ITA-IMMUNO-PET: The Role of [18F]FDG PET/CT for Assessing Response to Immunotherapy in Patients with Some Solid Tumors
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
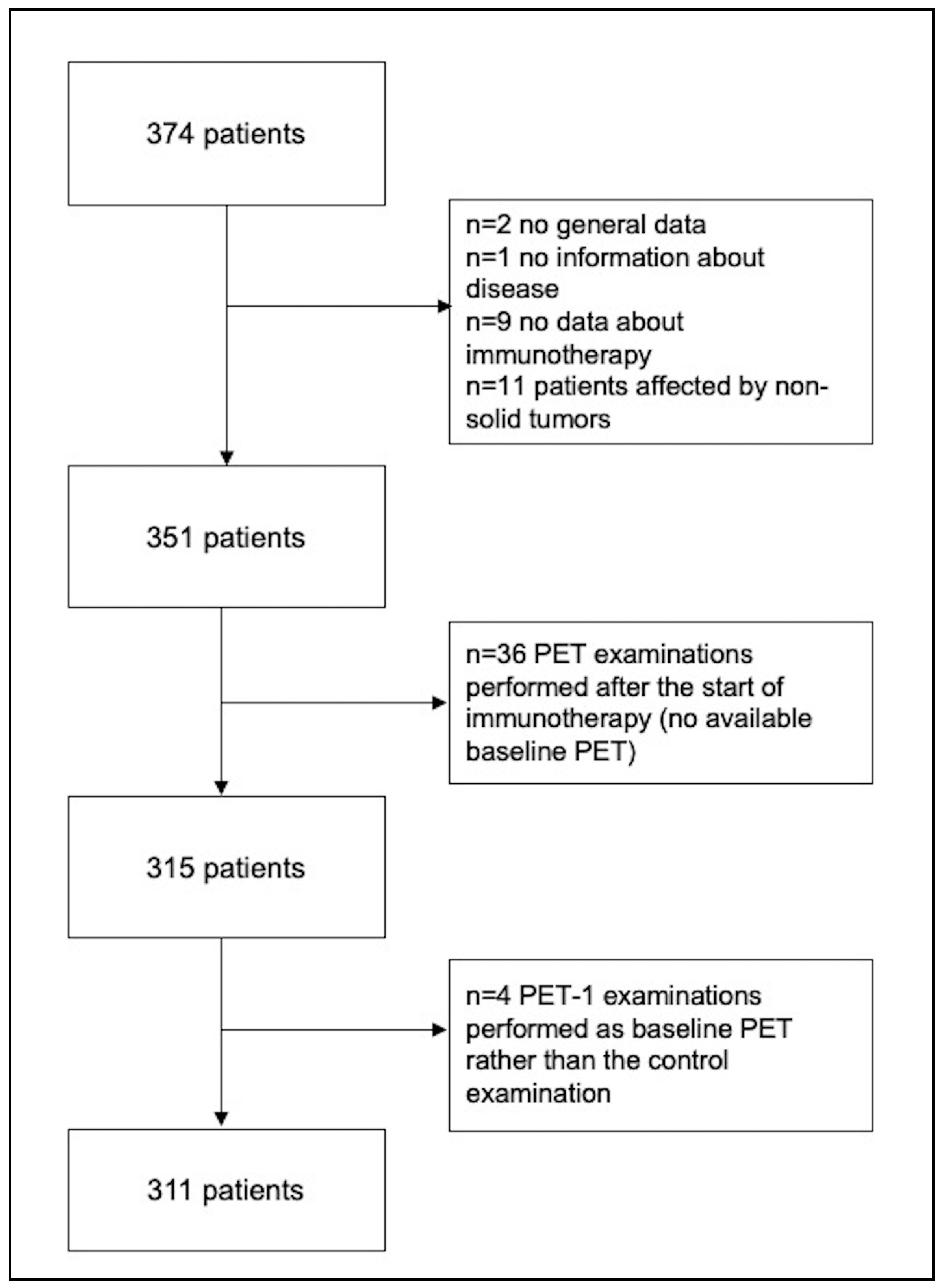
2.1. Study Approval and Patient Population
2.2. Patient Population
2.3. PET/CT Equipment and Image Acquisition Protocol
2.4. Interpretation of PET/CT Images
2.5. Clinical Response to Immunotherapy
2.6. Follow-Up
2.7. Statistical Analysis
3. Results
3.1. Patient Population
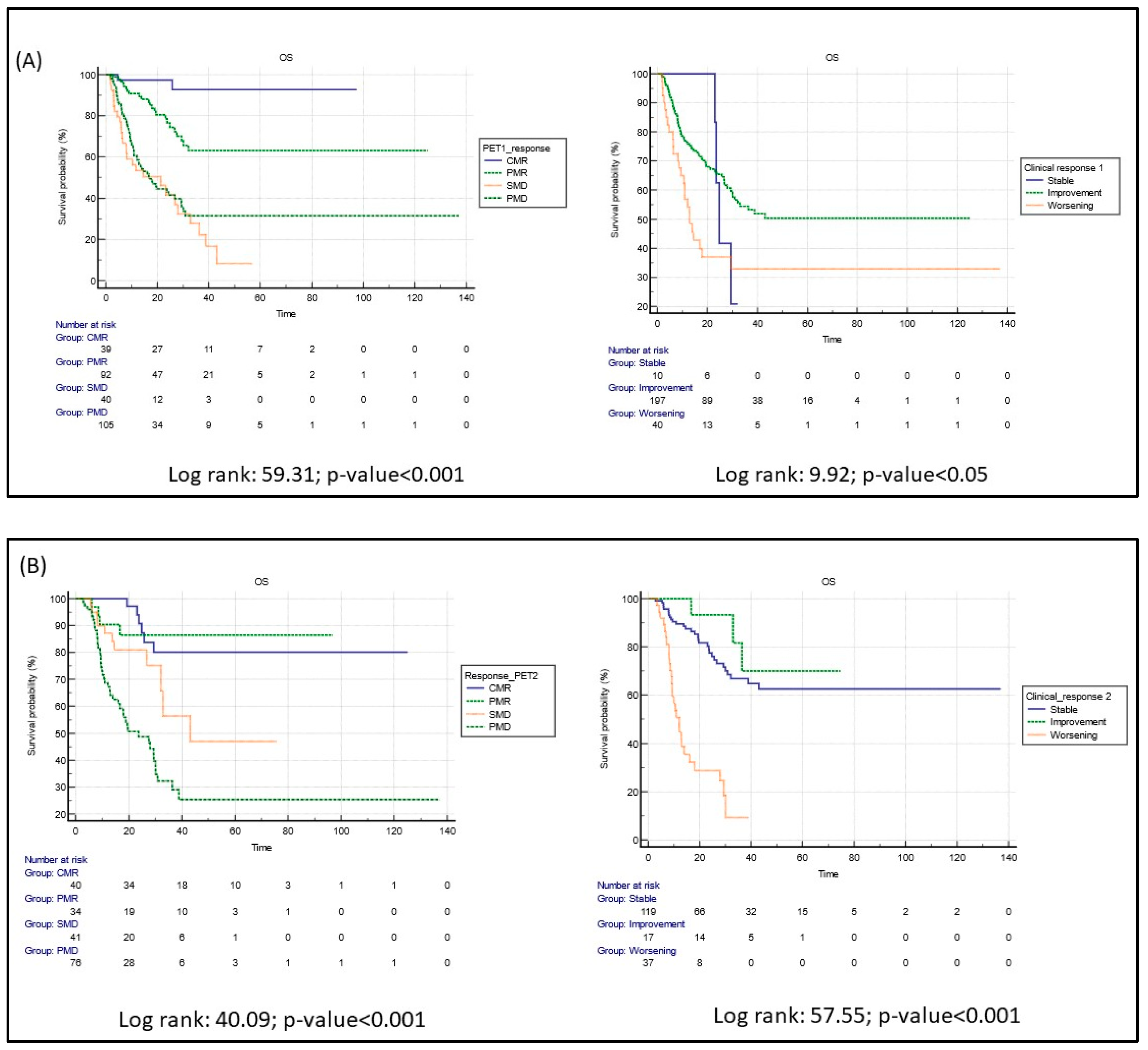
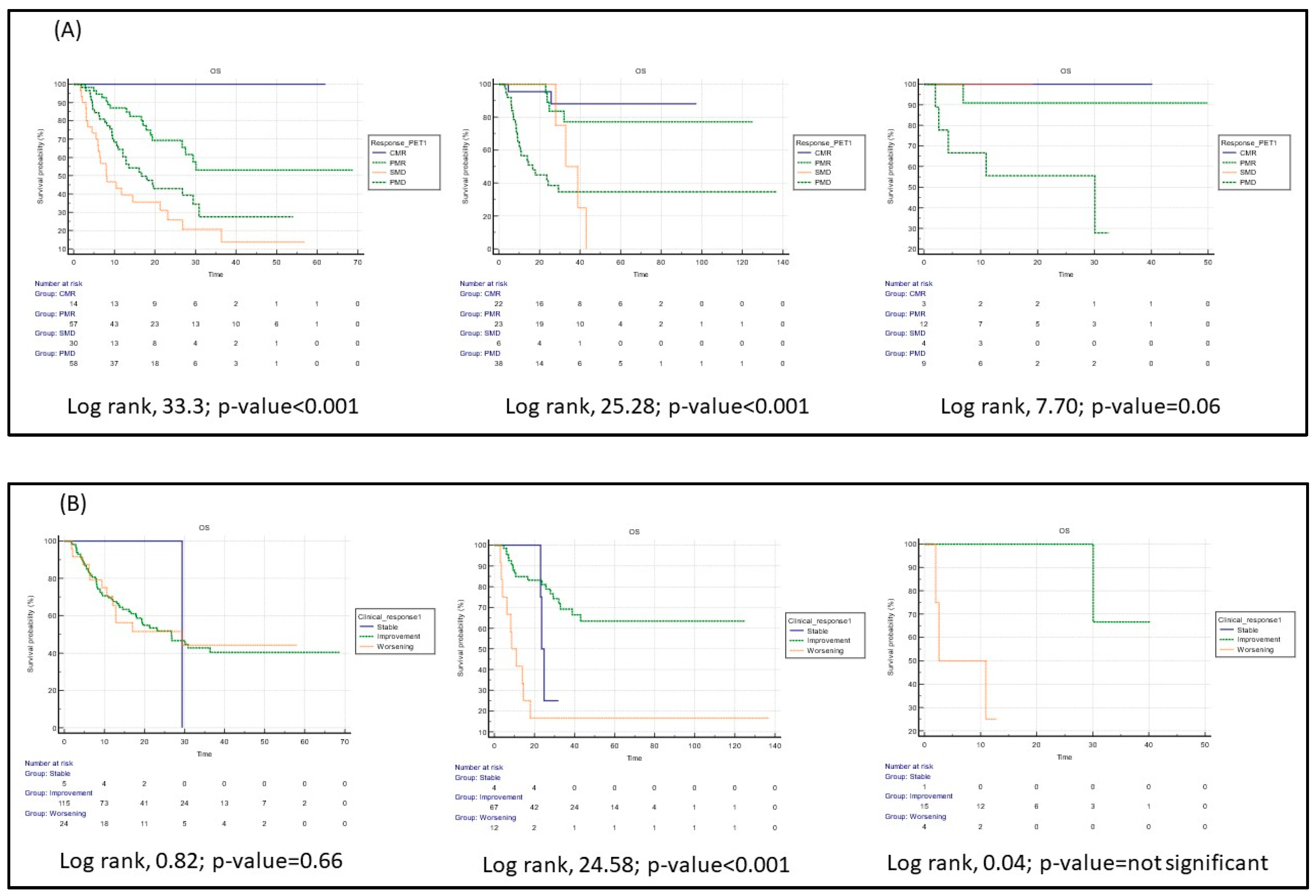
3.2. Clinical and PET/CT Response to Immunotherapy
3.3. Follow-Up
3.4. Inflammatory Side Effects of Immunotherapy and [18F]FDG PET/CT
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Holt, G.E.; Podack, E.R.; Raez, L.E. Immunotherapy as a strategy for the treatment of non-small-cell lung cancer. Therapy 2011, 8, 43–54. [Google Scholar] [CrossRef] [PubMed]
- Sharma, P.; Wagner, K.; Wolchok, J.D.; Allison, J.P. Novel cancer immunotherapy agents with survival benefit: Recent successes and next steps. Nat. Rev. Cancer 2011, 11, 805–812. [Google Scholar] [CrossRef] [PubMed]
- Antonia, S.; Goldberg, S.B.; Balmanoukian, A.; Chaft, J.E.; Sanborn, R.E.; Gupta, A.; Narwal, R.; Steele, K.; Gu, Y.; Karakunnel, J.J.; et al. Safety and antitumour activity of durvalumab plus tremelimumab in non-small cell lung cancer: A multicentre, phase 1b study. Lancet Oncol. 2016, 17, 299–308. [Google Scholar] [CrossRef]
