Tumor-Infiltrating CD45RO+ Memory Cells Are Associated with Favorable Prognosis in Oral Squamous Cell Carcinoma Patients
Abstract
Simple Summary
Abstract
1. Introduction
2. Material and Methods
2.1. Patients and Specimens
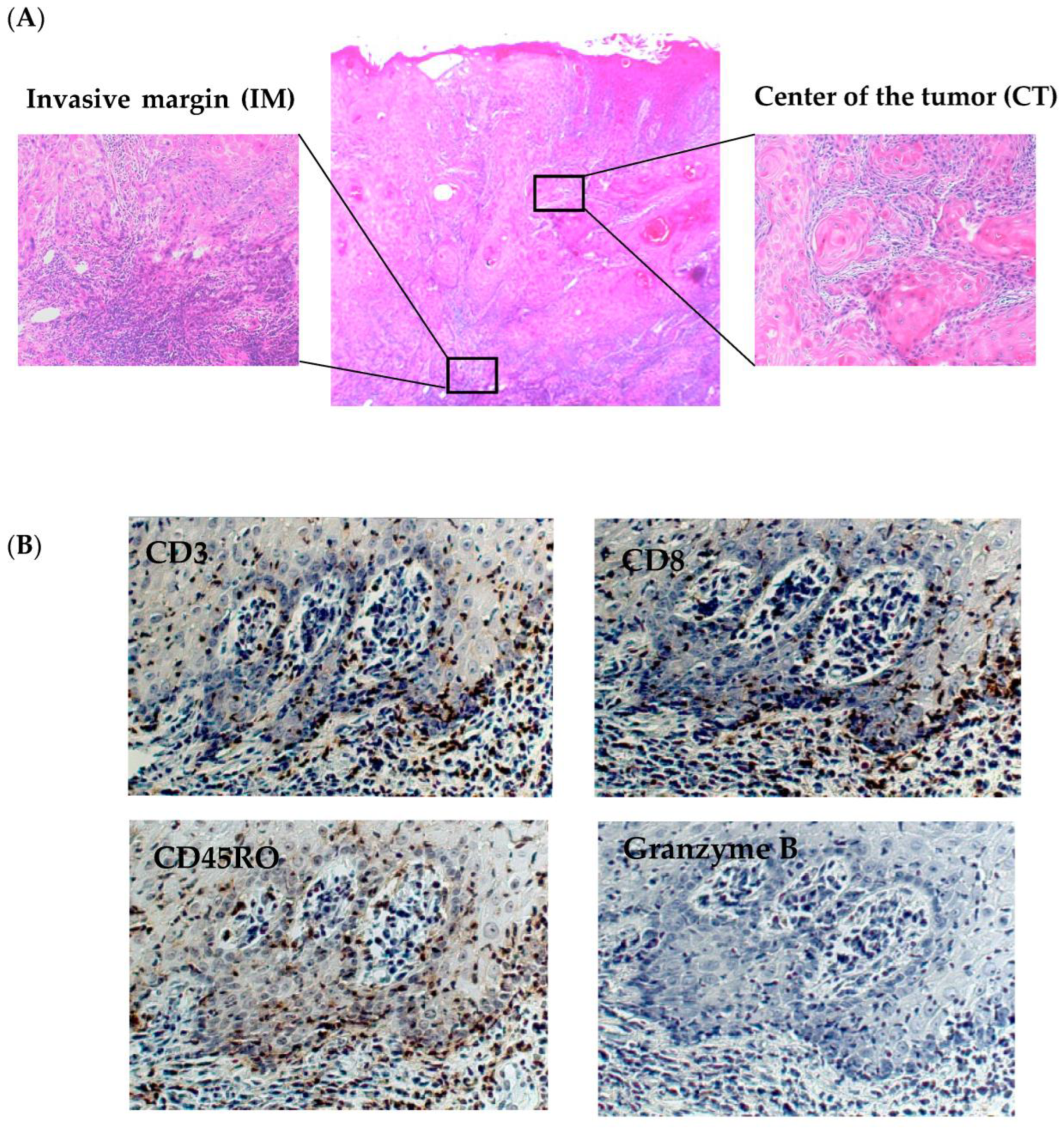
2.2. Immunohistochemical Analysis
2.3. Statistical Analysis
2.4. Ethical Considerations
3. Results
3.1. Clinicopathological Characteristics
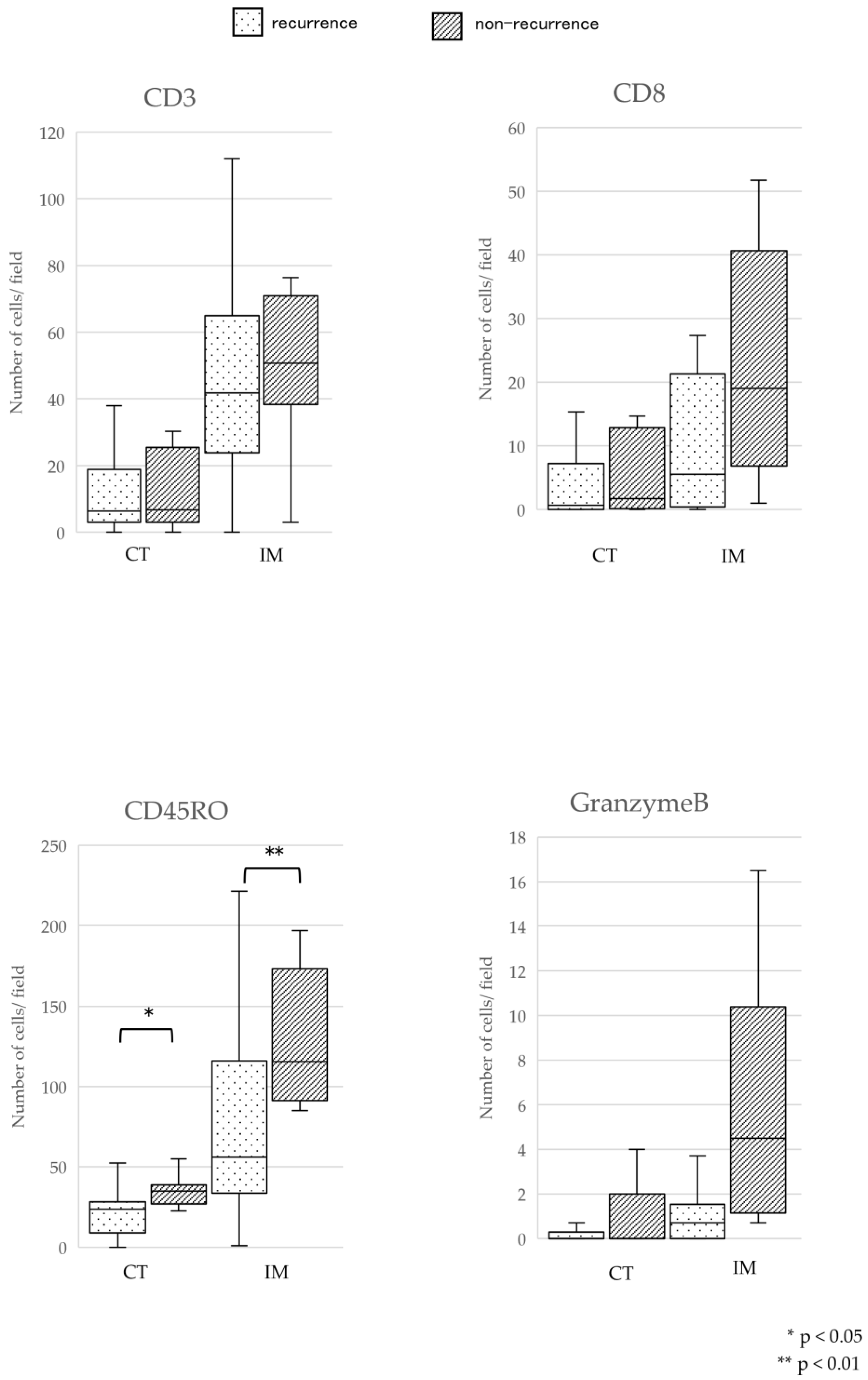
3.2. Comparison of TILs Density between Recurrence and Nonrecurrence Groups
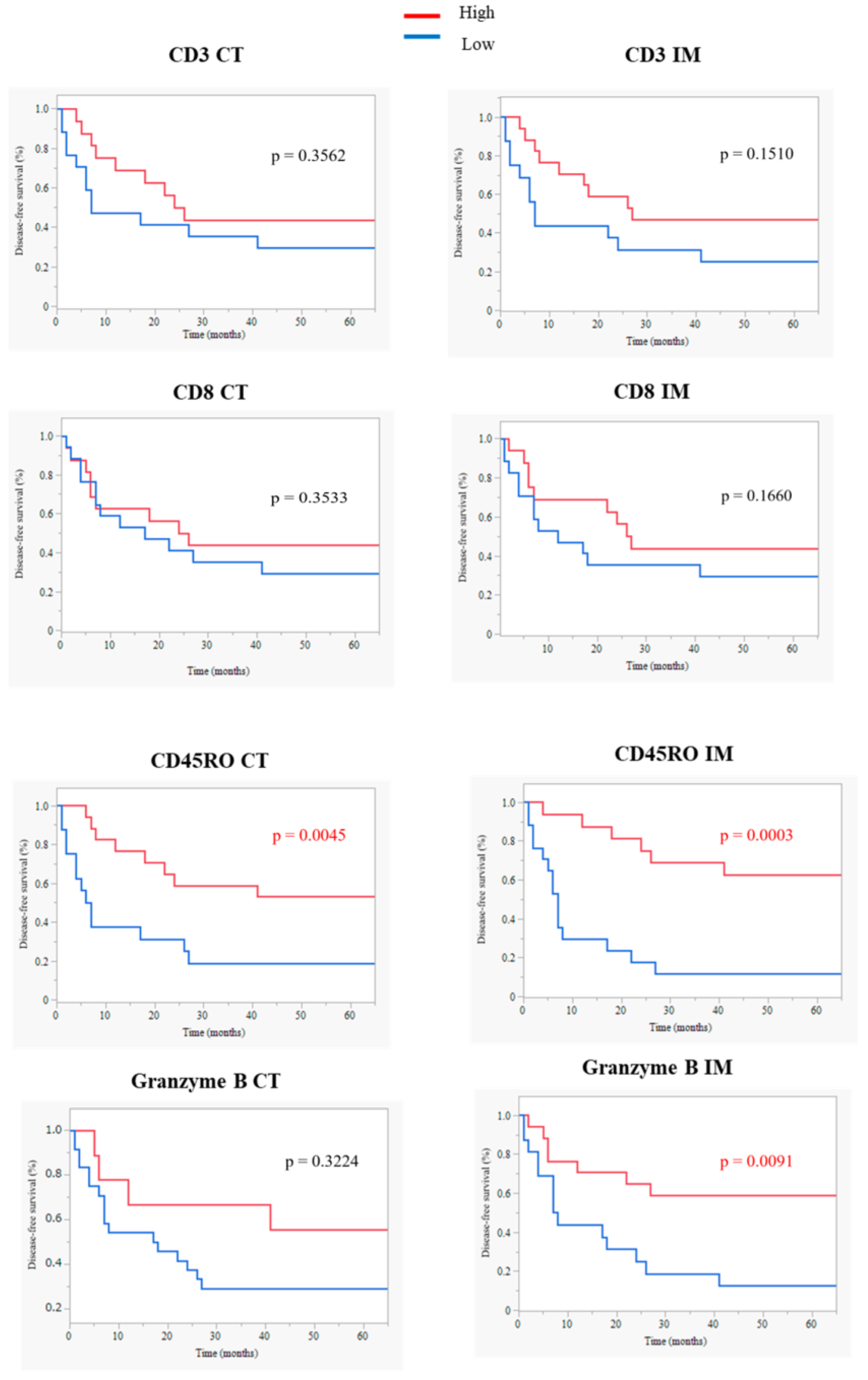
3.3. Comparison of DFS and OS Rates between the TILsHigh and TILsLow Groups
3.4. Comparison of Tumor MICA Expression Score between TILsHigh and TILsLow Groups
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hendry, S.; Salgado, R.; Gevaert, T.; Russell, P.A.; John, T.; Thapa, B.; Christie, M.; van de Vijver, K.; Estrada, M.V.; Gonzalez-Ericsson, P.I.; et al. Assessing Tumor-Infiltrating Lymphocytes in Solid Tumors: A Practical Review for Pathologists and Proposal for a Standardized Method from the International Immuno-Oncology Biomarkers Working Group: Part 2: TILs in Melanoma, Gastrointestinal Tract Carcinomas, Non-Small Cell Lung Carcinoma and Mesothelioma, Endometrial and Ovarian Carcinomas, Squamous Cell Carcinoma of the Head and Neck, Genitourinary Carcinomas, and Primary Brain Tumors. Adv. Anat. Pathol. 2017, 24, 311–335. [Google Scholar] [PubMed]
- Hanahan, D.; Weinberg, R.A. Hallmarks of cancer: The next generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef] [PubMed]
- Hu, G.; Wang, S. Tumor-infiltrating CD45RO(+) Memory T Lymphocytes Predict Favorable Clinical Outcome in Solid Tumors. Sci. Rep. 2017, 7, 10376. [Google Scholar] [CrossRef] [PubMed]
