Prognostic Significance of MRE11 Overexpression in Colorectal Cancer Patients
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients and Tissue Specimens
2.2. Sample Preparation and Tissue Microarrays
2.3. Immunohistochemistry
2.4. Statistical Analysis
3. Results
3.1. Study Population
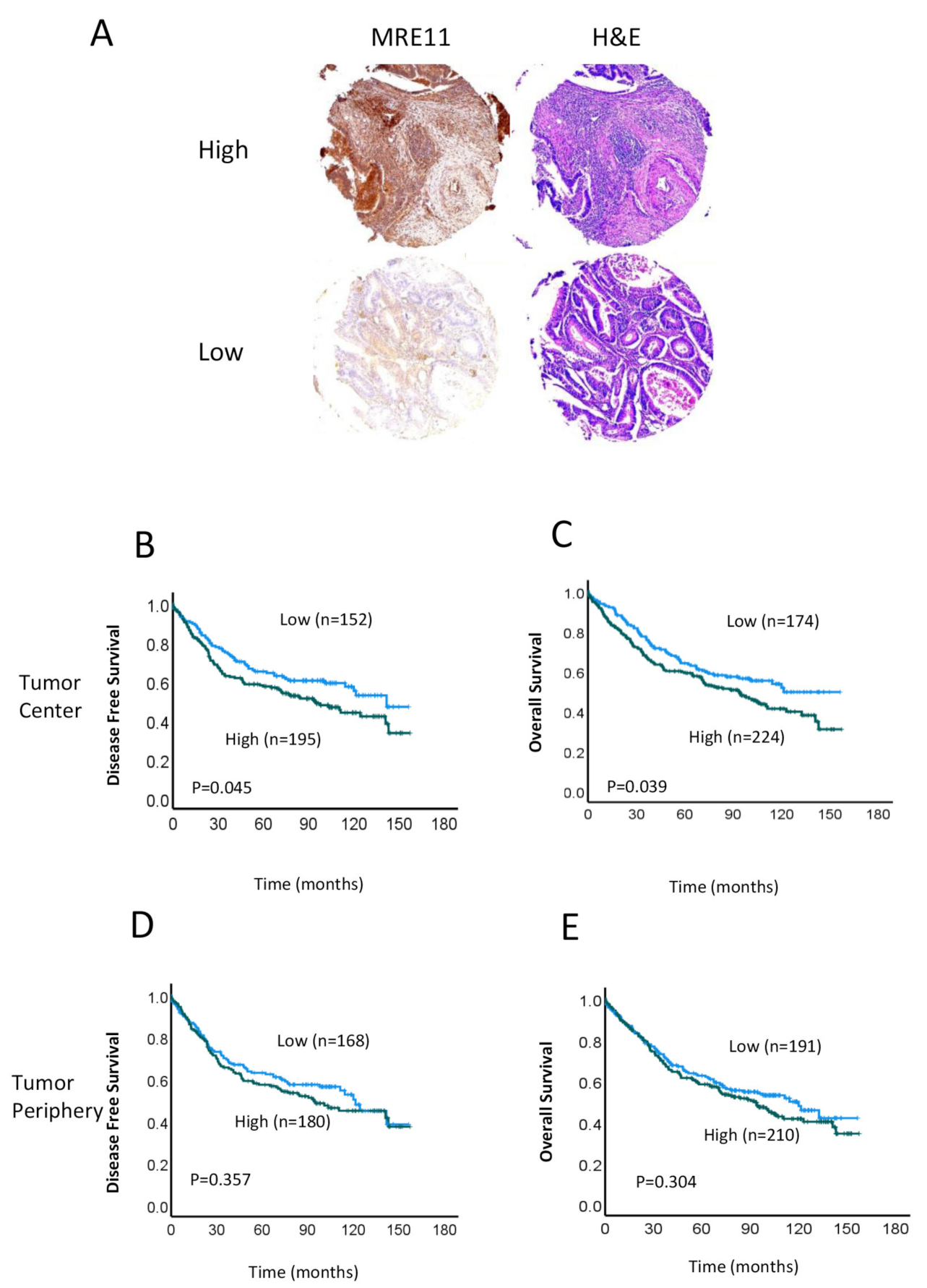
3.2. Association between MRE11 Expression and Clinicopathological Features and Prognosis
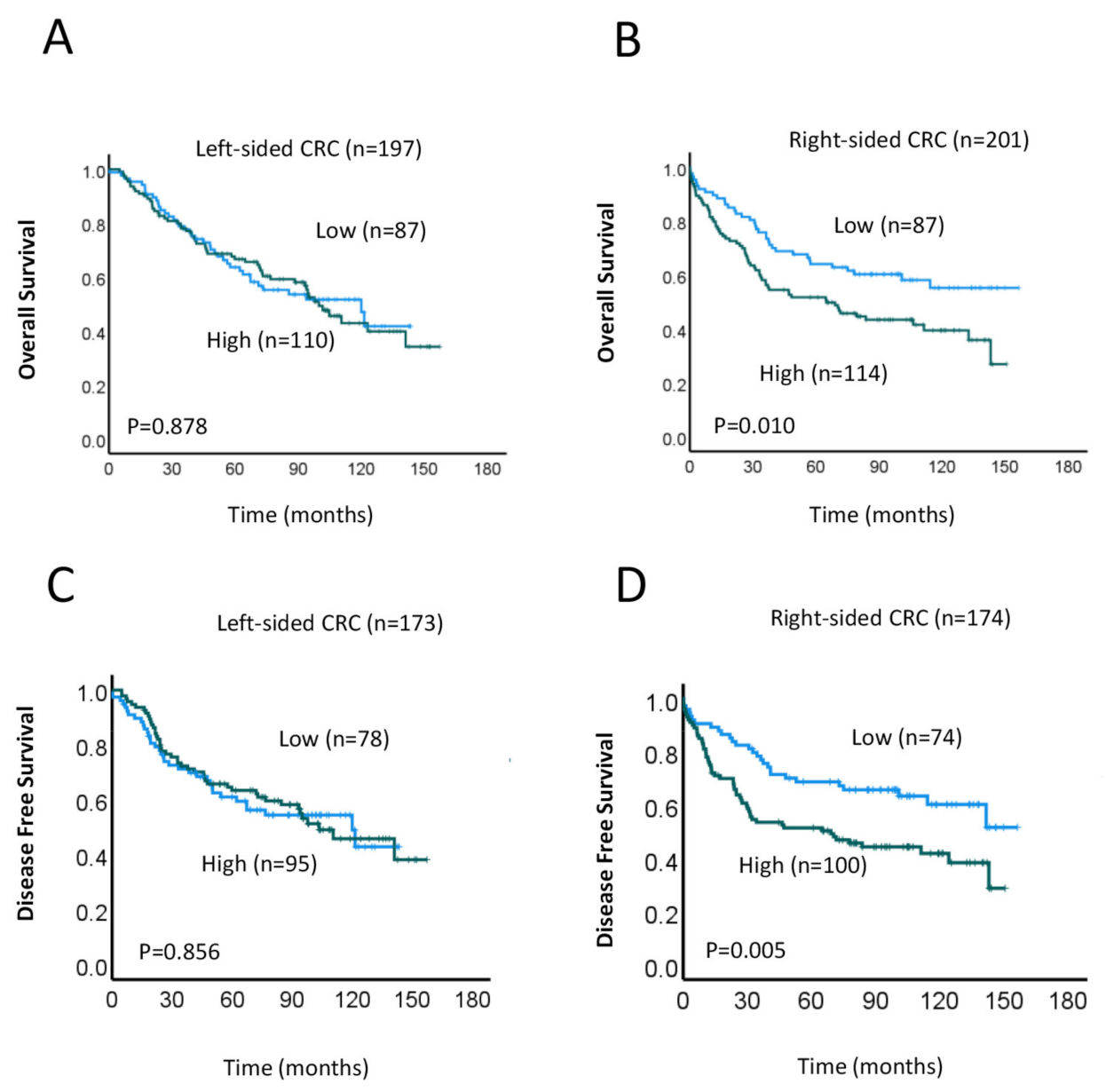
3.3. Correlation between MRE11 Expression and Survival Outcomes Based on CRC Location
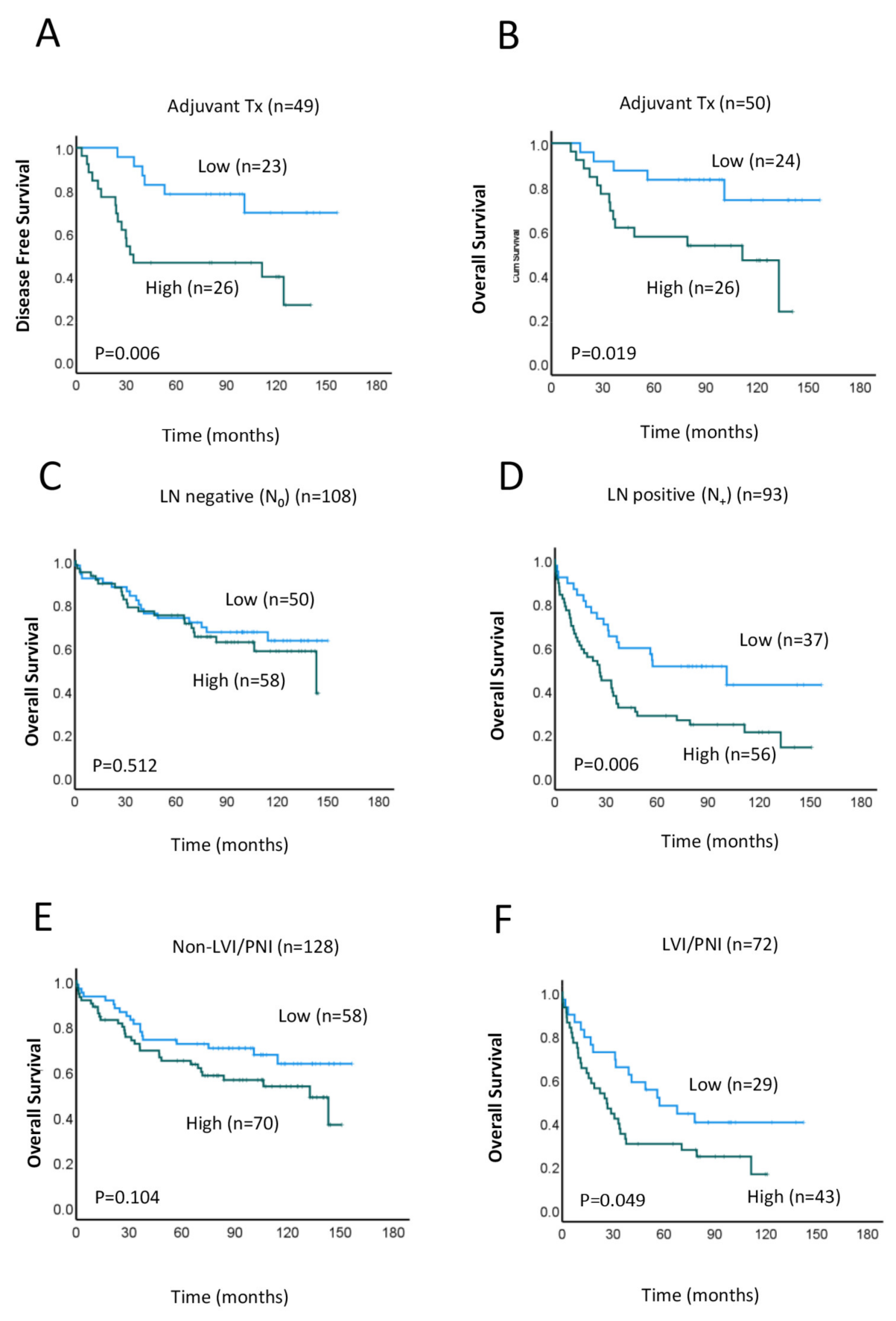
3.4. Prognostic Implications of MRE11 Expression in Right-Sided CRC Subgroups
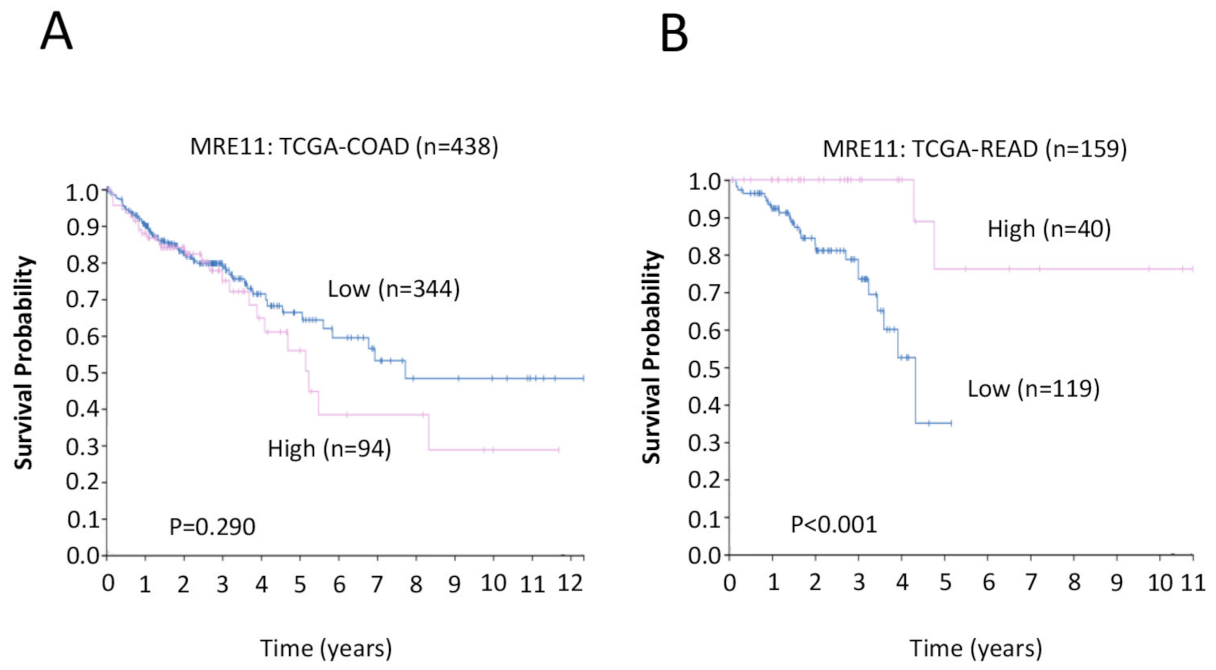
3.5. Clinical Significance of MRE11 in CRC
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA A Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Siegel, R.L.; Torre, L.A.; Soerjomataram, I.; Hayes, R.B.; Bray, F.; Weber, T.K.; Jemal, A. Global Patterns and Trends in Colorectal Cancer Incidence in Young Adults. Gut 2019, 68, 2179–2185. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer Statistics. CA Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef]
- Dayde, D.; Tanaka, I.; Jain, R.; Tai, M.C.; Taguchi, A. Predictive and Prognostic Molecular Biomarkers for Response to Neoadjuvant Chemoradiation in Rectal Cancer. Int. J. Mol. Sci. 2017, 18, 573. [Google Scholar] [CrossRef] [PubMed]
- Peluso, G.; Incollingo, P.; Calogero, A.; Tammaro, V.; Rupealta, N.; Chiacchio, G.; Sandoval Sotelo, M.L.; Minieri, G.; Pisani, A.; Riccio, E.; et al. Current Tissue Molecular Markers in Colorectal Cancer: A Literature Review. Biomed. Res. Int. 2017, 2017, 2605628. [Google Scholar] [CrossRef] [PubMed]
- Yoo, B.C.; Yeo, S.-G. Clinical Utility of Pretreatment Prediction of Chemoradiotherapy Response in Rectal Cancer: A Review. EPMA J. 2017, 8, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Bottarelli, L.; de’ Angelis, G.L.; Azzoni, C.; Mario, F.D.; de’ Angelis, N.; Leandro, G.; Fornaroli, F.; Gaiani, F.; Negri, F. Potential Predictive Biomarkers in Locally Advanced Rectal Cancer Treated with Preoperative Chemo-Radiotherapy. Acta Biomed. 2018, 89, 102–106. [Google Scholar] [CrossRef]
- Vacante, M.; Borzì, A.M.; Basile, F.; Biondi, A. Biomarkers in Colorectal Cancer: Current Clinical Utility and Future Perspectives. World J. Clin. Cases 2018, 6, 869–881. [Google Scholar] [CrossRef]
- Tomasini, P.P.; Guecheva, T.N.; Leguisamo, N.M.; Péricart, S.; Brunac, A.-C.; Hoffmann, J.S.; Saffi, J. Analyzing the Opportunities to Target DNA Double-Strand Breaks Repair and Replicative Stress Responses to Improve Therapeutic Index of Colorectal Cancer. Cancers 2021, 13, 3130. [Google Scholar] [CrossRef] [PubMed]
