Efficacy and Safety of Liver Chemoembolization Procedures, Combined with FOLFIRI Chemotherapy, in First-Line Treatment of Metastatic Colorectal Cancer in Patients with Oncogene Mutations
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Chemoembolization Procedure
2.2. Imaging and Tumor Response
2.3. Statistical Analyses
3. Results
3.1. Baseline Characteristics
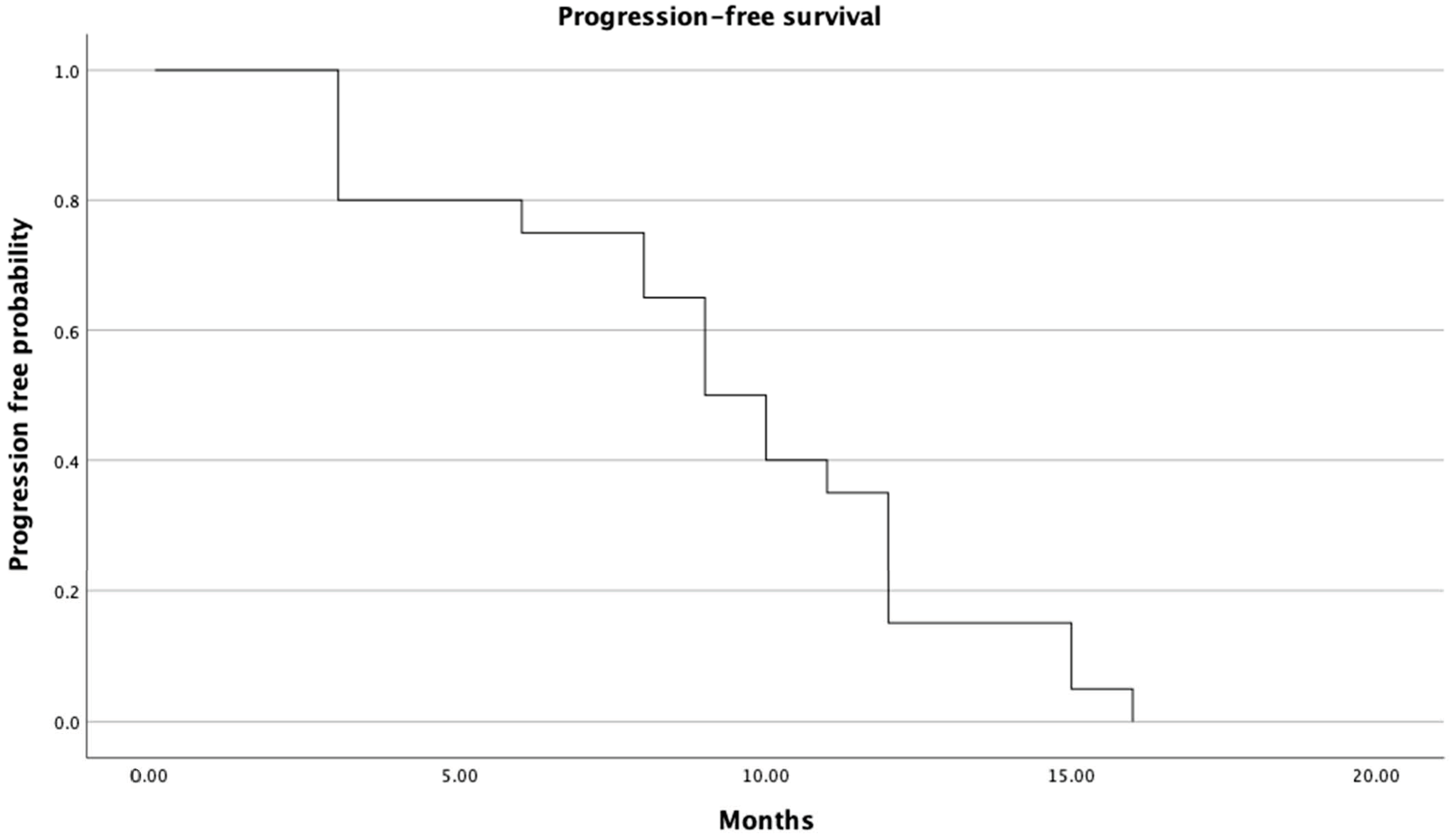
3.2. Response, Progression-Free Survival and Overall Survival
3.3. Adverse Events
4. Discussion
5. Conclusions
6. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vogl, T.J.; Lahrsow, M. The Role of Conventional TACE (cTACE) and DEBIRI-TACE in Colorectal Cancer Liver Metastases. Cancers 2022, 14, 1503. [Google Scholar] [CrossRef]
- Sánchez-Gundín, J.; Fernández-Carballido, A.M.; Martínez-Valdivieso, L.; Barreda-Hernández, D.; Torres-Suárez, A.I. New Trends in the Therapeutic Approach to Metastatic Colorectal Cancer. Int. J. Med. Sci. 2018, 15, 659–665. [Google Scholar] [CrossRef]
- Zhu, G.; Pei, L.; Xia, H.; Tang, Q.; Bi, F. Role of oncogenic KRAS in the prognosis, diagnosis and treatment of colorectal cancer. Mol. Cancer 2021, 20, 143. [Google Scholar] [CrossRef]
- Van Cutsem, E.; Lang, I.; Folprecht, G.; Nowacki, M.; Barone, C.; Maurel, I.S.; Cunningham, D.; Celik, I.; Kohne, C. Cetuximab plus FOLFIRI: Final data from the CRYSTAL study on the association of KRAS and BRAF biomarker status with treatment outcome. J. Clin. Oncol. 2010, 28, 3570. [Google Scholar] [CrossRef]
- Bylsma, L.C.; Gillezeau, C.; Garawin, T.A.; Kelsh, M.A.; Fryzek, J.P.; Sangaré, L.; Lowe, K.A. Prevalence of RAS and BRAF mutations in metastatic colorectal cancer patients by tumor sidedness: A systematic review and meta-analysis. Cancer Med. 2020, 9, 1044–1057. [Google Scholar] [CrossRef]
- Garcia-Carbonero, N.; Martinez-Useros, J.; Li, W.; Orta, A.; Perez, N.; Carames, C.; Hernandez, T.; Moreno, I.; Serrano, G.; Garcia-Foncillas, J. KRAS and BRAF Mutations as Prognostic and Predictive Biomarkers for Standard Chemotherapy Response in Metastatic Colorectal Cancer: A Single Institutional Study. Cells 2020, 9, 219. [Google Scholar] [CrossRef]
- Fiorentini, G.; Sarti, D.; Nani, R.; Aliberti, C.; Fiorentini, C.; Guadagni, S. Updates of colorectal cancer liver metastases therapy: Review on DEBIRI. Hepatic Oncol. 2020, 7, HEP16. [Google Scholar] [CrossRef]
- Huppert, P.; Wenzel, T.; Wietholtz, H. Transcatheter arterial chemoembolization (TACE) of colorectal cancer liver metastases by irinotecan-eluting microspheres in a salvage patient population. Cardiovasc. Interv. Radiol. 2014, 37, 154–164. [Google Scholar] [CrossRef]
- Cervantes, A.; Adam, R.; Roselló, S.; Arnold, D.; Normanno, N.; Taïeb, J.; Seligmann, J.; De Baere, T.; Osterlund, P.; Yoshino, T. Metastatic colorectal cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up. Ann. Oncol. 2022, 34, 10–32. [Google Scholar] [CrossRef] [PubMed]