- Postow, M.A.; Chesney, J.; Pavlick, A.C.; Robert, C.; Grossmann, K.; McDermott, D.; Linette, G.P.; Meyer, N.; Giguere, J.K.; Agarwala, S.S.; et al. Nivolumab and Ipilimumab versus Ipilimumab in Untreated Melanoma. N. Engl. J. Med. 2015, 372, 2006–2017. [Google Scholar] [CrossRef] [PubMed]
- Reck, M.; Bondarenko, I.; Luft, A.; Serwatowski, P.; Barlesi, F.; Chacko, R.; Sebastian, M.; Lu, H.; Cuillerot, J.M.; Lynch, T.J. Ipilimumab in combination with paclitaxel and car-boplatin as first-line therapy in extensive-disease-small-cell lung cancer: Results from a randomized, double-blind, multicenter phase 2 trial. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2013, 24, 75–83. [Google Scholar] [CrossRef]
- Lynch, T.J.; Bondarenko, I.; Luft, A.; Serwatowski, P.; Barlesi, F.; Chacko, R.; Sebastian, M.; Neal, J.; Lu, H.; Cuillerot, J.M.; et al. Ipilimumab in combination with paclitaxel and car-boplatin as first-line treatment in stage IIIB/IV non-small-cell lung cancer: Results from a randomized, double-blind, multicenter phase II study. J. Clin. Oncol. 2012, 30, 2046–2054. [Google Scholar] [CrossRef]
- Larkin, J.; Chiarion-Sileni, V.; Gonzalez, R.; Grob, J.-J.; Cowey, C.L.; Lao, C.D.; Schadendorf, D.; Dummer, R.; Smylie, M.; Rutkowski, P.; et al. Combined Nivolumab and Ipilimumab or Monotherapy in Untreated Melanoma. N. Engl. J. Med. 2015, 373, 23–34. [Google Scholar] [CrossRef]
