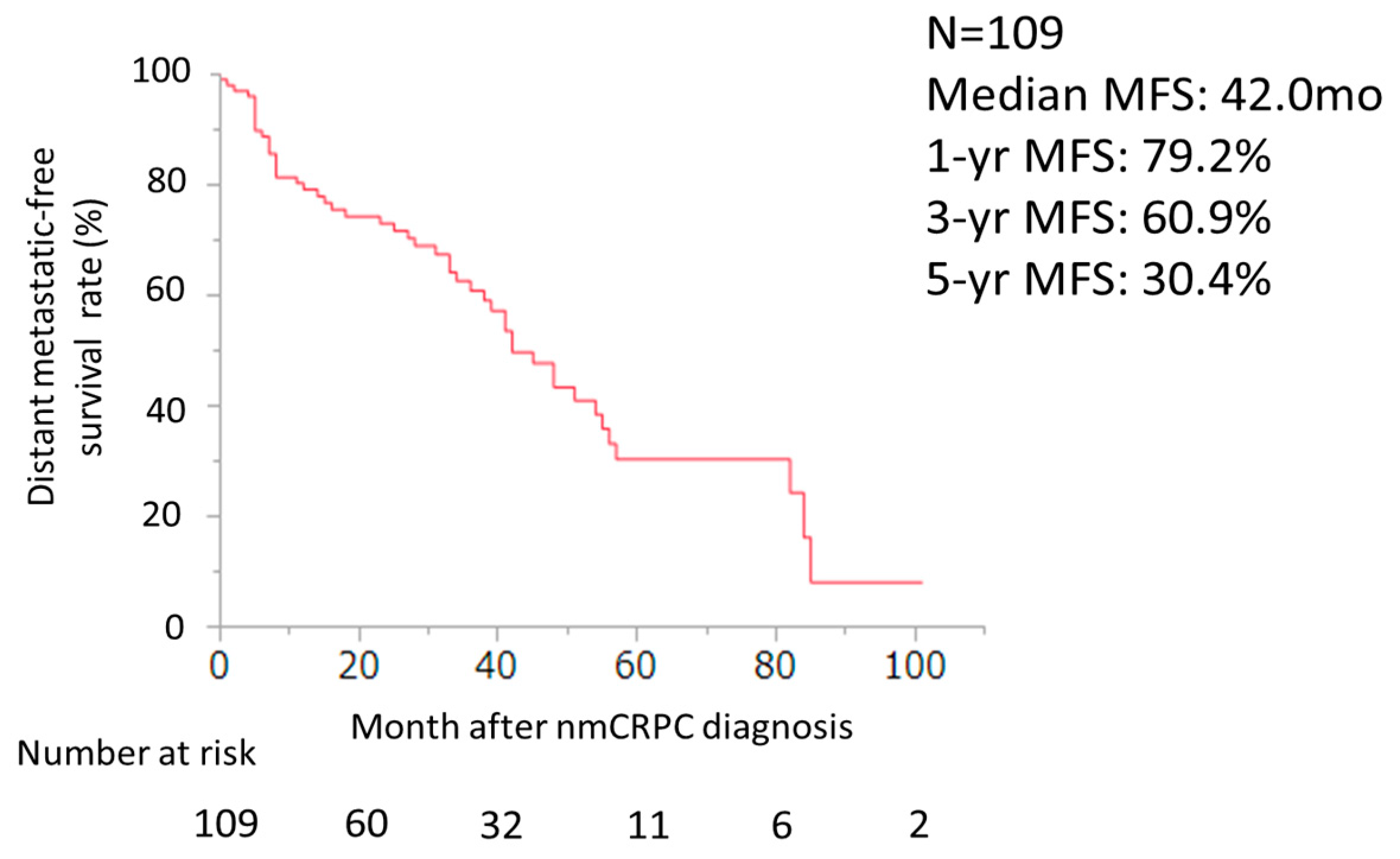
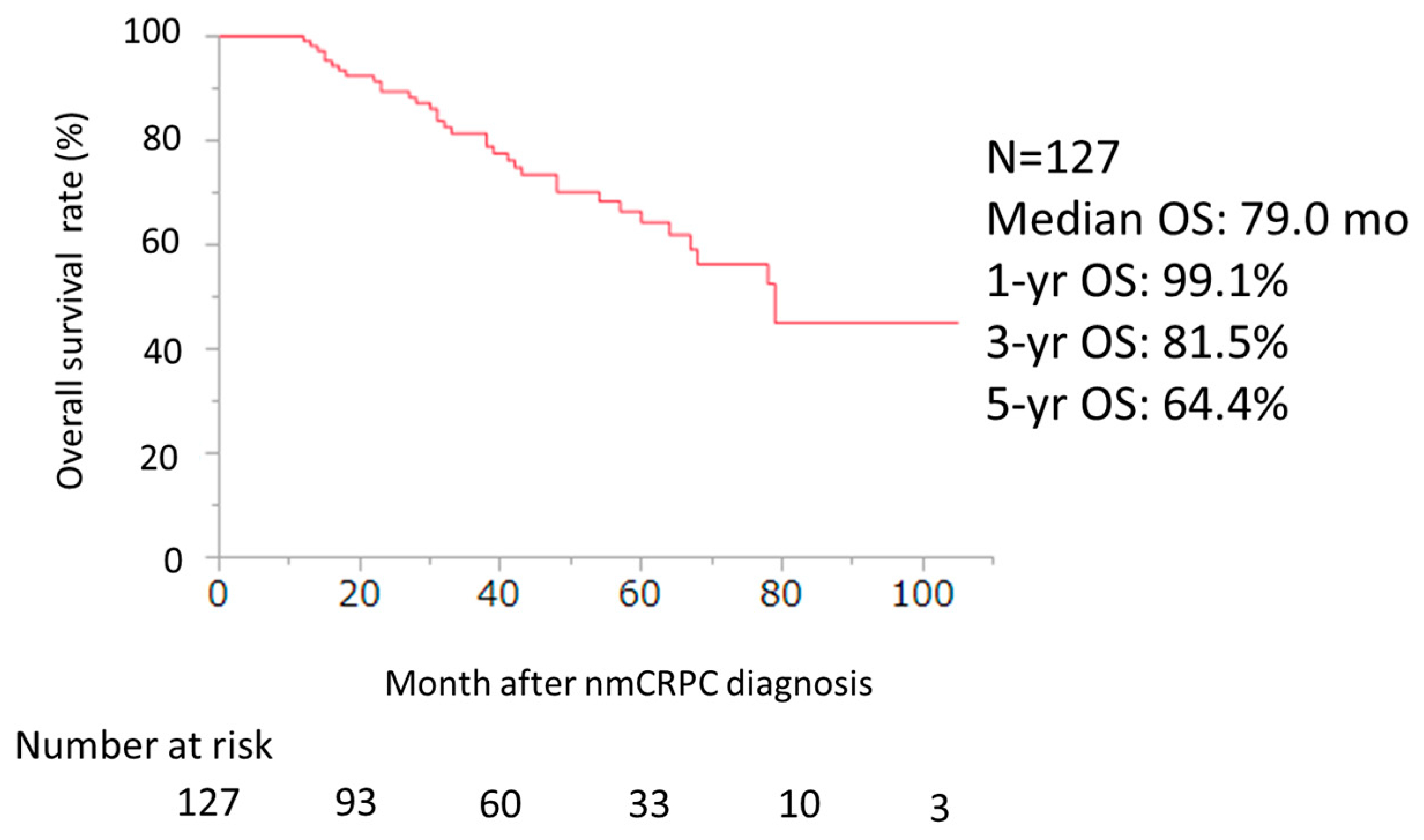
3.2. Efficacy of ARSI Therapy
3.3. Safety of ARSI Therapy
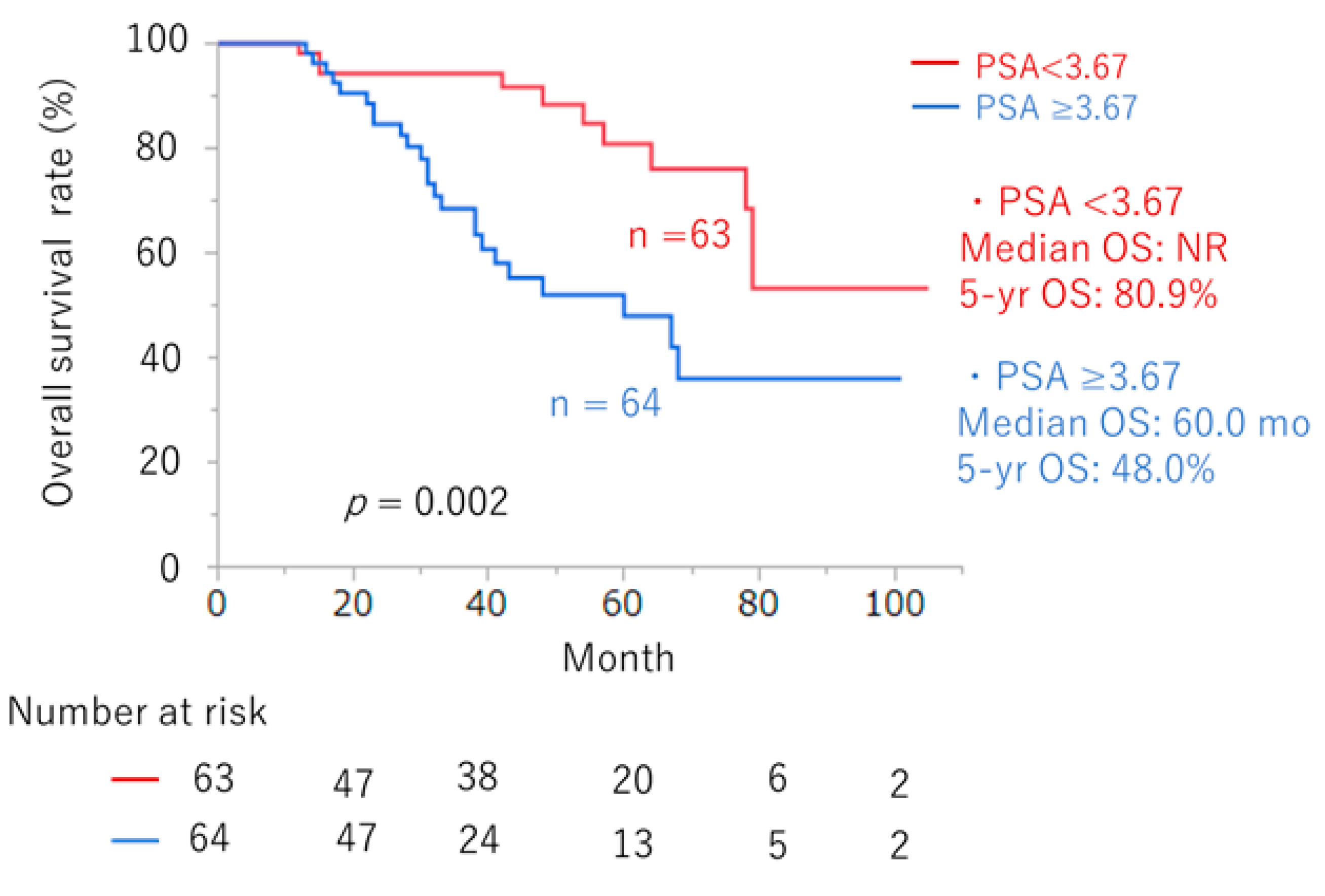
3.4. Predictors of Prognosis in ARSI Therapy
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bergengren, O.; Pekala, K.R.; Matsoukas, K.; Fainberg, J.; Mungovan, S.F.; Bratt, O.; Bray, F.; Brawley, O.; Luckenbaugh, A.N.; Mucci, L.; et al. 2022 update on prostate cancer epidemiology and risk factors—A systematic review. Eur. Urol. 2023, 84, 191–206. [Google Scholar] [CrossRef] [PubMed]
- Zumsteg, Z.S.; Spratt, D.E.; Romesser, P.B.; Pei, X.; Zhang, Z.; Polkinghorn, W.; McBride, S.; Kollmeier, M.; Yamada, Y.; Zelefsky, M.J. The natural history and predictors of outcome following biochemical relapse in the dose escalation era for prostate cancer patients undergoing definitive external beam radiotherapy. Eur. Urol. 2015, 67, 1009–1016. [Google Scholar] [CrossRef] [PubMed]
- Boorjian, S.A.; Thompson, R.H.; Tollefson, M.K.; Rangel, L.J.; Bergstralh, E.J.; Blute, M.L.; Karnes, R.J. Long-term risk of clinical progression after biochemical recurrence following radical prostatectomy: The impact of time from surgery to recurrence. Eur. Urol. 2011, 59, 893–899. [Google Scholar] [CrossRef] [PubMed]
- Kluth, L.A.; Shariat, S.F.; Kratzik, C.; Tagawa, S.; Sonpavde, G.; Rieken, M.; Scherr, D.S.; Pummer, K. The hypothalamic-pituitary-gonadal axis and prostate cancer: Implications for androgen deprivation therapy. World J. Urol. 2014, 32, 669–676. [Google Scholar] [CrossRef] [PubMed]
- Aly, M.; Hashim, M.; Heeg, B.; Liwing, J.; Leval, A.; Mehra, M.; Lawson, J.; Brookman-May, S.D.; Akre, O. Time-to-event outcomes in men with nonmetastatic castrate-resistant prostate cancer-A systematic literature review and pooling of individual participant data. Eur. Urol. Focus 2019, 5, 788–798. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.R.; Saad, F.; Chowdhury, S.; Oudard, S.; Hadaschik, B.A.; Graff, J.N.; Olmos, D.; Mainwaring, P.N.; Lee, J.Y.; Uemura, H.; et al. Apalutamide and overall survival in prostate cancer. Eur. Urol. 2021, 79, 150–158. [Google Scholar] [CrossRef] [PubMed]
