Enhancing Post-Mastectomy Care: Telehealth’s Impact on Breast Reconstruction Accessibility for Breast Cancer Patients
Abstract
Simple Summary
Abstract
1. Introduction
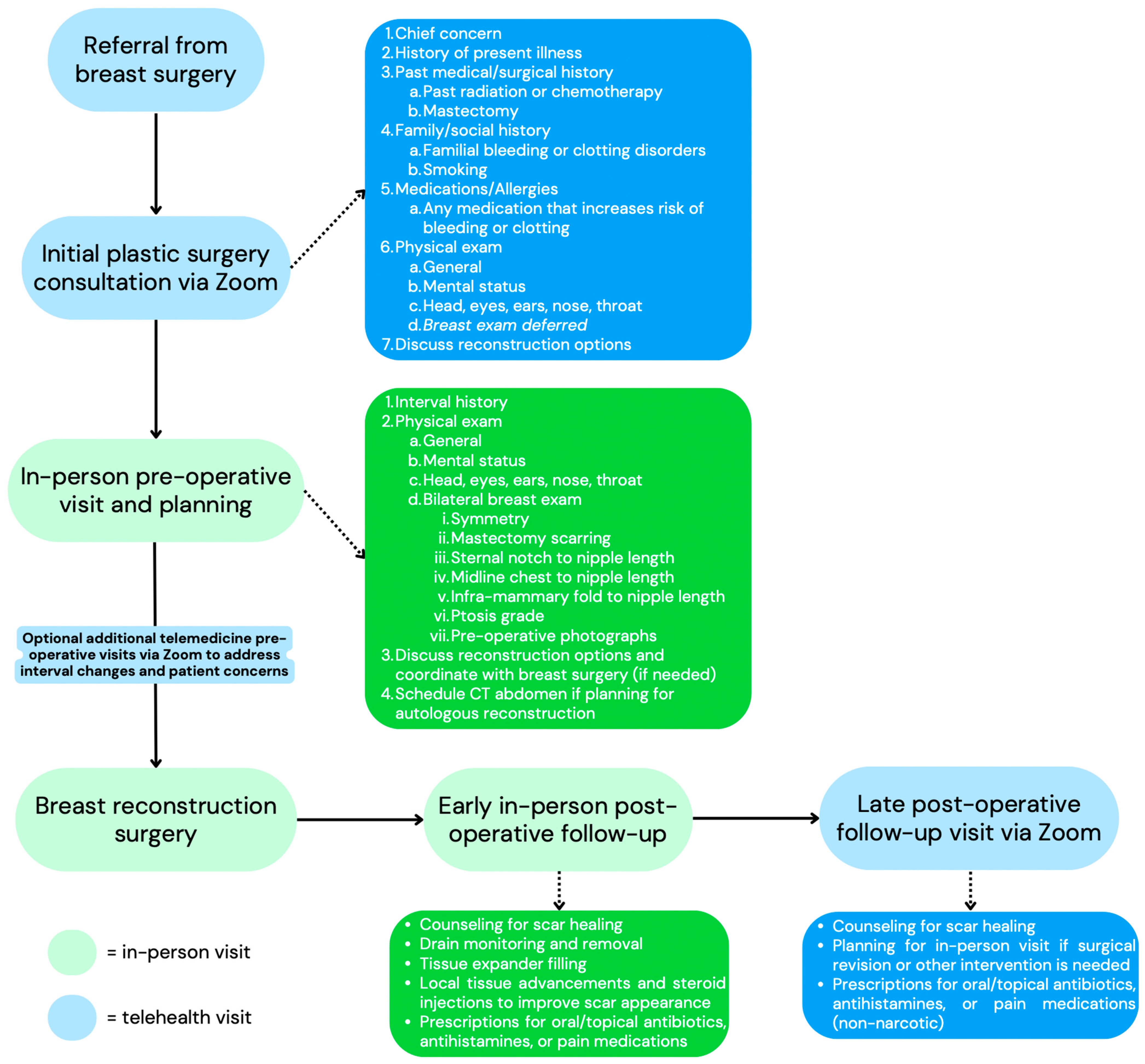
2. Methods
2.1. Study Setting and Design
2.2. Variables
2.3. Aims
2.4. Statistical Analysis
3. Results
