Dose Escalation of Oropharyngeal Cancer: Long-Time Follow-Up and Side Effects
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Treatment
2.2.1. Standard Dose Radiotherapy
2.2.2. Dose-Escalated Radiotherapy
2.2.3. Medical Treatment
2.3. Toxicity Outcomes
2.4. Statistics
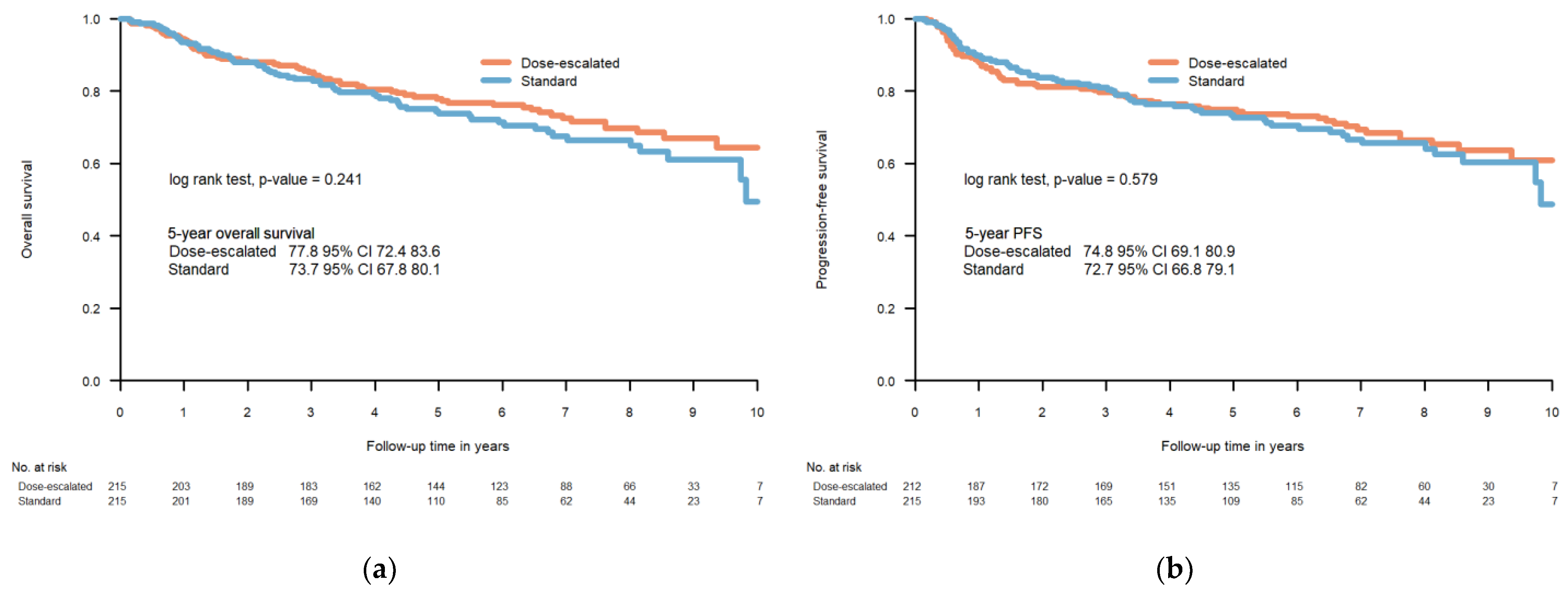
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Australia, C. Head and Neck Cancer in Australia Statistics. 2022. Available online: https://www.canceraustralia.gov.au/cancer-types/head-and-neck-cancer/statistics (accessed on 1 February 2023).
- Centres Corc. The Swedish Head and Neck Cancer Register. 2020. Available online: https://cancercentrum.se/globalassets/cancerdiagnoser/huvud-och-hals/kvalitetsregister/presentation-in-english-swehncr.pdf (accessed on 1 February 2023).
