Telemedical Consultations in Palliative Care: Benefits through Knowledge Exchange and Intercollegiate Collaboration—Findings from the German oVID Project
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
3. Results
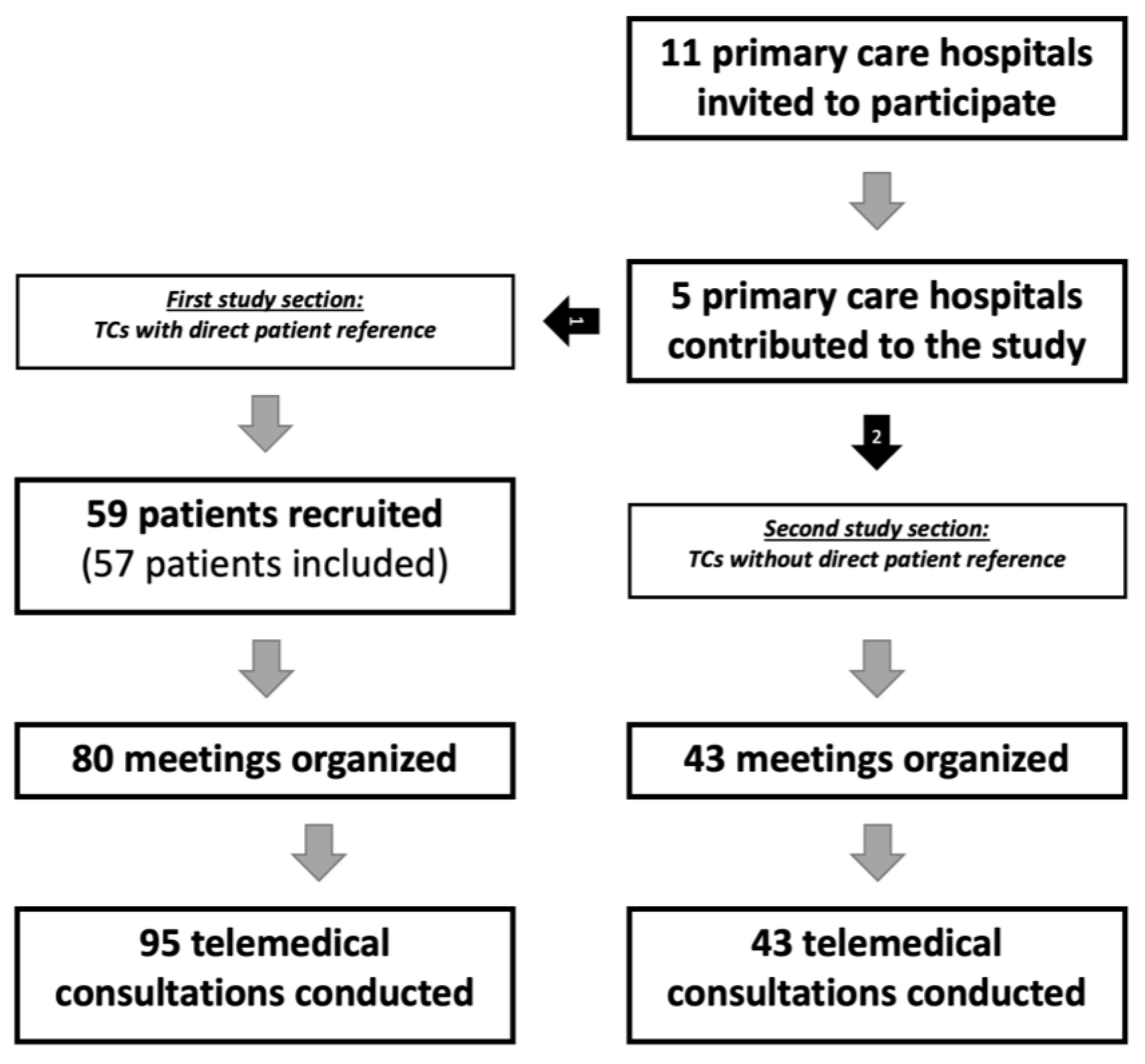
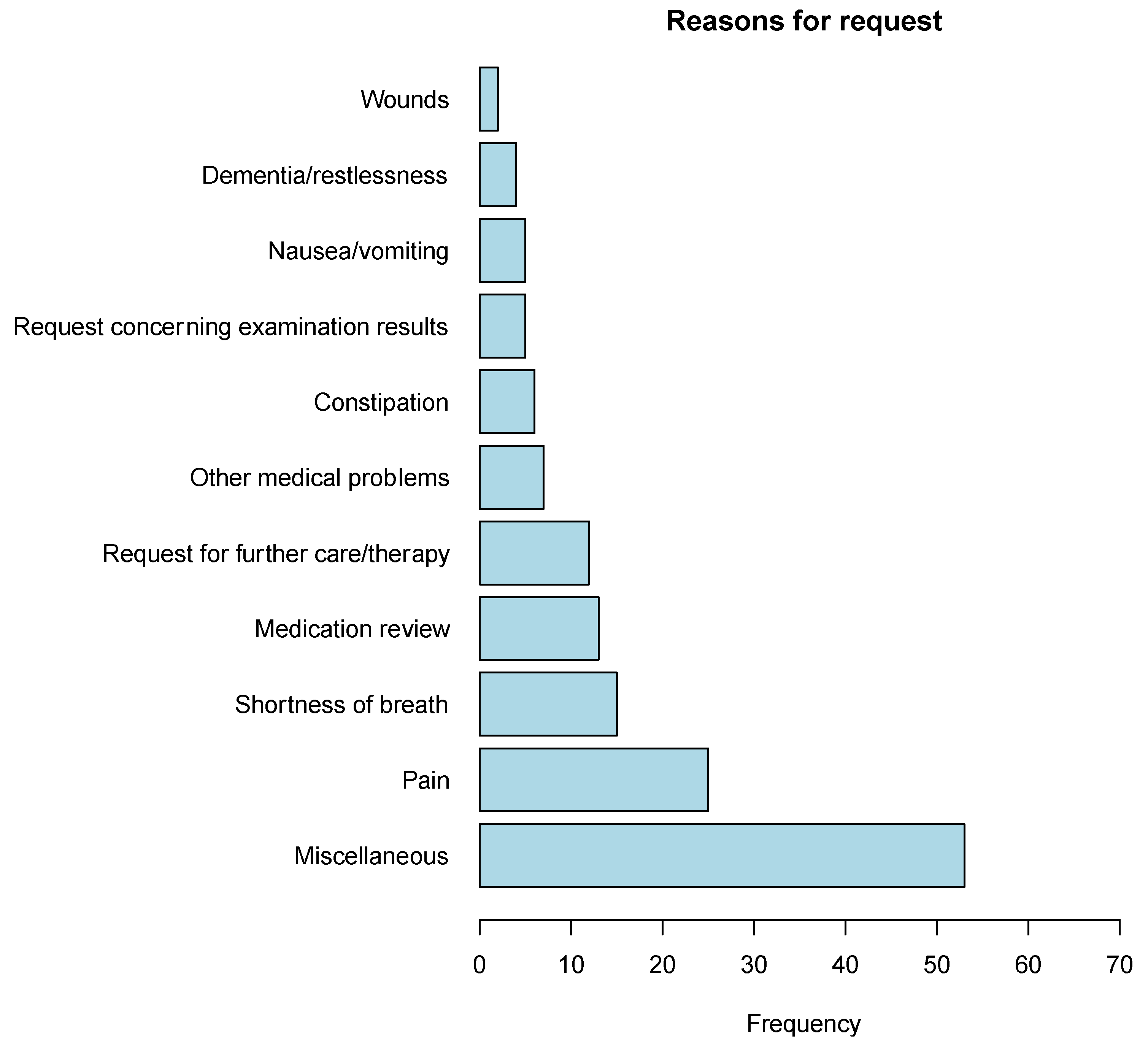
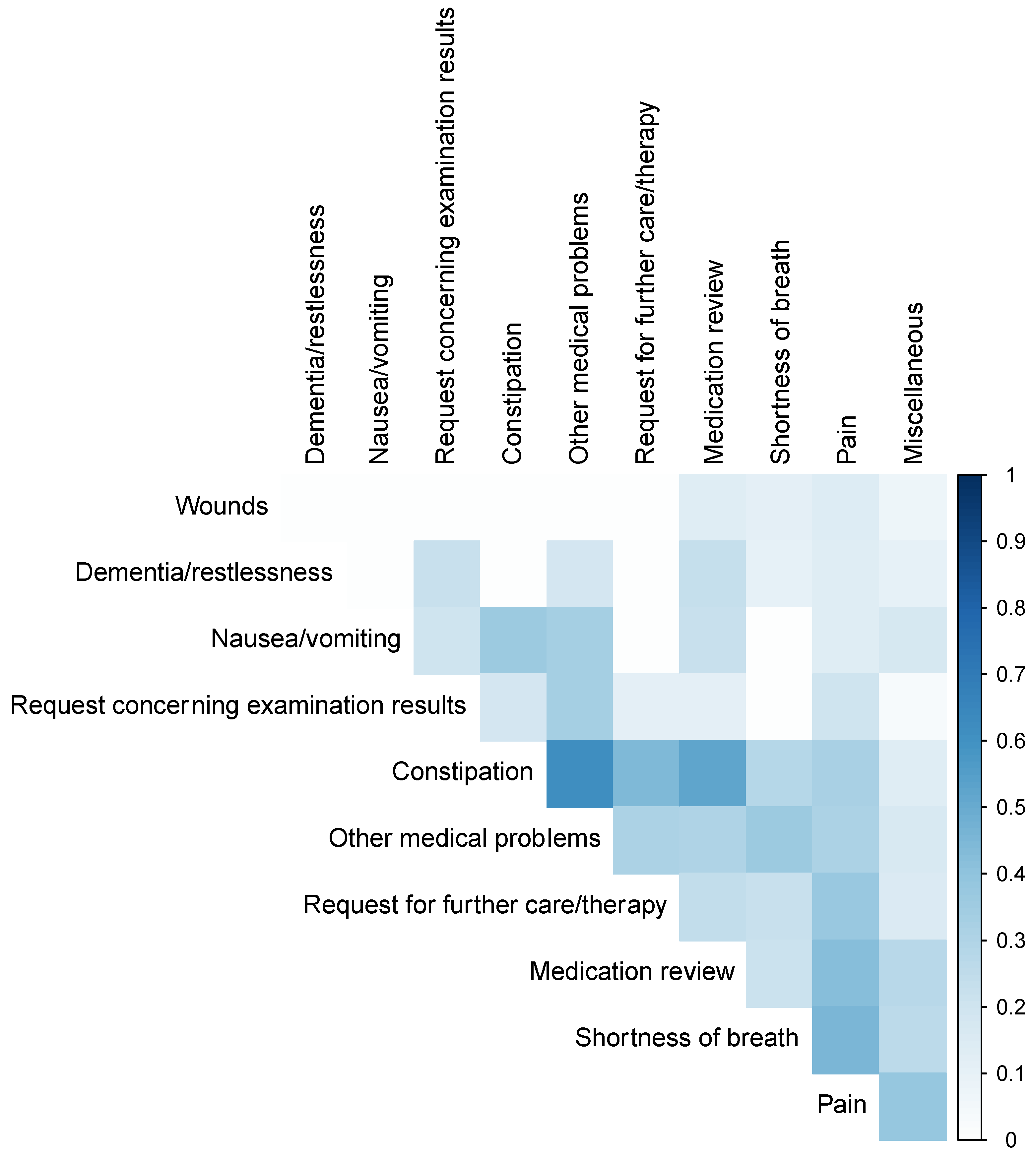
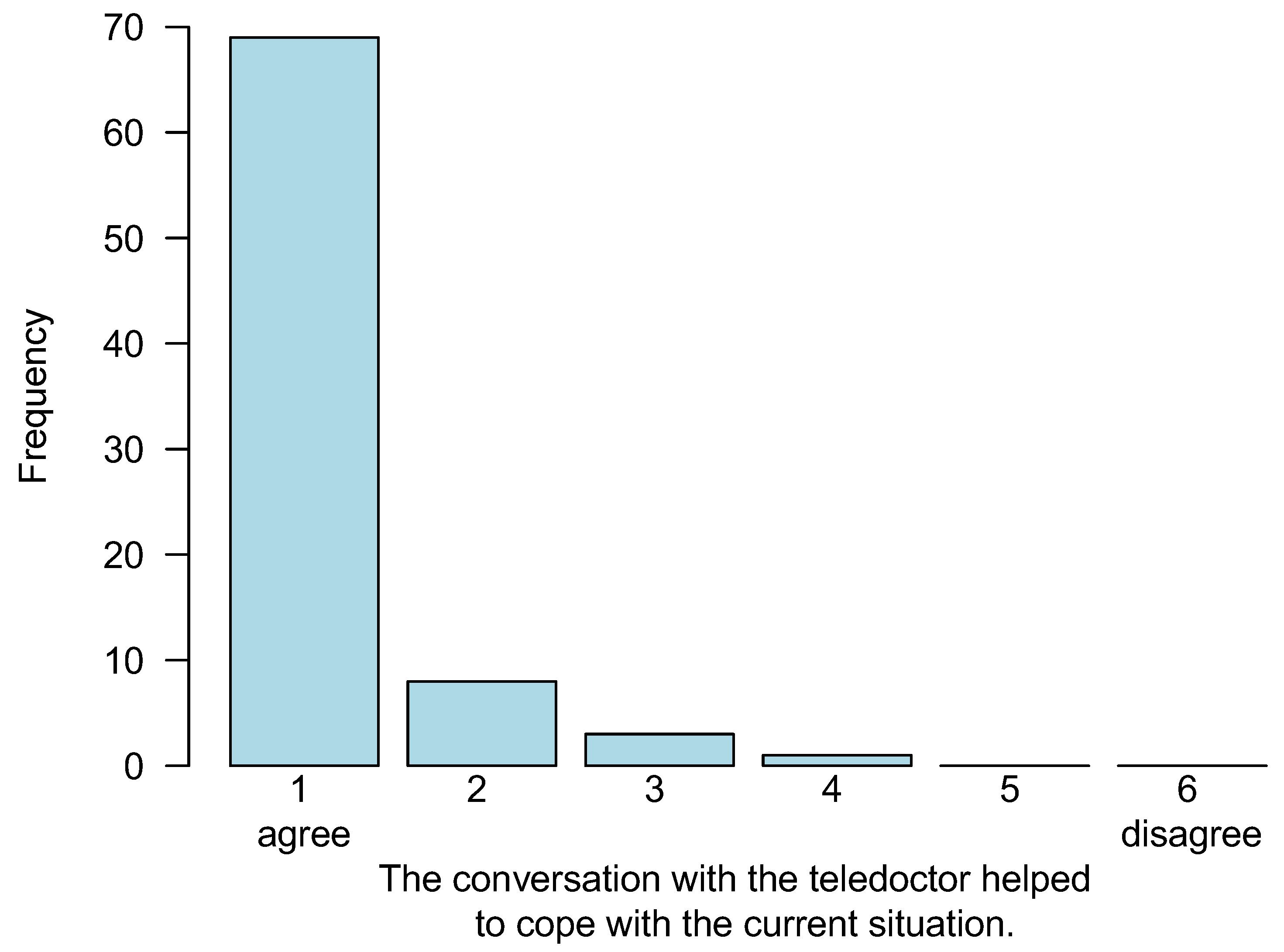
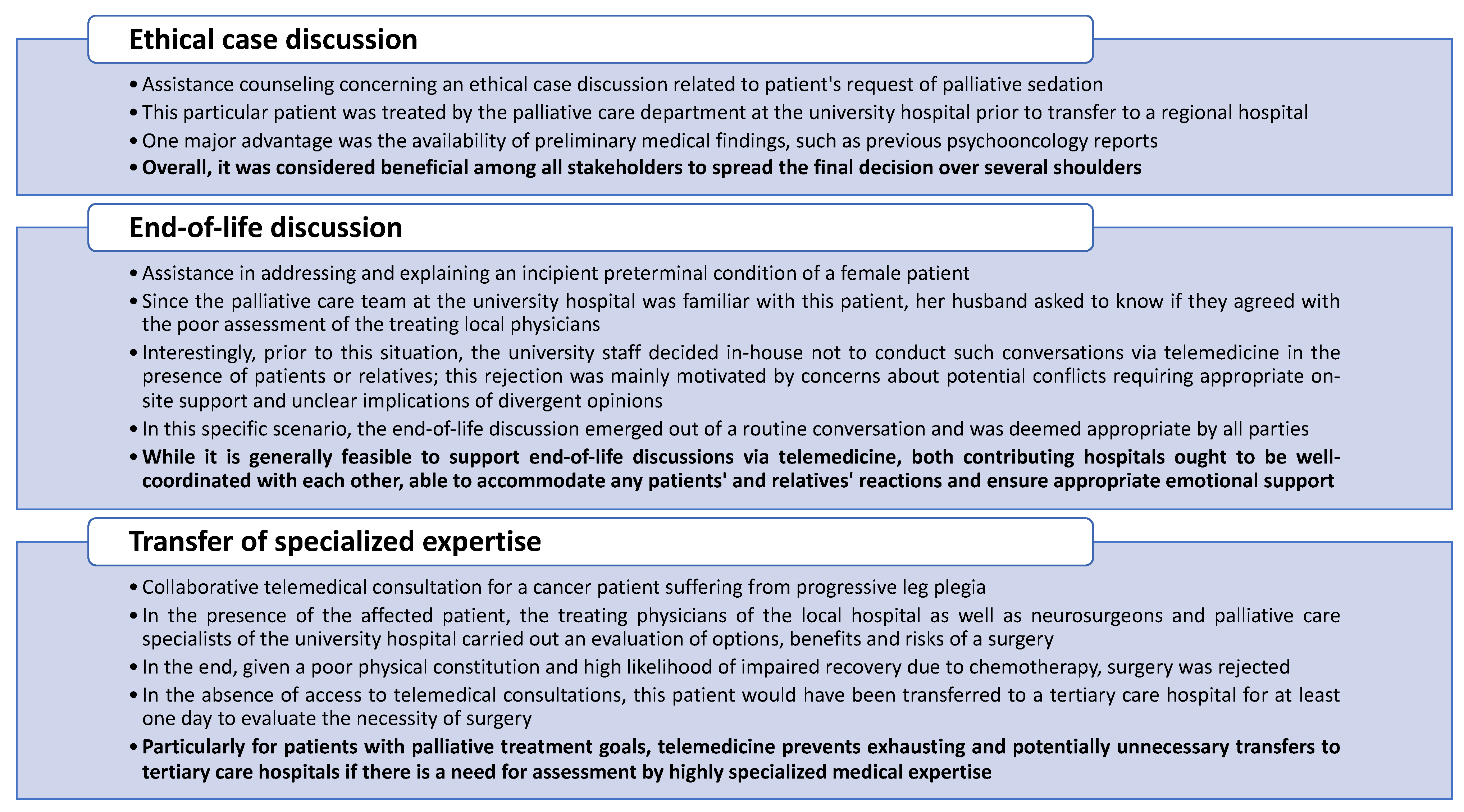
3.1. First Study Section: TCs with Direct Patient Reference
3.2. Second Study Section: TCs without Direct Patient Reference