3.1. Demographics
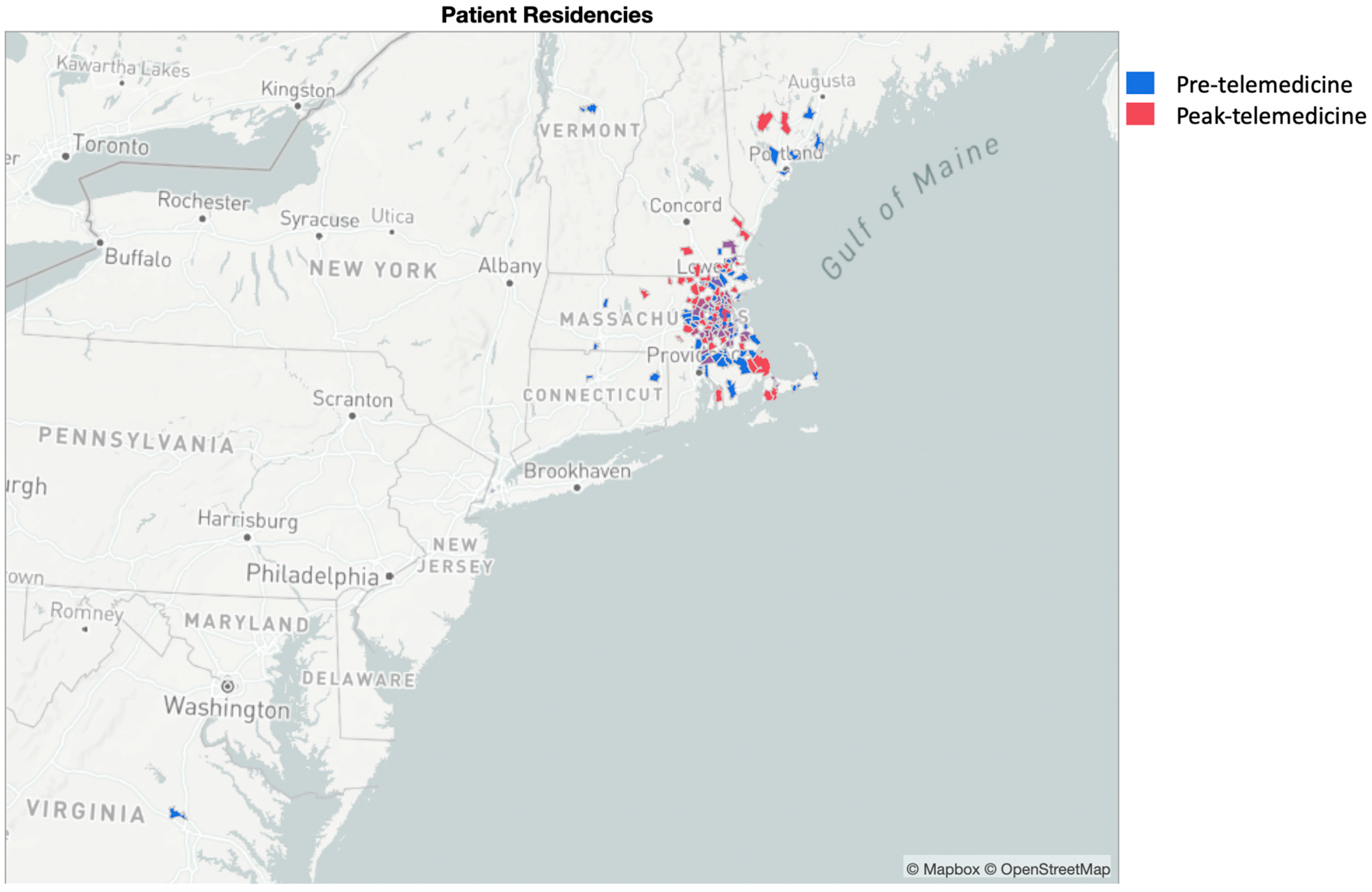
3.2. Distance and Breast Reconstruction Decision
3.3. Clinical Characteristics
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Female Breast Cancer—Cancer Stat Facts. Available online: https://seer.cancer.gov/statfacts/html/breast.html (accessed on 29 March 2022).
