Latest Findings on Minimally Invasive Anatomical Liver Resection
Abstract
Simple Summary
Abstract
1. Introduction
2. Latest Findings on the MIALR–PAM Consensus Meeting and Tokyo 2020 Terminology
3. Laparoscopic Anatomic Liver Resection at Ageo Central General Hospital (ACGH)
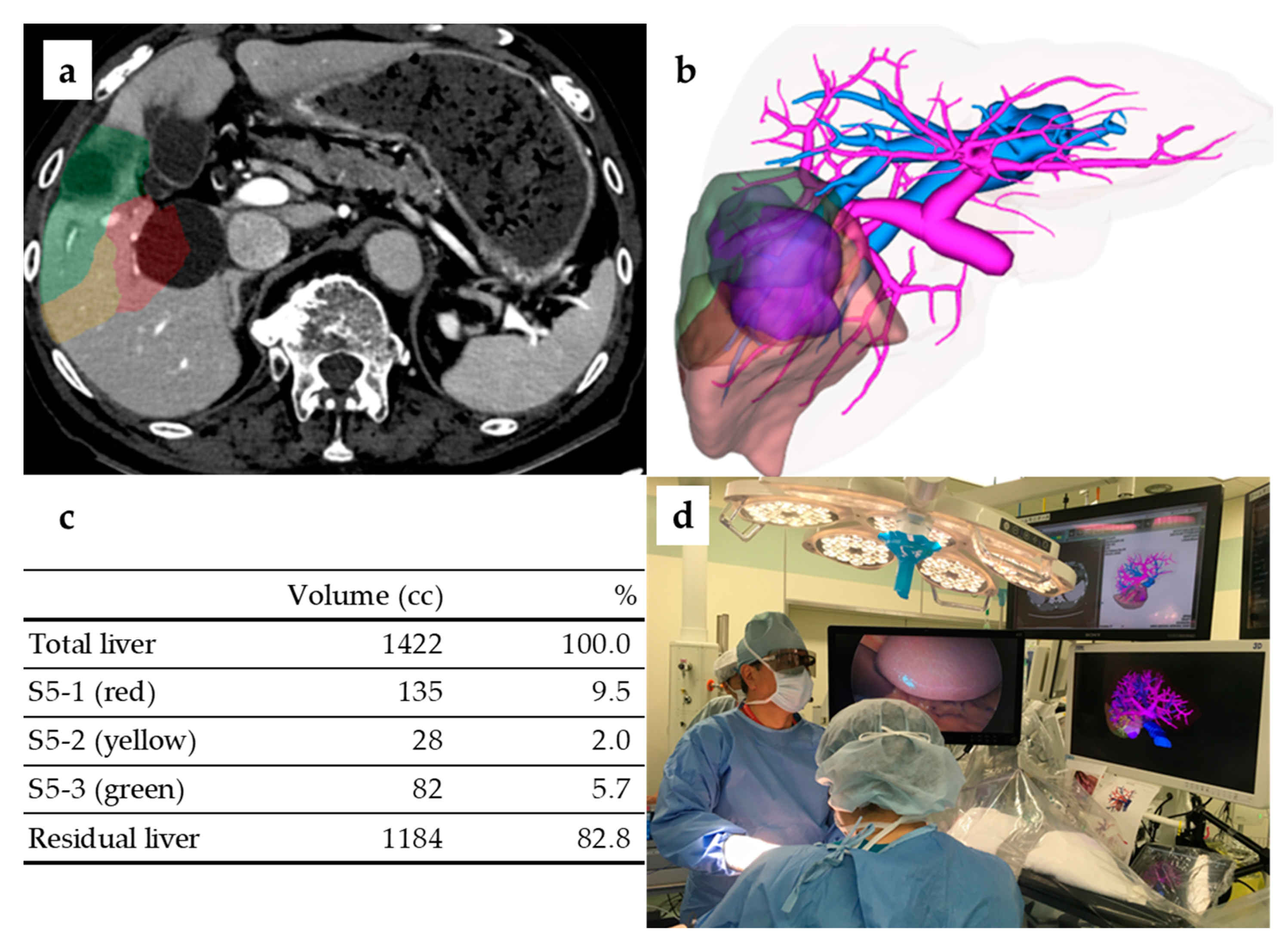
3.1. Preoperative 3D Simulation Imaging and Intraoperative 3D Monitor
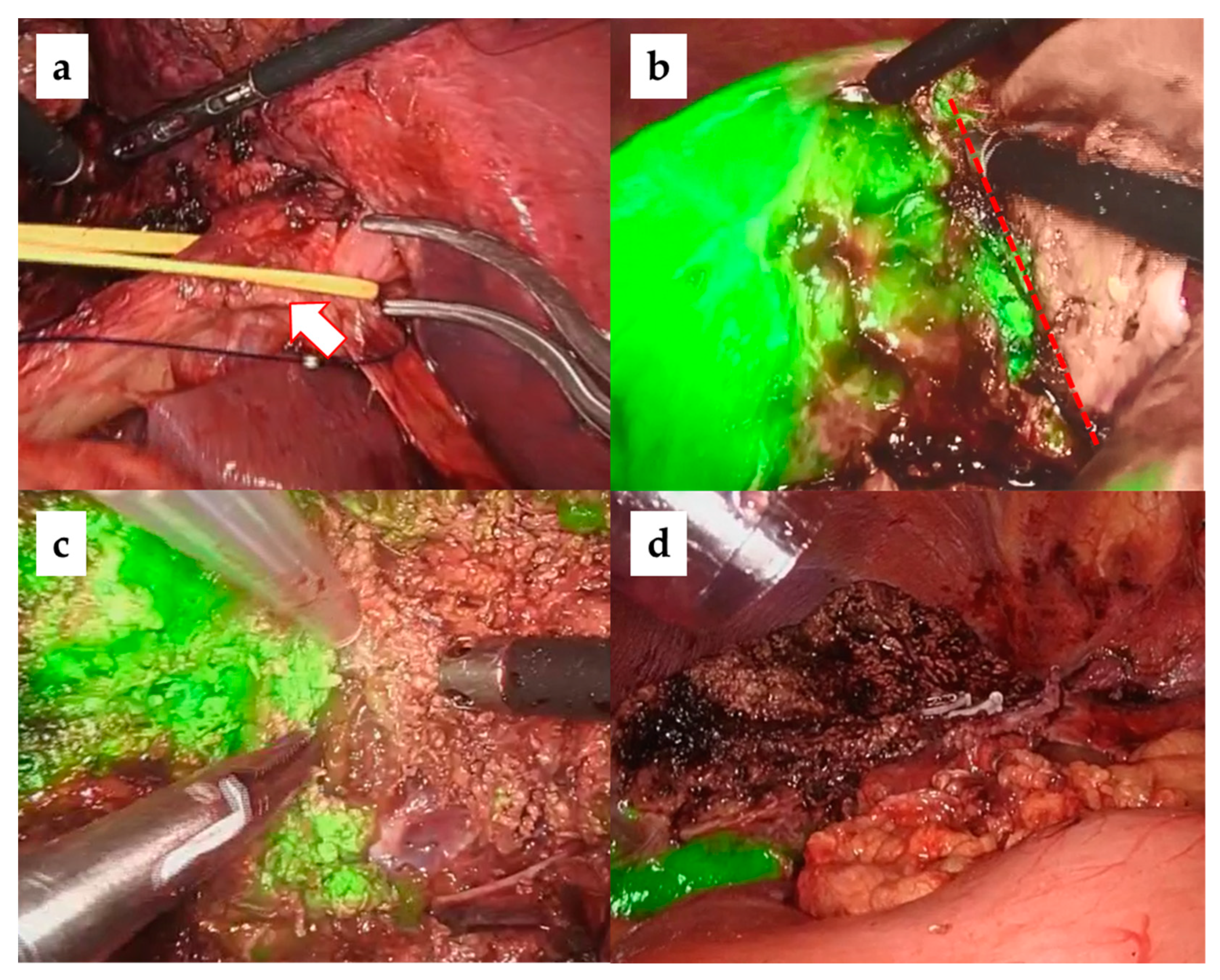
3.2. Liver Parenchyma Dissection with the Glissonean Approach and ICG Negative Staining
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Morise, Z. Current status of minimally invasive liver surgery for cancers. World J. Gastroenterol. 2022, 28, 6090–6098. [Google Scholar] [CrossRef] [PubMed]
- Ciria, R.; Berardi, G.; Alconchel, F.; Briceño, J.; Choi, G.H.; Wu, Y.; Sugioka, A.; Troisi, R.I.; Salloum, C.; Soubrane, O.; et al. The impact of robotics in liver surgery: A worldwide systematic review and short-term outcomes meta-analysis on 2728 cases. J. Hepato-Biliary-Pancreat. Sci. 2020, 29, 181–197. [Google Scholar] [CrossRef] [PubMed]
- Wakabayashi, G.; Tanabe, M. ILLS 2019 and the development of laparoscopic liver resection in Japan. J. Hepato-Biliary-Pancreat. Sci. 2019, 27, 1–2. [Google Scholar] [CrossRef]
- Wakabayashi, G.; Kaneko, H. Can major laparoscopic liver and pancreas surgery become standard practices? J. Hepato-Biliary-Pancreat. Sci. 2016, 23, 89–91. [Google Scholar] [CrossRef] [PubMed]
- Kaneko, H.; Otsuka, Y.; Kubota, Y.; Wakabayashi, G. Evolution and revolution of laparoscopic liver resection in Japan. Ann. Gastroenterol. Surg. 2017, 1, 33–43. [Google Scholar] [CrossRef]
- Buell, J.F.; Cherqui, D.; Geller, D.A.; O’Rourke, N.; Iannitti, D.; Dagher, I.; Koffron, A.J.; Thomas, M.; Gayet, B.; Han, H.S.; et al. The International Position on Laparoscopic Liver Surgery: The Louisville Statement, 2008. Ann. Surg. 2009, 250, 825–830. [Google Scholar] [CrossRef] [PubMed]
- Wakabayashi, G.; Cherqui, D.; Geller, D.A.; Buell, J.F.; Kaneko, H.; Han, H.S.; Asbun, H.; Oʼrourke, N.; Tanabe, M.; Koffron, A.J.; et al. Recommendations for laparoscopic liver resection: A report from the second international consensus conference held in Morioka. Ann. Surg. 2015, 261, 619–629. [Google Scholar] [CrossRef]