- Xu, Q.; Wang, C.; Yuan, X.; Feng, Z.; Han, Z. Prognostic Value of Tumor-Infiltrating Lymphocytes for Patients with Head and Neck Squamous Cell Carcinoma. Transl. Oncol. 2017, 10, 10–16. [Google Scholar] [CrossRef] [PubMed]
- Balermpas, P.; Michel, Y.; Wagenblast, J.; Seitz, O.; Weiss, C.; Rödel, F.; Rödel, C.; Fokas, E. Tumour-infiltrating lymphocytes predict response to definitive chemoradiotherapy in head and neck cancer. Br. J. Cancer 2014, 110, 501–509. [Google Scholar] [CrossRef]
- Nguyen, N.; Bellile, E.; Thomas, D.; McHugh, J.; Rozek, L.; Virani, S.; Peterson, L.; Carey, T.E.; Walline, H.; Moyer, J.; et al. Tumor infiltrating lymphocytes and survival in patients with head and neck squamous cell carcinoma. Head Neck 2016, 38, 1074–1084. [Google Scholar] [CrossRef]
- Zhou, C.; Li, J.; Wu, Y.; Diao, P.; Yang, J.; Cheng, J. High Density of Intratumor CD45RO(+) Memory Tumor-Infiltrating Lymphocytes Predicts Favorable Prognosis in Patients with Oral Squamous Cell Carcinoma. J. Oral Maxillofac. Surg. 2019, 77, 536–545. [Google Scholar] [CrossRef]
- Distel, L.V.; Fickenscher, R.; Dietel, K.; Hung, A.; Iro, H.; Zenk, J.; Nkenke, E.; Büttner, M.; Niedobitek, G.; Grabenbauer, G.G. Tumour infiltrating lymphocytes in squamous cell carcinoma of the oro- and hypopharynx: Prognostic impact may depend on type of treatment and stage of disease. Oral Oncol. 2009, 45, e167–e174. [Google Scholar] [CrossRef]
- Pretscher, D.; Distel, L.V.; Grabenbauer, G.G.; Wittlinger, M.; Buettner, M.; Niedobitek, G. Distribution of immune cells in head and neck cancer: CD8+ T-cells and CD20+ B-cells in metastatic lymph nodes are associated with favourable outcome in patients with oro- and hypopharyngeal carcinoma. BMC Cancer 2009, 9, 292. [Google Scholar] [CrossRef]
