Shall We Screen Lung Cancer with Volume Computed Tomography in Austria? A Cost-Effectiveness Modelling Study
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Cost-Effectiveness Analysis
2.2. Model Structure
2.3. Model Inputs
2.3.1. Eligible Population
| Parameters | Base-Case Value | PSA Distribution | Reference |
|---|---|---|---|
| General settings | |||
| Discount rate for costs | 5.00% | Fixed | [18] |
| Discount rate for health outcomes | 5.00% | Fixed | [18] |
| Time horizon | Lifetime * | Fixed | [17] |
| Screening uptake rate | 50.00% | Beta | Assumption |
| Demography and epidemiology | |||
| Total population | 8,978,929 | Gamma | [26] |
| Population aged 50–74 years | 32.22% | Beta | [27] |
| Smoking rate | 20.76% | Beta | [29] |
| Lung cancer incidence aged 50–74 years | 0.45% | Gamma | [11,26,27,28,29,31] |
| Stage distribution (no screening) | |||
| Stage I | 16.30% | Dirichlet | [32] |
| Stage II | 7.80% | Dirichlet | [32] |
| Stage III | 27.70% | Dirichlet | [32] |
| Stage IV | 48.20% | Dirichlet | [32] |
| Costs | |||
| Recruitment costs | |||
| Invitation letter | EUR 3 | Gamma | [33,34] |
| GP consult | EUR 22 | Gamma | [33,34] |
| Screening costs | |||
| CT scan | EUR 280 | Gamma | [33,34] |
| Diagnostic costs | |||
| Diagnostic costs for screening detected patients (per person) | EUR 803 | Gamma | [2,32,33,34,35] |
| Diagnostic costs for clinically presented patients (per person) | EUR 1093 | Gamma | [2,32,33,34,35] |
| Treatment costs | |||
| Stage I | |||
| First line treatments | |||
| First 3 months | EUR 8564 | Gamma | [36,37] |
| First year (excluding the first 3 months) | EUR 1956 | Gamma | [36,37] |
| Second year | EUR 736 | Gamma | [33,34,36,37] |
| Second line treatment (per patient) | EUR 32,085 | Gamma | [2,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51] |
| Stage II | |||
| First line treatments | |||
| First 3 months | EUR 8215 | Gamma | [36,37] |
| First year (excluding the first 3 months) | EUR 2588 | Gamma | [36,37] |
| Second year | EUR 736 | Gamma | [33,34,36,37] |
| Second line treatment (per patient) | EUR 32,085 | Gamma | [2,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51] |
| Stage III | |||
| First line treatments | |||
| First 3 months | EUR 16,606 | Gamma | [2,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51] |