- Abu Hilal, M.; Aldrighetti, L.; Dagher, I.; Edwin, B.; Troisi, R.I.; Alikhanov, R.; Aroori, S.; Belli, G.; Besselink, M.; Briceno, J.; et al. The Southampton Consensus Guidelines for Laparoscopic Liver Surgery: From indication to implementation. Ann. Surg. 2018, 268, 11–18. [Google Scholar] [CrossRef]
- Morimoto, M.; Monden, K.; Wakabayashi, T.; Gotohda, N.; Abe, Y.; Honda, G.; Abu Hilal, M.; Aoki, T.; Asbun, H.J.; Berardi, G.; et al. Minimally invasive anatomic liver resection: Results of a survey of world experts. J. Hepato-Biliary-Pancreat. Sci. 2021, 29, 33–40. [Google Scholar] [CrossRef]
- Sugioka, A.; Kato, Y.; Tanahashi, Y. Systematic extrahepatic Glissonean pedicle isolation for anatomical liver resection based on Laennec’s capsule: Proposal of a novel comprehensive surgical anatomy of the liver. J. Hepato-Biliary-Pancreat. Sci. 2017, 24, 17–23. [Google Scholar] [CrossRef]
- Felli, E.; Ishizawa, T.; Cherkaoui, Z.; Diana, M.; Tripon, S.; Baumert, T.F.; Schuster, C.; Pessaux, P. Laparoscopic anatomical liver resection for malignancies using positive or negative staining technique with intraoperative indocyanine green-fluorescence imaging. HPB 2021, 23, 1647–1655. [Google Scholar] [CrossRef]
- Ciria, R.; Berardi, G.; Nishino, H.; Chan, A.C.; Chanwat, R.; Chen, K.; Chen, Y.; Cheung, T.T.; Fuks, D.; Geller, D.A.; et al. A snapshot of the 2020 conception of anatomic liver resections and their applicability on minimally invasive liver surgery. A preparatory survey for the Expert Consensus Meeting on Precision Anatomy for Minimally Invasive HBP Surgery. J. Hepato-Biliary-Pancreat. Sci. 2021, 29, 41–50. [Google Scholar] [CrossRef]
- Gotohda, N.; Cherqui, D.; Geller, D.A.; Abu Hilal, M.; Berardi, G.; Ciria, R.; Abe, Y.; Aoki, T.; Asbun, H.J.; Chan, A.C.Y.; et al. Expert Consensus Guidelines: How to safely perform minimally invasive anatomic liver resection. J. Hepato-Biliary-Pancreat. Sci. 2021, 29, 16–32. [Google Scholar] [CrossRef] [PubMed]