- Hu, Y.; He, M.Y.; Zhu, L.F.; Yang, C.C.; Zhou, M.L.; Wang, Q.; Zhang, W.; Zheng, Y.Y.; Wang, D.M.; Xu, Z.Q.; et al. Tumor-associated macrophages correlate with the clinicopathological features and poor outcomes via inducing epithelial to mesenchymal transition in oral squamous cell carcinoma. J. Exp. Clin. Cancer Res. 2016, 35, 12. [Google Scholar] [CrossRef]
- Zeromski, J.; Dworacki, G.; Kruk-Zagajewska, A.; Szmeja, Z.; Jezewska, E.; Kostecka, J. Assessment of immunophenotype of potentially cytotoxic tumor infiltrating cells in laryngeal carcinoma. Arch. Immunol. Ther. Exp. 1993, 41, 57–62. [Google Scholar]
- Dworacki, G.; Kruk-Zagajewska, A.; Jezewska, E.; Sikora, J.; Zeromski, J. Tumor infiltrating lymphocytes in HLA+ and HLA- laryngeal cancer--quantitative approach. Arch. Immunol. Ther. Exp. 1999, 47, 161–168. [Google Scholar]
- Ogino, T.; Shigyo, H.; Ishii, H.; Katayama, A.; Miyokawa, N.; Harabuchi, Y.; Ferrone, S. HLA class I antigen down-regulation in primary laryngeal squamous cell carcinoma lesions as a poor prognostic marker. Cancer Res. 2006, 66, 9281–9289. [Google Scholar] [CrossRef]
- Bahram, S.; Bresnahan, M.; Geraghty, D.E.; Spies, T. A second lineage of mammalian major histocompatibility complex class I genes. Proc. Natl. Acad. Sci. USA 1994, 91, 6259–6263. [Google Scholar] [CrossRef] [PubMed]
- Groh, V.; Bahram, S.; Bauer, S.; Herman, A.; Beauchamp, M.; Spies, T. Cell stress-regulated human major histocompatibility complex class I gene expressed in gastrointestinal epithelium. Proc. Natl. Acad. Sci. USA 1996, 93, 12445–12450. [Google Scholar] [CrossRef]