| First year (excluding the first 3 months) | EUR 41,502 | Gamma | [2,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51] |
| Second year | EUR 13,598 | Gamma | [2,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51] |
| Second line treatment (per patient) | EUR 24,795 | Gamma | [2,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51] |
| Stage IV | |||
| First line treatments | |||
| First 3 months | EUR 12,529 | Gamma | [2,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51] |
| First year (excluding the first 3 months) | EUR 25,442 | Gamma | [2,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51] |
| Second year | EUR 2517 | Gamma | [2,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51] |
| Second line treatment (per patient) | EUR 24,795 | Gamma | [2,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51] |
| Follow up costs ** | |||
| CT scan | EUR 280 | Gamma | [33,34] |
| Lung physician consult | EUR 88 | Gamma | [33,34] |
| End of life costs | EUR 7466 | Gamma | [37] |
| Utilities | |||
| Pre-progression state | |||
| Stage I | 0.78 | Beta | [52] |
| Stage II | 0.78 | Beta | [52] |
| Stage III | 0.69 | Beta | [52] |
| Stage IV | 0.69 | Beta | [52] |
| Post-progression state | |||
| Stage I | 0.69 | Beta | [52] |
| Stage II | 0.69 | Beta | [52] |
| Stage III | 0.69 | Beta | [52] |
| Stage IV | 0.69 | Beta | [52] |
| Survival | |||
| OS (five-year survival rate) | |||
| Stage I | 78.63% | NA. | [53] |
| Stage II | 54.90% | NA. | [53] |
| Stage III | 29.24% | NA. | [53] |
| Stage IV | 5.91% | NA. | [53] |
| D/PFS (one-year D/PFS rate) | |||
| Stage I | 87.80% | NA. | [54] |
| Stage II | 87.80% | NA. | [54,55] |
| Stage III | 41.81% | NA. | [48] |
| Stage IV | 40.13% | NA. | [41,56,57] |
| Background mortality | |||
| Life expectancy by age | General population | Beta | [58] |
2.3.2. Lung Cancer Epidemiology
2.3.3. Survival
2.3.4. Utilities
2.3.5. Expenses
2.4. Sensitivity Analysis
2.5. Scenario Analysis
3. Results
3.1. Base-Case Analysis
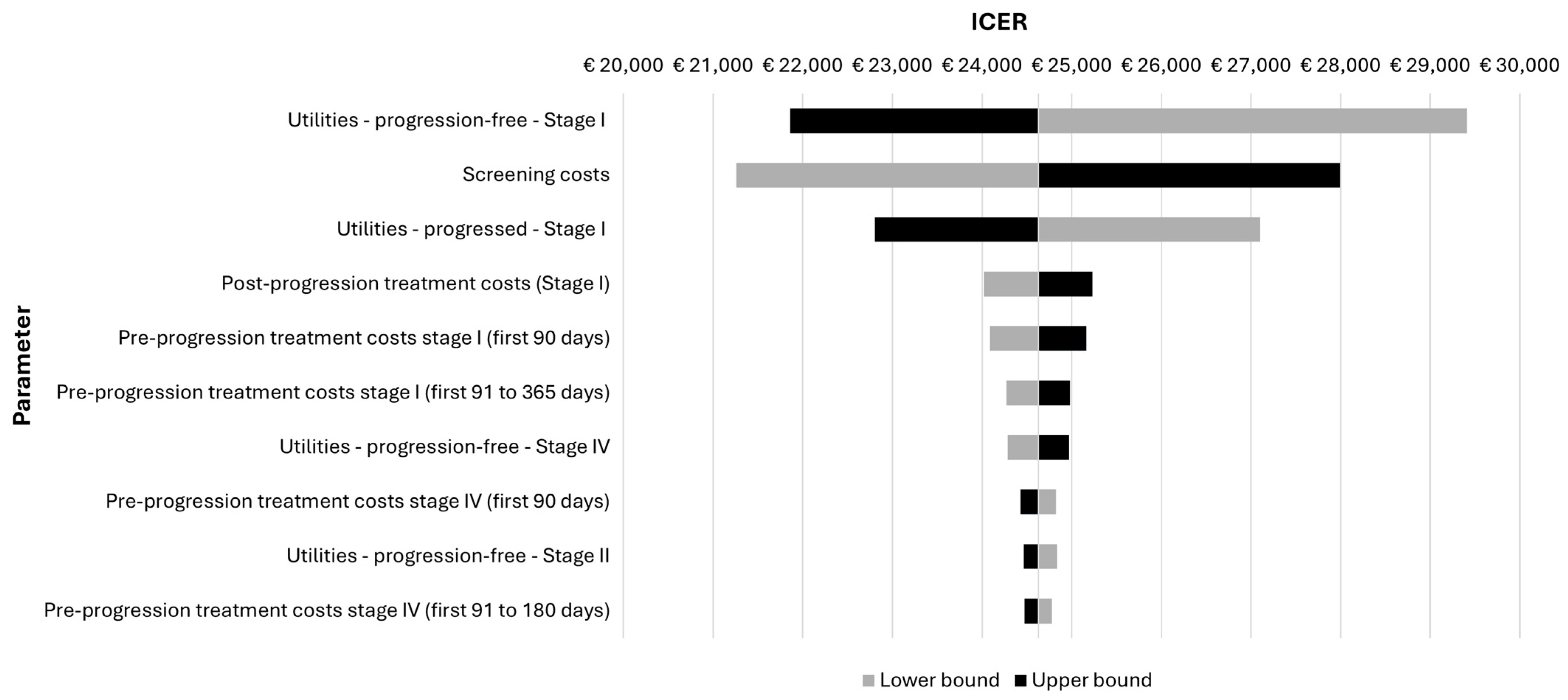
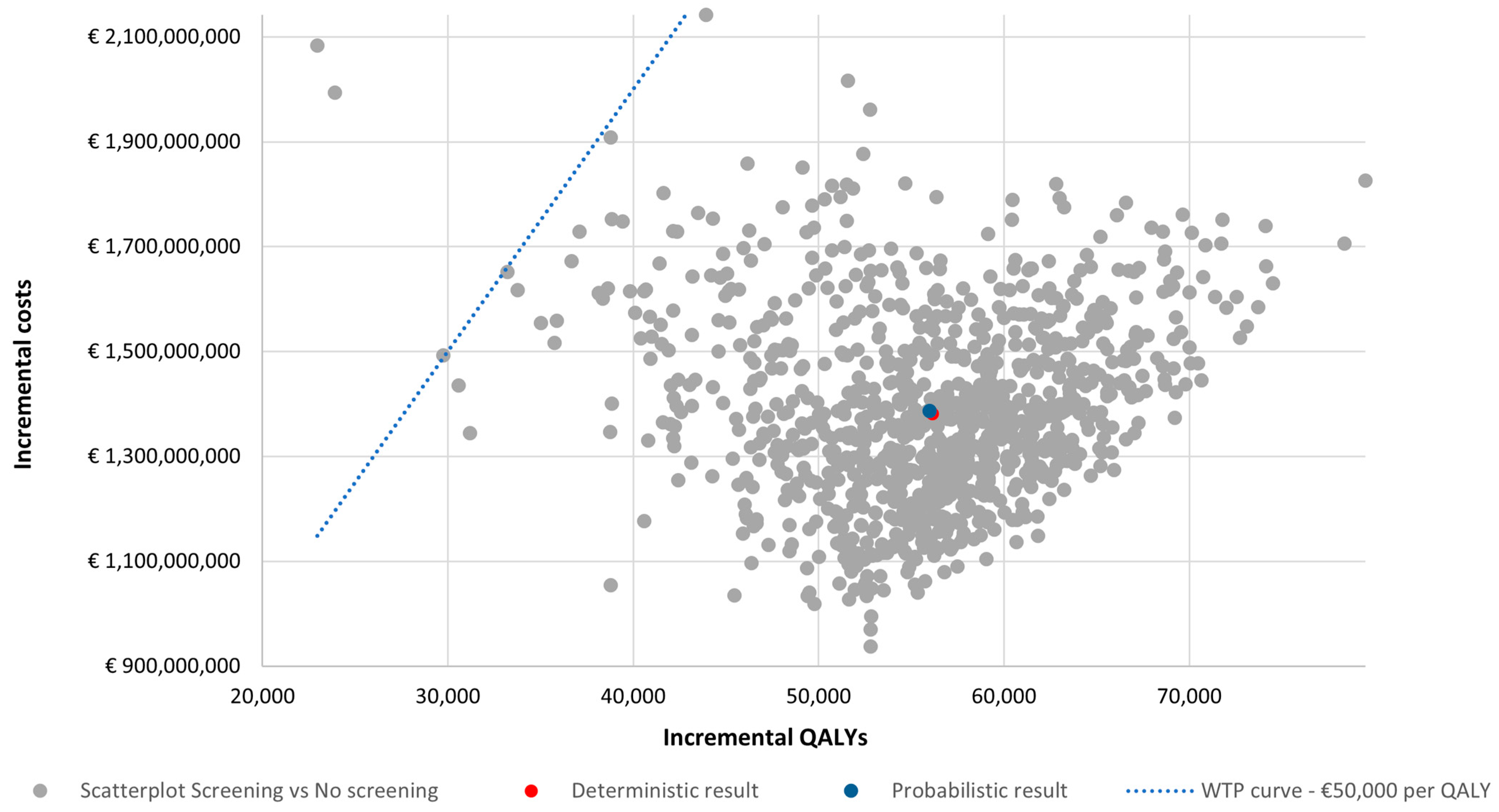
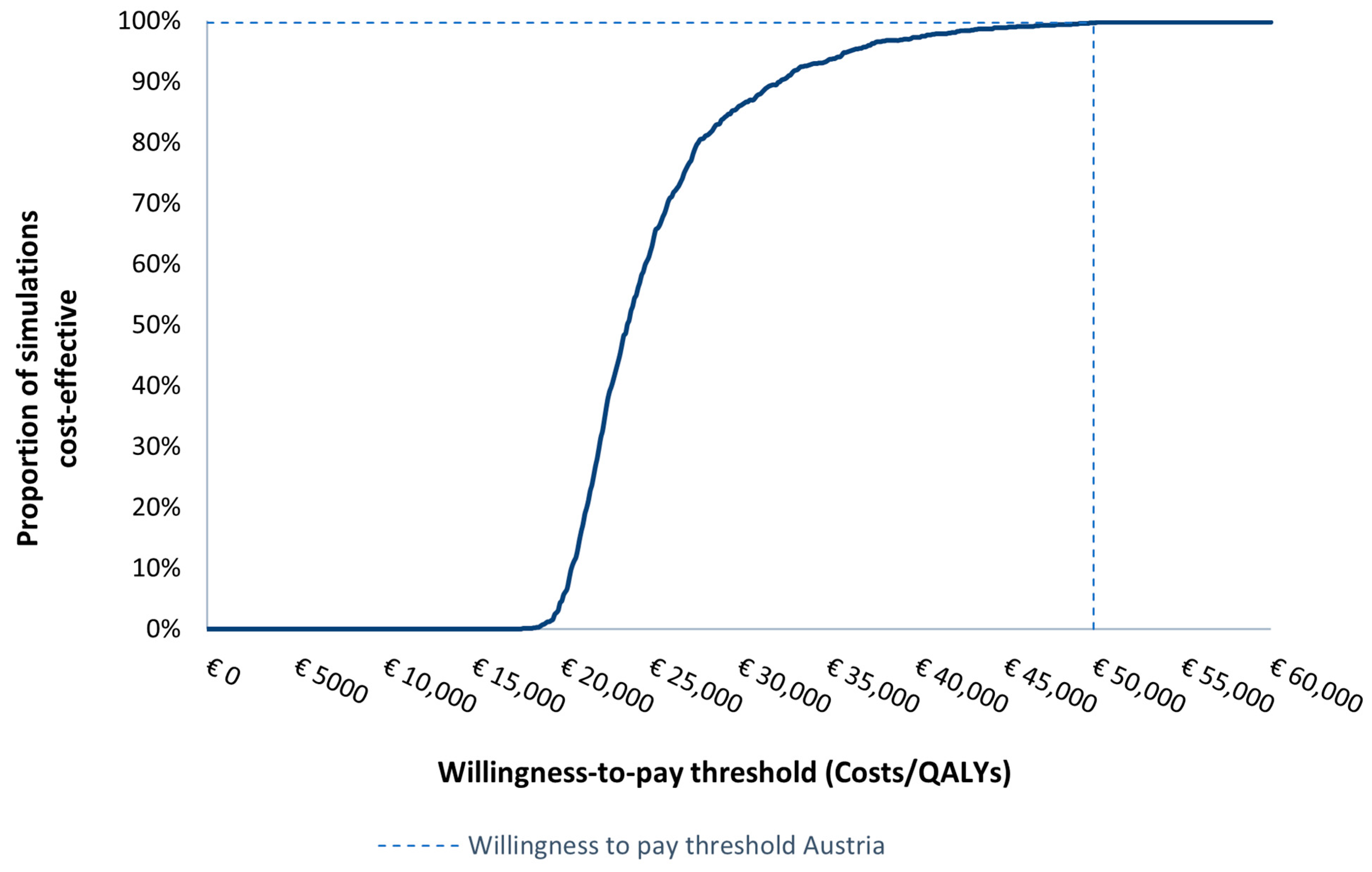
3.2. Sensitivity Analyses
3.3. Scenario Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Craig, H.; Are, C. Incidence and Cancer-Related Mortality in Austria—The ASCO Post. Available online: https://ascopost.com/issues/october-25-2022/incidence-and-cancer-related-mortality-in-austria/ (accessed on 11 October 2023).