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ritchey, K.C.; Foy, A.; McArdel, E.; Gruenewald, D.A. Reinventing palliative care delivery in the era of COVID-19: How telemedicine can support end of life care. Am. J. Hosp. Palliat. Med. 2020, 37, 992–997. [Google Scholar] [CrossRef] [PubMed]
- Sirintrapun, S.J.; Lopez, A.M. Telemedicine in cancer care. Am. Soc. Clin. Oncol. Educ. Book 2018, 38, 540–545. [Google Scholar] [CrossRef] [PubMed]
- Worster, B.; Swartz, K. Telemedicine and palliative care: An increasing role in supportive oncology. Curr. Oncol. Rep. 2017, 19, 37. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Cárdenas, M.A.; Iriarte-Aristizábal, M.F.; León-Delgado, M.X.; Rodríguez-Campos, L.F.; Correa-Morales, J.E.; Cañón-Piñeros, A.; Parra, S.L. Rural Palliative Care Telemedicine for Advanced Cancer Patients: A Systematic Review. Am. J. Hosp. Palliat. Care 2022. online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Hayes Bauer, E.; Ørsted Schultz, A.N.; Brink, A.; Oechsle Jørgensen, L.; Bollig, G. Patients’ and Relatives’ Preferences for a Palliative/Oncology Day Ward and Out-of-Hours Telemedicine—An Interpretive Description. Healthcare 2021, 9, 758. [Google Scholar] [CrossRef] [PubMed]
- Kamal, A.H.; Bausewein, C.; Casarett, D.J.; Currow, D.C.; Dudgeon, D.J.; Higginson, I.J. Standards, guidelines, and quality measures for successful specialty palliative care integration into oncology: Current approaches and future directions. J. Clin. Oncol. 2020, 38, 987. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. World Health Organisation Definition of Palliative Care. Available online: http://www.who.int/cancer/palliative/definition/en/ (accessed on 28 June 2022).
