Diagnostic Performance of Afirma and Interpace Diagnostics Genetic Testing in Indeterminate Thyroid Nodules: A Single Center Study †
Abstract
Simple Summary
Abstract
1. Introduction
2. Material and Methods
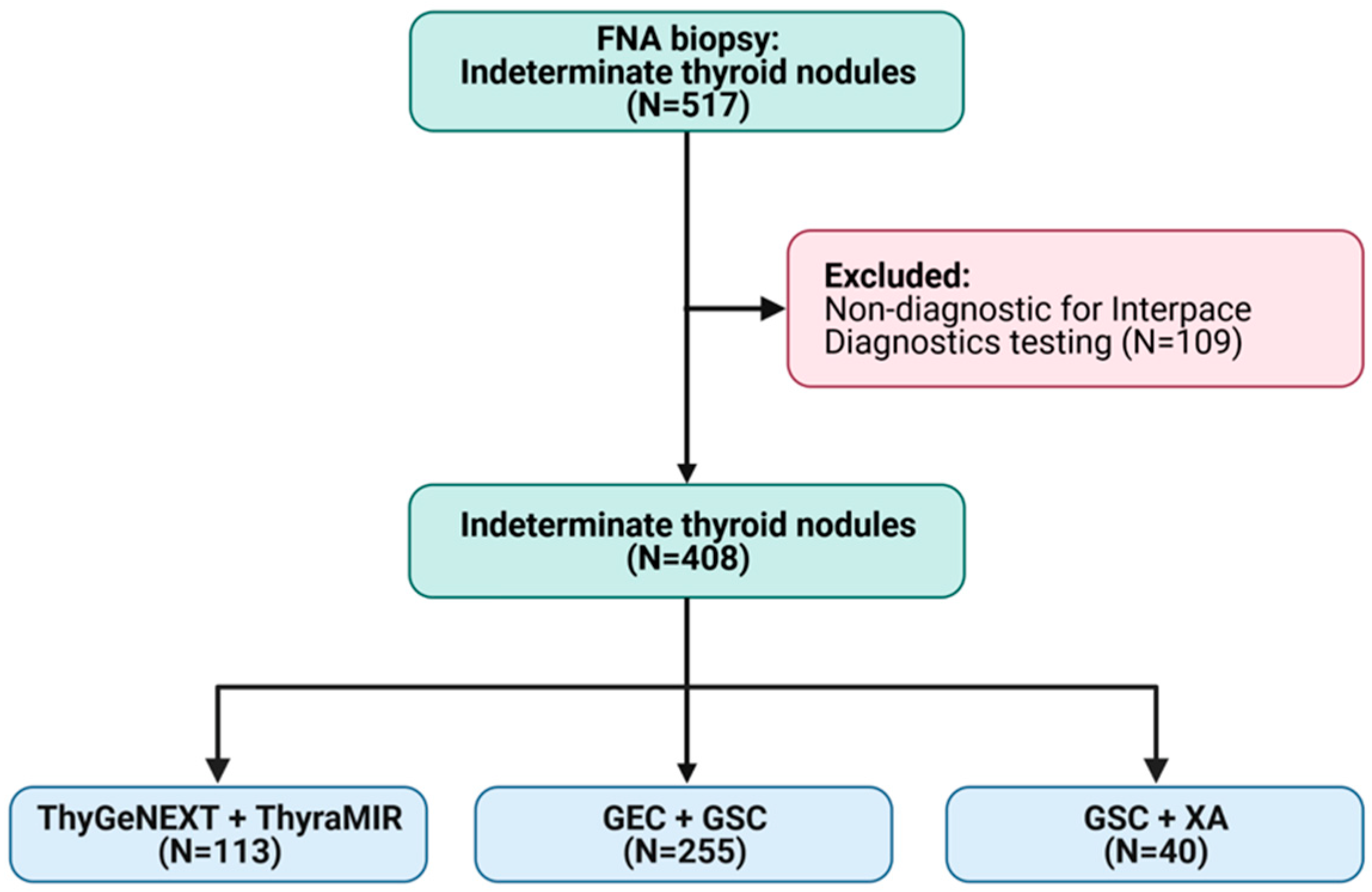
2.1. Study Design
2.2. Ultrasound Assessment
2.3. Fine-Needle Aspiration
2.4. Afirma Molecular Testing
2.5. Interpace Molecular Testing
2.6. Cohorts
2.7. Statistical Analysis
3. Results
3.1. Study Population
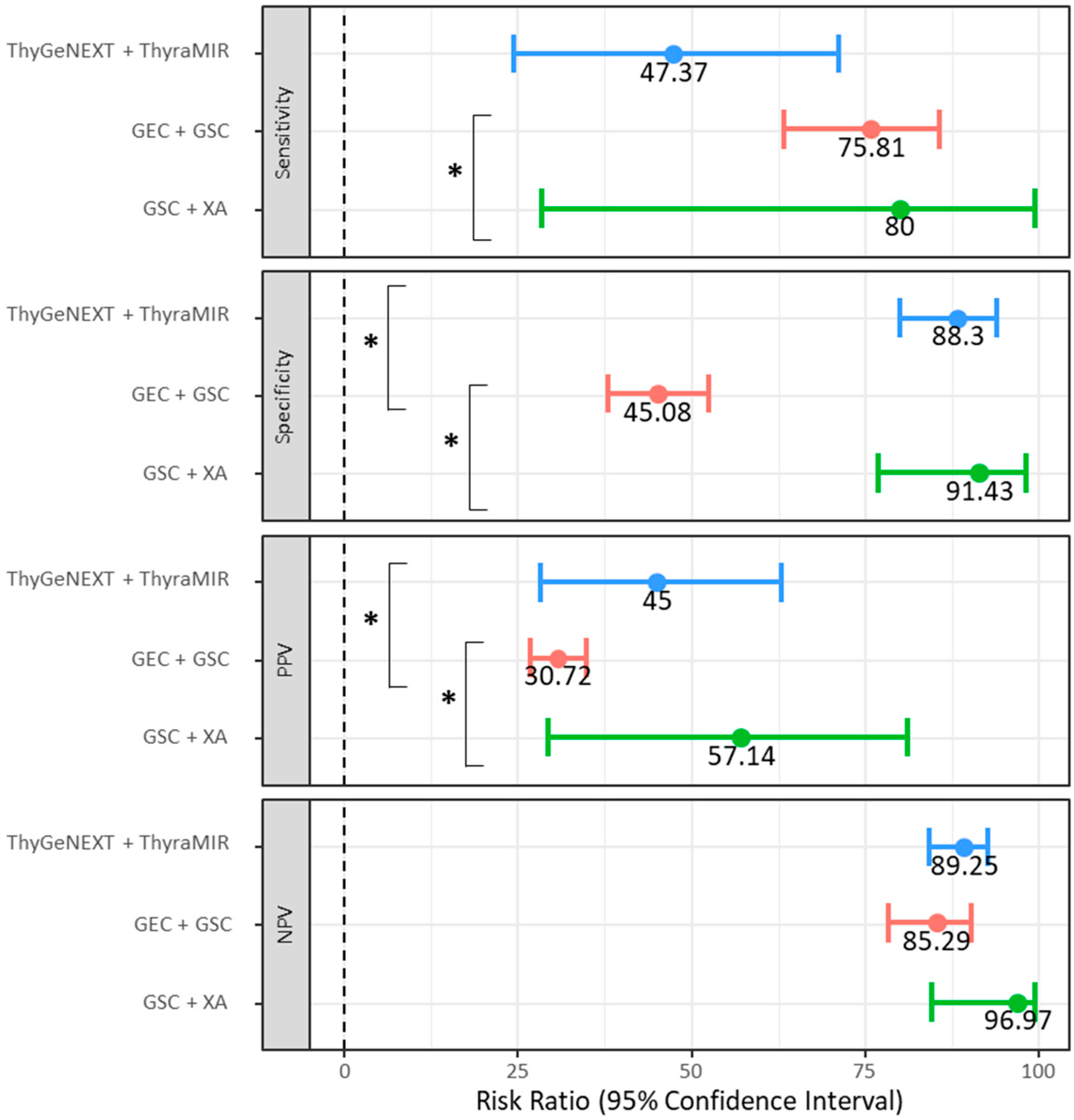
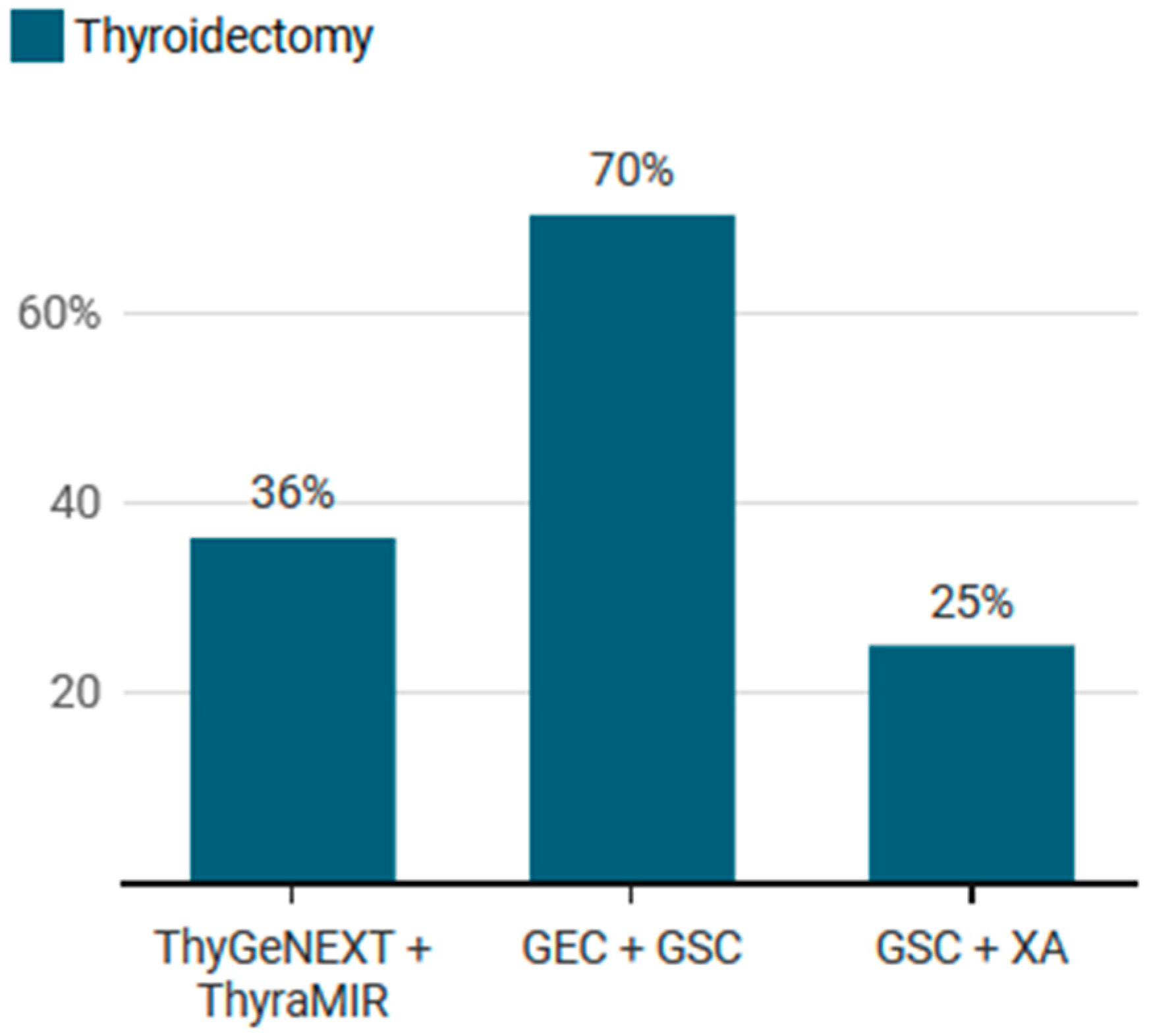
3.2. Sub-Group Analysis including Nodules Undergoing Surgery
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Guth, S.; Theune, U.; Aberle, J.; Galach, A.; Bamberger, C. Very High Prevalence of Thyroid Nodules Detected by High Frequency (13 MHz) Ultrasound Examination. Eur. J. Clin. Investig. 2009, 39, 699–706. [Google Scholar] [CrossRef] [PubMed]
- Haugen, B.R.; Alexander, E.K.; Bible, K.C.; Doherty, G.M.; Mandel, S.J.; Nikiforov, Y.E.; Pacini, F.; Randolph, G.W.; Sawka, A.M.; Schlumberger, M. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2016, 26, 1–133. [Google Scholar] [CrossRef] [PubMed]
- Cibas, E.S.; Ali, S.Z. The 2017 Bethesda System for Reporting Thyroid Cytopathology. Thyroid 2017, 27, 1341–1346. [Google Scholar] [CrossRef] [PubMed]
- Durante, C.; Grani, G.; Lamartina, L.; Filetti, S.; Mandel, S.J.; Cooper, D.S. The Diagnosis and Management of Thyroid Nodules: A Review. JAMA 2018, 319, 914–924. [Google Scholar] [CrossRef]
- Vargas-Salas, S.; Martínez, J.R.; Urra, S.; Domínguez, J.M.; Mena, N.; Uslar, T.; Lagos, M.; Henríquez, M.; González, H.E. Genetic Testing for Indeterminate Thyroid Cytology: Review and Meta-Analysis. Endocr. Relat. Cancer 2018, 25, R163. [Google Scholar] [CrossRef]