- Plevritis, S.K.; Munoz, D.; Kurian, A.W.; Stout, N.K.; Alagoz, O.; Near, A.M.; Lee, S.J.; van den Broek, J.J.; Huang, X.; Schechter, C.B.; et al. Association of Screening and Treatment with Breast Cancer Mortality by Molecular Subtype in US Women, 2000–2012. JAMA 2018, 319, 154–164. [Google Scholar] [CrossRef] [PubMed]
- Centers for Medicare and Medicaid Services. Women’s Health and Cancer Rights Act (WHCRA); U.S. Centers for Medicare & Medicaid Services: Baltimore, MD, USA, 1998. Available online: https://www.cms.gov/CCIIO/Programs-and-Initiatives/Other-Insurance-Protections/whcra_factsheet (accessed on 28 April 2022).
- Rubin, L.R.; Chavez, J.; Alderman, A.; Pusic, A.L. ‘Use what God has given me’: Difference and disparity in breast reconstruction. Psychol. Health 2013, 28, 1099–1120. [Google Scholar] [CrossRef] [PubMed]
- Butler, P.D.; Nelson, J.A.; Fischer, J.P.; Wink, J.D.; Chang, B.; Fosnot, J.; Wu, L.C.; Serletti, J.M. Clinical Science Racial and age disparities persist in immediate breast reconstruction: An updated analysis of 48,564 patients from the 2005 to 2011 American College of Surgeons National Surgery Quality Improvement Program data sets. Am. J. Surg. 2016, 212, 96–101. [Google Scholar] [CrossRef] [PubMed]
- Retrouvey, H.; Solaja, O.; Gagliardi, A.R.; Webster, F.; Zhong, T. Barriers of Access to Breast Reconstruction: A Systematic Review. Plast. Reconstr. Surg. 2019, 143, 465E–476E. [Google Scholar] [CrossRef] [PubMed]
- Samson, L.; Tarazi, W.; Turrini, G.; Sheingold, S. Medicare Beneficiaries’ Use of Telehealth Services in 2020—Trends by Beneficiary Characteristics and Location; Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services: Washington, DC, USA, 2021.
- Mann, D.M.; Chen, J.; Chunara, R.; Testa, P.A.; Nov, O. COVID-19 transforms health care through telemedicine: Evidence from the field. J. Am. Med. Inform. Assoc. 2020, 27, 1132–1135. [Google Scholar] [CrossRef] [PubMed]
- Contreras, C.M.; Metzger, G.A.; Beane, J.D.; Dedhia, P.H.; Ejaz, A.; Pawlik, T.M. Telemedicine: Patient-provider clinical engagement during the COVID-19 pandemic and beyond. J. Gastrointest. Surg. 2020, 24, 1692–1697. [Google Scholar] [CrossRef] [PubMed]
- Office for Civil Rights. OCR Announces Notification of Enforcement Discretion for Telehealth Remote Communications during the COVID-19 Nationwide Public Health Emergency; U.S. Department of Health and Human Services: Washington, DC, USA, 2020.
