18F-Fluorodeoxyglucose Positron Emission Tomography-Based Risk Score Model for Prediction of Five-Year Survival Outcome after Curative Resection of Non-Small-Cell Lung Cancer
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
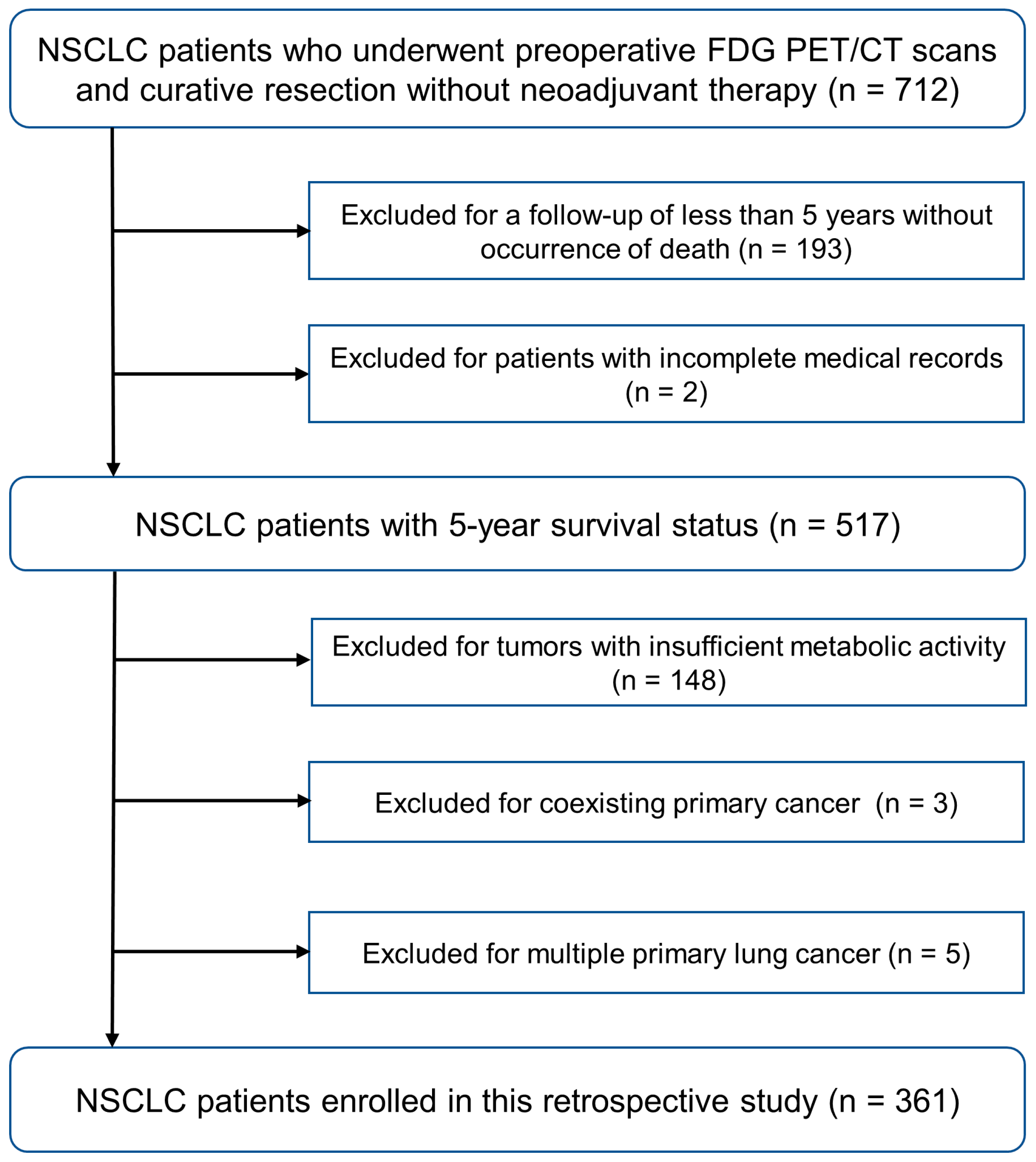
2.1. Study Population
2.2. Data Collection
2.3. FDG PET/CT Image Acquisition
2.4. FDG PET/CT Image Analysis and Feature Extraction
2.5. Feature Selection and Imaging-Based Risk Score Model Construction
2.6. Statistical Analysis
3. Results
3.1. Baseline Characteristics of Patients
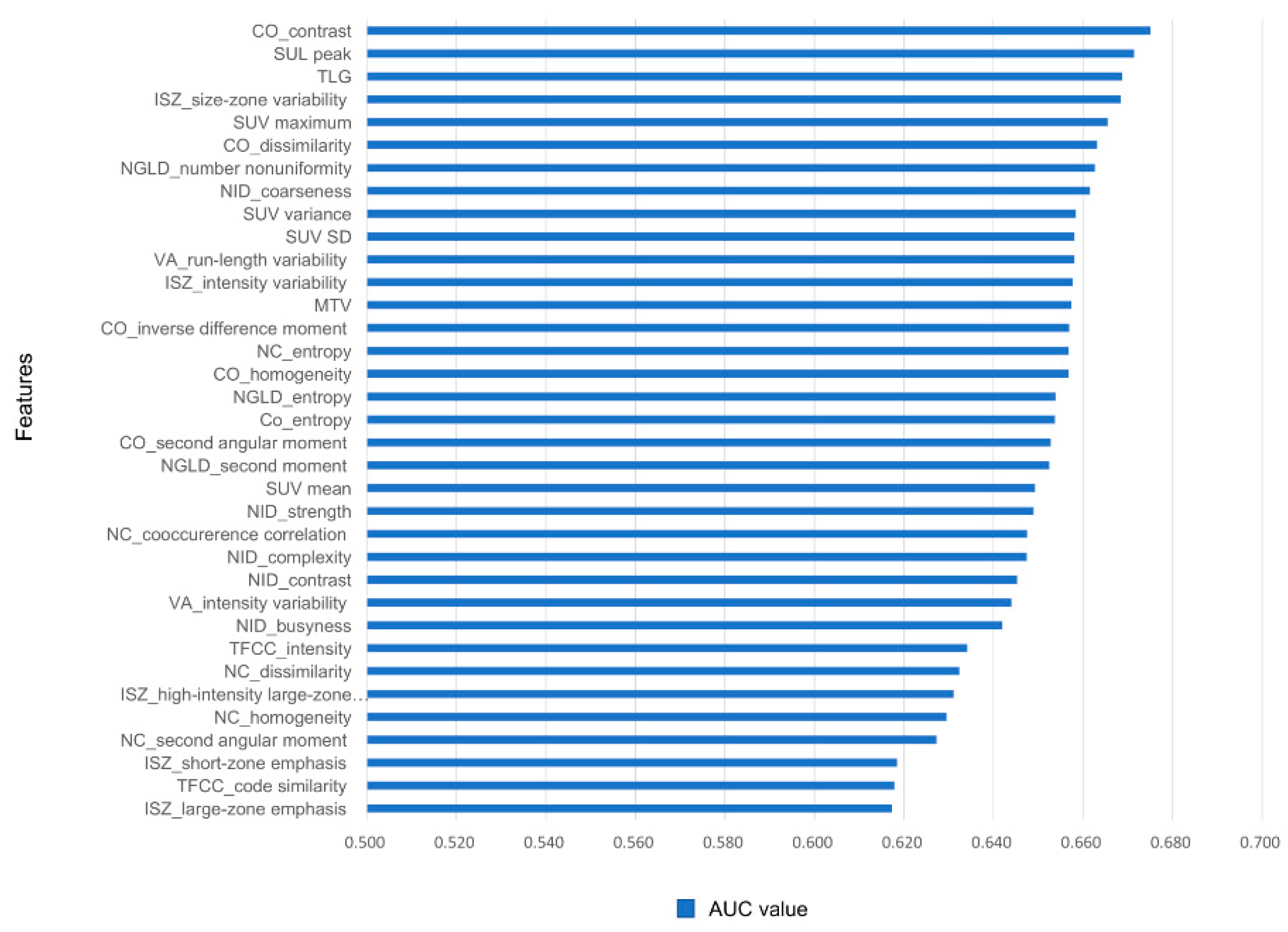
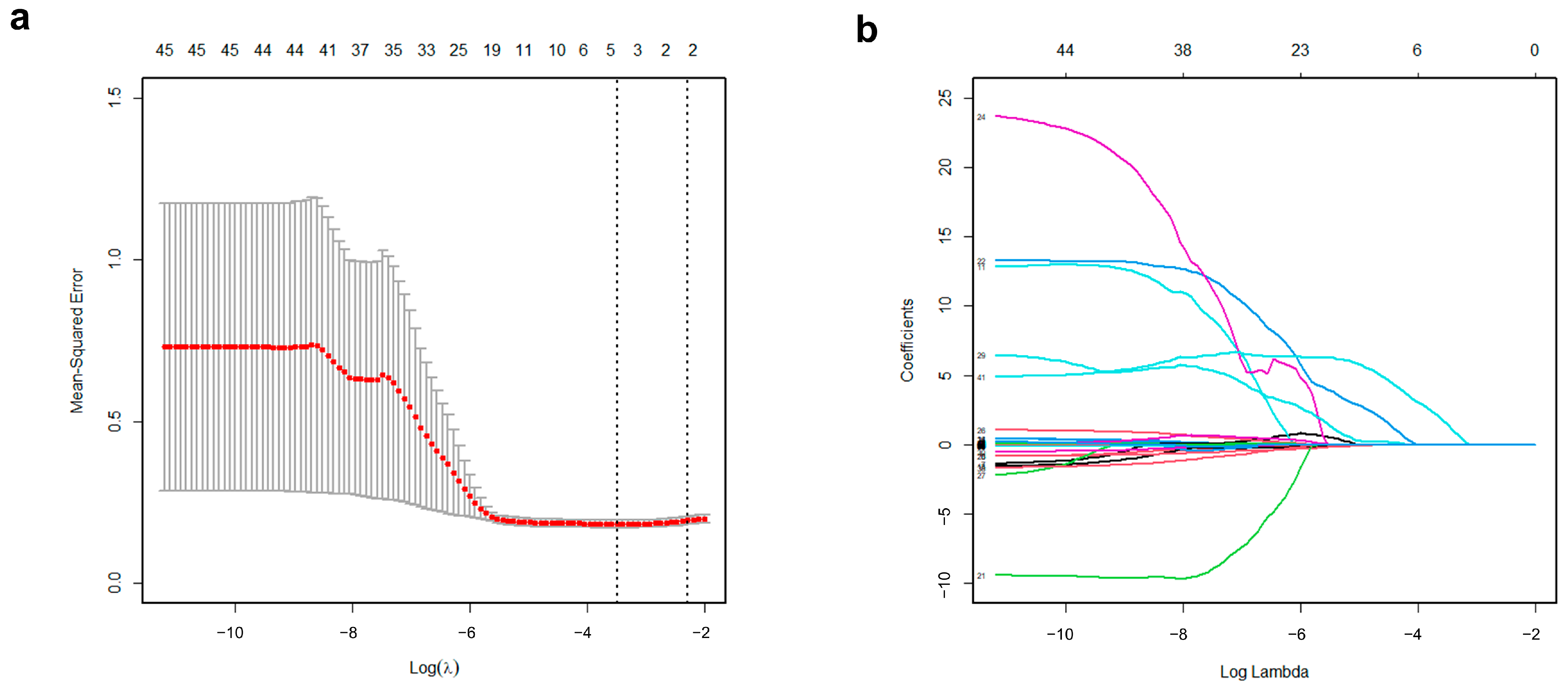
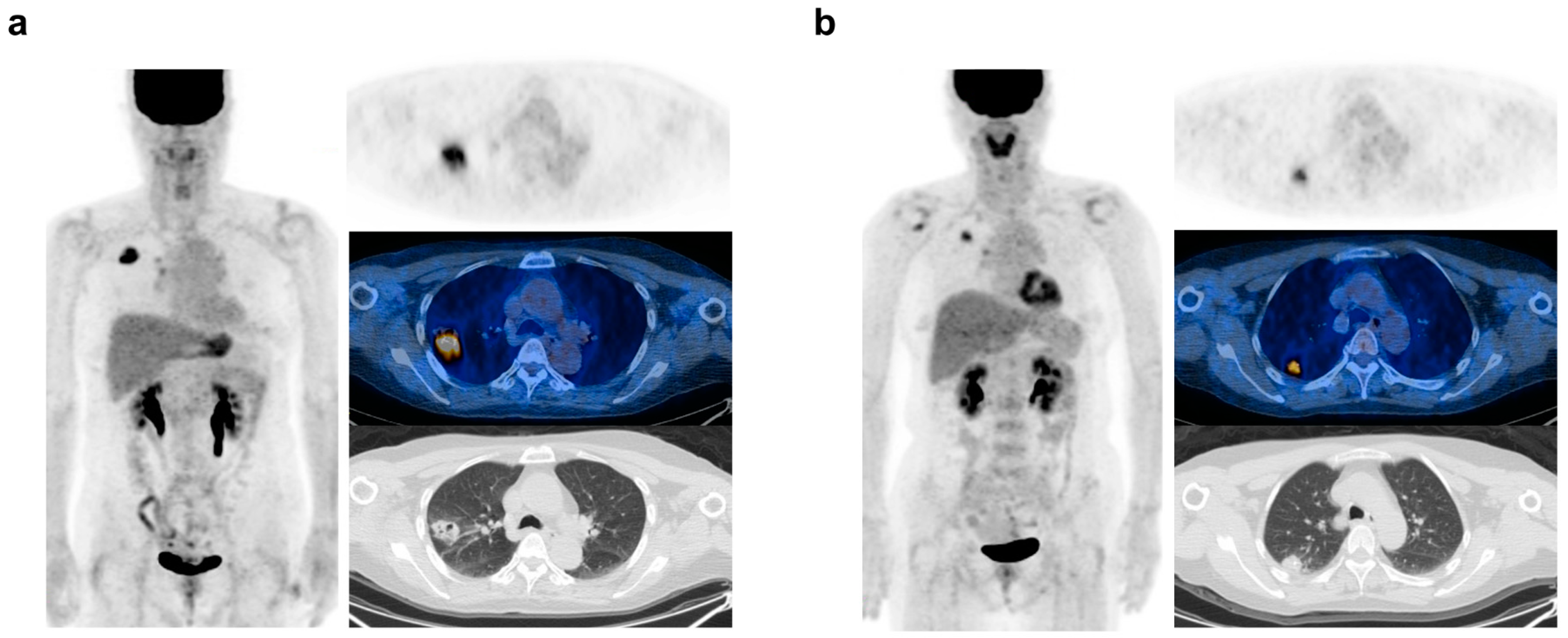
3.2. Establishment of the Imaging-Based Model
3.3. Construction of Clinical and Hybrid Model
3.4. Model Validtion
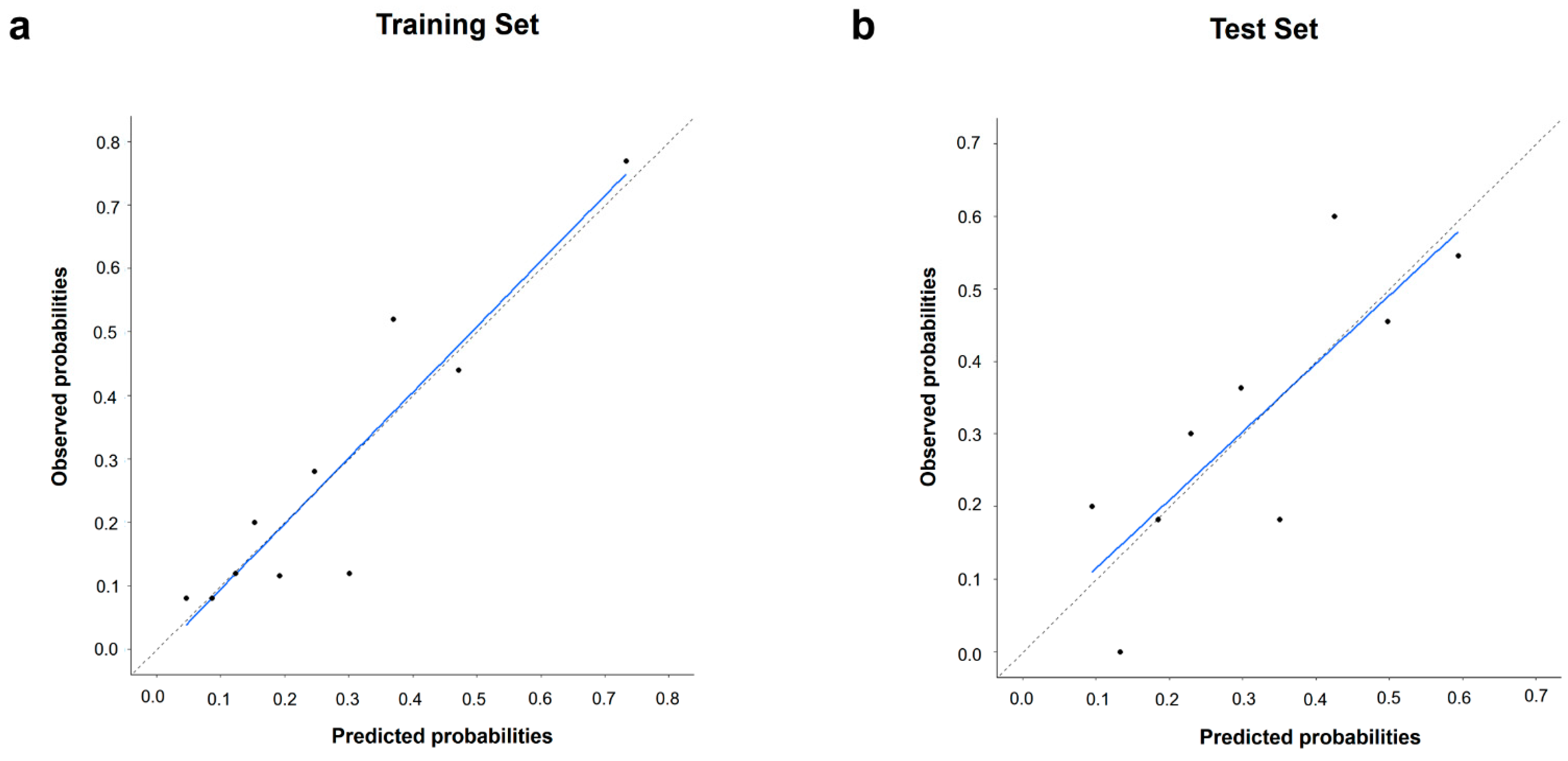
3.5. Model Performance and Calibration
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Zappa, C.; Mousa, S.A. Non-small cell lung cancer: Current treatment and future advances. Transl. Lung Cancer Res. 2016, 5, 288–300. [Google Scholar] [CrossRef] [PubMed]
- Araghi, M.; Mannani, R.; Heidarnejad maleki, A.; Hamidi, A.; Rostami, S.; Safa, S.H.; Faramarzi, F.; Khorasani, S.; Alimohammadi, M.; Tahmasebi, S. Recent advances in non-small cell lung cancer targeted therapy; an update review. Cancer Cell Int. 2023, 23, 162. [Google Scholar] [CrossRef] [PubMed]
- Flury, D.V.; Minervini, F.; Kocher, G.J. Heterogeneity of stage IIIA non-small cell lung cancer-different tumours, different nodal status, different treatment, different prognosis: A narrative review. Curr. Chall. Thorac. Surg. 2022, 4, 13. [Google Scholar] [CrossRef]
- Fares, J.; Fares, M.Y.; Khachfe, H.H.; Salhab, H.A.; Fares, Y. Molecular principles of metastasis: A hallmark of cancer revisited. Signal Transduct. Target. Ther. 2020, 5, 28. [Google Scholar] [CrossRef] [PubMed]