- Annovazzi, A.; Vari, S.; Giannarelli, D.; Pasqualoni, R.; Sciuto, R.; Carpano, S.; Cognetti, F.; Ferraresi, V. Comparison of 18F-FDG PET/CT Criteria for the Prediction of Therapy Response and Clinical Outcome in Patients With Metastatic Melanoma Treated With Ipilimumab and PD-1 Inhibitors. Clin. Nucl. Med. 2020, 45, 187–194. [Google Scholar] [CrossRef]
- Postow, M.A.; Sidlow, R.; Hellmann, M.D. Immune-Related Adverse Events Associated with Immune Checkpoint Blockade. N. Engl. J. Med. 2018, 378, 158–168. [Google Scholar] [CrossRef]
- Seymour, L.; Bogaerts, J.; Perrone, A.; Ford, R.; Schwartz, L.H.; Mandrekar, S.; Lin, N.U.; Litière, S.; Dancey, J.; Chen, A.; et al. iRECIST: Guidelines for response criteria for use in trials testing immunotherapeutics. Lancet Oncol. 2017, 18, e143–e152. [Google Scholar] [CrossRef]
- Cho, S.Y.; Lipson, E.J.; Im, H.-J.; Rowe, S.P.; Gonzalez, E.M.; Blackford, A.; Chirindel, A.; Pardoll, D.M.; Topalian, S.L.; Wahl, R.L. Prediction of Response to Immune Checkpoint Inhibitor Therapy Using Early-Time-Point18F-FDG PET/CT Imaging in Patients with Advanced Melanoma. J. Nucl. Med. 2017, 58, 1421–1428. [Google Scholar] [CrossRef] [PubMed]
- Sachpekidis, C.; Larribere, L.; Pan, L.; Haberkorn, U.; Dimitrakopoulou-Strauss, A.; Hassel, J.C. Predictive value of early 18F-FDG PET/CT studies for treatment response evaluation to ipilimumab in metastatic melanoma: Preliminary results of an ongoing study. Eur. J. Nucl. Med. Mol. Imaging 2015, 42, 386–396. [Google Scholar] [CrossRef] [PubMed]