- Pirker, R.; Prosch, H.; Popper, H.; Klepetko, W.; Dieckmann, K.; Burghuber, O.C.; Klikovits, T.; Hoda, M.A.; Zöchbauer-Müller, S.; Filipits, M. Lung Cancer in Austria. J. Thorac. Oncol. 2021, 16, 725–733. [Google Scholar] [CrossRef] [PubMed]
- Eberle, A.; Jansen, L.; Castro, F.; Krilaviciute, A.; Luttmann, S.; Emrich, K.; Holleczek, B.; Nennecke, A.; Katalinic, A.; Brenner, H.; et al. Lung Cancer Survival in Germany: A Population-Based Analysis of 132,612 Lung Cancer Patients. Lung Cancer 2015, 90, 528–533. [Google Scholar] [CrossRef] [PubMed]
- The National Lung Screening Trial Research Team. Reduced Lung-Cancer Mortality with Low-Dose Computed Tomographic Screening. N. Engl. J. Med. 2011, 365, 395–409. [Google Scholar] [CrossRef]
- de Koning, H.J.; van der Aalst, C.M.; de Jong, P.A.; Scholten, E.T.; Nackaerts, K.; Heuvelmans, M.A.; Lammers, J.-W.J.; Weenink, C.; Yousaf-Khan, U.; Horeweg, N.; et al. Reduced Lung-Cancer Mortality with Volume CT Screening in a Randomized Trial. N. Engl. J. Med. 2020, 382, 503–513. [Google Scholar] [CrossRef]
- Infante, M.; Lutman, F.R.; Cavuto, S.; Brambilla, G.; Chiesa, G.; Passera, E.; Angeli, E.; Chiarenza, M.; Aranzulla, G.; Cariboni, U.; et al. Lung Cancer Screening with Spiral CT: Baseline Results of the Randomized DANTE Trial. Lung Cancer 2008, 59, 355–363. [Google Scholar] [CrossRef] [PubMed]
- Pegna, A.L.; Picozzi, G.; Falaschi, F.; Carrozzi, L.; Falchini, M.; Carozzi, F.M.; Pistelli, F.; Comin, C.; Deliperi, A.; Grazzini, M.; et al. Four-Year Results of Low-Dose CT Screening and Nodule Management in the ITALUNG Trial. J. Thorac. Oncol. 2013, 8, 866–875. [Google Scholar] [CrossRef]
- Pastorino, U.; Rossi, M.; Rosato, V.; Marchianò, A.; Sverzellati, N.; Morosi, C.; Fabbri, A.; Galeone, C.; Negri, E.; Sozzi, G.; et al. Annual or Biennial CT Screening versus Observation in Heavy Smokers: 5-Year Results of the MILD Trial. Eur. J. Cancer Prev. 2012, 21, 308–315. [Google Scholar] [CrossRef] [PubMed]
- Becker, N.; Motsch, E.; Trotter, A.; Heussel, C.P.; Dienemann, H.; Schnabel, P.A.; Kauczor, H.U.; Maldonado, S.G.; Miller, A.B.; Kaaks, R.; et al. Lung Cancer Mortality Reduction by LDCT Screening-Results from the Randomized German LUSI Trial. Int. J. Cancer 2020, 146, 1503–1513. [Google Scholar] [CrossRef] [PubMed]
- Field, J.K.; Duffy, S.W.; Baldwin, D.R.; Brain, K.E.; Devaraj, A.; Eisen, T.; Green, B.A.; Holemans, J.A.; Kavanagh, T.; Kerr, K.M.; et al. The UK Lung Cancer Screening Trial: A Pilot Randomised Controlled Trial of Low-Dose Computed Tomography Screening for the Early Detection of Lung Cancer. Health Technol. Assess. 2016, 20, 1–146. [Google Scholar] [CrossRef] [PubMed]
- Walser, T.; Cui, X.; Yanagawa, J.; Lee, J.M.; Heinrich, E.; Lee, G.; Sharma, S.; Dubinett, S.M. Smoking and Lung Cancer: The Role of Inflammation. Proc. Am. Thorac. Soc. 2008, 5, 811–815. [Google Scholar] [CrossRef] [PubMed]
- Council of the European Union. Council Recommendation on Strengthening Prevention through Early Detection: A New EU Approach on Cancer Screening; Council of the European Union: Brussels, Belgium, 2022.
- Wait, S.; Alvarez-Rosete, A.; Osama, T.; Bancroft, D.; Cornelissen, R.; Marušić, A.; Garrido, P.; Adamek, M.; van Meerbeeck, J.; Snoeckx, A.; et al. Implementing Lung Cancer Screening in Europe: Taking a Systems Approach. JTO Clin. Res. Rep. 2022, 3, 100329. [Google Scholar] [CrossRef] [PubMed]
- Pîrlog, C.F.; Costache, R.; Paroșanu, A.I.; Slavu, C.O.; Olaru, M.; Popa, A.M.; Iaciu, C.; Niță, I.; Moțatu, P.; Cotan, H.T.; et al. Restricted Mean Survival Time-Can It Be a New Tool in Assessing the Survival of Non-Small Cell Lung Cancer Patients Treated with Immune Checkpoint Inhibitors? Diagnostics 2023, 13, 1892. [Google Scholar] [CrossRef] [PubMed]
- Putzu, C.; Canova, S.; Paliogiannis, P.; Lobrano, R.; Sala, L.; Cortinovis, D.L.; Colonese, F. Duration of Immunotherapy in Non-Small Cell Lung Cancer Survivors: A Lifelong Commitment? Cancers 2023, 15, 689. [Google Scholar] [CrossRef] [PubMed]
- Berger, M.; Mayer, S.; Simon, J. A Novel Set of Austrian Reference Unit Costs for Comprehensive Societal Perspectives Consistent with Latest European Costing Methods for Economic Evaluations. Wien. Klin. Wochenschr. 2022, 136, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Böhler, C.E.H.; Wolf, S. Lung Cancer Screening in Risk Groups (Part II): A Review-Update of the Economic Evidence; AIHTA Project Report No.: 132b; HTA Austria—Austrian Institute for Health Technology Assessment GmbH: Vienna, Austria, 2020. [Google Scholar]
- Walter, E.; Zehetmayr, S. Guidelines Zur Gesundheitsökonomischen Evaluation Konsenspapier. Wien. Med. Wochenschr. 2006, 156, 628–632. [Google Scholar] [CrossRef] [PubMed]
- Pan, X.; Dvortsin, E.; Baldwin, D.R.; Groen, H.J.M.; Ramaker, D.; Ryan, J.; ten Berge, H.; Velikanova, R.; Oudkerk, M.; Postma, M.J. Cost-Effectiveness of Volume Computed Tomography in Lung Cancer Screening: A Cohort Simulation Based on Nelson Study Outcomes. J. Med. Econ. 2024, 27, 27–38. [Google Scholar] [CrossRef] [PubMed]
- Edejer, T.T.-T. Making Choices in Health: WHO Guide to Cost-Effectiveness Analysis; World Health Organization: Geneva, Switzerland, 2003.