- Nagakawa, Y.; Nakata, K.; Nishino, H.; Ohtsuka, T.; Ban, D.; Asbun, H.J.; Boggi, U.; He, J.; Kendrick, M.L.; Palanivelu, C.; et al. International expert consensus on precision anatomy for minimally invasive pancreatoduodenectomy: PAM-HBP surgery project. J. Hepato-Biliary-Pancreat. Sci. 2021, 29, 124–135. [Google Scholar] [CrossRef]
- Wakabayashi, G.; Cherqui, D.; Geller, D.A.; Abu Hilal, M.; Berardi, G.; Ciria, R.; Abe, Y.; Aoki, T.; Asbun, H.J.; Chan, A.C.Y.; et al. The Tokyo 2020 terminology of liver anatomy and resections: Updates of the Brisbane 2000 system. J. Hepato-Biliary-Pancreat. Sci. 2021, 29, 6–15. [Google Scholar] [CrossRef] [PubMed]
- Strasberg, S.; Belghiti, J.; Clavien, P.-A.; Gadzijev, E.; Garden, J.; Lau, W.-Y.; Makuuchi, M.; Strong, R. The Brisbane 2000 Terminology of Liver Anatomy and Resections. HPB 2000, 2, 333–339. [Google Scholar] [CrossRef]
- Strasberg, S.M.; Phillips, C. Use and Dissemination of the Brisbane 2000 Nomenclature of Liver Anatomy and Resections. Ann. Surg. 2013, 257, 377–382. [Google Scholar] [CrossRef]
- Strasberg, S.M. Nomenclature of hepatic anatomy and resections: A review of the Brisbane 2000 system. J. Hepato-Biliary-Pancreat. Surg. 2005, 12, 351–355. [Google Scholar] [CrossRef]
- Morimoto, M.; Tomassini, F.; Berardi, G.; Mori, Y.; Shirata, C.; Abu Hilal, M.; Asbun, H.J.; Cherqui, D.; Gotohda, N.; Han, H.; et al. Glissonean approach for hepatic inflow control in minimally invasive anatomic liver resection: A systematic review. J. Hepato-Biliary-Pancreat. Sci. 2021, 29, 51–65. [Google Scholar] [CrossRef]
- Monden, K.; Alconchel, F.; Berardi, G.; Ciria, R.; Akahoshi, K.; Miyasaka, Y.; Urade, T.; Vázquez, A.G.; Hasegawa, K.; Honda, G.; et al. Landmarks and techniques to perform minimally invasive liver surgery: A systematic review with a focus on hepatic outflow. J. Hepato-Biliary-Pancreat. Sci. 2021, 29, 66–81. [Google Scholar] [CrossRef]
- Wakabayashi, T.; Cacciaguerra, A.B.; Ciria, R.; Ariizumi, S.; Durán, M.; Golse, N.; Ogiso, S.; Abe, Y.; Aoki, T.; Hatano, E.; et al. Landmarks to identify segmental borders of the liver: A review prepared for PAM-HBP expert consensus meeting 2021. J. Hepato-Biliary-Pancreat. Sci. 2021, 29, 82–98. [Google Scholar] [CrossRef]