- Anwar, H.; Sachpekidis, C.; Winkler, J.; Kopp-Schneider, A.; Haberkorn, U.; Hassel, J.C.; Dimitrakopoulou-Strauss, A. Absolute number of new lesions on 18F-FDG PET/CT is more predictive of clinical response than SUV changes in metastatic melanoma patients receiving ipili-mumab. Eur. J. Nucl. Med. Mol. Imaging 2018, 45, 376–383. [Google Scholar] [CrossRef] [PubMed]
- Cheson, B.D.; Ansell, S.; Schwartz, L.; Gordon, L.I.; Advani, R.; Jacene, H.A.; Hoos, A.; Barrington, S.F.; Armand, P. Refinement of the Lugano Classification lymphoma response criteria in the era of immunomodulatory therapy. Blood 2016, 128, 2489–2496. [Google Scholar] [CrossRef] [PubMed]
- Ito, K.; Teng, R.; Schöder, H.; Humm, J.L.; Ni, A.; Michaud, L.; Nakajima, R.; Yamashita, R.; Wolchok, J.D.; Weber, W.A. 18F-FDG PET/CT for Monitoring of Ipilimumab Therapy in Patients with Metastatic Melanoma. J. Nucl. Med. 2019, 60, 335–341. [Google Scholar] [CrossRef]
- Seban, R.-D.; Assié, J.-B.; Giroux-Leprieur, E.; Massiani, M.-A.; Soussan, M.; Bonardel, G.; Chouaid, C.; Playe, M.; Goldfarb, L.; Duchemann, B.; et al. Association of the Metabolic Score Using Baseline FDG-PET/CT and dNLR with Immunotherapy Outcomes in Advanced NSCLC Patients Treated with First-Line Pembrolizumab. Cancers 2020, 12, 2234. [Google Scholar] [CrossRef] [PubMed]
- Grizzi, F.; Castello, A.; Lopci, E. Is it time to change our vision of tumor metabolism prior to immunotherapy? Eur. J. Nucl. Med. Mol. Imaging 2018, 45, 1072–1075. [Google Scholar] [CrossRef]