- Fischer, S.H.; Predmore, Z.; Roth, E.; Uscher-Pines, L.; Baird, M.D.; Breslau, J. Use of and Willingness to Use Video Telehealth through the COVID-19 Pandemic. Health Aff. 2022, 41, 1645–1651. [Google Scholar] [CrossRef] [PubMed]
- Albornoz, C.R.; Cohen, W.A.; Razdan, S.N.; Mehrara, B.J.; McCarthy, C.M.; Disa, J.J.; Dayan, J.H.; Pusic, A.L.; Cordeiro, P.G.; Matros, E. The impact of travel distance on breast reconstruction in the United States. Plast. Reconstr. Surg. 2016, 137, 12–18. [Google Scholar] [CrossRef] [PubMed]
- Zhong, T.; Fernandes, K.A.; Saskin, R.; Sutradhar, R.; Platt, J.; Beber, B.A.; Novak, C.B.; McCready, D.R.; Hofer, S.O.P.; Irish, J.C.; et al. Barriers to Immediate Breast Reconstruction in the Canadian Universal Health Care System. J. Clin. Oncol. 2014, 32, 2133–2141. [Google Scholar] [CrossRef] [PubMed]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef] [PubMed]
- COVIDSurg Collaborative. Elective surgery cancellations due to the COVID-19 pandemic: Global predictive modelling to inform surgical recovery plans. Br. J. Surg. 2020, 107, 1440–1449. [Google Scholar] [CrossRef]
- Illmann, C.F.; Doherty, C.; Wheelock, M.; Vorstenbosch, J.; Lipa, J.E.; Zhong, T.; Isaac, K.V. The Impact of the COVID-19 Pandemic on Breast Reconstruction: A Canadian Perspective. Plast. Surg. 2021, 29, 287–293. [Google Scholar] [CrossRef] [PubMed]
- Bovill, E.S.; Doherty, C.; Warburton, R.; Macadam, S.A.; Laeken, N.V.; Lennox, P.A.; Isaac, K.V. Management of patients requiring reconstructive breast surgery during the COVID-19 pandemic: Recommendations from the BC Regional Breast Reconstruction Network. Can. J. Surg. 2021, 64, E377–E380. [Google Scholar] [CrossRef]
- Abdullah, M.; Dias, C.; Muley, D.; Shahin, M. Exploring the impacts of COVID-19 on travel behavior and mode preferences. Transp. Res. Interdiscip. Perspect. 2020, 8, 100255. [Google Scholar] [CrossRef] [PubMed]
- Boserup, B.; McKenney, M.; Elkbuli, A. The impact of the COVID-19 pandemic on emergency department visits and patient safety in the United States. Am. J. Emerg. Med. 2020, 38, 1732–1736. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, D.; Karpman, M.; Kenney, G.M.; Zuckerman, S. Delayed and Forgone Health Care for Nonelderly Adults during the COVID-19 Pandemic Findings from the September 11–28 Coronavirus Tracking Survey; Urban Institute: Washington, DC, USA, 2021. [Google Scholar]
- van Walraven, C.; Mamdani, M.; Fang, J.; Austin, P.C. Continuity of Care and Patient Outcomes after Hospital Discharge. J. Gen. Intern. Med. 2004, 19, 624–631. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.; Kim, C. The association between continuity of care and surgery in lumbar disc herniation patients. Sci. Rep. 2021, 11, 5550. [Google Scholar] [CrossRef] [PubMed]
- Tan, J.; Mehrotra, A.; Nadkarni, G.N.; He, J.C.; Langhoff, E.; Post, J.; Galvao-Sobrinho, C.; Thode, H.C., Jr.; Rohatgi, R. Telenephrology: Providing Healthcare to Remotely Located Patients with Chronic Kidney Disease. Am. J. Nephrol. 2018, 47, 200–207. [Google Scholar] [CrossRef]
- Baughman, D.J.; Jabbarpour, Y.; Westfall, J.M.; Jetty, A.; Zain, A.; Baughman, K.; Pollak, B.; Waheed, A. Comparison of Quality Performance Measures for Patients Receiving In-Person vs Telemedicine Primary Care in a Large Integrated Health System. JAMA Netw. Open 2022, 5, e2233267. [Google Scholar] [CrossRef]
- Donelan, K.; Barreto, E.A.; Sossong, S.; Michael, C.; Estrada, J.J.; Cohen, A.B.; Wozniak, J.; Schwamm, L.H. Patient and clinician experiences with telehealth for patient follow-up care. Am. J. Manag. Care 2019, 25, 40–44. [Google Scholar]
- Hamiel, U.; Fuhrer, A.E.; Landau, N.; Reches, A.; Ponger, P.; Elhanan, E.; Tali, B.; Barel, D.; Simchoni, S.; Glassner, V.O.; et al. Telemedicine Versus Traditional In-Person Consultations: Comparison of Patient Satisfaction Rates. Telemed. J. E Health 2024, 30, 1013–1019. [Google Scholar] [CrossRef]
- Al-Rahimi, J.S.; Nass, N.M.; Hassoubah, S.A.; Wazqar, D.Y.; Alamoudi, S.A. Levels and predictors of fear and health anxiety during the current outbreak of COVID-19 in immunocompromised and chronic disease patients in Saudi Arabia: A cross-sectional correlational study. PLoS ONE 2021, 16, e0250554. [Google Scholar] [CrossRef]
- Kibbey, M.M.; Fedorenko, E.J.; Farris, S.G. Anxiety, depression, and health anxiety in undergraduate students living in initial US outbreak “hotspot” during COVID-19 pandemic. Cogn. Behav. Ther. 2021, 50, 409–421. [Google Scholar] [CrossRef]
- Aksoy, N.C.; Kabadayi, E.T.; Alan, A.K. An unintended consequence of COVID-19: Healthy nutrition. Appetite 2021, 166, 105430. [Google Scholar] [CrossRef]
- National Coalition for Cancer Survivorship Telehealth Project. Available online: https://canceradvocacy.org/wp-content/uploads/NCCS-Telehealth-Project-Executive-Summary-2114.pdf (accessed on 3 July 2024).