- Berardi, G.; Colasanti, M.; Meniconi, R.L.; Ferretti, S.; Guglielmo, N.; Mariano, G.; Burocchi, M.; Campanelli, A.; Scotti, A.; Pecoraro, A.; et al. The Applications of 3D Imaging and Indocyanine Green Dye Fluorescence in Laparoscopic Liver Surgery. Diagnostics 2021, 11, 2169. [Google Scholar] [CrossRef]
- Mishima, K.; Wakabayashi, T.; Fujiyama, Y.; Alomari, M.; Colella, M.; Wakabayashi, G. Resection margin status in laparoscopic liver resection for colorectal liver metastases: Literature review and future perspectives. Minerva Surg. 2022, 77, 428–432. [Google Scholar] [CrossRef] [PubMed]
- Funamizu, N.; Ozaki, T.; Mishima, K.; Igarashi, K.; Omura, K.; Takada, Y.; Wakabayashi, G. Evaluation of accuracy of laparoscopic liver mono-segmentectomy using the Glissonian approach with indocyanine green fluorescence negative staining by comparing estimated and actual resection volumes: A single-center retrospective cohort study. J. Hepato-Biliary-Pancreat. Sci. 2021, 28, 1060–1068. [Google Scholar] [CrossRef] [PubMed]
- Mori, S.M.; Mishima, K.; Ozaki, T.; Fujiyama, Y.; Wakabayashi, G.M. Short-term Outcomes and Difficulty of Repeat Laparoscopic Liver Resection. Ann. Surg. Open 2022, 3, e191. [Google Scholar] [CrossRef]
- Monden, K.; Sadamori, H.; Hioki, M.; Ohno, S.; Takakura, N. Intrahepatic Glissonean Approach for Laparoscopic Bisegmentectomy 7 and 8 With Root-Side Hepatic Vein Exposure. Ann. Surg. Oncol. 2021, 29, 970–971. [Google Scholar] [CrossRef]
- Takasaki, K. Glissonean pedicle transection method for hepatic resection: A new concept of liver segmentation. J. Hepato-Biliary-Pancreat. Surg. 1998, 5, 286–291. [Google Scholar] [CrossRef]
- Wakabayashi, T.; Cacciaguerra, A.B.; Abe, Y.; Bona, E.D.; Nicolini, D.; Mocchegiani, F.; Kabeshima, Y.; Vivarelli, M.; Wakabayashi, G.; Kitagawa, Y. Indocyanine Green Fluorescence Navigation in Liver Surgery: A Systematic Review on Dose and Timing of Administration. Ann. Surg. 2022, 275, 1025–1034. [Google Scholar] [CrossRef] [PubMed]