- Fizazi, K.; Shore, N.; Tammela, T.L.; Ulys, A.; Vjaters, E.; Polyakov, S.; Jievaltas, M.; Luz, M.; Alekseev, B.; Kuss, I.; et al. ARAMIS Investigators. Nonmetastatic, castration-resistant prostate cancer and survival with darolutamide. N. Engl. J. Med. 2020, 383, 1040–1049. [Google Scholar] [CrossRef] [PubMed]
- Sternberg, C.N.; Fizazi, K.; Saad, F.; Shore, N.D.; De Giorgi, U.; Penson, D.F.; Ferreira, U.; Efstathiou, E.; Madziarska, K.; Kolinsky, M.P.; et al. Enzalutamide and survival in nonmetastatic, castration-resistant prostate cancer. N. Engl. J. Med. 2020, 382, 2197–2206. [Google Scholar] [CrossRef]
- Schaeffer, E.M.; Srinivas, S.; Adra, N.; An, Y.; Barocas, D.; Bitting, R.; Bryce, A.; Chapin, B.; Cheng, H.H.; D’Amico, A.V.; et al. Prostate Cancer, Version 4.2023, NCCN clinical practice guidelines in oncology. J. Natl. Compr. Cancer Netw. 2023, 21, 1067–1096. [Google Scholar] [CrossRef]
- Miyake, H.; Matsushita, Y.; Watanabe, H.; Tamura, K.; Motoyama, D.; Ito, T.; Sugiyama, T.; Otsuka, A. Comparative assessment of prognostic outcomes between first-generation antiandrogens and novel androgen-receptor-axis-targeted agents in patients with non-metastatic castration-resistant prostate cancer. Int. J. Clin. Oncol. 2019, 24, 842–847. [Google Scholar] [CrossRef]
- Fujita, N.; Hatakeyama, S.; Tabata, R.; Okita, K.; Kido, K.; Hamano, I.; Tanaka, T.; Noro, D.; Tokui, N.; Suzuki, Y.; et al. Real-world effects of novel androgen receptor axis-targeted agents on oncological outcomes in non-metastatic castration-resistant prostate cancer: A multi-institutional retrospective study. Prostate Int. 2024, 12, 46–51. [Google Scholar] [CrossRef] [PubMed]
- Howard, L.E.; Moreira, D.M.; De Hoedt, A.; Aronson, W.J.; Kane, C.J.; Amling, C.L.; Cooperberg, M.R.; Terris, M.K.; Freedland, S.J. Thresholds for PSA doubling time in men with non-metastatic castration-resistant prostate cancer. BJU Int. 2017, 120, E80–E86. [Google Scholar] [CrossRef] [PubMed]