- Heinemann, V.; von Weikersthal, L.F.; Decker, T.; Kiani, A.; Kaiser, F.; Al-Batran, S.E.; Heintges, T.; Lerchenmüller, C.; Kahl, C.; Seipelt, G.; et al. FOLFIRI plus cetuximab or bevacizumab for advanced colorectal cancer: Final survival and per-protocol analysis of FIRE-3, a randomised clinical trial. Br. J. Cancer. 2021, 124, 587–594. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.-H.; Chen, Y.-X.; Fang, J.-Y. Comprehensive review of targeted therapy for colorectal cancer. Signal Transduct. Target. Ther. 2020, 5, 22. [Google Scholar] [CrossRef] [PubMed]
- Fernández Montes, A.; Alonso Orduña, V.; Asensio Martínez, E.; Rodríguez Salas, N.; Torres, E.; Cacho Lavín, D.; Rodríguez Alonso, R.M.; Falcó, E.; Oliva, J.C.; Cirera, L.; et al. The Frequency of Specific KRAS Mutations, and Their Impact on Treatment Choice and Survival, in Patients With Metastatic Colorectal Cancer. Oncologist 2023, 28, e902–e909. [Google Scholar] [CrossRef] [PubMed]
- Chu, J.E.; Johnson, B.; Kugathasan, L.; Morris, V.K.; Raghav, K.; Swanson, L.; Lim, H.J.; Renouf, D.J.; Gill, S.; Wolber, R.; et al. Population-based screening for BRAF (V600E) in metastatic colorectal cancer reveals increased prevalence and poor prognosis. Clin. Cancer Res. 2020, 26, 4599–4605. [Google Scholar] [CrossRef]
- Ohishi, T.; Kaneko, M.K.; Yoshida, Y.; Takashima, A.; Kato, Y.; Kawada, M. Current Targeted Therapy for Metastatic Colorectal Cancer. Int. J. Mol. Sci. 2023, 24, 1702. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Jiang, C.; Yang, L.; Huang, J.; Peng, R.; Wang, X.; He, W.; Bai, L.; Zhou, Y.; Zhang, B.; et al. First-line cetuximab improves the efficacy of subsequent bevacizumab for RAS wild-type left-sided metastatic colorectal cancer: An observational retrospective study. Sci. Rep. 2020, 10, 12336. [Google Scholar] [CrossRef] [PubMed]
- Ciardiello, F.; Ciardiello, D.; Martini, G.; Napolitano, S.; Tabernero, J.; Cervantes, A. Clinical management of metastatic colorectal cancer in the era of precision medicine. CA A Cancer J. Clin. 2022, 72, 372–401. [Google Scholar] [CrossRef] [PubMed]
- Totzeck, M.; Mincu, R.I.; Rassaf, T. Cardiovascular Adverse Events in Patients With Cancer Treated With Bevacizumab: A Meta-Analysis of More Than 20,000 Patients. J. Am. Heart Assoc. 2017, 6, e006278. [Google Scholar] [CrossRef] [PubMed]
- Scappaticci, F.A.; Skillings, J.R.; Holden, S.N.; Gerber, H.P.; Miller, K.; Kabbinavar, F.; Bergsland, E.; Ngai, J.; Holmgren, E.; Wang, J.; et al. Arterial thromboembolic events in patients with metastatic carcinoma treated with chemotherapy and bevacizumab. J. Natl. Cancer Inst. 2007, 99, 1232–1239. [Google Scholar] [CrossRef]
- Van Cutsem, E.; Lenz, H.-J.; Köhne, C.-H.; Heinemann, V.; Tejpar, S.; Melezínek, I.; Beier, F.; Stroh, C.; Rougier, P.; van Krieken, J.H.; et al. Fluorouracil, leucovorin, and irinotecan plus cetuximab treatment and RAS mutations in colorectal cancer. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2015, 33, 692–700. [Google Scholar] [CrossRef]