- Pagh, A.; Grau, C.; Overgaard, J. Failure pattern and salvage treatment after radical treatment of head and neck cancer. Acta Oncol. 2016, 55, 625–632. [Google Scholar] [CrossRef] [PubMed]
- Overgaard, J.; Hansen, H.S.; Specht, L.; Overgaard, M.; Grau, C.; Andersen, E.; Bentzen, J.; Bastholt, L.; Hansen, O.; Johansen, J.; et al. Five compared with six fractions per week of conventional radiotherapy of squamous-cell carcinoma of head and neck: DAHANCA 6 and 7 randomised controlled trial. Lancet 2003, 362, 933–940. [Google Scholar] [CrossRef]
- Corvo, R. Evidence-based radiation oncology in head and neck squamous cell carcinoma. Radiother Oncol. 2007, 85, 156–170. [Google Scholar] [CrossRef]
- Leclerc, M.; Maingon, P.; Hamoir, M.; Dalban, C.; Calais, G.; Nuyts, S.; Serre, A.; Gregoire, V. A dose escalation study with intensity modulated radiation therapy (IMRT) in T2N0, T2N1, T3N0 squamous cell carcinomas (SCC) of the oropharynx, larynx and hypopharynx using a simultaneous integrated boost (SIB) approach. Radiother Oncol. 2013, 106, 333–340. [Google Scholar] [CrossRef]
- Gebre-Medhin, M.; Brun, E.; Engstrom, P.; Haugen Cange, H.; Hammarstedt-Nordenvall, L.; Reizenstein, J.; Nyman, J.; Abel, E.; Friesland, S.; Sjodin, H.; et al. ARTSCAN III: A Randomized Phase III Study Comparing Chemoradiotherapy With Cisplatin Versus Cetuximab in Patients With Locoregionally Advanced Head and Neck Squamous Cell Cancer. J. Clin. Oncol. 2021, 39, 38–47. [Google Scholar] [CrossRef] [PubMed]
- Atwell, D.; Elks, J.; Cahill, K.; Hearn, N.; Vignarajah, D.; Lagopoulos, J.; Min, M. A Review of Modern Radiation Therapy Dose Escalation in Locally Advanced Head and Neck Cancer. Clin. Oncol. 2020, 32, 330–341. [Google Scholar] [CrossRef]
- Welz, S.; Monnich, D.; Pfannenberg, C.; Nikolaou, K.; Reimold, M.; La Fougere, C.; Reischl, G.; Mauz, P.S.; Paulsen, F.; Alber, M.; et al. Prognostic value of dynamic hypoxia PET in head and neck cancer: Results from a planned interim analysis of a randomized phase II hypoxia-image guided dose escalation trial. Radiother Oncol. 2017, 124, 526–532. [Google Scholar] [CrossRef] [PubMed]
- Ang, K.K.; Harris, J.; Wheeler, R.; Weber, R.; Rosenthal, D.I.; Nguyen-Tan, P.F.; Westra, W.H.; Chung, C.H.; Jordan, R.C.; Lu, C.; et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N. Eng. J. Med. 2010, 363, 24–35. [Google Scholar] [CrossRef] [PubMed]
- Caudell, J.J.; Gillison, M.L.; Maghami, E.; Spencer, S.; Pfister, D.G.; Adkins, D.; Birkeland, A.C.; Brizel, D.M.; Busse, P.M.; Cmelak, A.J.; et al. NCCN Guidelines(R) Insights: Head and Neck Cancers, Version 1.2022. J. Natl. Compr. Cancer Netw. 2022, 20, 224–234. [Google Scholar]
- AJCC Cancer Staging Manual; Springer: Berlin/Heidelberg, Germany, 2010.
- Incanet. Nationellt kvalitetsregister för Huvud- och Halscancer (SweHNCR). 2019. Available online: https://statistik.incanet.se/Huvud-hals/ (accessed on 1 April 2023).
- Platek, M.E.; Jayaprakash, V.; Gupta, V.; Cohan, D.M.; Hicks, W.L., Jr.; Winslow, T.B.; Platek, A.J.; Groman, A.; Dibaj, S.; Arshad, H.; et al. Subsite variation in survival of oropharyngeal squamous cell carcinomas 2004 to 2011. Laryngoscope 2017, 127, 1087–1092. [Google Scholar] [CrossRef]
- Pfister, D.G.; Spencer, S.; Adelstein, D.; Adkins, D.; Anzai, Y.; Brizel, D.M.; Bruce, J.Y.; Busse, P.M.; Caudell, J.J.; Cmelak, A.J.; et al. Head and Neck Cancers, Version 2.2020, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Canc. Netw. 2020, 18, 873–898. [Google Scholar] [CrossRef] [PubMed]
- Embring, A.; Onjukka, E.; Mercke, C.; Lax, I.; Berglund, A.; Friesland, S. Dose escalation in oropharyngeal cancer: A comparison of simultaneous integrated boost and brachytherapy boost. Radiat. Oncol. 2023, 18, 65. [Google Scholar] [CrossRef] [PubMed]
- LENT SOMA tables. Radiother Oncol. 1995, 35, 17–60. [CrossRef]
- Cox, J.D.; Stetz, J.; Pajak, T.F. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int. J. Radiat. Oncol. Biol. Phys. 1995, 31, 1341–1346. [Google Scholar] [CrossRef]
- Institute, N.C. SEER*Explorer: An Interactive Website for SEER Cancer Statistics [Internet]; Surveillance Research Program: 2022. Available online: https://seer.cancer.gov/statistics-network/explorer (accessed on 27 December 2022).