- Silaghi, C.A.; Lozovanu, V.; Georgescu, C.E.; Georgescu, R.D.; Susman, S.; Năsui, B.A.; Dobrean, A.; Silaghi, H. Thyroseq v3, Afirma GSC, and MicroRNA Panels versus Previous Molecular Tests in the Preoperative Diagnosis of Indeterminate Thyroid Nodules: A Systematic Review and Meta-Analysis. Front. Endocrinol. 2021, 472, 649522. [Google Scholar] [CrossRef] [PubMed]
- Nishino, M. Molecular Cytopathology for Thyroid Nodules: A Review of Methodology and Test Performance. Cancer Cytopathol. 2016, 124, 14–27. [Google Scholar] [CrossRef]
- Lithwick-Yanai, G.; Dromi, N.; Shtabsky, A.; Morgenstern, S.; Strenov, Y.; Feinmesser, M.; Kravtsov, V.; Leon, M.E.; Hajdúch, M.; Ali, S.Z. Multicentre Validation of a MicroRNA-Based Assay for Diagnosing Indeterminate Thyroid Nodules Utilising Fine Needle Aspirate Smears. J. Clin. Pathol. 2017, 70, 500–507. [Google Scholar] [CrossRef]
- Nishino, M.; Bellevicine, C.; Baloch, Z. Molecular Tests for Risk-Stratifying Cytologically Indeterminate Thyroid Nodules: An Overview of Commercially Available Testing Platforms in the United States. J. Mol. Pathol. 2021, 2, 135–146. [Google Scholar] [CrossRef]
- Alexander, E.K.; Kennedy, G.C.; Baloch, Z.W.; Cibas, E.S.; Chudova, D.; Diggans, J.; Friedman, L.; Kloos, R.T.; LiVolsi, V.A.; Mandel, S.J. Preoperative Diagnosis of Benign Thyroid Nodules with Indeterminate Cytology. N. Engl. J. Med. 2012, 367, 705–715. [Google Scholar] [CrossRef]
- Patel, K.N.; Angell, T.E.; Babiarz, J.; Barth, N.M.; Blevins, T.; Duh, Q.-Y.; Ghossein, R.A.; Harrell, R.M.; Huang, J.; Kennedy, G.C. Performance of a Genomic Sequencing Classifier for the Preoperative Diagnosis of Cytologically Indeterminate Thyroid Nodules. JAMA Surg. 2018, 153, 817–824. [Google Scholar] [CrossRef] [PubMed]