- Middleton, G.; Robbins, H.; Andre, F.; Swanton, C. A state-of-the-art review of stratified medicine in cancer: Towards a future precision medicine strategy in cancer. Ann. Oncol. 2022, 33, 143–157. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.; Carter, C.A.; McGlynn, K.A.; Zahm, S.H.; Nations, J.A.; Anderson, W.F.; Shriver, C.D.; Zhu, K. A prognostic model to predict mortality among non–small-cell lung cancer patients in the US military health system. J. Thorac. Oncol. 2015, 10, 1694–1702. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Oikonomou, A.; Wong, A.; Haider, M.A.; Khalvati, F. Radiomics-based prognosis analysis for non-small cell lung cancer. Sci. Rep. 2017, 7, srep46349. [Google Scholar] [CrossRef] [PubMed]
- García-Figueiras, R.; Baleato-González, S.; Padhani, A.R.; Luna-Alcalá, A.; Vallejo-Casas, J.A.; Sala, E.; Vilanova, J.C.; Koh, D.-M.; Herranz-Carnero, M.; Vargas, H.A. How clinical imaging can assess cancer biology. Insights Into Imaging 2019, 10, 28. [Google Scholar] [CrossRef] [PubMed]
- Lim, C.H.; Park, Y.-J.; Shin, M.; Cho, Y.S.; Choi, J.Y.; Lee, K.-H.; Hyun, S.H. Tumor SUVs on 18F-FDG PET/CT and aggressive pathological features in esophageal squamous cell carcinoma. Clin. Nucl. Med. 2020, 45, e128–e133. [Google Scholar] [CrossRef] [PubMed]
- Xu, C.; Li, H.; Seng, D.; Liu, F. Significance of SUV Max for Predicting Occult Lymph Node Metastasis and Prognosis in Early-Stage Tongue Squamous Cell Carcinoma. J. Oncol. 2020, 2020, 6241637. [Google Scholar] [CrossRef]
- Im, H.-J.; Pak, K.; Cheon, G.J.; Kang, K.W.; Kim, S.-J.; Kim, I.-J.; Chung, J.-K.; Kim, E.E.; Lee, D.S. Prognostic value of volumetric parameters of 18F-FDG PET in non-small-cell lung cancer: A meta-analysis. Eur. J. Nucl. Med. 2015, 42, 241–251. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Choi, Y.-L.; Kim, H.K.; Choi, Y.S.; Kim, H.; Ahn, M.-J.; Pyo, H.R.; Choi, J.Y. Prognostic Significance of Volumetric Parameters Based on FDG PET/CT in Patients with Lung Adenocarcinoma Undergoing Curative Surgery. Cancers 2023, 15, 4380. [Google Scholar] [CrossRef] [PubMed]