- Incanet. Nationellt kvalitetsregister för huvudoch halscancer (Swedish head and neck cancer registry). 2021. Available online: https://statistik.incanet.se/Huvud-hals/ (accessed on 20 December 2022).
- Hoebers, F.J.; Pameijer, F.A.; de Bois, J.; Heemsbergen, W.; Balm, A.J.; Schornagel, J.H.; Rasch, C.R. Prognostic value of primary tumor volume after concurrent chemoradiation with daily low-dose cisplatin for advanced-stage head and neck carcinoma. Head Neck. 2008, 30, 1216–1223. [Google Scholar] [CrossRef]
- Lok, B.H.; Setton, J.; Caria, N.; Romanyshyn, J.; Wolden, S.L.; Zelefsky, M.J.; Park, J.; Rowan, N.; Sherman, E.J.; Fury, M.G.; et al. Intensity-modulated radiation therapy in oropharyngeal carcinoma: Effect of tumor volume on clinical outcomes. Int. J. Radiat. Oncol. Biol. Phys. 2012, 82, 1851–1857. [Google Scholar] [CrossRef]
- Okunieff, P.; Morgan, D.; Niemierko, A.; Suit, H.D. Radiation dose-response of human tumors. Int. J. Radiat. Oncol. Biol. Phys. 1995, 32, 1227–1237. [Google Scholar] [CrossRef]
- Adrian, G.; Carlsson, H.; Kjellen, E.; Sjovall, J.; Zackrisson, B.; Nilsson, P.; Gebre-Medhin, M. Primary tumor volume and prognosis for patients with p16-positive and p16-negative oropharyngeal squamous cell carcinoma treated with radiation therapy. Radiat. Oncol. 2022, 17, 107. [Google Scholar] [CrossRef]
- Lassen, P.; Lacas, B.; Pignon, J.P.; Trotti, A.; Zackrisson, B.; Zhang, Q.; Overgaard, J.; Blanchard, P.; Group, M.C. Prognostic impact of HPV-associated p16-expression and smoking status on outcomes following radiotherapy for oropharyngeal cancer: The MARCH-HPV project. Radiother Oncol. 2018, 126, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Van den Bogaert, W.; van der Schueren, E.; Horiot, J.C.; De Vilhena, M.; Schraub, S.; Svoboda, V.; Arcangeli, G.; de Pauw, M.; van Glabbeke, M. The EORTC randomized trial on three fractions per day and misonidazole in advanced head and neck cancer: Prognostic factors. Radiother Oncol. 1995, 35, 100–106. [Google Scholar] [CrossRef]
- Lauve, A.; Morris, M.; Schmidt-Ullrich, R.; Wu, Q.; Mohan, R.; Abayomi, O.; Buck, D.; Holdford, D.; Dawson, K.; Dinardo, L.; et al. Simultaneous integrated boost intensity-modulated radiotherapy for locally advanced head-and-neck squamous cell carcinomas: II—clinical results. Int. J. Radiat. Oncol. Biol. Phys. 2004, 60, 374–387. [Google Scholar] [CrossRef]
- Guerrero Urbano, T.; Clark, C.H.; Hansen, V.N.; Adams, E.J.; A’Hern, R.; Miles, E.A.; McNair, H.; Bidmead, M.; Warrington, A.P.; Dearnaley, D.P.; et al. A phase I study of dose-escalated chemoradiation with accelerated intensity modulated radiotherapy in locally advanced head and neck cancer. Radiother Oncol. 2007, 85, 36–41. [Google Scholar] [CrossRef] [PubMed]
- Gujral, D.M.; Miah, A.B.; Bodla, S.; Richards, T.M.; Welsh, L.; Schick, U.; Powell, C.J.; Clark, C.H.; Bidmead, M.A.; Grove, L.; et al. Final long-term results of a phase I/II study of dose-escalated intensity-modulated radiotherapy for locally advanced laryngo-hypopharyngeal cancers. Oral Oncol. 2014, 50, 1089–1097. [Google Scholar] [CrossRef] [PubMed]