- Bauer, S.; Groh, V.; Wu, J.; Steinle, A.; Phillips, J.H.; Lanier, L.L.; Spies, T. Activation of NK cells and T cells by NKG2D, a receptor for stress-inducible MICA. Science 1999, 285, 727–729. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Song, Y.; Bakker, A.B.; Bauer, S.; Spies, T.; Lanier, L.L.; Phillips, J.H. An activating immunoreceptor complex formed by NKG2D and DAP10. Science 1999, 285, 730–732. [Google Scholar] [CrossRef] [PubMed]
- Kaech, S.M.; Hemby, S.; Kersh, E.; Ahmed, R. Molecular and functional profiling of memory CD8 T cell differentiation. Cell 2002, 111, 837–851. [Google Scholar] [CrossRef]
- Tani, R.; Ito, N.; Matsui, K.; Yamasaki, S.; Hamada, A.; Tokumaru, K.; Toratani, S.; Okamoto, T. MICA A5.1 homozygous genotype is associated with a risk for early-onset oral cancer. Oral Oncol. 2021, 116, 105256. [Google Scholar] [CrossRef]
- Higaki, M.; Shintani, T.; Hamada, A.; Rosli, S.N.Z.; Okamoto, T. Eldecalcitol (ED-71)-induced exosomal miR-6887-5p suppresses squamous cell carcinoma cell growth by targeting heparin-binding protein 17/fibroblast growth factor-binding protein-1 (HBp17/FGFBP-1). In Vitro Cell Dev Biol Anim. 2020, 56, 222–233. [Google Scholar] [CrossRef]
- Shintani, T.; Higaki, M.; Okamoto, T. Heparin-Binding Protein 17/Fibroblast Growth Factor-Binding Protein-1 Knockout Inhibits Proliferation and Induces Differentiation of Squamous Cell Carcinoma Cells. Cancers 2021, 13, 2684. [Google Scholar] [CrossRef] [PubMed]
- Begum, S.; Zhang, Y.; Shintani, T.; Toratani, S.; Sato, J.D.; Okamoto, T. Immunohistochemical expression of heparin-binding protein 17/fibroblast growth factor-binding protein-1 (HBp17/FGFBP-1) as an angiogenic factor in head and neck tumorigenesis. Oncol Rep. 2007, 17, 591–596. [Google Scholar] [CrossRef] [PubMed]