- Bajwah, S.; Oluyase, A.O.; Yi, D.; Gao, W.; Evans, C.J.; Grande, G.; Todd, C.; Costantini, M.; Murtagh, F.E.; Higginson, I.J. The effectiveness and cost-effectiveness of hospital-based specialist palliative care for adults with advanced illness and their caregivers. Cochrane Database Syst. Rev. 2020, 9, cd012780. [Google Scholar] [CrossRef]
- Smith, S.; Brick, A.; O’Hara, S.; Normand, C. Evidence on the cost and cost-effectiveness of palliative care: A literature review. Palliat. Med. 2014, 28, 130–150. [Google Scholar] [CrossRef]
- Temel, J.S.; Greer, J.A.; Muzikansky, A.; Gallagher, E.R.; Admane, S.; Jackson, V.A.; Dahlin, C.M.; Blinderman, C.D.; Jacobsen, J.; Pirl, W.F.; et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N. Engl. J. Med. 2010, 363, 733–742. [Google Scholar] [CrossRef]
- Hess, S.; Stiel, S.; Hofmann, S.; Klein, C.; Lindena, G.; Ostgathe, C. Trends in specialized palliative care for non-cancer patients in Germany--data from the national hospice and palliative care evaluation (HOPE). Eur. J. Intern. Med. 2014, 25, 187–192. [Google Scholar] [CrossRef]
- Kirkova, J.; Walsh, D.; Rybicki, L.; Davis, M.P.; Aktas, A.; Tao, J.; Homsi, J. Symptom severity and distress in advanced cancer. Palliat. Med. 2010, 24, 330–339. [Google Scholar] [CrossRef] [PubMed]
- Sewtz, C.; Muscheites, W.; Grosse-Thie, C.; Kriesen, U.; Leithaeuser, M.; Glaeser, D.; Hansen, P.; Kundt, G.; Fuellen, G.; Junghanss, C. Longitudinal observation of anxiety and depression among palliative care cancer patients. Ann. Palliat. Med. 2021, 10, 3836–3846. [Google Scholar] [CrossRef] [PubMed]
- See, D.; Le, B.; Gorelik, A.; Eastman, P. Symptom burden in malignant and non-malignant disease on admission to a palliative care unit. BMJ Support Palliat. Care 2019, 12, e792–e797. [Google Scholar] [CrossRef] [PubMed]
- van Riet Paap, J.; Vernooij-Dassen, M.; Sommerbakk, R.; Moyle, W.; Hjermstad, M.J.; Leppert, W.; Vissers, K.; Engels, Y. Implementation of improvement strategies in palliative care: An integrative review. Implement. Sci. 2015, 10, 1–9. [Google Scholar] [CrossRef]
- Oertel, M.; Schmidt, R.; Steike, D.R.; Eich, H.T.; Lenz, P. Palliative care on the radiation oncology ward—Improvements in clinical care through interdisciplinary ward rounds. Strahlenther. Onkol. 2023, 199, 251–257. [Google Scholar] [CrossRef]
- van Gurp, J.; van Selm, M.; van Leeuwen, E.; Vissers, K.; Hasselaar, J. Teleconsultation for integrated palliative care at home: A qualitative study. Palliat. Med. 2016, 30, 257–269. [Google Scholar] [CrossRef]
- Hoek, P.D.; Schers, H.J.; Bronkhorst, E.M.; Vissers, K.C.P.; Hasselaar, J.G.J. The effect of weekly specialist palliative care teleconsultations in patients with advanced cancer—A randomized clinical trial. BMC Med. 2017, 15, 119. [Google Scholar] [CrossRef]
- Dillen, K.; Joshi, M.; Krumm, N.; Hesse, M.; Brunsch, H.; Schmidt, H.; Strupp, J.; Radbruch, L.; Rolke, R.; Voltz, R. Availability as key determinant in the palliative home care setting from the patients’ and family caregivers’ perspectives: A quantitative-qualitative-content analysis approach. Palliat. Support. Care 2021, 19, 570–579. [Google Scholar] [CrossRef]
- der Hospiz, G.z.V. und Palliativversorgung in Deutschland (Hospiz-und Palliativgesetz–HPG). xav 2015. Available online: https://www.bgbl.de/xaver/bgbl/start.xav?start=/#__bgbl____1682582526887 (accessed on 28 June 2022).