- Scher, H.I.; Morris, M.J.; Stadler, W.M.; Higano, C.; Basch, E.; Fizazi, K.; Antonarakis, E.S.; Beer, T.M.; Carducci, M.A.; Chi, K.N.; et al. Trial design and objectives for castration-resistant prostate cancer: Updated recommendations from the Prostate Cancer Clinical Trials Working Group 3. J. Clin. Oncol. 2016, 34, 1402–1418. [Google Scholar] [CrossRef] [PubMed]
- Pound, C.R.; Partin, A.W.; Eisenberger, M.A.; Chan, D.W.; Pearson, J.D.; Walsh, P.C. Natural history of progression after PSA elevation following radical prostatectomy. JAMA 1999, 281, 1591–1597. [Google Scholar] [CrossRef] [PubMed]
- Ryan, C.J.; Crawford, E.D.; Shore, N.D.; Underwood, W., III; Taplin, M.E.; Londhe, A.; Francis, P.S.J.; Phillips, J.; McGowan, T.; Kantoff, P.W. The IMAAGEN Study: Effect of abiraterone acetate and prednisone on prostate specific antigen and radiographic disease progression in patients with nonmetastatic castration resistant prostate cancer. J. Urol. 2018, 200, 344–352. [Google Scholar] [CrossRef] [PubMed]
- Yokomizo, A.; Yonese, J.; Egawa, S.; Fukuhara, H.; Uemura, H.; Nishimura, K.; Nagata, M.; Saito, A.; Lee, T.; Yamaguchi, S.; et al. Correction to: Real-world use of enzalutamide in men with nonmetastatic castration-resistant prostate cancer in Japan. Int. J. Clin. Oncol. 2022, 27, 633–634. [Google Scholar] [CrossRef] [PubMed]
- Lowentritt, B.; Brown, G.; Pilon, D.; Ellis, L.; Germain, G.; Rossi, C.; Lefebvre, P.; Kernen, K.; Sieber, P.; Shore, N. Real-world prostate-specific antigen response and treatment adherence of apalutamide in patients with non-metastatic castration-resistant prostate cancer. Urology 2022, 166, 182–188. [Google Scholar] [CrossRef] [PubMed]
- Wenzel, M.; Nocera, L.; Collà Ruvolo, C.; Würnschimmel, C.; Tian, Z.; Shariat, S.F.; Saad, F.; Tilki, D.; Graefen, M.; Kluth, L.A.; et al. Overall survival and adverse events after treatment with darolutamide vs. apalutamide vs. enzalutamide for high-risk non-metastatic castration-resistant prostate cancer: A systematic review and network meta-analysis. Prostate Cancer Prostatic Dis. 2022, 25, 139–148. [Google Scholar] [CrossRef] [PubMed]