- Jackson, S.P.; Bartek, J. The DNA-Damage Response in Human Biology and Disease. Nature 2009, 461, 1071–1078. [Google Scholar] [CrossRef]
- Pećina-Šlaus, N.; Kafka, A.; Salamon, I.; Bukovac, A. Mismatch Repair Pathway, Genome Stability and Cancer. Front. Mol. Biosci. 2020, 7, 122. [Google Scholar] [CrossRef]
- French, A.J.; Sargent, D.J.; Burgart, L.J.; Foster, N.R.; Kabat, B.F.; Goldberg, R.; Shepherd, L.; Windschitl, H.E.; Thibodeau, S.N. Prognostic Significance of Defective Mismatch Repair and BRAF V600E in Patients with Colon Cancer. Clin. Cancer Res. 2008, 14, 3408–3415. [Google Scholar] [CrossRef]
- Tennstedt, P.; Fresow, R.; Simon, R.; Marx, A.; Terracciano, L.; Petersen, C.; Sauter, G.; Dikomey, E.; Borgmann, K. RAD51 Overexpression Is a Negative Prognostic Marker for Colorectal Adenocarcinoma. Int. J. Cancer 2013, 132, 2118–2126. [Google Scholar] [CrossRef]
- Ho, V.; Chung, L.; Singh, A.; Lea, V.; Revoltar, M.; Lim, S.H.; Tut, T.-G.; Ng, W.; Lee, M.; De Souza, P.; et al. Early Postoperative Low Expression of RAD50 in Rectal Cancer Patients Associates with Disease-Free Survival. Cancers 2017, 9, 163. [Google Scholar] [CrossRef] [PubMed]
- Ho, V.; Chung, L.; Singh, A.; Lea, V.; Abubakar, A.; Lim, S.H.; Chua, W.; Ng, W.; Lee, M.; Roberts, T.L.; et al. Aberrant Expression of RAD52, Its Prognostic Impact in Rectal Cancer and Association with Poor Survival of Patients. Int. J. Mol. Sci. 2020, 21, 1768. [Google Scholar] [CrossRef]
- Hestetun, K.E.; Aasebø, K.; Rosenlund, N.B.; Müller, Y.; Dahl, O.; Myklebust, M.P. Mismatch Repair Phenotype Determines the Implications of Tumor Grade and CDX2 Expression in Stage II–III Colon Cancer. Mod. Pathol. 2021, 34, 161–170. [Google Scholar] [CrossRef] [PubMed]
- Ho, V.; Chung, L.; Lim, S.H.; Ma, Y.; Wang, B.; Lea, V.; Abubakar, A.; Ng, W.; Lee, M.; Roberts, T.L.; et al. Prognostic Impact of TP53 Mutations and Tumor Mutational Load in Colorectal Cancer. Gastrointest. Disord. 2022, 4, 165–179. [Google Scholar] [CrossRef]
- Mladenov, E.; Magin, S.; Soni, A.; Iliakis, G. DNA Double-Strand Break Repair as Determinant of Cellular Radiosensitivity to Killing and Target in Radiation Therapy. Front. Oncol. 2013, 3, 113. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, M.; Kastan, M.B. The DNA Damage Response: Implications for Tumor Responses to Radiation and Chemotherapy. Annu. Rev. Med. 2015, 66, 129–143. [Google Scholar] [CrossRef]