- Hatt, M.; Tixier, F.; Pierce, L.; Kinahan, P.E.; Le Rest, C.C.; Visvikis, D. Characterization of PET/CT images using texture analysis: The past, the present… any future? Eur. J. Nucl. Med. Mol. Imaging 2017, 44, 151–165. [Google Scholar] [CrossRef] [PubMed]
- Erol, M.; Önner, H.; Küçükosmanoğlu, İ. Association of Fluorodeoxyglucose Positron Emission Tomography Radiomics Features with Clinicopathological Factors and Prognosis in Lung Squamous Cell Cancer. Nucl. Med. Mol. Imaging 2022, 56, 306–312. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Zhang, B.; Ge, S.; Deng, S.; Hu, C.; Sang, S. Prognostic value of 18F-FDG PET/CT radiomic model based on primary tumor in patients with non-small cell lung cancer: A large single-center cohort study. Front. Oncol. 2022, 12, 1047905. [Google Scholar] [CrossRef]
- Yang, B.; Zhong, J.; Zhong, J.; Ma, L.; Li, A.; Ji, H.; Zhou, C.; Duan, S.; Wang, Q.; Zhu, C. Development and validation of a radiomics nomogram based on 18F-fluorodeoxyglucose positron emission tomography/computed tomography and clinicopathological factors to predict the survival outcomes of patients with non-small cell lung cancer. Front. Oncol. 2020, 10, 1042. [Google Scholar] [CrossRef] [PubMed]
- Zeng, Z.; Gao, Y.; Li, J.; Zhang, G.; Sun, S.; Wu, Q.; Gong, Y.; Xie, C. Violations of proportional hazard assumption in Cox regression model of transcriptomic data in TCGA pan-cancer cohorts. Comput. Struct. Biotechnol. J. 2022, 20, 496–507. [Google Scholar] [CrossRef] [PubMed]
- Suresh, K.; Severn, C.; Ghosh, D. Survival prediction models: An introduction to discrete-time modeling. BMC Med Res. Methodol. 2022, 22, 207. [Google Scholar] [CrossRef] [PubMed]