- International Monetary Fund. World Economic Outlook Database. Available online: https://www.imf.org/en/Publications/WEO/weo-database/2023/October (accessed on 1 May 2024).
- Horeweg, N.; Van Der Aalst, C.M.; Vliegenthart, R.; Zhao, Y.; Xie, X.; Scholten, E.T.; Mali, W.; Thunnissen, E.; Weenink, C.; Groen, H.J.M.; et al. Volumetric Computed Tomography Screening for Lung Cancer: Three Rounds of the NELSON Trial. Eur. Respir. J. 2013, 42, 1659–1667. [Google Scholar] [CrossRef] [PubMed]
- Postmus, P.E.; Kerr, K.M.; Oudkerk, M.; Senan, S.; Waller, D.A.; Vansteenkiste, J.; Escriu, C.; Peters, S. Early and Locally Advanced Non-Small-Cell Lung Cancer (NSCLC): ESMO Clinical Practice Guidelines for Diagnosis, Treatment and Follow-Up. Ann. Oncol. 2017, 28, iv1–iv21. [Google Scholar] [CrossRef] [PubMed]
- Yousaf-Khan, U.; Van Der Aalst, C.; De Jong, P.A.; Heuvelmans, M.; Scholten, E.; Lammers, J.W.; Van Ooijen, P.; Nackaerts, K.; Weenink, C.; Groen, H.; et al. Final Screening Round of the NELSON Lung Cancer Screening Trial: The Effect of a 2.5-Year Screening Interval. Thorax 2017, 72, 48–56. [Google Scholar] [CrossRef] [PubMed]
- Xu, D.M.; Gietema, H.; de Koning, H.; Vernhout, R.; Nackaerts, K.; Prokop, M.; Weenink, C.; Lammers, J.W.; Groen, H.; Oudkerk, M.; et al. Nodule Management Protocol of the NELSON Randomised Lung Cancer Screening Trial. Lung Cancer 2006, 54, 177–184. [Google Scholar] [CrossRef]
- Statistics Austria. Population at Beginning of Year/Quarter. Available online: https://www.statistik.at/en/statistics/population-and-society/population/population-stock/population-at-beginning-of-year/quarter (accessed on 11 January 2023).
- United Nations Department of Economics and Social Affairs. Population Division. 2022. Available online: https://population.un.org/wpp/Download/Standard/Population/ (accessed on 3 May 2023).
- Statistics Austria. Population by Age/Sex. Available online: https://www.statistik.at/en/statistics/population-and-society/population/population-stock/population-by-age-/sex (accessed on 19 September 2023).
- Statistics Austria. Smoking Habits. Available online: https://www.statistik.at/en/statistics/population-and-society/health/health-determinants/smoking-habits (accessed on 13 September 2022).
- Grover, H.; King, W.; Bhattarai, N.; Moloney, E.; Sharp, L.; Fuller, L. Systematic Review of the Cost-Effectiveness of Screening for Lung Cancer with Low Dose Computed Tomography. Lung Cancer 2022, 170, 20–33. [Google Scholar] [CrossRef] [PubMed]
- International Agency for Research on Cancer. Cancer Today. Available online: https://gco.iarc.fr/today/online-analysis-table?v=2020&mode=population&mode_population=countries&population=900&populations=900&key=asr&sex=0&cancer=15&type=0&statistic=5&prevalence=0&population_group=0&ages_group%5B%5D=0&ages_group%5B%5D=17&group_cancer=0&include_nmsc=0&include_nmsc_other=1 (accessed on 18 November 2022).
- Burghuber, O.C.; Kirchbacher, K.; Mohn-Staudner, A.; Hochmair, M.; Breyer, M.K.; Studnicka, M.; Mueller, M.R.; Feurstein, P.; Schrott, A.; Lamprecht, B.; et al. Results of the Austrian National Lung Cancer Audit. Clin. Med. Insights Oncol. 2020, 14, 1179554920950548. [Google Scholar] [CrossRef] [PubMed]
- Department of Health Economics (DHE), Center for Public Health, Medical University of Vienna. DHE Unit Cost Online Database: Cost Collection from Existing Studies; Version 3.1/2019; Medical University of Vienna: Vienna, Austria, 2019. [Google Scholar]
- Mayer, S.; Kiss, N.; Łaszewska, A.; Simon, J. Costing Evidence for Health Care Decision-Making in Austria: A Systematic Review. PLoS ONE 2017, 12, e0183116. [Google Scholar] [CrossRef] [PubMed]
- Kassenärztliche Bundesvereinigung Germany (National Association of Statutory Health Insurance Physicians). EBM. Available online: https://www.kbv.de/html/13259.php?srt=relevance&stp=fulltext&q=Bronchoskopie&s=Zoeken (accessed on 2 August 2023).
- Schwarzkopf, L.; Wacker, M.; Holle, R.; Leidl, R.; Günster, C.; Adler, J.B.; Huber, R.M. Cost-Components of Lung Cancer Care within the First Three Years after Initial Diagnosis in Context of Different Treatment Regimens. Lung Cancer 2015, 90, 274–280. [Google Scholar] [CrossRef] [PubMed]
- Hofer, F.; Kauczor, H.U.; Stargardt, T. Cost-Utility Analysis of a Potential Lung Cancer Screening Program for a High-Risk Population in Germany: A Modelling Approach. Lung Cancer 2018, 124, 189–198. [Google Scholar] [CrossRef] [PubMed]
- McGahan, L. Pembrolizumab (Keytruda®) as First-Line Therapy for PD-L1-Expressing, Locally Advanced or Metastatic Non-Small-Cell Lung Cancer (NSCLC). In DSD: Horizon Scanning in Oncology 91; Ludwig Boltzmann Institute for Health Technology Assessments: Vienna, Austria, 2019. [Google Scholar]
- Grössmann, N. Atezolizumab (Tecentriq®) as Monotherapy for the First-Line Treatment of Adult Patients with Metastatic Non-Small Cell Lung Cancer (NSCLC). In Oncology Fact Sheet Nr. 45; HTA Austria—Austrian Institute for Health Technology Assessment GmbH: Vienna, Austria, 2021. [Google Scholar]
- Mok, T.; Camidge, D.R.; Gadgeel, S.M.; Rosell, R.; Dziadziuszko, R.; Kim, D.-W.; Pérol, M.; Ou, S.-H.I.; Ahn, J.S.; Shaw, A.T.; et al. Updated Overall Survival and Final Progression-Free Survival Data for Patients with Treatment-Naive Advanced ALK-Positive Non-Small-Cell Lung Cancer in the ALEX Study. Ann. Oncol. 2020, 31, 1056–1064. [Google Scholar] [CrossRef] [PubMed]
- Soria, J.-C.; Ohe, Y.; Vansteenkiste, J.; Reungwetwattana, T.; Chewaskulyong, B.; Lee, K.H.; Dechaphunkul, A.; Imamura, F.; Nogami, N.; Kurata, T.; et al. Osimertinib in Untreated EGFR-Mutated Advanced Non-Small-Cell Lung Cancer. N. Engl. J. Med. 2018, 378, 113–125. [Google Scholar] [CrossRef] [PubMed]
- Park, K.; Tan, E.H.; O’Byrne, K.; Zhang, L.; Boyer, M.; Mok, T.; Hirsh, V.; Yang, J.C.H.; Lee, K.H.; Lu, S.; et al. Afatinib versus Gefitinib as First-Line Treatment of Patients with EGFR Mutation-Positive Non-Small-Cell Lung Cancer (LUX-Lung 7): A Phase 2B, Open-Label, Randomised Controlled Trial. Lancet. Oncol. 2016, 17, 577–589. [Google Scholar] [CrossRef] [PubMed]
- Shaw, A.T.; Bauer, T.M.; de Marinis, F.; Felip, E.; Goto, Y.; Liu, G.; Mazieres, J.; Kim, D.-W.; Mok, T.; Polli, A.; et al. First-Line Lorlatinib or Crizotinib in Advanced ALK-Positive Lung Cancer. N. Engl. J. Med. 2020, 383, 2018–2029. [Google Scholar] [CrossRef] [PubMed]
- Österreichische Sozialversicherung (Austrian Social Insurance). Information Tool on the Reimbursement Code. Available online: https://www.sozialversicherung.at/oeko/views/index.xhtml (accessed on 1 August 2023).