- Van den Bosch, M.; Bree, R.T.; Lowndes, N.F. The MRN Complex: Coordinating and Mediating the Response to Broken Chromosomes. EMBO Rep. 2003, 4, 844–849. [Google Scholar] [CrossRef]
- Shiloh, Y. The ATM-Mediated DNA-Damage Response: Taking Shape. Trends Biochem. Sci. 2006, 31, 402–410. [Google Scholar] [CrossRef] [PubMed]
- Lavin, M.F.; Kozlov, S.; Gatei, M.; Kijas, A.W. ATM-Dependent Phosphorylation of All Three Members of the MRN Complex: From Sensor to Adaptor. Biomolecules 2015, 5, 2877–2902. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.C.; Padget, K.; Curtis, H.; Cowell, I.G.; Moiani, D.; Sondka, Z.; Morris, N.J.; Jackson, G.H.; Cockell, S.J.; Tainer, J.A.; et al. MRE11 Facilitates the Removal of Human Topoisomerase II Complexes from Genomic DNA. Biol. Open 2012, 1, 863–873. [Google Scholar] [CrossRef] [PubMed]
- Dmitrieva, N.I.; Malide, D.; Burg, M.B. Mre11 Is Expressed in Mammalian Mitochondria Where It Binds to Mitochondrial DNA. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2011, 301, R632–R640. [Google Scholar] [CrossRef] [PubMed]
- Rashid, S.; Freitas, M.O.; Cucchi, D.; Bridge, G.; Yao, Z.; Gay, L.; Williams, M.; Wang, J.; Suraweera, N.; Silver, A.; et al. MLH1 Deficiency Leads to Deregulated Mitochondrial Metabolism. Cell Death Dis. 2019, 10, 795. [Google Scholar] [CrossRef] [PubMed]
- Situ, Y.; Chung, L.; Lee, C.S.; Ho, V. MRN (MRE11-RAD50-NBS1) Complex in Human Cancer and Prognostic Implications in Colorectal Cancer. Int. J. Mol. Sci. 2019, 20, 816. [Google Scholar] [CrossRef] [PubMed]
- Pavelitz, T.; Renfro, L.; Foster, N.R.; Caracol, A.; Welsch, P.; Lao, V.V.; Grady, W.B.; Niedzwiecki, D.; Saltz, L.B.; Bertagnolli, M.M.; et al. MRE11-Deficiency Associated with Improved Long-Term Disease Free Survival and Overall Survival in a Subset of Stage III Colon Cancer Patients in Randomized CALGB 89803 Trial. PLoS ONE 2014, 9, e108483. [Google Scholar] [CrossRef]
- Ho, V.; Chung, L.; Revoltar, M.; Lim, S.H.; Tut, T.-G.; Abubakar, A.; Henderson, C.J.; Chua, W.; Ng, W.; Lee, M.; et al. MRE11 and ATM Expression Levels Predict Rectal Cancer Survival and Their Association with Radiotherapy Response. PLoS ONE 2016, 11, e0167675. [Google Scholar] [CrossRef] [PubMed]
- Ho, V.; Chung, L.; Singh, A.; Lea, V.; Abubakar, A.; Lim, S.H.; Ng, W.; Lee, M.; de Souza, P.; Shin, J.-S.; et al. Overexpression of the MRE11-RAD50-NBS1 (MRN) Complex in Rectal Cancer Correlates with Poor Response to Neoadjuvant Radiotherapy and Prognosis. BMC Cancer 2018, 18, 869. [Google Scholar] [CrossRef]