- Shintani, T.; Rosli, S.N.Z.; Takatsu, F.; Choon, Y.F.; Hayashido, Y.; Toratani, S.; Usui, E.; Okamoto, T. Eldecalcitol (ED-71), an analog of 1α,25-dihydroxyvitamin D3 as a potential anti-cancer agent for oral squamous cell carcinomas. J. Steroid Biochem Mol. Biol. 2016, 164, 79–84. [Google Scholar] [CrossRef]
- Sharma, P.; Shen, Y.; Wen, S.; Yamada, S.; Jungbluth, A.A.; Gnjatic, S.; Bajorin, D.F.; Reuter, V.E.; Herr, H.; Old, L.J.; et al. CD8 tumor-infiltrating lymphocytes are predictive of survival in muscle-invasive urothelial carcinoma. Proc. Natl. Acad. Sci. USA 2007, 104, 3967–3972. [Google Scholar] [CrossRef]
- Chatzopoulos, K.; Kotoula, V.; Manoussou, K.; Markou, K.; Vlachtsis, K.; Angouridakis, N.; Nikolaou, A.; Vassilakopoulou, M.; Psyrri, A.; Fountzilas, G. Tumor Infiltrating Lymphocytes and CD8+ T Cell Subsets as Prognostic Markers in Patients with Surgically Treated Laryngeal Squamous Cell Carcinoma. Head Neck Pathol. 2020, 14, 689–700. [Google Scholar] [CrossRef] [PubMed]
- Spector, M.E.; Bellile, E.; Amlani, L.; Zarins, K.; Smith, J.; Brenner, J.C.; Rozek, L.; Nguyen, A.; Thomas, D.; McHugh, J.B.; et al. Prognostic Value of Tumor-Infiltrating Lymphocytes in Head and Neck Squamous Cell Carcinoma. JAMA Otolaryngol. Head Neck Surg. 2019, 145, 1012–1019. [Google Scholar] [CrossRef]
- Kawaguchi, T.; Ono, T.; Sato, F.; Kawahara, A.; Kakuma, T.; Akiba, J.; Sato, K.; Chitose, S.I.; Umeno, H. CD8+ T Cell Infiltration Predicts Chemoradiosensitivity in Nasopharyngeal or Oropharyngeal Cancer. Laryngoscope 2021, 131, E1179–E1189. [Google Scholar] [CrossRef]