- Herbst, F.A.; Heckel, M.; Stiel, S.; Ostgathe, C. Development of empirical recommendations for regional hospice and palliative care networks in Germany: A qualitative study. Z. Evid. Fortbild. Qual. Gesundh. 2019, 140, 35–42. [Google Scholar] [CrossRef]
- Oelmeier, K.; Schmitz, R.; Möllers, M.; Braun, J.; Deharde, D.; Sourouni, M.; Köster, H.A.; Apsite, G.; Eveslage, M.; Fischhuber, K.; et al. Satisfaction with and Feasibility of Prenatal Counseling via Telemedicine: A Prospective Cohort Study. Telemed. J. E Health 2022, 28, 1193–1198. [Google Scholar] [CrossRef]
- Dice, L.R. Measures of the amount of ecologic association between species. Ecology 1945, 26, 297–302. [Google Scholar] [CrossRef]
- Team, R.C. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2016. [Google Scholar]
- Widberg, C.; Wiklund, B.; Klarare, A. Patients’ experiences of eHealth in palliative care: An integrative review. BMC Palliat. Care 2020, 19, 158. [Google Scholar] [CrossRef] [PubMed]
- Jess, M.; Timm, H.; Dieperink, K.B. Video consultations in palliative care: A systematic integrative review. Palliat Med. 2019, 33, 942–958. [Google Scholar] [CrossRef]
- Ebneter, A.S.; Sauter, T.C.; Christen, A.; Eychmueller, S. Feasibility, acceptability and needs in telemedicine for palliative care. Swiss Med. Wkly. 2022, 152, w30148. [Google Scholar] [CrossRef]
- Kazazian, K.; Ng, D.; Swallow, C.J. Impact of the coronavirus disease 2019 pandemic on delivery of and models for supportive and palliative care for oncology patients. Curr. Opin. Support Palliat. Care 2022, 16, 130–137. [Google Scholar] [CrossRef]
- Dotzauer, R.; Böhm, K.; Brandt, M.P.; Sparwasser, P.; Haack, M.; Frees, S.K.; Kamal, M.M.; Mager, R.; Jäger, W.; Höfner, T.; et al. Global change of surgical and oncological clinical practice in urology during early COVID-19 pandemic. World J. Urol. 2021, 39, 3139–3145. [Google Scholar] [CrossRef]
- Marom, T.; Pitaro, J.; Shah, U.K.; Torretta, S.; Marchisio, P.; Kumar, A.T.; Barth, P.C.; Tamir, S.O. Otitis Media Practice During the COVID-19 Pandemic. Front. Cell. Infect. Microbiol. 2021, 11, 749911. [Google Scholar] [CrossRef]
- Bandini, J.I.; Scherling, A.; Farmer, C.; Fratkin, M.; Mistler, B.; Ast, K.; Ahluwalia, S.C. Experiences with Telehealth for Outpatient Palliative Care: Findings from a Mixed-Methods Study of Patients and Providers across the United States. J. Palliat. Med. 2022, 25, 1079–1087. [Google Scholar] [CrossRef]
- Nanda, M.; Sharma, R. A Review of Patient Satisfaction and Experience with Telemedicine: A Virtual Solution During and Beyond COVID-19 Pandemic. Telemed. J. E Health 2021, 27, 1325–1331. [Google Scholar] [CrossRef]
- Bramati, P.S.; Amaram-Davila, J.S.; Reddy, A.S.; Bruera, E. Reduction of Missed Palliative Care Appointments After the Implementation of Telemedicine. J. Pain Symptom. Manag. 2022, 63, e777–e779. [Google Scholar] [CrossRef]
- Dielissen, P.W.; van den Beuken-van Everdingen, M.H.J. Quality of discharge summary for patients with limited life expectancy. Ned. Tijdschr. Geneeskd. 2022, 166, D6575. [Google Scholar] [PubMed]
- Kuusisto, A.; Saranto, K.; Korhonen, P.; Haavisto, E. Quality of information transferred to palliative care. J. Clin. Nurs. 2022. online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Eze, N.D.; Mateus, C.; Cravo Oliveira Hashiguchi, T. Telemedicine in the OECD: An umbrella review of clinical and cost-effectiveness, patient experience and implementation. PLoS ONE 2020, 15, e0237585. [Google Scholar] [CrossRef] [PubMed]
- Snoswell, C.L.; Taylor, M.L.; Comans, T.A.; Smith, A.C.; Gray, L.C.; Caffery, L.J. Determining if Telehealth Can Reduce Health System Costs: Scoping Review. J. Med. Internet Res. 2020, 22, e17298. [Google Scholar] [CrossRef] [PubMed]
- Menon, P.R.; Stapleton, R.D.; McVeigh, U.; Rabinowitz, T. Telemedicine as a tool to provide family conferences and palliative care consultations in critically ill patients at rural health care institutions: A pilot study. Am. J. Hosp. Palliat. Care 2015, 32, 448–453. [Google Scholar] [CrossRef] [PubMed]