- Werner-Wasik, M.; Nelson, A.D.; Choi, W.; Arai, Y.; Faulhaber, P.F.; Kang, P.; Almeida, F.D.; Xiao, Y.; Ohri, N.; Brockway, K.D.; et al. What Is the Best Way to Contour Lung Tumors on PET Scans? Multiobserver Validation of a Gradient-Based Method Using a NSCLC Digital PET Phantom. Int. J. Radiat. Oncol. 2012, 82, 1164–1171. [Google Scholar] [CrossRef]
- Fang, Y.-H.D.; Lin, C.-Y.; Shih, M.-J.; Wang, H.-M.; Ho, T.-Y.; Liao, C.-T.; Yen, T.-C. Development and Evaluation of an Open-Source Software Package “CGITA” for Quantifying Tumor Heterogeneity with Molecular Images. BioMed Res. Int. 2014, 2014, 248505. [Google Scholar] [CrossRef] [PubMed]
- Ha, S.; Park, S.; Bang, J.-I.; Kim, E.-K.; Lee, H.-Y. Metabolic Radiomics for Pretreatment 18F-FDG PET/CT to Characterize Locally Advanced Breast Cancer: Histopathologic Characteristics, Response to Neoadjuvant Chemotherapy, and Prognosis. Sci. Rep. 2017, 7, 1556. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Berdine, G. The receiver operating characteristic (ROC) curve. Southwest. Respir. Crit. Care Chron. 2017, 5, 34–36. [Google Scholar] [CrossRef]
- Emmert-Streib, F.; Dehmer, M. High-dimensional LASSO-based computational regression models: Regularization, shrinkage, and selection. Mach. Learn. Knowl. Extr. 2019, 1, 359–383. [Google Scholar] [CrossRef]
- DeLong, E.R.; DeLong, D.M.; Clarke-Pearson, D.L. Comparing the areas under two or more correlated receiver operating characteristic curves: A nonparametric approach. Biometrics 1988, 837–845. [Google Scholar] [CrossRef]
- Hosmer, D.W.; Hosmer, T.; Le Cessie, S.; Lemeshow, S. A comparison of goodness-of-fit tests for the logistic regression model. Stat. Med. 1997, 16, 965–980. [Google Scholar] [CrossRef]