- Wolf, A.; Stratmann, J.A.; Shaid, S.; Niklas, N.; Calleja, A.; Ubhi, H.; Munro, R.; Waldenberger, D.; Carroll, R.; Daumont, M.J.; et al. Evolution of Treatment Patterns and Survival Outcomes in Patients with Advanced Non-Small Cell Lung Cancer Treated at Frankfurt University Hospital in 2012-2018. BMC Pulm. Med. 2023, 23, 16. [Google Scholar] [CrossRef] [PubMed]
- Reck, M.; Rodríguez-Abreu, D.; Robinson, A.G.; Hui, R.; Csoszi, T.; Fülöp, A.; Gottfried, M.; Peled, N.; Tafreshi, A.; Cuffe, S.; et al. Updated Analysis of KEYNOTE-024: Pembrolizumab versus Platinum-Based Chemotherapy for Advanced Non–Small-Cell Lung Cancer with PD-L1 Tumor Proportion Score of 50% or Greater. J. Clin. Oncol. 2019, 37, 537–546. [Google Scholar] [CrossRef]
- Gadgeel, S.; Rodríguez-Abreu, D.; Speranza, G.; Esteban, E.; Felip, E.; Dómine, M.; Hui, R.; Hochmair, M.J.; Clingan, P.; Powell, S.F.; et al. Updated Analysis From KEYNOTE-189: Pembrolizumab or Placebo Plus Pemetrexed and Platinum for Previously Untreated Metastatic Nonsquamous Non-Small-Cell Lung Cancer. J. Clin. Oncol. 2020, 38, 1505–1517. [Google Scholar] [CrossRef] [PubMed]
- Antonia, S.J.; Villegas, A.; Daniel, D.; Vicente, D.; Murakami, S.; Hui, R.; Yokoi, T.; Chiappori, A.; Lee, K.H.; de Wit, M.; et al. Durvalumab after Chemoradiotherapy in Stage III Non–Small-Cell Lung Cancer. N. Engl. J. Med. 2017, 377, 1919–1929. [Google Scholar] [CrossRef] [PubMed]
- Socinski, M.A.; Jotte, R.M.; Cappuzzo, F.; Orlandi, F.; Stroyakovskiy, D.; Nogami, N.; Rodríguez-Abreu, D.; Moro-Sibilot, D.; Thomas, C.A.; Barlesi, F.; et al. Atezolizumab for First-Line Treatment of Metastatic Nonsquamous NSCLC. N. Engl. J. Med. 2018, 378, 2288–2301. [Google Scholar] [CrossRef] [PubMed]
- Socinski, M.A.; Nishio, M.; Jotte, R.M.; Cappuzzo, F.; Orlandi, F.; Stroyakovskiy, D.; Nogami, N.; Rodríguez-Abreu, D.; Moro-Sibilot, D.; Thomas, C.A.; et al. IMpower150 Final Overall Survival Analyses for Atezolizumab Plus Bevacizumab and Chemotherapy in First-Line Metastatic Nonsquamous NSCLC. J. Thorac. Oncol. 2021, 16, 1909–1924. [Google Scholar] [CrossRef] [PubMed]
- McGahan, L. Durvalumab (ImfinziTM) for the Treatment of Patients with Stage III Non-Small-Cell Lung Cancer after Prior Chemoradiotherapy. In DSD: Horizon Scanning in Oncology 76; Ludwig Boltzmann Institute for Health Technology Assessments: Vienna, Austria, 2017. [Google Scholar]
- Blom, E.F.; ten Haaf, K.; de Koning, H.J. Systematic Review and Meta-Analysis of Community- and Choice-Based Health State Utility Values for Lung Cancer. Pharmacoeconomics 2020, 38, 1187–1200. [Google Scholar] [CrossRef]
- Goldstraw, P.; Chansky, K.; Crowley, J.; Rami-Porta, R.; Asamura, H.; Eberhardt, W.E.E.; Nicholson, A.G.; Groome, P.; Mitchell, A.; Bolejack, V.; et al. The IASLC Lung Cancer Staging Project: Proposals for Revision of the TNM Stage Groupings in the Forthcoming (Eighth) Edition of the TNM Classification for Lung Cancer. J. Thorac. Oncol. 2016, 11, 39–51. [Google Scholar] [CrossRef]
- McPherson, I.; Bradley, N.A.; Govindraj, R.; Kennedy, E.D.; Kirk, A.J.B.; Asif, M. The Progression of Non-Small Cell Lung Cancer from Diagnosis to Surgery. Eur. J. Surg. Oncol. 2020, 46, 1882–1887. [Google Scholar] [CrossRef]
- Felip, E.; Altorki, N.; Zhou, C.; Csőszi, T.; Vynnychenko, I.; Goloborodko, O.; Luft, A.; Akopov, A.; Martinez-Marti, A.; Kenmotsu, H.; et al. Adjuvant Atezolizumab after Adjuvant Chemotherapy in Resected Stage IB–IIIA Non-Small-Cell Lung Cancer (IMpower010): A Randomised, Multicentre, Open-Label, Phase 3 Trial. Lancet 2021, 398, 1344–1357. [Google Scholar] [CrossRef]
- Gandhi, L.; Rodríguez-Abreu, D.; Gadgeel, S.; Esteban, E.; Felip, E.; De Angelis, F.; Domine, M.; Clingan, P.; Hochmair, M.J.; Powell, S.F.; et al. Pembrolizumab plus Chemotherapy in Metastatic Non–Small-Cell Lung Cancer. N. Engl. J. Med. 2018, 378, 2078–2092. [Google Scholar] [CrossRef] [PubMed]
- Horn, L.; Mansfield, A.S.; Szczęsna, A.; Havel, L.; Krzakowski, M.; Hochmair, M.J.; Huemer, F.; Losonczy, G.; Johnson, M.L.; Nishio, M.; et al. First-Line Atezolizumab plus Chemotherapy in Extensive-Stage Small-Cell Lung Cancer. N. Engl. J. Med. 2018, 379, 2220–2229. [Google Scholar] [CrossRef] [PubMed]
- Statistics Austria. Life Tables. Available online: https://www.statistik.at/en/statistics/population-and-society/population/demographic-indicators-and-tables/life-tables (accessed on 11 July 2023).