- Nutting, C.M.; Griffin, C.L.; Sanghera, P.; Foran, B.; Beasley, M.; Bernstein, D.; Cosgrove, V.; Fisher, S.; West, C.M.; Sibtain, A.; et al. Dose-escalated intensity-modulated radiotherapy in patients with locally advanced laryngeal and hypopharyngeal cancers: ART DECO, a phase III randomised controlled trial. Eur. J. Cancer 2021, 153, 242–256. [Google Scholar] [CrossRef] [PubMed]
- Cvek, J.; Kubes, J.; Skacelikova, E.; Otahal, B.; Kominek, P.; Halamka, M.; Feltl, D. Hyperfractionated accelerated radiotherapy with concomitant integrated boost of 70–75 Gy in 5 weeks for advanced head and neck cancer. A phase I dose escalation study. Strahlenther Onkol. 2012, 188, 666–670. [Google Scholar] [CrossRef] [PubMed]
- Chakraborty, S.; Ghoshal, S.; Patil, V.M.; Oinam, A.S.; Sharma, S.C. Preliminary results of SIB-IMRT in head and neck cancers: Report from a regional cancer center in northern India. J. Cancer Res. Ther. 2009, 5, 165–172. [Google Scholar] [CrossRef]
- Kubes, J.; Cvek, J.; Vondracek, V.; Pala, M.; Feltl, D. Accelerated radiotherapy with concomitant boost technique (69.5 Gy/5 weeks): An alternative in the treatment of locally advanced head and neck cancer. Strahlenther Onkol. 2011, 187, 651–655. [Google Scholar] [CrossRef]
- Baudelet, M.; Van den Steen, L.; Tomassen, P.; Bonte, K.; Deron, P.; Huvenne, W.; Rottey, S.; De Neve, W.; Sundahl, N.; Van Nuffelen, G.; et al. Very late xerostomia, dysphagia, and neck fibrosis after head and neck radiotherapy. Head Neck. 2019, 41, 3594–3603. [Google Scholar] [CrossRef]
- Christianen, M.E.; Verdonck-de Leeuw, I.M.; Doornaert, P.; Chouvalova, O.; Steenbakkers, R.J.; Koken, P.W.; Leemans, C.R.; Oosting, S.F.; Roodenburg, J.L.; van der Laan, B.F.; et al. Patterns of long-term swallowing dysfunction after definitive radiotherapy or chemoradiation. Radiother Oncol. 2015, 117, 139–144. [Google Scholar] [CrossRef]
- Dragan, T.; Beauvois, S.; Moreau, M.; Paesmans, M.; Vandekerkhove, C.; Cordier, L.; Van Gestel, D. Clinical outcome and toxicity after simultaneous integrated boost IMRT in head and neck squamous cell cancer patients. Oral Oncol. 2019, 98, 132–140. [Google Scholar] [CrossRef] [PubMed]
- Langendijk, J.A.; Doornaert, P.; Verdonck-de Leeuw, I.M.; Leemans, C.R.; Aaronson, N.K.; Slotman, B.J. Impact of late treatment-related toxicity on quality of life among patients with head and neck cancer treated with radiotherapy. J. Clin. Oncol. 2008, 26, 3770–3776. [Google Scholar] [CrossRef]
- Taberna, M.; Rullan, A.J.; Hierro, C.; Navarro, V.; Vazquez, S.; Lozano, A.; Vilajosana, E.; Manos, M.; Mari, A.; Vinals, J.; et al. Late toxicity after radical treatment for locally advanced head and neck cancer. Oral Oncol. 2015, 51, 795–799. [Google Scholar] [CrossRef] [PubMed]
- Nabil, S.; Samman, N. Incidence and prevention of osteoradionecrosis after dental extraction in irradiated patients: A systematic review. Int. J. Oral Maxillofac Surg. 2011, 40, 229–243. [Google Scholar] [CrossRef] [PubMed]
- Reuther, T.; Schuster, T.; Mende, U.; Kubler, A. Osteoradionecrosis of the jaws as a side effect of radiotherapy of head and neck tumour patients—A report of a thirty year retrospective review. Int. J. Oral Maxillofac Surg. 2003, 32, 289–295. [Google Scholar] [CrossRef]