- Xue, E.Y.; Chu, C.K.; Winocour, S.; Cen, N.; Reece, E. Establishing a Telemedicine Program for Breast Reconstruction. Plast. Reconstr. Surg. Glob. Open 2020, 8, e2594. [Google Scholar] [CrossRef]
- One Hundred Seventeenth Congress of the United States of America. Consolidated Appropriations Act, 2023. H.R.2617. 117th Congress, 2nd Session. Enacted 3 January 2023. Available online: https://officeofbudget.od.nih.gov/pdfs/FY24/cy/BILLS-117hr2617enr.pdf (accessed on 3 July 2024).
| Pre-Telemedicine (n = 176) | Peak-Telemedicine (n = 183) | p Value | |
|---|---|---|---|
| Age mean (SD a) | 56.4 (15.3) | 54.6 (12.4) | 0.21 |
| Sex n (%) | |||
| Female | 176 (100%) | 183 (100%) | |
| Marital status n (%) | |||
| Single | 8 (4.5%) | 5 (2.7%) | 0.92 |
| Married | 50 (28.4%) | 43 (23.5%) | |
| Divorced | 2 (1.1%) | 2 (1.1%) | |
| Widowed | 4 (2.3%) | 2 (1.1%) | |
| Not specified | 112 (63.6%) | 131 (71.6%) | |
| Ethnicity n (%) | |||
| Hispanic | 8 (4.5%) | 19 (10.4%) | 0.09 |
| Non-Hispanic | 150 (85.2%) | 150 (82.0%) | |
| Not specified | 18 (10.2%) | 14 (7.7%) | |
| Race n (%) | |||
| White | 119 (67.6%) | 130 (71.0%) | 0.81 |
| American Indian | 1 (0.6%) | 0 (0%) | |
| Asian | 21 (11.9%) | 21 (11.5%) | |
| Black | 19 (10.8%) | 20 (10.9%) | |
| Not specified | 16 (9.1%) | 12 (6.6%) | |
| Language n (%) | |||
| English | 78 (44.3%) | 58 (31.7%) | 0.68 |
| Spanish | 2 (1.1%) | 4 (2.2%) | |
| Japanese | 1 (0.6%) | 0 (0%) | |
| Mandarin | 1 (0.6%) | 0 (0%) | |
| Cantonese | 4 (2.3%) | 3 (1.6%) | |
| Vietnamese | 0 (0%) | 1 (0.5%) | |
| Not specified | 90 (51.1%) | 117 (63.9%) | |
| Education n (%) | |||
| Less than college degree | 53 (30.1%) | 68 (37.2%) | 0.13 |
| College or higher | 101 (57.4%) | 102 (55.7%) | |
| Not specified | 22 (12.5%) | 13 (7.1%) |
| Pre-Telemedicine (n = 176) | Peak-Telemedicine (n = 183) | p Value | |
|---|---|---|---|
| Distance in miles mean (SD a) | 36.7 (71.3) | 45.9 (282.3) | 0.67 |
| Telemedicine 1 n (%) | |||
| Yes | 3 (1.7%) | 53 (29.0%) | <0.001 |
| No | 148 (84.1%) | 115 (62.8%) | |
| Not specified | 25 (14.2%) | 15 (8.2%) | |
| Follow-up 2 n (%) | |||
| Yes | 119 (67.6%) | 155 (84.7%) | <0.001 |
| No | 57 (32.4%) | 28 (15.3%) | |
| Days of follow-up mean (SD a) | 566.5 (427.5) | 286.8 (168.9) | <0.001 |
| Pre-Telemedicine (n = 176) | Peak-Telemedicine (n = 183) | p Value | |
|---|---|---|---|