- Zou, J.; Wang, E. Cancer biomarker discovery for precision medicine: New progress. Curr. Med. Chem. 2019, 26, 7655–7671. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; DeBerardinis, R.J. Mechanisms and implications of metabolic heterogeneity in cancer. Cell Metab. 2019, 30, 434–446. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.W.; Kim, S.Y.; Han, S.W.; Lee, J.E.; Hong, S.H.; Lee, S.M.; Jo, I.Y. Clinical significance of peritumoral adipose tissue PET/CT imaging features for predicting axillary lymph node metastasis in patients with breast cancer. J. Pers. Med. 2021, 11, 1029. [Google Scholar] [CrossRef] [PubMed]
- Haralick, R.M.; Shanmugam, K.; Dinstein, I.H. Textural features for image classification. IEEE Trans. Syst. Man Cybern. 1973, 6, 610–621. [Google Scholar] [CrossRef]
- Han, S.; Woo, S.; Suh, C.H.; Kim, Y.J.; Oh, J.S.; Lee, J.J. A systematic review of the prognostic value of texture analysis in 18 F-FDG PET in lung cancer. Ann. Nucl. Med. 2018, 32, 602–610. [Google Scholar] [CrossRef] [PubMed]
- Park, J.E.; Park, S.Y.; Kim, H.J.; Kim, H.S. Reproducibility and Generalizability in Radiomics Modeling: Possible Strategies in Radiologic and Statistical Perspectives. Korean J. Radiol. 2019, 20, 1124–1137. [Google Scholar] [CrossRef] [PubMed]
- Jeon, D.S.; Kim, H.C.; Kim, S.H.; Kim, T.-J.; Kim, H.K.; Moon, M.H.; Beck, K.S.; Suh, Y.-G.; Song, C.; Ahn, J.S.; et al. Five-Year Overall Survival and Prognostic Factors in Patients with Lung Cancer: Results from the Korean Association of Lung Cancer Registry (KALC-R) 2015. Cancer Res. Treat. 2023, 55, 103–111. [Google Scholar] [CrossRef] [PubMed]
- Ahn, H.; Lee, H.; Kim, S.; Hyun, S. Pre-treatment 18F-FDG PET-based radiomics predict survival in resected non-small cell lung cancer. Clin. Radiol. 2019, 74, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Park, S.B.; Kim, K.-U.; Park, Y.W.; Hwang, J.H.; Lim, C.H. Application of 18F-fluorodeoxyglucose PET/CT radiomic features and machine learning to predict early recurrence of non-small cell lung cancer after curative-intent therapy. Nucl. Med. Commun. 2023, 44, 161–168. [Google Scholar] [CrossRef] [PubMed]