- Guyot, P.; Ades, A.E.; Beasley, M.; Lueza, B.; Pignon, J.-P.; Welton, N.J. Extrapolation of Survival Curves from Cancer Trials Using External Information. Med. Decis. Making 2017, 37, 353–366. [Google Scholar] [CrossRef]
- Latimer, N. NICE DSU Technical Support Document 14: Survival Analysis for Economic Evaluations alongside Clinical Trials-Extrapolation with Patient-Level Data Report by the Decision Support Unit; Decision Support Unit: Sheffield, UK, 2011. [Google Scholar]
- Marten, O.; Greiner, W. EQ-5D-5L Reference Values for the German General Elderly Population. Health Qual. Life Outcomes 2021, 19, 76. [Google Scholar] [CrossRef] [PubMed]
- Szende, A.; Janssen, B.; Cabasés, J. Self-Reported Population Health: An International Perspective Based on EQ-5D; Springer: Dordrecht, The Netherlands, 2014; ISBN 9789400775961. [Google Scholar]
- Reck, M.; Rodríguez-Abreu, D.; Robinson, A.G.; Hui, R.; Csőszi, T.; Fülöp, A.; Gottfried, M.; Peled, N.; Tafreshi, A.; Cuffe, S.; et al. Pembrolizumab versus Chemotherapy for PD-L1-Positive Non-Small-Cell Lung Cancer. N. Engl. J. Med. 2016, 375, 1823–1833. [Google Scholar] [CrossRef] [PubMed]
- Statistics|Eurostat—HICP—Inflation Rate. Available online: https://ec.europa.eu/eurostat/databrowser/view/tec00118/default/table?lang=en (accessed on 20 September 2023).
- OECD (Organisation for Economic Co-Operation and Development) Purchasing Power Parities (PPP). Available online: https://data.oecd.org/conversion/purchasing-power-parities-ppp.htm (accessed on 20 September 2023).
- Czypionka, T.; Eisenberg, S.; Arnhold, T. Wert von Innovation Im Gesundheitswesen II: Beispiel Mammakarzinom [Value of Innovation in Healthcare II: Example of Breast Cancer]; Institute für Höhere Studien: Vienna, Austria, 2022. [Google Scholar]
- Goetz, G. Stool DNA Testing for Colorectal Cancer (CRC) Screening—Policy Brief. AIHTA Policy Brief 011; Austrian Institute for Health Technology Assessment GmbH: Vienna, Austria, 2021. [Google Scholar]
- Treskova, M.; Aumann, I.; Golpon, H.; Vogel-Claussen, J.; Welte, T.; Kuhlmann, A. Trade-off between Benefits, Harms and Economic Efficiency of Low-Dose CT Lung Cancer Screening: A Microsimulation Analysis of Nodule Management Strategies in a Population-Based Setting. BMC Med. 2017, 15, 162. [Google Scholar] [CrossRef] [PubMed]
- Veronesi, G.; Navone, N.; Novellis, P.; Dieci, E.; Toschi, L.; Velutti, L.; Solinas, M.; Vanni, E.; Alloisio, M.; Ghislandi, S. Favorable Incremental Cost-Effectiveness Ratio for Lung Cancer Screening in Italy. Lung Cancer 2020, 143, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Jahn, B.; Sroczynski, G.; Bundo, M.; Mühlberger, N.; Puntscher, S.; Todorovic, J.; Rochau, U.; Oberaigner, W.; Koffijberg, H.; Fischer, T.; et al. Effectiveness, Benefit Harm and Cost Effectiveness of Colorectal Cancer Screening in Austria. BMC Gastroenterol. 2019, 19, 209. [Google Scholar] [CrossRef] [PubMed]
- Schiller-Fruehwirth, I.; Jahn, B.; Einzinger, P.; Zauner, G.; Urach, C.; Siebert, U. The Long-Term Effectiveness and Cost Effectiveness of Organized versus Opportunistic Screening for Breast Cancer in Austria. Value Health 2017, 20, 1048–1057. [Google Scholar] [CrossRef] [PubMed]
- Kerpel-Fronius, A.; Monostori, Z.; Kovacs, G.; Ostoros, G.; Horvath, I.; Solymosi, D.; Pipek, O.; Szatmari, F.; Kovacs, A.; Markoczy, Z.; et al. Nationwide Lung Cancer Screening with Low-Dose Computed Tomography: Implementation and First Results of the HUNCHEST Screening Program. Eur. Radiol. 2022, 32, 4457–4467. [Google Scholar] [CrossRef] [PubMed]
- Field, J.K.; Vulkan, D.; Davies, M.P.A.; Baldwin, D.R.; Brain, K.E.; Devaraj, A.; Eisen, T.; Gosney, J.; Green, B.A.; Holemans, J.A.; et al. Lung Cancer Mortality Reduction by LDCT Screening: UKLS Randomised Trial Results and International Meta-Analysis. Lancet Reg. Health Eur. 2021, 10, 100179. [Google Scholar] [CrossRef] [PubMed]
- Pozzessere, C.; von Garnier, C.; Beigelman-Aubry, C. Radiation Exposure to Low-Dose Computed Tomography for Lung Cancer Screening: Should We Be Concerned? Tomography 2023, 9, 166–177. [Google Scholar] [CrossRef]
- Grutters, J.P.C.; Joore, M.A.; Wiegman, E.M.; Langendijk, J.A.; De Ruysscher, D.; Hochstenbag, M.; Botterweck, A.; Lambin, P.; Pijls-Johannesma, M. Health-Related Quality of Life in Patients Surviving Non-Small Cell Lung Cancer. Thorax 2010, 65, 903–907. [Google Scholar] [CrossRef] [PubMed]
- van den Hout, W.B.; Kramer, G.W.P.M.; Noordijk, E.M.; Leer, J.W.H. Cost-Utility Analysis of Short- versus Long-Course Palliative Radiotherapy in Patients with Non-Small-Cell Lung Cancer. J. Natl. Cancer Inst. 2006, 98, 1786–1794. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Matter-Walstra, K.; Klingbiel, D.; Szucs, T.; Pestalozzi, B.C.; Schwenkglenks, M. Using the EuroQol EQ-5D in Swiss Cancer Patients, Which Value Set Should Be Applied? Pharmacoeconomics 2014, 32, 591–599. [Google Scholar] [CrossRef] [PubMed]
- Bendixen, M.; Kronborg, C.; Jørgensen, O.D.; Andersen, C.; Licht, P.B. Cost-Utility Analysis of Minimally Invasive Surgery for Lung Cancer: A Randomized Controlled Trial. Eur. J. Cardiothorac. Surg. 2019, 56, 754–761. [Google Scholar] [CrossRef] [PubMed]
- Maximiano, C.; López, I.; Martõn, C.; Zugazabeitia, L.; Martõ-Ciriquián, J.L.; Núñez, M.A.; Contreras, J.; Herdman, M.; Traseira, S.; Provencio, M. An Exploratory, Large-Scale Study of Pain and Quality of Life Outcomes in Cancer Patients with Moderate or Severe Pain, and Variables Predicting Improvement. PLoS ONE 2018, 13, e0193233. [Google Scholar] [CrossRef] [PubMed]
- Meregaglia, M.; Borsoi, L.; Cairns, J.; Tarricone, R. Mapping Health-Related Quality of Life Scores from FACT-G, FAACT, and FACIT-F onto Preference-Based EQ-5D-5L Utilities in Non-Small Cell Lung Cancer Cachexia. Eur. J. Health Econ. 2019, 20, 181–193. [Google Scholar] [CrossRef] [PubMed]
- Lancaster, H.L.; Zheng, S.; Aleshina, O.O.; Yu, D.; Chernina, V.Y.; Heuvelmans, M.A.; de Bock, G.H.; Dorrius, M.D.; Willem Gratama, J.; Morozov, S.P.; et al. Outstanding Negative Prediction Performance of Solid Pulmonary Nodule Volume AI for Ultra-LDCT Baseline Lung Cancer Screening Risk Stratification. Lung Cancer 2022, 165, 133–140. [Google Scholar] [CrossRef] [PubMed]
- Gollmer, A.; Link, T. Weißenhofer Sabine Dritter Evaluati Onsbericht Zum Österreichischen Brustkrebs-Früherkennungsprogramm. Evaluationsbericht Für Die Jahre 2014 Bis 2019 (Third Evaluation Report on the Austrian Breast Cancer Early Detection Program. Evaluation Report for the Years 2014 to 2019); Gesundheit Österreich: Vienna, Austria, 2021. [Google Scholar]
- European Federation of Pharmaceutical Industries and Associations. The Root Cause of Unavailability and Delay to Innovative Medicines: Reducing the Time before Patients Have Access to Innovative Medicines; European Federation of Pharmaceutical Industries and Associations: Brussel, Belgium, 2022. [Google Scholar]
- Ismail, R.K.; Schramel, F.M.N.H.; van Dartel, M.; Hilarius, D.L.; de Boer, A.; Wouters, M.W.J.M.; Smit, H.J.M. The Dutch Lung Cancer Audit: Nationwide Quality of Care Evaluation of Lung Cancer Patients. Lung Cancer 2020, 149, 68–77. [Google Scholar] [CrossRef] [PubMed]
- NHS England. Targeted Screening for Lung Cancer with Low Radiation Dose Computed Tomography—Standard Protocol Prepared for the Targeted Lung Health Checks Programme; NHS: London, UK, 2022.