- Ionov, Y.; Peinado, M.A.; Malkhosyan, S.; Shibata, D.; Perucho, M. Ubiquitous Somatic Mutations in Simple Repeated Sequences Reveal a New Mechanism for Colonic Carcinogenesis. Nature 1993, 363, 558–561. [Google Scholar] [CrossRef]
- Peltomäki, P. Deficient DNA Mismatch Repair: A Common Etiologic Factor for Colon Cancer. Hum. Mol. Genet. 2001, 10, 735–740. [Google Scholar] [CrossRef]
- Sinicrope, F.A.; Foster, N.R.; Thibodeau, S.N.; Marsoni, S.; Monges, G.; Labianca, R.; Kim, G.P.; Yothers, G.; Allegra, C.; Moore, M.J.; et al. DNA Mismatch Repair Status and Colon Cancer Recurrence and Survival in Clinical Trials of 5-Fluorouracil-Based Adjuvant Therapy. J. Natl. Cancer Inst. 2011, 103, 863–875. [Google Scholar] [CrossRef] [PubMed]
- Le, D.T.; Uram, J.N.; Wang, H.; Bartlett, B.R.; Kemberling, H.; Eyring, A.D.; Skora, A.D.; Luber, B.S.; Azad, N.S.; Laheru, D.; et al. PD-1 Blockade in Tumors with Mismatch-Repair Deficiency. N. Engl. J. Med. 2015, 372, 2509–2520. [Google Scholar] [CrossRef] [PubMed]
- Sinicrope, F.A.; Shi, Q.; Allegra, C.J.; Smyrk, T.C.; Thibodeau, S.N.; Goldberg, R.M.; Meyers, J.P.; Pogue-Geile, K.L.; Yothers, G.; Sargent, D.J.; et al. Association of DNA Mismatch Repair and Mutations in BRAF and KRAS With Survival After Recurrence in Stage III Colon Cancers: A Secondary Analysis of 2 Randomized Clinical Trials. JAMA Oncol. 2017, 3, 472–480. [Google Scholar] [CrossRef] [PubMed]
- Du, F.; Liu, Y. Predictive Molecular Markers for the Treatment with Immune CheckpoInt. Inhibitors in Colorectal Cancer. J. Clin. Lab. Anal. 2022, 36, e24141. [Google Scholar] [CrossRef] [PubMed]
- Giannini, G.; Ristori, E.; Cerignoli, F.; Rinaldi, C.; Zani, M.; Viel, A.; Ottini, L.; Crescenzi, M.; Martinotti, S.; Bignami, M.; et al. Human MRE11 Is Inactivated in Mismatch Repair-Deficient Cancers. EMBO Rep. 2002, 3, 248–254. [Google Scholar] [CrossRef] [PubMed]
- Ottini, L.; Falchetti, M.; Saieva, C.; De Marco, M.; Masala, G.; Zanna, I.; Paglierani, M.; Giannini, G.; Gulino, A.; Nesi, G.; et al. MRE11 Expression Is Impaired in Gastric Cancer with Microsatellite Instability. Carcinogenesis 2004, 25, 2337–2343. [Google Scholar] [CrossRef] [PubMed]
- Miquel, C.; Jacob, S.; Grandjouan, S.; Aimé, A.; Viguier, J.; Sabourin, J.-C.; Sarasin, A.; Duval, A.; Praz, F. Frequent Alteration of DNA Damage Signalling and Repair Pathways in Human Colorectal Cancers with Microsatellite Instability. Oncogene 2007, 26, 5919–5926. [Google Scholar] [CrossRef] [PubMed]
- Bufill, J.A. Colorectal Cancer: Evidence for Distinct Genetic Categories Based on Proximal or Distal Tumor Location. Ann. Intern. Med. 1990, 113, 779–788. [Google Scholar] [CrossRef] [PubMed]