- Angell, T.E.; Wirth, L.J.; Cabanillas, M.E.; Shindo, M.L.; Cibas, E.S.; Babiarz, J.E.; Hao, Y.; Kim, S.Y.; Walsh, P.S.; Huang, J. Analytical and Clinical Validation of Expressed Variants and Fusions from the Whole Transcriptome of Thyroid FNA Samples. Front. Endocrinol. 2019, 10, 612. [Google Scholar] [CrossRef] [PubMed]
- Partyka, K.L.; Trevino, K.; Randolph, M.L.; Cramer, H.; Wu, H.H. Risk of Malignancy and Neoplasia Predicted by Three Molecular Testing Platforms in Indeterminate Thyroid Nodules on Fine-needle Aspiration. Diagn. Cytopathol. 2019, 47, 853–862. [Google Scholar] [CrossRef]
- VanderLaan, P.A. Molecular Markers: Implications for Cytopathology and Specimen Collection. Cancer Cytopathol. 2015, 123, 454–460. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, H.; Schnitzer-Perlman, T.; Shtabsky, A.; Vanden Bussche, C.J.; Ali, S.Z.; Kolar, Z.; Pagni, F.; Rosetta Genomics Group; Bar, D.; Meiri, E. Analytical Validity of a MicroRNA-based Assay for Diagnosing Indeterminate Thyroid FNA Smears from Routinely Prepared Cytology Slides. Cancer Cytopathol. 2016, 124, 711–721. [Google Scholar] [CrossRef] [PubMed]
- Finkelstein, S.D.; Sistrunk, J.W.; Malchoff, C.; Thompson, D.V.; Kumar, G.; Timmaraju, V.A.; Repko, B.; Mireskandari, A.; Evoy-Goodman, L.A.; Massoll, N.A. A Retrospective Evaluation of the Diagnostic Performance of an Interdependent Pairwise MicroRNA Expression Analysis with a Mutation Panel in Indeterminate Thyroid Nodules. Thyroid 2022, 32, 1362–1371. [Google Scholar] [CrossRef]
- Angell, T.E.; Heller, H.T.; Cibas, E.S.; Barletta, J.A.; Kim, M.I.; Krane, J.F.; Marqusee, E. Independent Comparison of the Afirma Genomic Sequencing Classifier and Gene Expression Classifier for Cytologically Indeterminate Thyroid Nodules. Thyroid 2019, 29, 650–656. [Google Scholar] [CrossRef]