- Im, H.-J.; Bradshaw, T.; Solaiyappan, M.; Cho, S.Y. Current methods to define metabolic tumor volume in positron emission tomography: Which one is better? Nucl. Med. Mol. Imaging 2018, 52, 5–15. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Kang, S.K.; Hwang, D.; Choi, H.; Ha, S.; Seo, J.M.; Eo, J.S.; Lee, J.S. Automatic Lung Cancer Segmentation in [18F]FDG PET/CT Using a Two-Stage Deep Learning Approach. Nucl. Med. Mol. Imaging 2023, 57, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Guezennec, C.; Bourhis, D.; Orlhac, F.; Robin, P.; Corre, J.-B.; Delcroix, O.; Gobel, Y.; Schick, U.; Salaün, P.-Y.; Abgral, R. Inter-observer and segmentation method variability of textural analysis in pre-therapeutic FDG PET/CT in head and neck cancer. PLoS ONE 2019, 14, e0214299. [Google Scholar] [CrossRef] [PubMed]
- Garrido, P.; Conde, E.; de Castro, J.; Gómez-Román, J.J.; Felip, E.; Pijuan, L.; Isla, D.; Sanz, J.; Paz-Ares, L.; López-Ríos, F. Updated guidelines for predictive biomarker testing in advanced non-small-cell lung cancer: A National Consensus of the Spanish Society of Pathology and the Spanish Society of Medical Oncology. Clin. Transl. Oncol. 2020, 22, 989–1003. [Google Scholar] [CrossRef] [PubMed]

| Variable | Total (n = 361) | Training Set (n = 253) | Test Set (n = 108) | p Value |
|---|---|---|---|---|
| Age, years (mean ± SD) | 63.1 ± 10.2 | 62.8 ± 10.2 | 63.8 ± 10.2 | 0.382 |
| Sex, male (%) | 237 (65.7) | 161 (63.6) | 76 (70.3) | 0.218 |
| Tumor size, cm (mean ± SD) | 3.6 ± 1.9 | 3.7 ± 2.0 | 3.5 ± 1.6 | 0.327 |
| Histology | 0.762 | |||
| Adenocarcinoma (%) | 232 (64.3) | 165 (65.2) | 67 (62.0) | |
| Squamous cell carcinoma (%) | 104 (28.8) | 70 (27.7) | 34 (31.5) | |
| Others (%) | 25 (6.9) | 18 (7.1) | 7 (6.5) | |
| Tumor stage | 0.526 | |||
| I (%) | 140 (38.8) | 95 (37.6) | 45 (41.7) | |