- Gervaz, P.; Bucher, P.; Morel, P. Two Colons-Two Cancers: Paradigm Shift and Clinical Implications. J. Surg. Oncol. 2004, 88, 261–266. [Google Scholar] [CrossRef]
- Shen, H.; Yang, J.; Huang, Q.; Jiang, M.-J.; Tan, Y.-N.; Fu, J.-F.; Zhu, L.-Z.; Fang, X.-F.; Yuan, Y. Different Treatment Strategies and Molecular FeatuRes. between Right-Sided and Left-Sided Colon Cancers. World J. Gastroenterol. 2015, 21, 6470–6478. [Google Scholar] [CrossRef] [PubMed]
- Jung, M.-K.; Shin, U.S.; Ki, Y.-J.; Kim, Y.-B.; Moon, S.-M.; Sung, S.-J. Is the Location of the Tumor Another Prognostic Factor for Patients with Colon Cancer? Ann. Coloproctol. 2017, 33, 210–218. [Google Scholar] [CrossRef] [PubMed]
- Baran, B.; Mert Ozupek, N.; Yerli Tetik, N.; Acar, E.; Bekcioglu, O.; Baskin, Y. Difference Between Left-Sided and Right-Sided Colorectal Cancer: A Focused Review of Literature. Gastroenterol. Res. 2018, 11, 264–273. [Google Scholar] [CrossRef] [PubMed]
- Yuan, S.-S.F.; Hou, M.-F.; Hsieh, Y.-C.; Huang, C.-Y.; Lee, Y.-C.; Chen, Y.-J.; Lo, S. Role of MRE11 in Cell Proliferation, Tumor Invasion, and DNA Repair in Breast Cancer. J. Natl. Cancer Inst. 2012, 104, 1485–1502. [Google Scholar] [CrossRef]
- Fan, C.-W.; Kopsida, M.; Liu, Y.-B.; Zhang, H.; Gao, J.-F.; Arbman, G.; Cao, S.-Y.-W.; Li, Y.; Zhou, Z.-G.; Sun, X.-F. Prognostic Heterogeneity of MRE11 Based on the Location of Primary Colorectal Cancer Is Caused by Activation of Different Immune Signals. Front. Oncol. 2020, 9, 1465. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.-Y.; Chen, Y.-K.; Lo, S.; Chi, T.-C.; Chen, Y.-H.; Hu, S.C.-S.; Chen, Y.-W.; Jiang, S.S.; Tsai, F.-Y.; Liu, W.; et al. MRE11 Promotes Oral Cancer Progression through RUNX2/CXCR4/AKT/FOXA2 Signaling in a Nuclease-Independent Manner. Oncogene 2021, 40, 3510–3532. [Google Scholar] [CrossRef]
- Horak, J.; Dolnikova, A.; Cumaogullari, O.; Cumova, A.; Navvabi, N.; Vodickova, L.; Levy, M.; Schneiderova, M.; Liska, V.; Andera, L.; et al. MiR-140 Leads to MRE11 Downregulation and Ameliorates Oxaliplatin Treatment and Therapy Response in Colorectal Cancer Patients. Front. Oncol. 2022, 12, 959407. [Google Scholar] [CrossRef] [PubMed]
- Sheridan, J.; Tosetto, M.; Gorman, J.; O’Donoghue, D.; Sheahan, K.; Hyland, J.; Mulcahy, H.; Gibbons, D.; O’Sullivan, J. Effects of Radiation on Levels of DNA Damage in Normal Non-Adjacent Mucosa from Colorectal Cancer Cases. J. Gastrointest Cancer 2013, 44, 41–45. [Google Scholar] [CrossRef]