- Harrell, R.M.; Eyerly-Webb, S.A.; Golding, A.C.; Edwards, C.M.; Bimston, D.N. Statistical Comparison of Afirma GSC and Afirma GEC Outcomes in a Community Endocrine Surgical Practice: Early Findings. Endocr. Pract. 2019, 25, 161–164. [Google Scholar] [CrossRef]
- Davies, L.; Ouellette, M.; Hunter, M.; Welch, H.G. The Increasing Incidence of Small Thyroid Cancers: Where Are the Cases Coming From? Laryngoscope 2010, 120, 2446–2451. [Google Scholar] [CrossRef]
- Hsiao, V.; Massoud, E.; Jensen, C.; Zhang, Y.; Hanlon, B.M.; Hitchcock, M.; Arroyo, N.; Chiu, A.S.; Fernandes-Taylor, S.; Alagoz, O. Diagnostic Accuracy of Fine-Needle Biopsy in the Detection of Thyroid Malignancy: A Systematic Review and Meta-Analysis. JAMA Surg. 2022, 157, 1105–1113. [Google Scholar] [CrossRef]
- Bergenfelz, A.; Jansson, S.; Kristoffersson, A.; Mårtensson, H.; Reihnér, E.; Wallin, G.; Lausen, I. Complications to Thyroid Surgery: Results as Reported in a Database from a Multicenter Audit Comprising 3660 Patients. Langenbecks Arch. Surg. 2008, 393, 667–673. [Google Scholar] [CrossRef]
- Schneider, D.F.; Stafford, L.M.C.; Brys, N.; Greenberg, C.C.; Balentine, C.J.; Elfenbein, D.M.; Pitt, S.C. Gauging the Extent of Thyroidectomy for Indeterminate Thyroid Nodules: An Oncologic Perspective. Endocr. Pract. 2017, 23, 442–450. [Google Scholar] [CrossRef]
- Balentine, C.J.; Domingo, R.P.; Patel, R.; Laucirica, R.; Suliburk, J.W. Thyroid Lobectomy for Indeterminate FNA: Not without Consequences. J. Surg. Res. 2013, 184, 189–192. [Google Scholar] [CrossRef] [PubMed]
- Nasr, C.E.; Andrioli, M.; Endo, M.; Harrell, R.M.; Livhits, M.J.; Osakwe, I.; Polavarapu, P.; Siperstein, A.; Wei, S.; Zheng, X. Real-World Performance of the Afirma Genomic Sequencing Classifier (GSC)—A Meta-Analysis. J. Clin. Endocrinol. Metab. 2022. [Google Scholar] [CrossRef]