- Cao, B.; Kim, M.; Reizine, N.M.; Moreira, D.M. Adverse events and androgen receptor signaling inhibitors in the treatment of prostate cancer: A systematic review and multivariate network meta-analysis. Eur. Urol. Oncol. 2023, 6, 237–250. [Google Scholar] [CrossRef]
- Moreira, D.M.; Howard, L.E.; Sourbeer, K.N.; Amarasekara, H.S.; Chow, L.C.; Cockrell, D.C.; Hanyok, B.T.; Aronson, W.J.; Kane, C.J.; Terris, M.K.; et al. Predictors of time to metastasis in castration-resistant prostate cancer. Urology 2016, 96, 171–176. [Google Scholar] [CrossRef]
- Metwalli, A.R.; Rosner, I.L.; Cullen, J.; Chen, Y.; Brand, T.; Brassell, S.A.; Lesperance, J.; Porter, C.; Sterbis, J.; McLeod, D.G. Elevated alkaline phosphatase velocity strongly predicts overall survival and the risk of bone metastases in castrate-resistant prostate cancer. Urol. Oncol. 2014, 32, 761–768. [Google Scholar] [CrossRef]
- Smith, M.R.; Saad, F.; Oudard, S.; Shore, N.; Fizazi, K.; Sieber, P.; Tombal, B.; Damiao, R.; Marx, G.; Miller, K.; et al. Denosumab and bone metastasis-free survival in men with nonmetastatic castration-resistant prostate cancer: Exploratory analyses by baseline prostate-specific antigen doubling time. J. Clin. Oncol. 2013, 31, 3800–3806. [Google Scholar] [CrossRef]
- Mori, K.; Kimura, T.; Fukuokaya, W.; Iwatani, K.; Sakanaka, K.; Kurokawa, G.; Yanagisawa, T.; Sasaki, H.; Miki, J.; Shimomura, T.; et al. Values of alkaline phosphatase at the diagnosis of castration resistance and response to primary androgen deprivation therapy as predictors of subsequent metastasis in non-metastatic castration-resistant prostate cancer. Int. J. Clin. Oncol. 2020, 25, 479–485. [Google Scholar] [CrossRef]
- Madan, R.A.; Gulley, J.L.; Schlom, J.; Steinberg, S.M.; Liewehr, D.J.; Dahut, W.L.; Arlen, P.M. Analysis of overall survival in patients with nonmetastatic castration-resistant prostate cancer treated with vaccine, nilutamide, and combination therapy. Clin. Cancer Res. 2008, 14, 4526–4531. [Google Scholar] [CrossRef]