- European Commission. 4-IN THE LUNG RUN: Towards INdividually Tailored INvitations, Screening INtervals, and INtegrated Co-Morbidity Reducing Strategies in Lung Cancer Screening. Available online: https://cordis.europa.eu/project/id/848294 (accessed on 27 October 2023).
- Tomonaga, Y.; de Nijs, K.; Bucher, H.C.; de Koning, H.; ten Haaf, K. Cost-Effectiveness of Risk-Based Low-Dose Computed Tomography Screening for Lung Cancer in Switzerland. Int. J. Cancer 2024, 154, 636–647. [Google Scholar] [CrossRef] [PubMed]
- Brain, K.; Carter, B.; Lifford, K.J.; Burke, O.; Devaraj, A.; Baldwin, D.R.; Duffy, S.; Field, J.K. Impact of Low-Dose CT Screening on Smoking Cessation among High-Risk Participants in the UK Lung Cancer Screening Trial. Thorax 2017, 72, 912–918. [Google Scholar] [CrossRef] [PubMed]
- Sheikh, M.; Mukeriya, A.; Shangina, O.; Brennan, P.; Zaridze, D. Postdiagnosis Smoking Cessation and Reduced Risk for Lung Cancer Progression and Mortality: A Prospective Cohort Study. Ann. Intern. Med. 2021, 174, 1232–1239. [Google Scholar] [CrossRef] [PubMed]
| Screening | No Screening | Incremental | |
|---|---|---|---|
| Clinical and health outcomes | |||
| Lung cancer diagnoses | |||
| Total | 61,039 (100%) | 40,667 (100%) | 20,372 |
| Stage I | 31,182 (51%) | 6629 (16%) | 24,553 |
| Stage II | 4512 (7%) | 3172 (8%) | 1340 |
| Stage III | 12,029 (20%) | 11,265 (28%) | 764 |
| Stage IV | 13,317 (22%) | 19,602 (48%) | −6285 |
| Missed individuals | NA. | 20,372 | NA. |
| Stage III and IV averted | 5521 | ||
| Lung cancer deaths | |||
| Total | 37,986 | 49,893 | −11,906 |
| Stage I | 11,645 | 2473 | 9173 |
| Stage II | 2394 | 1681 | 713 |
| Stage III | 10,947 | 10,244 | 704 |
| Stage IV | 13,000 | 19,135 | −6135 |
| Missed individuals | NA. | 16,361 | NA. |
| LYs | |||
| Total | 8,143,767 | 8,059,718 | 84,049 |
| Stage I | 207,142 | 43,808 | 163,334 |
| Stage II | 23,215 | 16,070 | 7145 |
| Stage III | 28,653 | 26,607 | 2045 |
| Stage IV | 13,378 | 19,668 | −6290 |
| Missed individuals | NA. | 82,186 | −82,186 |
| Lung cancer-free individuals * | 7,871,380 | 7,871,380 | 0 |
| QALYs | |||
| Total | 7,094,500 | 7,038,378 | 56,122 |
| Stage I | 159,154 | 33,646 | 125,507 |
| Stage II | 18,071 | 12,493 | 5578 |
| Stage III | 19,760 | 18,349 | 1411 |
| Stage IV | 9230 | 13,570 | −4340 |
| Missed individuals | NA. | 72,034 | NA. |
| Lung-cancer-free individuals * | 6,888,286 | 6,888,286 | 0 |
| Cost outcomes | |||
| Total | EUR 2,667,599,196 | EUR 1,285,508,127 | EUR 1,382,091,070 |
| Recruitment costs | EUR 15,658,995 | − | EUR 15,658,995 |
| Screening costs | EUR 944,862,093 | − | EUR 944,862,093 |
| Diagnostic costs | EUR 67,205,929 | EUR 31,641,587 | EUR 35,564,342 |
| Treatment costs | EUR 1,639,872,179 | EUR 1,253,866,539 | EUR 386,005,640 |
| Stage I | EUR 628,288,448 | EUR 133,053,631 | EUR 495,234,817 |
| Stage II | EUR 83,909,760 | EUR 58,326,545 | EUR 25,583,215 |
| Stage III | EUR 557,339,147 | EUR 518,006,566 | EUR 39,332,581 |
| Stage IV | EUR 370,334,824 | EUR 544,479,797 | EUR −174,144,972 |
| Health economic outcomes | |||
| ICER (per QALY) | EUR 24,627 | ||
| NMB | EUR 1,424,012,194 |
| Scenario Name | Screening | No Screening | Incremental Total Costs | Incremental QALYs | ICER | ||
|---|---|---|---|---|---|---|---|
| Total Costs | Total QALYs | Total Costs | Total QALYs | ||||
| Base-case analysis | EUR 2,667,599,196 | 7,094,500 | EUR 1,285,508,127 | 7,038,378 | EUR 1,382,091,070 | 56,122 | EUR 24,627 |
| Time horizon—10 year | EUR 1,875,220,197 | 4,246,046 | EUR 892,861,312 | 4,237,076 | EUR 982,358,885 | 8,970 | EUR 109,510 |
| Time horizon—20 year | EUR 2,654,058,718 | 6,260,895 | EUR 1,279,280,611 | 6,224,315 | EUR 1,374,778,107 | 36,580 | EUR 37,583 |
| Time horizon—30 year | EUR 2,666,645,093 | 6,961,351 | EUR 1,285,182,774 | 6,908,586 | EUR 1,381,462,318 | 52,765 | EUR 26,182 |
| Decrease discount rate (costs: 0%, health outcomes: 0%) | EUR 3,817,460,602 | 12,072,272 | EUR 1,852,663,992 | 11,934,416 | EUR 1,964,796,609 | 137,856 | EUR 14,252 |
| Decrease discount rate (costs: 3%, health outcomes: 3%) | EUR 3,049,548,566 | 8,572,349 | EUR 1,473,957,511 | 8,493,647 | EUR 1,575,591,055 | 78,702 | EUR 20,020 |
| Increase discount rate (costs: 10%, health outcomes: 10%) | EUR 2,002,629,443 | 4,894,393 | EUR 957,437,818 | 4,867,585 | EUR 1,045,191,625 | 26,808 | EUR 38,989 |
| Number of screening rounds—3 | EUR 755,476,931 | 7,308,584 | EUR 343,798,748 | 7,290,868 | EUR 411,678,182 | 17,716 | EUR 23,237 |
| Number of screening rounds—5 | EUR 1,154,543,454 | 7,262,156 | EUR 539,349,004 | 7,234,965 | EUR 615,194,450 | 27,191 | EUR 22,625 |
| Number of screening rounds—10 | EUR 1,946,938,252 | 7,165,845 | EUR 929,028,991 | 7,122,063 | EUR 1,017,909,262 | 43,782 | EUR 23,249 |