- Al-Qurayshi, Z.; Deniwar, A.; Thethi, T.; Mallik, T.; Srivastav, S.; Murad, F.; Bhatia, P.; Moroz, K.; Sholl, A.B.; Kandil, E. Association of Malignancy Prevalence with Test Properties and Performance of the Gene Expression Classifier in Indeterminate Thyroid Nodules. JAMA Otolaryngol. Neck Surg. 2017, 143, 403–408. [Google Scholar] [CrossRef]
- Al-Qurayshi, Z.; Sholl, A.B.; Kandil, E. Exclusion of Eligible Indeterminate Thyroid Nodules in Estimates of Negative Predictive Value for the Gene Expression Classifier—Reply. JAMA Otolaryngol. Neck Surg. 2017, 143, 738–739. [Google Scholar] [CrossRef] [PubMed]
- Marti, J.L.; Avadhani, V.; Donatelli, L.A.; Niyogi, S.; Wang, B.; Wong, R.J.; Shaha, A.R.; Ghossein, R.A.; Lin, O.; Morris, L.G. Wide Inter-Institutional Variation in Performance of a Molecular Classifier for Indeterminate Thyroid Nodules. Ann. Surg. Oncol. 2015, 22, 3996–4001. [Google Scholar] [CrossRef]
- Kuo, J.H.; McManus, C.; Graves, C.E.; Madani, A.; Khokhar, M.T.; Huang, B.; Lee, J.A. Updates in the Management of Thyroid Nodules. Curr. Probl. Surg. 2019, 56, 103–127. [Google Scholar] [CrossRef]
- Nicholson, K.J.; Roberts, M.S.; McCoy, K.L.; Carty, S.E.; Yip, L. Molecular Testing versus Diagnostic Lobectomy in Bethesda III/IV Thyroid Nodules: A Cost-Effectiveness Analysis. Thyroid 2019, 29, 1237–1243. [Google Scholar] [CrossRef]
- Najafzadeh, M.; Marra, C.A.; Lynd, L.D.; Wiseman, S.M. Cost-Effectiveness of Using a Molecular Diagnostic Test to Improve Preoperative Diagnosis of Thyroid Cancer. Value Health 2012, 15, 1005–1013. [Google Scholar] [CrossRef] [PubMed]
- Eszlinger, M.; Lau, L.; Ghaznavi, S.; Symonds, C.; Chandarana, S.P.; Khalil, M.; Paschke, R. Molecular Profiling of Thyroid Nodule Fine-Needle Aspiration Cytology. Nat. Rev. Endocrinol. 2017, 13, 415–424. [Google Scholar] [CrossRef] [PubMed]