- Otsuka, Y.; Matsumoto, Y.; Ito, Y.; Okada, R.; Maeda, T.; Ishii, J.; Kajiwara, Y.; Okubo, K.; Funahashi, K.; Kaneko, H. Intraoperative guidance using ICG fluorescence imaging system for safe and precise laparoscopic liver resection. Int. J. Clin. Rev. 2021, 76, 211–219. [Google Scholar] [CrossRef]
- Wakabayashi, G.; Cherqui, D.; Geller, D.A.; Han, H.-S.; Kaneko, H.; Buell, J.F. Laparoscopic hepatectomy is theoretically better than open hepatectomy: Preparing for the 2nd International Consensus Conference on Laparoscopic Liver Resection. J. Hepato-Biliary-Pancreat. Sci. 2014, 21, 723–731. [Google Scholar] [CrossRef]
- Aoki, T.; Yasuda, D.; Shimizu, Y.; Odaira, M.; Niiya, T.; Kusano, T.; Mitamura, K.; Hayashi, K.; Murai, N.; Koizumi, T.; et al. Image-Guided Liver Mapping Using Fluorescence Navigation System with Indocyanine Green for Anatomical Hepatic Resection. World J. Surg. 2008, 32, 1763–1767. [Google Scholar] [CrossRef] [PubMed]
- Cucchetti, A.; Cescon, M.; Ercolani, G.; Bigonzi, E.; Torzilli, G.; Pinna, A.D. A Comprehensive Meta-regression Analysis on Outcome of Anatomic Resection Versus Nonanatomic Resection for Hepatocellular Carcinoma. Ann. Surg. Oncol. 2012, 19, 3697–3705. [Google Scholar] [CrossRef] [PubMed]
- Kwon, J.H.; Lee, J.-W.; Lee, J.W.; Lee, Y.J. Effects of Anatomical or Non-Anatomical Resection of Hepatocellular Carcinoma on Survival Outcome. J. Clin. Med. 2022, 11, 1369. [Google Scholar] [CrossRef] [PubMed]
- Brown, K.M.; Albania, M.F.; Samra, J.S.; Kelly, P.J.; Hugh, T.J. Propensity score analysis of non-anatomical versus anatomical resection of colorectal liver metastases. BJS Open 2019, 3, 521–531. [Google Scholar] [CrossRef] [PubMed]


| Disease | n (%) |
|---|---|
| Hepatocellular carcinoma | 104 (48.4%) |
| Metastatic tumor | 72 (33.8%) |
| Intrahepatic cholangiocarcinoma | 16 (7.5%) |
| Benign liver disease | 11 (5.2%) |
| Malignant lymphoma | 3 (1.4%) |
| Others | 7 (3.3%) |
| Case (%) | Procedure | Operation Time (min) | Blood Loss (mL) | Conversion to Open | Postoperative Complication (CD ≥ IIIa) | Postoperative Hospital Stay (Day) | ||