- Yajima, R.; Yajima, T.; Fujii, T.; Yanagita, Y.; Fujisawa, T.; Miyamoto, T.; Tsutsumi, S.; Iijima, M.; Kuwano, H. Tumor-infiltrating CD45RO(+) memory cells are associated with a favorable prognosis breast cancer. Breast Cancer 2016, 23, 668–674. [Google Scholar] [CrossRef]
- Galon, J.; Costes, A.; Sanchez-Cabo, F.; Kirilovsky, A.; Mlecnik, B.; Lagorce-Pagès, C.; Tosolini, M.; Camus, M.; Berger, A.; Wind, P.; et al. Type, density, and location of immune cells within human colorectal tumors predict clinical outcome. Science 2006, 313, 1960–1964. [Google Scholar] [CrossRef]
- Hartan, R.; Schnellhardt, S.; Büttner-Herold, M.; Daniel, C.; Hartmann, A.; Fietkau, R.; Distel, L. The Prognostic and Predictive Significance of Tumor-Infiltrating Memory T Cells Is Reversed in High-Risk HNSCC. Cells 2022, 11, 1960. [Google Scholar] [CrossRef]


| Characteristics | N | % |
|---|---|---|
| OSCC patients | 33 | |
| Age (Mean ± SD) | 66.2 ± 12.9 | |
| Sex | ||
| Male | 13 | 39.4 |
| Female | 20 | 60.6 |
| Localization | ||
| Tongue | 17 | 51.5 |
| Maxillary gingiva | 3 | 9.1 |
| Mandibular gingiva | 10 | 30.3 |
| Buccal mucosa | 1 | 3.0 |
| Plantar of the mouth | 2 | 6.1 |
| UICC stage | ||
| Ⅰ | 4 | 12.1 |
| Ⅱ | 14 | 42.4 |
| Ⅲ | 3 | 9.1 |
| Ⅳ A | 10 | 30.3 |
| Ⅳ B | 2 | 6.1 |
| Treatment | ||
| Surgery | 16 | 48.4 |
| Chemoradiotherapy | 12 | 36.4 |
| PDT | 5 | 15.2 |
| Recurrence/Nonrecurrence | 22/11 | 66.7/33.3 |
| Parameter (Reference) | DFS | OS | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p Value a | HR | 95% CI | p Value a | |
| Age < 60 years | 0.318 | 0.110–0.918 | 0.034 * | 0.58 | 0.186–1.814 | 0.349 |
| Tumor stages 3–4 | 1.423 | 0.529–3.832 | 0.485 | 1.26 | 0.436–3.621 | 0.673 |