- Sahli, Z.T.; Smith, P.W.; Umbricht, C.B.; Zeiger, M.A. Preoperative Molecular Markers in Thyroid Nodules. Front. Endocrinol. 2018, 9, 179. [Google Scholar] [CrossRef] [PubMed]
- Zanocco, K.A.; Wu, J.X.; Yeh, M.W. Parathyroidectomy for Asymptomatic Primary Hyperparathyroidism: A Revised Cost-Effectiveness Analysis Incorporating Fracture Risk Reduction. Surgery 2017, 161, 16–24. [Google Scholar] [CrossRef] [PubMed]

| Bethesda Classification | ThyGeNEXT + ThyraMIR (N = 113) | GEC + GSC (N = 255) | GSC + XA (N = 40) |
|---|---|---|---|
| Bethesda III | 100 (88.5) | 221 (86.7) | 35 (87.5) |
| Bethesda IV | 4 (3.5) | 5 (2.0) | 1 (2.5) |
| Bethesda V | 9 (8.0) | 29 (11.4) | 4 (10) |
| ThyGeNEXT + ThyraMIR (N = 113) | GEC + GSC (N = 255) | GSC + XA (N = 40) | ||||
|---|---|---|---|---|---|---|
| Value | 95%CI | Value | 95%CI | Value | 95%CI | |
| Sensitivity | 47.37 | 24.45–71.14 | 75.81 | 63.26–85.78 | 80.00 | 28.36–99.49 |
| Specificity | 88.30 | 80.03–94.01 | 45.08 | 37.92–52.39 | 91.43 | 76.94–98.20 |
| Positive LR | 4.05 | 1.95–8.40 | 1.38 | 1.14–1.67 | 9.33 | 2.90–29.99 |
| Negative LR | 0.60 | 0.39–0.92 | 0.54 | 0.34–0.86 | 0.22 | 0.04–1.27 |
| PPV | 45.00 | 28.28–62.93 | 30.72 | 26.83–34.90 | 57.14 | 29.32–81.08 |
| NPV | 89.25 | 84.34–92.75 | 85.29 | 78.42–90.25 | 96.97 | 84.68–99.46 |
| DOR | 6.79 | 2.26–20.37 | 2.57 | 1.35–4.91 | 42.67 | 3.54–514.85 |
| Accuracy | 81.42 | 73.01–88.11 | 52.55 | 46.23–58.81 | 90.00 | 76.34–97.21 |
| ThyGeNEXT + ThyraMIR (N = 41) | GEC + GSC (N = 179) | GSC + XA (N = 10) | ||||
|---|---|---|---|---|---|---|
| Value | 95%CI | Value | 95%CI | Value | 95%CI | |
| Sensitivity | 50.00 | 26.02–73.98 | 75.41 | 62.71–85.54 | 80.00 | 28.36–99.49 |
| Specificity | 65.22 | 42.73–83.62 | 40.68 | 31.73–50.11 | 66.67 | 22.28–95.67 |
| Positive LR | 1.44 | 0.70–2.97 | 1.27 | 1.03–1.56 | 2.40 | 0.71–8.08 |