| Mastectomy indication n (%) | |||
| Prophylactic | 14 (8.0%) | 15 (8.2%) | 0.83 |
| Unilateral breast cancer | 94 (53.4%) | 90 (49.2%) | |
| Bilateral breast cancer | 11 (6.3%) | 15 (8.2%) | |
| Unilateral cancer with prophylactic surgery of the other breast | 57 (32.4%) | 63 (34.3%) | |
| Breast reconstruction n (%) | |||
| Yes | 96 (54.5%) | 112 (61.2%) | 0.22 |
| No | 80 (45.5%) | 71 (38.8%) |
| Pre-Telemedicine (n = 96) | Peak-Telemedicine (n = 112) | p Value | |
|---|---|---|---|
| Timing n (%) | |||
| Immediate reconstruction | 15 (15.6%) | 15 (13.4%) | 0.88 |
| Delayed reconstruction | 10 (10.4%) | 13 (11.6%) | |
| Immediate TE with delayed reconstruction | 71 (74.0%) | 84 (75.0%) | |
| Completion n (%) | |||
| Yes | 78 (81.3%) | 87 (78.4%) | 0.61 |
| No | 18 (18.8%) | 24 (21.6%) | |
| Type a n (%) | |||
| Implant | 64 (82.1%) | 49 (56.3%) | <0.001 |
| Autologous | 14 (18.0%) | 38 (43.7%) | |
| DIEP | 11 (78.6%) | 33 (84.6%) | 0.40 |
| TRAM | 1 (7.1%) | 0 (0.0%) | |
| Latissimus dorsi | 2 (14.3%) | 6 (15.4%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stearns, S.A.; Lee, D.; Bustos, V.P.; Haddad, A.; Hassell, N.; Kim, E.; Foppiani, J.A.; Lee, T.C.; Lin, S.J.; Lee, B.T. Enhancing Post-Mastectomy Care: Telehealth’s Impact on Breast Reconstruction Accessibility for Breast Cancer Patients. Cancers 2024, 16, 2555. https://doi.org/10.3390/cancers16142555
Stearns SA, Lee D, Bustos VP, Haddad A, Hassell N, Kim E, Foppiani JA, Lee TC, Lin SJ, Lee BT. Enhancing Post-Mastectomy Care: Telehealth’s Impact on Breast Reconstruction Accessibility for Breast Cancer Patients. Cancers. 2024; 16(14):2555. https://doi.org/10.3390/cancers16142555
Chicago/Turabian StyleStearns, Stephen A., Daniela Lee, Valeria P. Bustos, Anthony Haddad, Natalie Hassell, Erin Kim, Jose A. Foppiani, Theodore C. Lee, Samuel J. Lin, and Bernard T. Lee. 2024. "Enhancing Post-Mastectomy Care: Telehealth’s Impact on Breast Reconstruction Accessibility for Breast Cancer Patients" Cancers 16, no. 14: 2555. https://doi.org/10.3390/cancers16142555
APA StyleStearns, S. A., Lee, D., Bustos, V. P., Haddad, A., Hassell, N., Kim, E., Foppiani, J. A., Lee, T. C., Lin, S. J., & Lee, B. T. (2024). Enhancing Post-Mastectomy Care: Telehealth’s Impact on Breast Reconstruction Accessibility for Breast Cancer Patients. Cancers, 16(14), 2555. https://doi.org/10.3390/cancers16142555