- Glebov, O.K.; Rodriguez, L.M.; Nakahara, K.; Jenkins, J.; Cliatt, J.; Humbyrd, C.-J.; DeNobile, J.; Soballe, P.; Simon, R.; Wright, G.; et al. Distinguishing Right from Left Colon by the Pattern of Gene Expression. Cancer Epidemiol. Biomark. Prev. 2003, 12, 755–762. [Google Scholar]
- Muzny, D.M.; Bainbridge, M.N.; Chang, K.; Dinh, H.H.; Drummond, J.A.; Fowler, G.; Kovar, C.L.; Lewis, L.R.; Morgan, M.B.; Newsham, I.F.; et al. Comprehensive Molecular Characterization of Human Colon and Rectal Cancer. Nature 2012, 487, 330–337. [Google Scholar] [CrossRef]
- Koestler, D.C.; Li, J.; Baron, J.A.; Tsongalis, G.J.; Butterly, L.F.; Goodrich, M.; Lesseur, C.; Karagas, M.R.; Marsit, C.J.; Moore, J.H.; et al. Distinct Patterns of DNA Methylation in Conventional Adenomas Involving the Right and Left Colon. Mod. Pathol. 2014, 27, 145–155. [Google Scholar] [CrossRef] [PubMed]
- Missiaglia, E.; Jacobs, B.; D’Ario, G.; Di Narzo, A.F.; Soneson, C.; Budinska, E.; Popovici, V.; Vecchione, L.; Gerster, S.; Yan, P.; et al. Distal and Proximal Colon Cancers Differ in Terms of Molecular, Pathological, and Clinical Features. Ann. Oncol. 2014, 25, 1995–2001. [Google Scholar] [CrossRef] [PubMed]
- Brulé, S.Y.; Jonker, D.J.; Karapetis, C.S.; O’Callaghan, C.J.; Moore, M.J.; Wong, R.; Tebbutt, N.C.; Underhill, C.; Yip, D.; Zalcberg, J.R.; et al. Location of Colon Cancer (Right-Sided versus Left-Sided) as a Prognostic Factor and a Predictor of Benefit from Cetuximab in NCIC CO.17. Eur. J. Cancer 2015, 51, 1405–1414. [Google Scholar] [CrossRef] [PubMed]
- Vo, A.T.; Zhu, F.; Wu, X.; Yuan, F.; Gao, Y.; Gu, L.; Li, G.-M.; Lee, T.-H.; Her, C. HMRE11 Deficiency Leads to Microsatellite Instability and Defective DNA Mismatch Repair. EMBO Rep. 2005, 6, 438–444. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Zhang, H.; Arbman, G.; Sun, X.-F. RAD50/MRE11/NBS1 Proteins in Relation to Tumour Development and Prognosis in Patients with Microsatellite Stable Colorectal Cancer. Histol. HistoPathol. 2008, 23, 1495–1502. [Google Scholar] [CrossRef]
| Characteristics | All Patients (n = 408) | % |
|---|---|---|
| Age median | 70 (23–96 years) | |
| <70 | 190 | 46.6 |
| ≥70 | 218 | 53.4 |
| Sex | ||
| Male | 219 | 53.7 |
| Female | 189 | 46.3 |
| Tumor stage | ||
| T1, T2 | 81 | 19.9 |
| T3, T4 | 327 | 80.1 |
| Node stage | ||
| N0 | 213 | 52.2 |
| N1, N2 | 195 | 47.8 |
| Metastasis stage | ||
| M0 | 353 | 86.5 |
| M1 | 55 | 13.5 |
| Differentiation | ||
| Well/moderate | 337 | 82.5 |
| Poor | 71 | 17.5 |
| LVI/PNI | ||
| Absent | 265 | 65 |
| Present | 143 | 35 |
| Primary tumor site (Right/Left) | ||
| Right | 209 | 51.2 |
| Left | 199 | 48.8 |
| Treatment | ||