| Negative LR | 0.77 | 0.44–1.33 | 0.60 | 0.37–0.99 | 0.30 | 0.05–1.89 |
| PPV | 52.94 | 35.25–69.92 | 39.66 | 34.82–44.70 | 66.67 | 37.28–87.06 |
| NPV | 62.50 | 49.02–74.28 | 76.19 | 66.21–83.94 | 80.00 | 38.80–96.19 |
| DOR | 1.88 | 0.53–6.62 | 2.10 | 1.06–4.19 | 8.00 | 0.50–127.90 |
| Accuracy | 58.54 | 42.11–73.68 | 52.51 | 44.93–60.01 | 72.73 | 39.03–93.98 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kandil, E.; Metz, T.A.; Issa, P.P.; Aboueisha, M.; Omar, M.; Attia, A.S.; Chabot, B.; Hussein, M.; Moroz, K.; Shama, M.; et al. Diagnostic Performance of Afirma and Interpace Diagnostics Genetic Testing in Indeterminate Thyroid Nodules: A Single Center Study. Cancers 2023, 15, 2098. https://doi.org/10.3390/cancers15072098
Kandil E, Metz TA, Issa PP, Aboueisha M, Omar M, Attia AS, Chabot B, Hussein M, Moroz K, Shama M, et al. Diagnostic Performance of Afirma and Interpace Diagnostics Genetic Testing in Indeterminate Thyroid Nodules: A Single Center Study. Cancers. 2023; 15(7):2098. https://doi.org/10.3390/cancers15072098
Chicago/Turabian StyleKandil, Emad, Tyler A. Metz, Peter P. Issa, Mohamed Aboueisha, Mahmoud Omar, Abdallah S. Attia, Bert Chabot, Mohammad Hussein, Krzysztof Moroz, Mohamed Shama, and et al. 2023. "Diagnostic Performance of Afirma and Interpace Diagnostics Genetic Testing in Indeterminate Thyroid Nodules: A Single Center Study" Cancers 15, no. 7: 2098. https://doi.org/10.3390/cancers15072098
APA StyleKandil, E., Metz, T. A., Issa, P. P., Aboueisha, M., Omar, M., Attia, A. S., Chabot, B., Hussein, M., Moroz, K., Shama, M., & Toraih, E. (2023). Diagnostic Performance of Afirma and Interpace Diagnostics Genetic Testing in Indeterminate Thyroid Nodules: A Single Center Study. Cancers, 15(7), 2098. https://doi.org/10.3390/cancers15072098