| Number of screening rounds—15 | EUR 2,500,355,235 | 7,109,451 | EUR 1,202,568,477 | 7,055,872 | EUR 1,297,786,758 | 53,579 | EUR 24,222 |
| Screening uptake rate—15.4% | EUR 1,731,160,173 | 7,108,068 | EUR 1,299,135,231 | 7,090,783 | EUR 432,024,942 | 17,286 | EUR 24,993 |
| Screening uptake rate—16.8% | EUR 1,769,050,770 | 7,107,519 | EUR 1,298,583,845 | 7,088,662 | EUR 470,466,924 | 18,857 | EUR 24,949 |
| Screening uptake rate—41.0% | EUR 2,424,016,791 | 7,098,029 | EUR 1,289,052,749 | 7,052,009 | EUR 1,134,964,042 | 46,020 | EUR 24,662 |
| Screening adherence rate—30% | EUR 1,530,137,034 | 7,107,153 | EUR 1,300,473,717 | 7,098,500 | EUR 229,663,317 | 8,652 | EUR 26,544 |
| Screening adherence rate—50% | EUR 1,591,597,866 | 7,106,196 | EUR 1,299,291,176 | 7,094,502 | EUR 292,306,691 | 11,694 | EUR 24,997 |
| Screening adherence rate—70% | EUR 1,719,499,677 | 7,104,353 | EUR 1,297,035,858 | 7,086,641 | EUR 422,463,819 | 17,713 | EUR 23,851 |
| Smoking rate—15% | EUR 1,930,107,627 | 5,126,375 | EUR 928,888,150 | 5,085,822 | EUR 1,001,219,478 | 40,553 | EUR 24,689 |
| Smoking rate—10% | EUR 1,289,792,798 | 3,417,583 | EUR 619,258,767 | 3,390,548 | EUR 670,534,032 | 27,035 | EUR 24,802 |
| Smoking rate—5% | EUR 649,477,969 | 1,708,792 | EUR 309,629,383 | 1,695,274 | EUR 339,848,586 | 13,518 | EUR 25,141 |
| CT scan costs of EUR 82 | EUR 1,998,099,825 | 7,094,500 | EUR 1,285,508,127 | 7,038,378 | EUR 712,591,699 | 56,122 | EUR 12,697 |
| CT scan costs of EUR 103 | EUR 2,071,380,174 | 7,094,500 | EUR 1,285,508,127 | 7,038,378 | EUR 785,872,048 | 56,122 | EUR 14,003 |
| CT scan costs of EUR 175 | EUR 2,312,370,826 | 7,094,500 | EUR 1,285,508,127 | 7,038,378 | EUR 1,026,862,699 | 56,122 | EUR 18,297 |
| Smoking cessation program (EUR 300) | EUR 2,757,682,436 | 7,094,500 | EUR 1,285,508,127 | 7,038,378 | EUR 1,472,174,309 | 56,122 | EUR 26,232 |
| Smoking cessation program (EUR 400) | EUR 2,787,710,182 | 7,094,500 | EUR 1,285,508,127 | 7,038,378 | EUR 1,502,202,056 | 56,122 | EUR 26,767 |
| Increase immunotherapy utilization for late-stage lung cancer patients by 10% | EUR 2,719,836,302 | 7,095,042 | EUR 1,345,885,191 | 7,039,047 | EUR 1,373,951,112 | 55,996 | EUR 24,537 |
| Increase immunotherapy utilization for late-stage lung cancer patients by 20% | EUR 2,756,338,111 | 7,095,042 | EUR 1,384,950,157 | 7,039,047 | EUR 1,371,387,954 | 55,996 | EUR 24,491 |
| Increase immunotherapy utilization for late-stage lung cancer patients by 50% | EUR 2,865,843,537 | 7,095,042 | EUR 1,502,145,055 | 7,039,047 | EUR 1,363,698,481 | 55,996 | EUR 24,354 |
| Increase immunotherapy utilization for late-stage lung cancer patients by 100% | EUR 3,048,352,580 | 7,095,042 | EUR 1,697,469,886 | 7,039,047 | EUR 1,350,882,693 | 55,996 | EUR 24,125 |
| Apply disutility to false positives and indeterminate scans—0.015 | EUR 2,667,599,196 | 7,090,329 | EUR 1,285,508,127 | 7,038,378 | EUR 1,382,091,070 | 51,952 | EUR 26,603 |
| Apply disutility to false positives and indeterminate scans—0.03 | EUR 2,667,599,196 | 7,086,159 | EUR 1,285,508,127 | 7,038,378 | EUR 1,382,091,070 | 47,781 | EUR 28,925 |
| Apply disutility to false positives and indeterminate scans—0.05 | EUR 2,667,599,196 | 7,080,598 | EUR 1,285,508,127 | 7,038,378 | EUR 1,382,091,070 | 42,221 | EUR 32,735 |
| Increase utility values for stage I lung cancer patients by 20% | EUR 2,667,599,196 | 7,106,650 | EUR 1,285,508,127 | 7,043,913 | EUR 1,382,091,070 | 62,738 | EUR 22,030 |
| Increase background mortality by 100% | EUR 2,495,998,363 | 6,191,043 | EUR 1,199,101,303 | 6,149,484 | EUR 1,296,897,061 | 41,559 | EUR 31,206 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
ten Berge, H.; Ramaker, D.; Piazza, G.; Pan, X.; Lamprecht, B.; Valipour, A.; Prosch, H. Shall We Screen Lung Cancer with Volume Computed Tomography in Austria? A Cost-Effectiveness Modelling Study. Cancers 2024, 16, 2623. https://doi.org/10.3390/cancers16152623
ten Berge H, Ramaker D, Piazza G, Pan X, Lamprecht B, Valipour A, Prosch H. Shall We Screen Lung Cancer with Volume Computed Tomography in Austria? A Cost-Effectiveness Modelling Study. Cancers. 2024; 16(15):2623. https://doi.org/10.3390/cancers16152623
Chicago/Turabian Styleten Berge, Hilde, Dianne Ramaker, Greta Piazza, Xuanqi Pan, Bernd Lamprecht, Arschang Valipour, and Helmut Prosch. 2024. "Shall We Screen Lung Cancer with Volume Computed Tomography in Austria? A Cost-Effectiveness Modelling Study" Cancers 16, no. 15: 2623. https://doi.org/10.3390/cancers16152623
APA Styleten Berge, H., Ramaker, D., Piazza, G., Pan, X., Lamprecht, B., Valipour, A., & Prosch, H. (2024). Shall We Screen Lung Cancer with Volume Computed Tomography in Austria? A Cost-Effectiveness Modelling Study. Cancers, 16(15), 2623. https://doi.org/10.3390/cancers16152623