| II (%) | 105 (29.1) | 78 (30.8) | 27 (25.0) | |
| III (%) | 116 (32.1) | 80 (31.6) | 36 (33.3) | |
| Type of surgery | 0.438 | |||
| Pneumonectomy (%) | 12 (3.3) | 6 (2.4) | 6 (5.6) | |
| Bilobectomy (%) | 17 (4.7) | 11 (4.4) | 6 (5.6) | |
| Lobectomy (%) | 307 (85.1) | 218 (86.1) | 89 (82.4) | |
| Segmentectomy (%) | 25 (6.9) | 18 (7.1) | 7 (6.4) | |
| Adjuvant therapy | 0.466 | |||
| None (%) | 204 (56.5) | 138 (54.5) | 66 (61.1) | |
| Chemotherapy (%) | 128 (35.5) | 94 (37.2) | 34 (31.5) | |
| Radiotherapy (%) | 3 (0.8) | 3 (1.2) | 0 (0.0) | |
| Chemoradiotherapy (%) | 26 (7.2) | 18 (7.1) | 8 (7.4) | |
| Death within five years (%) | 108 (29.9) | 69 (27.3) | 39 (36.1) | 0.094 |
| Variable | Non-Survivor (n = 108) | Survivor (n = 253) | p Value |
|---|---|---|---|
| Age, years (mean ± SD) | 67.6 ± 9.3 | 61.2 ± 10.0 | <0.001 |
| Sex, male (%) | 83 (76.9) | 154 (60.9) | 0.004 |
| Tumor size, cm (mean ± SD) | 4.5 ± 2.4 | 3.3 ± 1.5 | <0.001 |
| Histology, ADC (%) | 56 (51.9) | 176 (69.6) | 0.001 |
| Tumor stage, II/III (%) | 80 (74.1) | 141 (55.7) | 0.001 |
| Adjuvant therapy, presence (%) | 45 (41.7) | 112 (44.3) | 0.648 |
| Variables | Clinical Model | Hybrid Model | ||||
|---|---|---|---|---|---|---|
| Adjusted OR | 95% CI | p Value | Adjusted OR | 95% CI | p Value | |
| Age, years | 1.080 | 1.041–1.120 | <0.001 | 1.083 | 1.043–1.125 | <0.001 |
| Sex (M vs. F) | 1.337 | 0.644–2.772 | 0.436 | 1.038 | 0.486–2.217 | 0.924 |
| Tumor stage (III/II vs. I) | 1.567 | 0.733–3.351 | 0.247 | 1.301 | 0.595–2.845 | 0.510 |
| Histology (ADC vs. others) | 0.667 | 0.334–1.335 | 0.253 | 0.881 | 0.421–1.845 | 0.737 |
| Tumor size, cm | 1.214 | 1.018–1.448 | 0.031 | 1.046 | 0.848–1.291 | 0.673 |
| PET-based risk score | 5.231 | 1.987–6.932 | 0.009 | |||
| Variables | Clinical Model | Hybrid Model | ||||
|---|---|---|---|---|---|---|
| Adjusted OR | 95% CI | p Value | Adjusted OR | 95% CI | p Value | |