- Prihodova, L.; Guerin, S.; Kernohan, W.G. Knowledge transfer and exchange frameworks in health and their applicability to palliative care: Scoping review protocol. J. Adv. Nurs. 2015, 71, 1717–1725. [Google Scholar] [CrossRef]
- Davies, H.; Powell, A.; Nutley, S. Mobilizing knowledge in health care. In The Oxford Handbook of Health Care Management; Oxford University Press: Oxford, UK, 2016; pp. 1–27. [Google Scholar]
- Finucane, A.; Carduff, E.; Meade, R.; Doyle, S.; Fenning, S.; Cumming, S.; Hekerem, D.; Rahman, F.; Lugton, J.; Johnston, B.; et al. Palliative care research promotion in policy and practice: A knowledge exchange process. BMJ Support Palliat. Care 2021, 12, e285–e292. [Google Scholar] [CrossRef]
- Pornrattanakavee, P.; Srichan, T.; Seetalarom, K.; Saichaemchan, S.; Oer-Areemitr, N.; Prasongsook, N. Impact of interprofessional collaborative practice in palliative care on outcomes for advanced cancer inpatients in a resource-limited setting. BMC Palliat. Care 2022, 21, 229. [Google Scholar] [CrossRef]
- Leslie, K.F.; Probst, M.K.; Hawkins, T.L. Evaluation of an Interprofessional Academic-Practice Partnership in End of Life Care. Innov. Pharm. 2021, 12, 4004. [Google Scholar] [CrossRef]
- Kruse, C.S.; Molina-Nava, A.; Kapoor, Y.; Anerobi, C.; Maddukuri, H. Analyzing the Effect of Telemedicine on Domains of Quality Through Facilitators and Barriers to Adoption: Systematic Review. J. Med. Internet Res. 2023, 25, e43601. [Google Scholar] [CrossRef]
- Ftouni, R.; AlJardali, B.; Hamdanieh, M.; Ftouni, L.; Salem, N. Challenges of Telemedicine during the COVID-19 pandemic: A systematic review. BMC Med. Inform. Decis. Mak. 2022, 22, 207. [Google Scholar] [CrossRef] [PubMed]
- Perez-Roman, R.J.; Trenchfield, D.R.; Perez-Roman, N.I.; Wang, M.Y. The Legal and Socioeconomic Considerations in Spine Telemedicine. Neurosurgery 2022, 90, 365–371. [Google Scholar] [CrossRef] [PubMed]
- Clark, P.A.; Capuzzi, K.; Harrison, J. Telemedicine: Medical, legal and ethical perspectives. Med. Sci. Monit. 2010, 16, Ra261–Ra272. [Google Scholar] [PubMed]
- De Panfilis, L.; Di Leo, S.; Peruselli, C.; Ghirotto, L.; Tanzi, S. “I go into crisis when…”: Ethics of care and moral dilemmas in palliative care. BMC Palliat. Care 2019, 18, 70. [Google Scholar] [CrossRef]
- Wang, T.; Molassiotis, A.; Chung, B.P.M.; Tan, J.Y. Unmet care needs of advanced cancer patients and their informal caregivers: A systematic review. BMC Palliat. Care 2018, 17, 96. [Google Scholar] [CrossRef]
- Bausewein, C.; Booth, S.; Gysels, M.; Kühnbach, R.; Haberland, B.; Higginson, I.J. Understanding breathlessness: Cross-sectional comparison of symptom burden and palliative care needs in chronic obstructive pulmonary disease and cancer. J. Palliat. Med. 2010, 13, 1109–1118. [Google Scholar] [CrossRef]
- Alkureishi, M.A.; Choo, Z.-Y.; Lenti, G.; Castaneda, J.; Zhu, M.; Nunes, K.; Weyer, G.; Oyler, J.; Shah, S.; Lee, W.W. Clinician perspectives on telemedicine: Observational cross-sectional study. JMIR Hum. Factors 2021, 8, e29690. [Google Scholar] [CrossRef]
- Avanesova, A.A.; Shamliyan, T.A. Worldwide implementation of telemedicine programs in association with research performance and health policy. Health Policy Technol. 2019, 8, 179–191. [Google Scholar] [CrossRef]
| Age (Years) | |
| Min/max Mean (SD) | 27.1/94.3 69.7 (13.6) |
| Sex | |
| Female, n (%) Male, n (%) | 34 (59.6%) 23 (40.4%) |
| Distance to clinic (km) | |
| Min/max Mean (SD) | 0/102.0 20.6 (21.6) |
| Marital status | |
| Married/partnered, n (%) Single, n (%) Divorced, n (%) Widowed, n (%) Not known, n (%) | 34 (59.6%) 6 (10.5%) 3 (5.3%) 12 (21.1%) 2 (3.6%) |
| Main diagnosis | |
| Cancer (total), n (%) Cancer (metastasized), n (%) COPD, n (%) Other, n (%) | 46 (80.7%) 39 (68.4%) 3 (5.3%) 8 (14.0%) |
| Phase of illness | |
| Stable, n (%) Unstable, n (%) Deteriorating, n (%) Dying, n (%) Not known, n (%) | 13 (22.8%) 24 (42.1%) 16 (28.1%) 1 (1.8%) 3 (5.3%) |