- Frankart, A.J.; Frankart, M.J.; Cervenka, B.; Tang, A.L.; Krishnan, D.G.; Takiar, V. Osteoradionecrosis: Exposing the Evidence Not the Bone. Int. J. Radiat. Oncol. Biol. Phys. 2021, 109, 1206–1218. [Google Scholar] [CrossRef]
- Toneatti, D.J.; Graf, R.R.; Burkhard, J.P.; Schaller, B. Survival of dental implants and occurrence of osteoradionecrosis in irradiated head and neck cancer patients: A systematic review and meta-analysis. Clin. Oral Investig. 2021, 25, 5579–5593. [Google Scholar] [CrossRef]
- Aarup-Kristensen, S.; Hansen, C.R.; Forner, L.; Brink, C.; Eriksen, J.G.; Johansen, J. Osteoradionecrosis of the mandible after radiotherapy for head and neck cancer: Risk factors and dose-volume correlations. Acta Oncol. 2019, 58, 1373–1377. [Google Scholar] [CrossRef]
- Mortensen, H.R.; Jensen, K.; Aksglaede, K.; Behrens, M.; Grau, C. Late dysphagia after IMRT for head and neck cancer and correlation with dose-volume parameters. Radiother Oncol. 2013, 107, 288–294. [Google Scholar] [CrossRef] [PubMed]
- Nutting, C.M.; Morden, J.P.; Harrington, K.J.; Urbano, T.G.; Bhide, S.A.; Clark, C.; Miles, E.A.; Miah, A.B.; Newbold, K.; Tanay, M.; et al. Parotid-sparing intensity modulated versus conventional radiotherapy in head and neck cancer (PARSPORT): A phase 3 multicentre randomised controlled trial. Lancet Oncol. 2011, 12, 127–136. [Google Scholar] [CrossRef] [PubMed]
- Machtay, M.; Moughan, J.; Trotti, A.; Garden, A.S.; Weber, R.S.; Cooper, J.S.; Forastiere, A.; Ang, K.K. Factors associated with severe late toxicity after concurrent chemoradiation for locally advanced head and neck cancer: An RTOG analysis. J. Clin. Oncol. 2008, 26, 3582–3589. [Google Scholar] [CrossRef]
- Olteanu, L.A.M.; Duprez, F.; De Neve, W.; Berwouts, D.; Vercauteren, T.; Bauters, W.; Deron, P.; Huvenne, W.; Bonte, K.; Goethals, I.; et al. Late mucosal ulcers in dose-escalated adaptive dose-painting treatments for head-and-neck cancer. Acta Oncol. 2018, 57, 262–268. [Google Scholar] [CrossRef]
- Rasmussen, J.H.; Hakansson, K.; Vogelius, I.R.; Aznar, M.C.; Fischer, B.M.; Friborg, J.; Loft, A.; Kristensen, C.A.; Bentzen, S.M.; Specht, L. Phase I trial of 18F-Fludeoxyglucose based radiation dose painting with concomitant cisplatin in head and neck cancer. Radiother Oncol. 2016, 120, 76–80. [Google Scholar] [CrossRef] [PubMed]
- Lyons, A.J.; Crichton, S.; Pezier, T. Trismus following radiotherapy to the head and neck is likely to have distinct genotype dependent cause. Oral Oncol. 2013, 49, 932–936. [Google Scholar] [CrossRef] [PubMed]
- Al-Mamgani, A.; van Rooij, P.; Verduijn, G.M.; Mehilal, R.; Kerrebijn, J.D.; Levendag, P.C. The impact of treatment modality and radiation technique on outcomes and toxicity of patients with locally advanced oropharyngeal cancer. Laryngoscope 2013, 123, 386–393. [Google Scholar] [CrossRef]
- Aggarwal, P.; Hutcheson, K.A.; Garden, A.S.; Mott, F.E.; Lu, C.; Goepfert, R.P.; Fuller, C.D.; Lai, S.Y.; Gunn, G.B.; Chambers, M.S.; et al. Determinants of patient-reported xerostomia among long-term oropharyngeal cancer survivors. Cancer 2021, 127, 4470–4480. [Google Scholar] [CrossRef]