| Age, years | 1.051 | 1.003–1.100 | 0.036 | 1.060 | 1.010–1.113 | 0.019 |
| Sex (M vs. F) | 1.538 | 0.548–4.316 | 0.414 | 1.450 | 0.500–4.201 | 0.494 |
| Tumor stage (III/II vs. I) | 1.392 | 0.480–4.041 | 0.543 | 1.386 | 0.462–4.156 | 0.560 |
| Histology (ADC vs. others) | 1.323 | 0.506–3.456 | 0.568 | 1.695 | 0.614–4.680 | 0.309 |
| Tumor size, cm | 1.475 | 1.046–2.080 | 0.027 | 1.008 | 0.619–1.642 | 0.976 |
| PET based-risk score | 1311.521 | 1.901–904,972.132 | 0.031 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lim, C.H.; Um, S.-W.; Kim, H.K.; Choi, Y.S.; Pyo, H.R.; Ahn, M.-J.; Choi, J.Y. 18F-Fluorodeoxyglucose Positron Emission Tomography-Based Risk Score Model for Prediction of Five-Year Survival Outcome after Curative Resection of Non-Small-Cell Lung Cancer. Cancers 2024, 16, 2525. https://doi.org/10.3390/cancers16142525
Lim CH, Um S-W, Kim HK, Choi YS, Pyo HR, Ahn M-J, Choi JY. 18F-Fluorodeoxyglucose Positron Emission Tomography-Based Risk Score Model for Prediction of Five-Year Survival Outcome after Curative Resection of Non-Small-Cell Lung Cancer. Cancers. 2024; 16(14):2525. https://doi.org/10.3390/cancers16142525
Chicago/Turabian StyleLim, Chae Hong, Sang-Won Um, Hong Kwan Kim, Yong Soo Choi, Hong Ryul Pyo, Myung-Ju Ahn, and Joon Young Choi. 2024. "18F-Fluorodeoxyglucose Positron Emission Tomography-Based Risk Score Model for Prediction of Five-Year Survival Outcome after Curative Resection of Non-Small-Cell Lung Cancer" Cancers 16, no. 14: 2525. https://doi.org/10.3390/cancers16142525
APA StyleLim, C. H., Um, S.-W., Kim, H. K., Choi, Y. S., Pyo, H. R., Ahn, M.-J., & Choi, J. Y. (2024). 18F-Fluorodeoxyglucose Positron Emission Tomography-Based Risk Score Model for Prediction of Five-Year Survival Outcome after Curative Resection of Non-Small-Cell Lung Cancer. Cancers, 16(14), 2525. https://doi.org/10.3390/cancers16142525