| Neoadjuvant therapy | ||
| No | 392 | 96.1 |
| Yes | 16 | 3.9 |
| Adjuvant therapy | ||
| No | 281 | 68.9 |
| Yes | 127 | 31.1 |
| MMR deficiency | ||
| Total | 87 | 21.3 (87/408) |
| No | 64 | 73.6 |
| Yes | 23 | 26.4 |
| Tumor Centre | Tumor Periphery | ||||||
|---|---|---|---|---|---|---|---|
| Low (%) | High (%) | p-Value | Low (%) | High (%) | p-Value | ||
| Sex | Male | 53.4 | 54.0 | 0.920 | 54.5 | 51.9 | 0.618 |
| Female | 46.6 | 46.0 | 45.5 | 48.1 | |||
| Age | <70 | 44.8 | 47.3 | 0.685 | 46.1 | 44.3 | 0.719 |
| ≥70 | 55.2 | 52.7 | 53.9 | 55.7 | |||
| Tumor stage | T1–2 | 24.1 | 30.0 | 0.172 | 20.9 | 21.0 | 0.998 |
| T3–4 | 75.9 | 70.0 | 79.1 | 79.0 | |||
| Node stage | Negative | 55.7 | 49.6 | 0.227 | 51.8 | 51.9 | 0.988 |
| Positive | 44.3 | 50.4 | 48.2 | 48.1 | |||
| Metastasis stage | M0 | 87.4 | 87.1 | 0.929 | 88.0 | 85.7 | 0.508 |
| M1 | 12.6 | 12.9 | 12.0 | 14.3 | |||
| Differentiation | Well/moderate | 83.3 | 82.1 | 0.756 | 82.2 | 82.4 | 0.962 |
| Poor | 16.7 | 17.9 | 17.8 | 17.6 | |||
| LVI/PNI | Absent | 67.8 | 62.8 | 0.297 | 63.2 | 66.2 | 0.562 |
| Present | 32.2 | 37.2 | 36.8 | 33.8 | |||
| Adjuvant therapy | No | 62.1 | 65.3 | 0.535 | 63.3 | 65.2 | 0.714 |
| Yes | 37.9 | 34.7 | 36.7 | 34.8 | |||
| Neoadjuvant therapy | No | 95.4 | 96.4 | 0.605 | 94.8 | 97.6 | 0.132 |
| Yes | 4.6 | 3.6 | 5.2 | 2.4 | |||
| MLH1 a | Normal IHC | 97.6 | 97.8 | 0.961 | 100 | 97.1 | 0.209 |
| Loss of staining | 2.4 | 2.2 | 0 | 2.9 | |||
| MSH2 | Normal IHC | 95.2 | 97.7 | 0.529 | 98.1 | 97 | 0.732 |
| Loss of staining | 4.8 | 2.3 | 1.9 | 3 | |||
| MSH6 | Normal IHC | 71.4 | 84.1 | 0.157 | 73.6 | 84.8 | 0.221 |
| Loss of staining | 28.6 | 15.9 | 26.4 | 15.2 | |||
| PMS2 | Normal IHC | 76.9 | 88.1 | 0.184 | 75 | 93.8 | 0.031 |
| Loss of staining | 23.1 | 11.9 | 25 | 6.2 | |||
| dMMR b | No | 64.3 | 80 | 0.101 | 69.8 | 79.4 | 0.322 |
| Yes | 35.7 | 20 | 30.2 | 20.6 | |||
| Univariate | Multivariate | ||||||
|---|---|---|---|---|---|---|---|
| n (%) | HR | 95% CI | p-Value | HR | 95% CI | p-Value | |
| MRE11 TC a | |||||||
| High | 54.9 | 1.352 | 1.015–1.801 | 0.040 | 1.433 | 1.026–2.002 | 0.035 |
| Low | 45.1 | ||||||
| Sex | |||||||
| Male | 53.7 | 1.19 | 0.905–1.565 | 0.214 | 0.912 | 0.651–1.267 | 0.584 |
| Female | 46.3 | ||||||
| Age | |||||||
| <70 | 46.6 | 1.828 | 1.375–2.401 | <0.001 | 2.314 | 1.576–3.396 | <0.001 |
| ≥70 | 53.4 | ||||||
| Tumor stage | |||||||
| T1, T2 | 19.9 | 2.103 | 1.393–3.173 | <0.001 | 1.292 | 0.807–2.070 | 0.286 |
| T3, T4 | 80.1 | ||||||
| Node stage | |||||||
| Negative | 52.2 | 2.286 | 1.727–3.027 | <0.001 | 3.379 | 2.263–5.047 | <0.001 |