- Smith, M.R.; Cook, R.; Lee, K.A.; Nelson, J.B. Disease and host characteristics as predictors of time to first bone metastasis and death in men with progressive castration-resistant nonmetastatic prostate cancer. Cancer 2011, 117, 2077–2085. [Google Scholar] [CrossRef]
- Smith, M.R.; Kabbinavar, F.; Saad, F.; Hussain, A.; Gittelman, M.C.; Bilhartz, D.L.; Wynne, C.; Murray, R.; Zinner, N.R.; Schulman, C.; et al. Natural history of rising serum prostate-specific antigen in men with castrate nonmetastatic prostate cancer. J. Clin. Oncol. 2005, 23, 2918–2925. [Google Scholar] [CrossRef] [PubMed]
- Nørgaard, M.; Jensen, A.Ø.; Jacobsen, J.B.; Cetin, K.; Fryzek, J.P.; Sørensen, H.T. Skeletal related events, bone metastasis and survival of prostate cancer: A population based cohort study in Denmark (1999 to 2007). J. Urol. 2010, 184, 162–167. [Google Scholar] [CrossRef] [PubMed]
- Scher, H.I.; Solo, K.; Valant, J.; Todd, M.B.; Mehra, M. Prevalence of prostate cancer clinical states and mortality in the United States: Estimates using a dynamic progression model. PLoS ONE 2015, 10, e0139440. [Google Scholar] [CrossRef] [PubMed]
- Lecouvet, F.E.; El Mouedden, J.; Collette, L.; Coche, E.; Danse, E.; Jamar, F.; Machiels, J.P.; Vande Berg, B.; Omoumi, P.; Tombal, B. Can whole-body magnetic resonance imaging with diffusion-weighted imaging replace Tc 99m bone scanning and computed tomography for single-step detection of metastases in patients with high-risk prostate cancer? Eur. Urol. 2012, 62, 68–75. [Google Scholar] [CrossRef]
- Fendler, W.P.; Weber, M.; Iravani, A.; Hofman, M.S.; Calais, J.; Czernin, J.; Ilhan, H.; Saad, F.; Small, E.J.; Smith, M.R.; et al. Prostate-specific membrane antigen ligand positron emission tomography in men with nonmetastatic castration-resistant prostate cancer. Clin. Cancer Res. 2019, 25, 7448–7454. [Google Scholar] [CrossRef]
| Clinical Factors | Number | |
|---|---|---|