| Active treatment | |
| Yes, n (%) No, n (%) Not known, n (%) | 21 (36.8%) 27 (47.4%) 9 (15.8%) |
| Type of active treatment | |
| Radiation therapy, n (%) Chemo- or immunotherapy, n (%) Surgery, n (%) | 13 (22.8%) 25 (43.9%) 21 (36.8%) |
| Defined treatment limits | |
| Yes, n (%) No, n (%) Not known, n (%) | 27 (47.4%) 23 (40.4%) 7 (12.3%) |
| Days of treatment | |
| Min/max Mean (SD) | 1.0/56.0 12.5 (13.7) |
| Care dependency (GSSC) | |
| No need for care, n (%) Level of care 1, n (%) Level of care 2, n (%) Level of care 3, n (%) Level of care 4, n (%) Level of care 5, n (%) Not known, n (%) | 11 (19.3%) 0 (0.0%) 8 (14.0%) 13 (22.8%) 1 (1.8%) 0 (0.0%) 24 (42.2%) |
| Duration (n = 80) | |
| Min/max Mean (SD) | 0/73.0 23.1 (14.7) |
| Involvement of further medical departments (n = 80) | |
| Yes, n (%) No, n (%) Not known, n (%) | 21 (26.2%) 57 (71.2%) 2 (2.5%) |
| Involved medical departments | Dermatology, Oncology, Gynecology, Infectiology, Neurology, Neurosurgery, Gastroenterology, Pneumology, Radiotherapy, Urology, Social Service |
| Purpose of the initial consultation request (related to n = 57 patients) | |
| Palliative medicine consultation *, n (%) Patient transfer, n (%) Intercollegiate case conference *, n (%) Symptoms or administration *, n (%) Education, n (%) Not known, n (%) | 22 (38.6%) 17 (29.8%) 12 (21.2%) 4 (7.0%) 1 (1.8%) 1 (1.8%) |
| Occurrence of technical issues (n = 80) | |
| Yes (both physicians), n (%) Yes (one physician), n (%) No, n (%) | 16 (20.0%) 13 (16.2%) 51 (63.7%) |
| Type of technical issues | Login, video quality, sound quality, session establishment, data exchange, session termination, internet connection difficulties, and consultation requests not received |
| Consultations in the presence of the patient (n = 95) | |
| Yes, n (%) No, n (%) Not known, n (%) | 34 (35.8%) 59 (62.1%) 2 (2.2%) |
| Consultation results (n = 71) | |
| Adjustment of therapy or medication No further measures Other unclassified usable results | 25 (35.2%) 13 (18.3%) 33 (46.5%) |
| Avoided Outpatient Presentations (n = 95) | |
| Yes, n (%) | 20 (21.1%) |
| No, n (%) | 3 (3.2%) |
| Contradictory, n (%) * | 15 (15.8%) |
| Not relevant, n (%) | 57 (60.0%) |
| Avoided Transfers of Patients (n = 95) | |
| Yes, n (%) | 12 (12.6%) |
| No, n (%) | 9 (9.5%) |
| Contradictory, n (%) * | 18 (19.0%) |
| Not relevant, n (%) | 56 (58.9%) |
| Gain of Knowledge (n = 95) | |
| Yes, n (%) | 93 (97.9%) |
| No, n (%) | 0 (0.0%) |
| Contradictory, n (%) * | 2 (2.1%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bückmann, A.; Bernhardt, F.; Eveslage, M.; Storck, M.; Thölking, G.; Buss, H.; Domagk, D.; Juhra, C.; Lenz, P. Telemedical Consultations in Palliative Care: Benefits through Knowledge Exchange and Intercollegiate Collaboration—Findings from the German oVID Project. Cancers 2023, 15, 2512. https://doi.org/10.3390/cancers15092512
Bückmann A, Bernhardt F, Eveslage M, Storck M, Thölking G, Buss H, Domagk D, Juhra C, Lenz P. Telemedical Consultations in Palliative Care: Benefits through Knowledge Exchange and Intercollegiate Collaboration—Findings from the German oVID Project. Cancers. 2023; 15(9):2512. https://doi.org/10.3390/cancers15092512
Chicago/Turabian StyleBückmann, Andreas, Florian Bernhardt, Maria Eveslage, Michael Storck, Gerold Thölking, Helga Buss, Dirk Domagk, Christian Juhra, and Philipp Lenz. 2023. "Telemedical Consultations in Palliative Care: Benefits through Knowledge Exchange and Intercollegiate Collaboration—Findings from the German oVID Project" Cancers 15, no. 9: 2512. https://doi.org/10.3390/cancers15092512
APA StyleBückmann, A., Bernhardt, F., Eveslage, M., Storck, M., Thölking, G., Buss, H., Domagk, D., Juhra, C., & Lenz, P. (2023). Telemedical Consultations in Palliative Care: Benefits through Knowledge Exchange and Intercollegiate Collaboration—Findings from the German oVID Project. Cancers, 15(9), 2512. https://doi.org/10.3390/cancers15092512