- Perez, C.A.; Patel, M.M.; Chao, K.S.; Simpson, J.R.; Sessions, D.; Spector, G.J.; Haughey, B.; Lockett, M.A. Carcinoma of the tonsillar fossa: Prognostic factors and long-term therapy outcome. Int. J. Radiat. Oncol. Biol. Phys. 1998, 42, 1077–1084. [Google Scholar] [CrossRef]
- Mendenhall, W.M.; Amdur, R.J.; Stringer, S.P.; Villaret, D.B.; Cassisi, N.J. Radiation therapy for squamous cell carcinoma of the tonsillar region: A preferred alternative to surgery? J. Clin. Oncol. 2000, 18, 2219–2225. [Google Scholar] [CrossRef] [PubMed]
- Mendenhall, W.M.; Stringer, S.P.; Amdur, R.J.; Hinerman, R.W.; Moore-Higgs, G.J.; Cassisi, N.J. Is radiation therapy a preferred alternative to surgery for squamous cell carcinoma of the base of tongue? J. Clin. Oncol. 2000, 18, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Parsons, J.T.; Mendenhall, W.M.; Stringer, S.P.; Amdur, R.J.; Hinerman, R.W.; Villaret, D.B.; Moore-Higgs, G.J.; Greene, B.D.; Speer, T.W.; Cassisi, N.J.; et al. Squamous cell carcinoma of the oropharynx: Surgery, radiation therapy, or both. Cancer 2002, 94, 2967–2980. [Google Scholar] [CrossRef]
- Mak, A.C.; Morrison, W.H.; Garden, A.S.; Ang, K.K.; Goepfert, H.; Peters, L.J. Base-of-tongue carcinoma: Treatment results using concomitant boost radiotherapy. Int. J. Radiat. Oncol. Biol. Phys. 1995, 33, 289–296. [Google Scholar] [CrossRef]
- Brunin, F.; Mosseri, V.; Jaulerry, C.; Point, D.; Cosset, J.M.; Rodriguez, J. Cancer of the base of the tongue: Past and future. Head Neck. 1999, 21, 751–759. [Google Scholar] [CrossRef]
- Olmi, P.; Crispino, S.; Fallai, C.; Torri, V.; Rossi, F.; Bolner, A.; Amichetti, M.; Signor, M.; Taino, R.; Squadrelli, M.; et al. Locoregionally advanced carcinoma of the oropharynx: Conventional radiotherapy vs. accelerated hyperfractionated radiotherapy vs. concomitant radiotherapy and chemotherapy—A multicenter randomized trial. Int. J. Radiat. Oncol. Biol. Phys. 2003, 55, 78–92. [Google Scholar] [CrossRef]
- Chen, J.; Pappas, L.; Moeller, J.H.; Rankin, J.; Sharma, P.K.; Bentz, B.G.; Fang, L.C.; Hayes, J.K.; Shrieve, D.C.; Hitchcock, Y.J. Treatment of oropharyngeal squamous cell carcinoma with external beam radiation combined with interstitial brachytherapy. Head Neck. 2007, 29, 362–369. [Google Scholar] [CrossRef]
- Ward, M.C.; Lee, N.Y.; Caudell, J.J.; Zajichek, A.; Awan, M.J.; Koyfman, S.A.; Dunlap, N.E.; Zakem, S.J.; Hassanzadeh, C.; Marcrom, S.; et al. A competing risk nomogram to predict severe late toxicity after modern re-irradiation for squamous carcinoma of the head and neck. Oral Oncol. 2019, 90, 80–86. [Google Scholar] [CrossRef] [PubMed]
- Chera, B.S.; Amdur, R.J.; Tepper, J.; Qaqish, B.; Green, R.; Aumer, S.L.; Hayes, N.; Weiss, J.; Grilley-Olson, J.; Zanation, A.; et al. Phase 2 Trial of De-intensified Chemoradiation Therapy for Favorable-Risk Human Papillomavirus-Associated Oropharyngeal Squamous Cell Carcinoma. Int. J. Radiat. Oncol. Biol. Phys. 2015, 93, 976–985. [Google Scholar] [CrossRef] [PubMed]