| Median age at the time of CRPC, years (IQR) | 76 (70–81) | |
| Median initial PSA, ng/mL (IQR) | 17 (10–59) | |
| Gleason Score (%) | <8 | 40 (31) |
| ≥8 | 87 (69) | |
| Clinical T Stage | 1–2 | 44 (35) |
| 3–4 | 82 (65) | |
| Unknown | 1 (1) | |
| Clinical N Stage | 0 | 103 (81) |
| 1 | 24 (19) | |
| Local therapy (%) | Surgery | 57 (45) |
| Radiation | 46 (36) | |
| No local treatment | 24 (19) | |
| Previous docetaxel therapy (%) | Yes | 6 (5) |
| No | 121 (95) | |
| PSA doubling time, month (%) | <6 | 99 (78) |
| ≥6 | 27 (21) | |
| Unknown | 1 (1) | |
| First-line ARAT agent (%) | Darolutamide | 17 (13) |
| Apalutamide | 12 (10) | |
| Abiraterone | 26 (20) | |
| Enzalutamide | 72 (57) |
| ENZ (n = 72) | ABI (n = 26) | APA (n = 12) | DARO (n = 17) | |||||
|---|---|---|---|---|---|---|---|---|
| Any Grade (%) | ≥Grade 3 (%) | Any Grade (%) | ≥Grade 3 (%) | Any Grade (%) | ≥Grade 3 (%) | Any Grade (%) | ≥Grade 3 (%) | |
| Rash | 1 (1) | 0 | 0 | 0 | 6 (50) | 1 (4) | 0 | 0 |
| Neuropathy | 2 (3) | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Fatigue | 11 (15) | 1 (2) | 2 (8) | 2 (17) | 0 | 2 (12) | 1 (6) | |
| Decreased appetite | 4 (6) | 0 | 0 | 0 | 0 | 0 | 0 | |
| Nausea | 1 (1) | 0 | 0 | 1 (8) | 0 | 0 | 0 | |
| Dysesthesia | 2 (3) | 0 | 0 | 1 (8) | 0 | 0 | 0 | |
| Dysgeusia | 1 (1) | 1 (4) | 1 (8) | 0 | 0 | 0 | ||
| Edema | 1 (1) | 1 (4) | 0 | 0 | 0 | 0 | ||
| Dizziness | 2 (3) | 0 | 0 | 0 | 0 | 0 | 0 | |
| Neutropenia | 1 (1) | 0 | 0 | 0 | 0 | 0 | 0 | |
| Hepatic dysfunction | 0 | 0 | 2 (8) | 0 | 0 | 1 (6) | 0 | |
| Hypokalemia | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Hypertension | 0 | 0 | 1 (4) | 1 (4) | 0 | 0 | 0 | 0 |
| Variables | Univariate | Multivariate | |||
|---|---|---|---|---|---|
| HR (95% CI) | p Value | HR (95% CI) | p Value | ||
| Gleason pattern 5 at biopsy | Yes vs. No | 1.75 (0.89, 3.56) | 0.107 | ||
| LDH (U/L) at first-line ARSI | ≥192 vs. <192 | 1.58 (0.79, 3.31) | 0.200 | ||
| ALP (U/L) at first-line ARSI | ≥271 vs. <271 | 1.87 (0.89, 3.75) | 0.097 | NS | |