- Stintzing, S.; von Weikersthal, L.F.; Decker, T.; Vehling-Kaiser, U.; Jäger, E.; Heintges, T.; Stoll, C.; Giessen, C.; Modest, D.P.; Neumann, J.; et al. FOLFIRI plus cetuximab versus FOLFIRI plus bevacizumab as first-line treatment for patients with metastatic colorectal cancer-subgroup analysis of patients with KRAS: Mutated tumours in the randomised German AIO study KRK-0306. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2012, 23, 1693–1699. [Google Scholar] [CrossRef]
- Brooks, A.J.; Hammond, J.S.; Girling, K.; Beckingham, I.J. The effect of hepatic vascular inflow occlusion on liver tissue pH, carbon dioxide, and oxygen partial pressures: Defining the optimal clamp/release regime for intermittent portal clamping. J. Surg. Res. 2007, 141, 247–251. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, T.; Nishiofuku, H.; Hukuoka, Y.; Sato, T.; Masada, T.; Takano, M.; Gilbert, C.W.; Obayashi, C.; Kichikawa, K. Pharmacokinetics and antitumorefficacy of chemoembolization using 40 μm irinotecan-loaded microspheresin a rabbit liver tumor model. J. Vasc. Interv. Radiol. 2014, 25, 1037–1044. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Yang, J.; Zhan, H.; Yang, B.; Rong, P.; Luo, Y.; Shi, C.; Chen, Y.; Yang, J. Incidence and non-genetic risk factors of irinotecan-induced severe neutropenia in Chinese adult inpatients. Medicine 2023, 102, e33005. [Google Scholar] [CrossRef] [PubMed]
- Bhutiani, N.; Akinwande, O.; Martin, R.C., 2nd. Efficacy and Toxicity of Hepatic Intra-Arterial Drug-Eluting (Irinotecan) Bead (DEBIRI) Therapy in Irinotecan-Refractory Unresectable Colorectal Liver Metastases. World J. Surg. 2016, 40, 1178–1190. [Google Scholar] [CrossRef] [PubMed]
- Pernot, S.; Pellerin, O.; Artru, P.; Montérymard, C.; Smith, D.; Raoul, J.-L.; De La Fouchardière, C.; Dahan, L.; Guimbaud, R.; Sefrioui, D.; et al. Intra-arterial hepatic beads loaded with irinotecan (DEBIRI) with mFOLFOX6 in unresectable liver metastases from colorectal cancer: A Phase 2 study. Br. J. Cancer 2020, 123, 518–524. [Google Scholar] [CrossRef] [PubMed]
- Kuboki, Y.; Mizunuma, N.; Ozaka, M.; Ogura, M.; Suenaga, M.; Shinozaki, E.; Matsusaka, S.; Chin, K.; Matsuura, M.; Hatake, K. Grade 3/4 neutropenia is a limiting factor in second-line FOLFIRI following FOLFOX4 failure in elderly patients with metastatic colorectal cancer. Oncol. Lett. 2011, 2, 493–498. [Google Scholar] [CrossRef]
- López, R.; Salgado, M.; Reboredo, M.; Grande, C.; Méndez, J.C.; Jorge, M.; Romero, C.; Quintero, G.; de la Cámara, J.; Candamio, S. A retrospective observational study on the safety and efficacy of first-line treatment with bevacizumab combined with FOLFIRI in metastatic colorectal cancer. Br. J. Cancer 2010, 103, 1536–1541. [Google Scholar] [CrossRef]