- Yom, S.S.; Torres-Saavedra, P.; Caudell, J.J.; Waldron, J.N.; Gillison, M.L.; Xia, P.; Truong, M.T.; Kong, C.; Jordan, R.; Subramaniam, R.M.; et al. Reduced-Dose Radiation Therapy for HPV-Associated Oropharyngeal Carcinoma (NRG Oncology HN002). J. Clin. Oncol. 2021, 39, 956–965. [Google Scholar] [CrossRef] [PubMed]

| Dose-Escalated | Standard Dose | p-Value | Overall | |
|---|---|---|---|---|
| Number (%) | Number (%) | |||
| Subjects | 215 | 215 | 430 | |
| Gender | 0.196 | |||
| Female | 53 (24.7) | 66 (30.7) | 119 (27.7) | |
| Male | 162 (75.3) | 149 (69.3) | 311 (72.3) | |
| Age, mean (SD) | 62.2 (8.8) | 64.5 (9.8) | 0.011 | 63.3 (9.4) |
| HPV status | 0.441 | |||
| Negative | 33 (15.3) | 40 (19.6) | 73 (17.0) | |
| Positive | 182 (84.7) | 175 (81.4) | 357 (83.0) | |
| Performance status (PS) | 0.894 | |||
| PS 0 | 183 (85.1) | 181 (84.2) | 364 (84.7) | |
| PS 1–2 | 32 (14.9) | 34 (15.8) | 66 (15.3) | |
| Tumour | <0.001 | |||
| Base of tongue | 120 (57.4) | 33 (15.3) | 153 (36.1) | |
| Tonsil | 89 (42.6) | 166 (77.2) | 255 (60.1) | |
| Other * | 0 (0.0) | 16 (7.4) | 16 (3.8) | |
| Smoking status | 0.789 | |||
| Never | 70 (32.6) | 65 (30.2) | 135 (31.4) | |
| Current | 50 (23.3) | 48 (22.3) | 98 (22.8) | |
| Former | 95 (44.2) | 102 (47.4) | 197 (45.8) | |
| Tumour stage † | 0.012 | |||
| I-II | 17 (7.9) | 15 (7.0) | 32 (7.4) | |
| III | 18 (8.4) | 39 (18.1) | 57 (13.3) | |
| IVA-B | 180 (83.7) | 161 (74.9) | 341 (79.3) | |
| T-stage | <0.001 | |||
| T1 | 29 (13.5) | 71 (33.0) | 100 (23.3) | |
| T2 | 67 (31.2) | 101 (47.0) | 168 (39.1) | |
| T3 | 56 (26.0) | 28 (13.0) | 84 (19.5) | |
| T4 | 63 (29.3) | 15 (7.0) | 78 (18.1) | |
| Therapy | 0.056 | |||
| Cetuximab | 96 (44.7) | 102 (47.4) | 198 (46.1) | |
| Cisplatin | 65 (30.2) | 64 (29.8) | 129 (30.0) | |
| Cisplatin + cetuximab | 7 (3.3) | 0 (0.0) | 7 (1.6) | |
| None | 47 (21.9) | 49 (22.8) | 96 (22.3) | |
| Data source | 1.000 | |||
| Local quality registry | 190 (88.4) | 189 (87.9) | 379 (88.1) | |
| Dose planning system | 25 (11.6) | 26 (12.1) | 51 (11.9) | |
| Recurrence | 0.073 | |||
| No recurrence | 170 (79.1) | 184 (85.6) | 354 (82.3) | |
| Local recurrence | 22 (10.2) | 10 (4.7) | 32 (7.4) | |
| Regional recurrence | 4 (1.9) | 5 (2.3) | 9 (2.1) | |
| Distant metastases | 10 (4.7) | 13 (6.0) | 23 (5.3) | |
| Locoregional + distant metastases | 6 (2.8) | 2 (0.9) | 8 (1.9) | |
| Progressive disease during RT | 0 (0.0) | 1 (0.5) | 1 (0.2) | |
| Not assessable | 3 (1.4) | 0 (0.0) | 3 (0.7) | |
| Mortality | |||
|---|---|---|---|
| HR | 95% CI | p-Value | |
| Cohort | |||
| Standard dose | 1.00 | reference | |
| Dose-escalated | 0.97 | 0.68–1.40 | 0.885 |
| HPV status | |||
| Negative | 1.00 | reference | |
| Positive | 0.45 | 0.30–0.68 | <0.001 |
| ECOG PS | |||
| PS 0 | 1.00 | reference | |
| PS 1–2 | 1.51 | 1.01–2.24 | 0.043 |
| T stage | |||
| T1-T2 | 1.00 | reference | |
| T3-T4 | 1.42 | 0.93–2.16 | 0.108 |
| Smoking status | |||
| Never | 1.00 | reference | |
| Former | 1.33 | 0.83–2.13 | 0.239 |
| Current | 2.57 | 1.57–4.23 | <0.001 |
| Age (per year) | 1.04 | 1.02–1.06 | <0.001 |
| Normalised Age * | 1.46 | 1.21–1.77 | <0.001 |
| GTVT (per cm3) | 1.01 | 1.00–1.02 | 0.010 |
| Normalised GTVT † | 1.22 | 1.05–1.41 | 0.010 |
| Dose-Escalated | Standard Dose | Total | |||||