| Time to CRPC (months) | ≤54 vs. >54 | 1.78 (0.82, 4.43) | 0.172 | ||
| PSA (ng/mL) at initiation of ARSI | >3.67 vs. ≤3.67 | 2.93 (1.46, 6.26) | 0.002 | 2.93 (1.46, 6.26) | 0.002 |
| Previous Docetaxel chemotherapy | Yes vs. No | 1.15 (0.28, 3.24) | 0.817 | ||
| Presence of regional lymph node | Yes vs. No | 2.31 (0.59, 8.15) | 0.215 | ||
| Treatment | 0.084 | NS | |||
| Surgery vs. CAB | 0.47 (0.19, 1.22) | 0.118 | |||
| Radiation vs. CAB | 1.04 (0.46, 2.59) | 0.914 | |||
| Surgery vs. Radiation | 2.22 (1.04, 4.92) | 0.040 | |||
| PSA-DT | ≤6 mo vs. >6 mo | 1.64 (0.59, 6.82) | 0.383 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fujiwara, R.; Yamamoto, S.; Takemura, K.; Yuasa, T.; Numao, N.; Oguchi, T.; Yasuda, Y.; Yoneoka, Y.; Yonese, J. Clinical Outcomes and Prognostic Factors in Nonmetastatic Castration-Resistant Prostate Cancer Treated with Androgen Receptor Signaling Inhibitors Therapy. Cancers 2024, 16, 2659. https://doi.org/10.3390/cancers16152659
Fujiwara R, Yamamoto S, Takemura K, Yuasa T, Numao N, Oguchi T, Yasuda Y, Yoneoka Y, Yonese J. Clinical Outcomes and Prognostic Factors in Nonmetastatic Castration-Resistant Prostate Cancer Treated with Androgen Receptor Signaling Inhibitors Therapy. Cancers. 2024; 16(15):2659. https://doi.org/10.3390/cancers16152659
Chicago/Turabian StyleFujiwara, Ryo, Shinya Yamamoto, Kosuke Takemura, Takeshi Yuasa, Noboru Numao, Tomohiko Oguchi, Yosuke Yasuda, Yusuke Yoneoka, and Junji Yonese. 2024. "Clinical Outcomes and Prognostic Factors in Nonmetastatic Castration-Resistant Prostate Cancer Treated with Androgen Receptor Signaling Inhibitors Therapy" Cancers 16, no. 15: 2659. https://doi.org/10.3390/cancers16152659
APA StyleFujiwara, R., Yamamoto, S., Takemura, K., Yuasa, T., Numao, N., Oguchi, T., Yasuda, Y., Yoneoka, Y., & Yonese, J. (2024). Clinical Outcomes and Prognostic Factors in Nonmetastatic Castration-Resistant Prostate Cancer Treated with Androgen Receptor Signaling Inhibitors Therapy. Cancers, 16(15), 2659. https://doi.org/10.3390/cancers16152659