| Positive | 47.8 | ||||||
| Metastasis stage | |||||||
| M0 | 86.5 | 5.831 | 4.173–8.150 | <0.001 | 2.747 | 0.370–20.367 | 0.323 |
| M1 | 13.5 | ||||||
| Differentiation | |||||||
| Well/moderate | 82.5 | 1.564 | 1.119–2.186 | 0.009 | 1.343 | 0.648–2.782 | 0.427 |
| Poor | 17.5 | ||||||
| LVI/PNI | |||||||
| Absent | 65 | 1.965 | 1.488–2.594 | <0.001 | 1.339 | 1.314–4.075 | 0.112 |
| Present | 35 | ||||||
| Adjuvant therapy | |||||||
| No | 68.9 | 0.603 | 0.404–0.806 | 0.005 | 0.288 | 0.184–0.451 | <0.001 |
| Yes | 31.1 | ||||||
| Neoadjuvant therapy | |||||||
| No | 96.1 | 1.049 | 0.538–2.048 | 0.888 | 2.207 | 0.996–4.888 | 0.151 |
| Yes | 3.9 | ||||||
| Right-Sided CRC | |||
|---|---|---|---|
| HR | 95% CI | p-Value | |
| MRE11 | |||
| High | 1.697 | 1.034–2.785 | 0.036 |
| Low | |||
| Sex | |||
| Male | 0.882 | 0.546–1.417 | 0.598 |
| Female | |||
| Age | |||
| <70 | 2.114 | 1.213–3.685 | <0.001 |
| ≥70 | |||
| Tumor stage | |||
| T1, T2 | 0.976 | 0.487–1.955 | 0.944 |
| T3, T4 | |||
| Node stage | |||
| Negative | 3.876 | 2.237–6.716 | <0.001 |
| Positive | |||
| Metastasis stage | |||
| M0 | 6.65 | 0.786–16.95 | 0.082 |
| M1 | |||
| Differentiation | |||
| Well/moderate | 1.479 | 0.848–2.581 | 0.168 |
| Poor | |||
| LVI/PNI | |||
| Absent | 1.922 | 1.122–3.293 | 0.017 |
| Present | |||
| Adjuvant therapy | |||
| No | 0.292 | 0.154–0.565 | <0.001 |
| Yes | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ho, V.; Chung, L.; Wilkinson, K.; Lea, V.; Lim, S.H.; Abubakar, A.; Ng, W.; Lee, M.; Roberts, T.L.; Chua, W.; et al. Prognostic Significance of MRE11 Overexpression in Colorectal Cancer Patients. Cancers 2023, 15, 2438. https://doi.org/10.3390/cancers15092438
Ho V, Chung L, Wilkinson K, Lea V, Lim SH, Abubakar A, Ng W, Lee M, Roberts TL, Chua W, et al. Prognostic Significance of MRE11 Overexpression in Colorectal Cancer Patients. Cancers. 2023; 15(9):2438. https://doi.org/10.3390/cancers15092438
Chicago/Turabian StyleHo, Vincent, Liping Chung, Kate Wilkinson, Vivienne Lea, Stephanie H. Lim, Askar Abubakar, Weng Ng, Mark Lee, Tara L. Roberts, Wei Chua, and et al. 2023. "Prognostic Significance of MRE11 Overexpression in Colorectal Cancer Patients" Cancers 15, no. 9: 2438. https://doi.org/10.3390/cancers15092438
APA StyleHo, V., Chung, L., Wilkinson, K., Lea, V., Lim, S. H., Abubakar, A., Ng, W., Lee, M., Roberts, T. L., Chua, W., & Lee, C. S. (2023). Prognostic Significance of MRE11 Overexpression in Colorectal Cancer Patients. Cancers, 15(9), 2438. https://doi.org/10.3390/cancers15092438