|---|---|---|---|---|---|---|---|
| Number (%) | Number (%) | p-Value | Number (%) | ||||
| Skin | 0.240 | ||||||
| Acute | 51 | (23.7) | 62 | (28.8) | 113 | (26.3) | |
| Late | 10 | (4.7) | 5 | (2.3) | 15 | (3.5) | |
| None | 154 | (71.6) | 148 | (68.8) | 302 | (70.2) | |
| Osteoradionecrosis | 0.001 | ||||||
| Late | 19 | (8.8) | 4 | (1.9) | 23 | (5.3) | |
| None | 196 | (91.2) | 211 | (98.1) | 407 | (94.7) | |
| Larynx | 1.000 | ||||||
| Acute | 0 | (0.0) | 0 | (0.0) | 0 | (0.0) | |
| Late | 3 | (1.4) | 2 | (0.9) | 5 | (1.2) | |
| None | 212 | (98.6) | 213 | (99.1) | 425 | (98.8) | |
| Salivary glands | 0.229 | ||||||
| Late | 15 | (7.0) | 22 | (10.2) | 37 | (8.6) | |
| None | 199 | (92.6) | 193 | (89.8) | 392 | (91.2) | |
| Trismus | 0.053 | ||||||
| Acute | 1 | (0.5) | 2 | (0.9) | 3 | (0.7) | |
| Late | 8 | (3.7) | 1 | (0.5) | 9 | (2.1) | |
| None | 206 | (95.8) | 212 | (98.6) | 418 | (97.2) | |
| Mucosa | 0.350 | ||||||
| Acute | 135 | (62.8) | 128 | (59.5) | 263 | (61.2) | |
| Late | 5 | (2.3) | 2 | (0.9) | 7 | (1.6) | |
| None | 75 | (34.9) | 85 | (39.5) | 160 | (37.2) | |
| Dysphagia | 0.012 | ||||||
| Late | 39 | (18.1) | 21 | (9.8) | 60 | (14.0) | |
| None | 176 | (81.9) | 194 | (90.2) | 370 | (86.1) | |
| Patient | Age (Years) | Gender | Performance Status at Start of Radiotherapy | Tumour Stage * | Dose Level | Cause of Death | Time of Death (After End of Radiotherapy) |
|---|---|---|---|---|---|---|---|
| 1 | 81 | Male | 0 | IVA | Dose-escalated | Massive pharyngeal bleeding | 6 months |
| 2 | 79 | Female | 0 | IVA | Dose-escalated | Acute radiation toxicity | 3 weeks |
| 3 | 73 | Male | 2 | II | Dose-escalated | Acute radiation toxicity | 6 days |
| 4 | 70 | Male | 1 | III | Dose-escalated | Infection | 3 weeks |
| 5 | 68 | Male | 0 | IVA | Standard dose | Acute radiation toxicity | 10 days |
| 6 | 65 | Male | 0 | IVA | Standard dose | Acute radiation toxicity | 4 weeks |
| 7 | 63 | Male | 0 | IVA | Dose-escalated | ORN and infection | 5 years |
| 8 | 63 | Female | 0 | IVA | Standard dose | Consequential late effects, infection | 6 months |
| 9 | 59 | Male | 0 | IVA | Dose-escalated | Massive pharyngeal bleeding | 1 year |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Embring, A.; Onjukka, E.; Mercke, C.; Lax, I.; Berglund, A.; Friesland, S. Dose Escalation of Oropharyngeal Cancer: Long-Time Follow-Up and Side Effects. Cancers 2023, 15, 2580. https://doi.org/10.3390/cancers15092580
Embring A, Onjukka E, Mercke C, Lax I, Berglund A, Friesland S. Dose Escalation of Oropharyngeal Cancer: Long-Time Follow-Up and Side Effects. Cancers. 2023; 15(9):2580. https://doi.org/10.3390/cancers15092580
Chicago/Turabian StyleEmbring, Anna, Eva Onjukka, Claes Mercke, Ingmar Lax, Anders Berglund, and Signe Friesland. 2023. "Dose Escalation of Oropharyngeal Cancer: Long-Time Follow-Up and Side Effects" Cancers 15, no. 9: 2580. https://doi.org/10.3390/cancers15092580
APA StyleEmbring, A., Onjukka, E., Mercke, C., Lax, I., Berglund, A., & Friesland, S. (2023). Dose Escalation of Oropharyngeal Cancer: Long-Time Follow-Up and Side Effects. Cancers, 15(9), 2580. https://doi.org/10.3390/cancers15092580