| Surgical therapy | 0.672 | 0.231–1.957 | 0.466 | 0.316 | 0.090–1.112 | 0.073 |
| CD45RO+/TILs CTHigh | 0.456 | 0.156–1.334 | 0.152 | 0.247 | 0.062–0.982 | 0.047 * |
| CD45RO+/TILs IMHigh | 0.319 | 0.112–0.911 | 0.033 * | 0.175 | 0.047–0.646 | 0.009 * |
| Granzyme B+/TILs IMHigh | 0.385 | 0.155–0.957 | 0.039 * | 0.687 | 0.233–2.024 | 0.496 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ito, N.; Yamasaki, S.; Shintani, T.; Matsui, K.; Obayashi, F.; Koizumi, K.; Tani, R.; Yanamoto, S.; Okamoto, T. Tumor-Infiltrating CD45RO+ Memory Cells Are Associated with Favorable Prognosis in Oral Squamous Cell Carcinoma Patients. Cancers 2023, 15, 2221. https://doi.org/10.3390/cancers15082221
Ito N, Yamasaki S, Shintani T, Matsui K, Obayashi F, Koizumi K, Tani R, Yanamoto S, Okamoto T. Tumor-Infiltrating CD45RO+ Memory Cells Are Associated with Favorable Prognosis in Oral Squamous Cell Carcinoma Patients. Cancers. 2023; 15(8):2221. https://doi.org/10.3390/cancers15082221
Chicago/Turabian StyleIto, Nanako, Sachiko Yamasaki, Tomoaki Shintani, Kensaku Matsui, Fumitaka Obayashi, Koichi Koizumi, Ryouji Tani, Souichi Yanamoto, and Tetsuji Okamoto. 2023. "Tumor-Infiltrating CD45RO+ Memory Cells Are Associated with Favorable Prognosis in Oral Squamous Cell Carcinoma Patients" Cancers 15, no. 8: 2221. https://doi.org/10.3390/cancers15082221
APA StyleIto, N., Yamasaki, S., Shintani, T., Matsui, K., Obayashi, F., Koizumi, K., Tani, R., Yanamoto, S., & Okamoto, T. (2023). Tumor-Infiltrating CD45RO+ Memory Cells Are Associated with Favorable Prognosis in Oral Squamous Cell Carcinoma Patients. Cancers, 15(8), 2221. https://doi.org/10.3390/cancers15082221