|---|---|---|---|---|---|---|---|---|
| Hr3 | 1 (0.5%) | Left trisectionectomy | 1 (0.5%) | 354 | 188 | 0 (0%) | 1 (100%) | 47 |
| Hr2 | 40 (19.4%) | Left hepatectomy | 20 (9.4%) | 353 (216–540) | 210 (15–2737) | 0 (0%) | 1 (5.0%) | 8 (5–15) |
| Right hepatectomy | 14 (6.6%) | 448 (305–798) | 118 (10–925) | 0 (0%) | 1 (7.1%) | 11.5 (6–53) | ||
| Central bisectionectomy | 6 (2.8%) | 372 (281–542) | 646 (80–1241) | 0 (0%) | 1 (16.7%) | 13.5 (6–142) | ||
| Hr1 | 60 (27.8%) | Right anterior sectionectomy | 20 (9.4%) | 389 (214–552) | 429 (47–1881) | 0 (0%) | 4 (20.0%) | 11 (6–90) |
| Right posterior sectionectomy | 19 (8.9%) | 405 (304–639) | 456 (5–1523) | 1 (5.3%) | 0 (0%) | 11 (5–21) | ||
| Left medial sectionectomy | 15 (7.0%) | 331 (215–420) | 190 (5–867) | 0 (0%) | 0 (0%) | 9 (6–97) | ||
| Left lateral sectionectomy | 6 (2.8%) | 267 (149–439) | 293 (35–2367) | 0 (0%) | 1 (16.7%) | 9 (5–15) | ||
| HrS | 112 (54.4%) | Segmentectomy | 88 (41.3%) | 338 (110–850) | 193 (10–5600) | 0 (0%) | 10 (11.4%) | 9 (5–251) |
| HrSS | Subsegmentectomy | 24 (11.3%) | 335 (163–585) | 173 (25–710) | 0 (0%) | 2 (8.3%) | 8 (6–76) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fujiyama, Y.; Wakabayashi, T.; Mishima, K.; Al-Omari, M.A.; Colella, M.; Wakabayashi, G. Latest Findings on Minimally Invasive Anatomical Liver Resection. Cancers 2023, 15, 2218. https://doi.org/10.3390/cancers15082218
Fujiyama Y, Wakabayashi T, Mishima K, Al-Omari MA, Colella M, Wakabayashi G. Latest Findings on Minimally Invasive Anatomical Liver Resection. Cancers. 2023; 15(8):2218. https://doi.org/10.3390/cancers15082218
Chicago/Turabian StyleFujiyama, Yoshiki, Taiga Wakabayashi, Kohei Mishima, Malek A. Al-Omari, Marco Colella, and Go Wakabayashi. 2023. "Latest Findings on Minimally Invasive Anatomical Liver Resection" Cancers 15, no. 8: 2218. https://doi.org/10.3390/cancers15082218
APA StyleFujiyama, Y., Wakabayashi, T., Mishima, K., Al-Omari, M. A., Colella, M., & Wakabayashi, G. (2023). Latest Findings on Minimally Invasive Anatomical Liver Resection. Cancers, 15(8), 2218. https://doi.org/10.3390/cancers15082218