- Tanaka, T.; Sato, T.; Nishiofuku, H.; Masada, T.; Tatsumoto, S.; Marugami, N.; Otsuji, T.; Kanno, M.; Koyama, F.; Sho, M.; et al. Selective TACE with irinotecan-loaded 40 μm microspheres and FOLFIRI for colorectal liver metastases: Phase I dose escalation pharmacokinetic study. BMC Cancer. 2019, 19, 758. [Google Scholar] [CrossRef]


| Parameter | Value (N = 20) |
|---|---|
| Age, median (range) | 66.2 (37–81) |
| Sex (n (%)) | |
| Female | 12 (60%) |
| Male | 8 (40%) |
| ECOG status (n (%)) | |
| 0 | 9 (45%) |
| 1 | 11 (55%) |
| Tumor distribution (n (%)) | |
| Bilobar | 18 (90%) |
| Unilobar | 2 (10%) |
| Number of liver metastases per patient, median (range) | 6.6 (2–9) |
| Largest nodule size diameter per patient, median (cm) | 6.3 |
| Extent of liver involvement (n, <25%/>25%) | 14/6 |
| Site of primary tumor (n) | |
| Left colon | 8 |
| Right colon | 12 |
| Molecular status (n) | |
| KRAS gene mutated | 18 |
| BRAF gene mutated | 1 |
| NRAS gene mutated | 1 |
| Carcinoembryonic antigen level (n) | |
| ≤15 ng/mL | 14 |
| >15 ng/mL | 6 |
| Adverse Event | Number of Patients | ||
|---|---|---|---|
| Grade 1 | Grade 2 | Grade 3 | |
| Abdominal Pain | 4 | 7 | 4 |
| Nausea | 8 | 7 | |
| Vomiting | 5 | 5 | |
| Fever | 4 | 3 | 1 |
| Diarrhea | 1 | 1 | |
| Neutropenia | 1 | 8 | 3 |
| Lymphopenia | 5 | 4 | 1 |
| Thrombocytopenia | 8 | 6 | 2 |
| Anemia | 10 | 10 | |
| Cholecystitis | 1 | ||
| Elevated AST | 5 | 1 | |
| Elevated ALT | 2 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szemitko, M.; Falkowski, A.; Modrzejewska, M.; Golubinska-Szemitko, E. Efficacy and Safety of Liver Chemoembolization Procedures, Combined with FOLFIRI Chemotherapy, in First-Line Treatment of Metastatic Colorectal Cancer in Patients with Oncogene Mutations. Cancers 2024, 16, 71. https://doi.org/10.3390/cancers16010071
Szemitko M, Falkowski A, Modrzejewska M, Golubinska-Szemitko E. Efficacy and Safety of Liver Chemoembolization Procedures, Combined with FOLFIRI Chemotherapy, in First-Line Treatment of Metastatic Colorectal Cancer in Patients with Oncogene Mutations. Cancers. 2024; 16(1):71. https://doi.org/10.3390/cancers16010071
Chicago/Turabian StyleSzemitko, Marcin, Aleksander Falkowski, Monika Modrzejewska, and Elzbieta Golubinska-Szemitko. 2024. "Efficacy and Safety of Liver Chemoembolization Procedures, Combined with FOLFIRI Chemotherapy, in First-Line Treatment of Metastatic Colorectal Cancer in Patients with Oncogene Mutations" Cancers 16, no. 1: 71. https://doi.org/10.3390/cancers16010071
APA StyleSzemitko, M., Falkowski, A., Modrzejewska, M., & Golubinska-Szemitko, E. (2024). Efficacy and Safety of Liver Chemoembolization Procedures, Combined with FOLFIRI Chemotherapy, in First-Line Treatment of Metastatic Colorectal Cancer in Patients with Oncogene Mutations. Cancers, 16(1), 71. https://doi.org/10.3390/cancers16010071