- Castello, A.; Rossi, S.; Toschi, L.; Lopci, E. Comparison of Metabolic and Morphological Response Criteria for Early Prediction of Response and Survival in NSCLC Patients Treated With Anti-PD-1/PD-L1. Front. Oncol. 2020, 10, 1090. [Google Scholar] [CrossRef]
- Castello, A.; Toschi, L.; Rossi, S.; Mazziotti, E.; Lopci, E. The immune-metabolic-prognostic index and clinical outcomes in patients with non-small cell lung carcinoma under checkpoint inhibitors. J. Cancer Res. Clin. Oncol. 2020, 146, 1235–1243. [Google Scholar] [CrossRef]
- Boellaard, R.; Delgado-Bolton, R.; Oyen, W.J.G.; Giammarile, F.; Tatsch, K.; Eschner, W.; Verzijlbergen, F.J.; Barrington, S.F.; Pike, L.C.; Weber, W.A.; et al. FDG PET/CT: EANM procedure guidelines for tumour imaging: Version 2.0. Eur. J. Nucl. Med. Mol. Imaging 2015, 42, 328–354. [Google Scholar] [CrossRef]
- Price, P.; Jones, T. Can positron emission tomography (PET) be used to detect subclinical response to cancer therapy? The EC PET Oncology Concerted Action and the EORTC PET Study Group. Eur. J. Cancer 1995, 31A, 1924–1927. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Kim, B.J.; Jang, H.J.; Kim, H.S. Comparison of the RECIST and EORTC PET criteria in the tumor response assessment: A pooled analysis and review. Cancer Chemother. Pharmacol. 2017, 80, 729–735. [Google Scholar] [CrossRef] [PubMed]
- Rossi, G.; Bauckneht, M.; Genova, C.; Rijavec, E.; Biello, F.; Mennella, S.; Dal Bello, M.G.; Cittadini, G.; Bruzzi, P.; Piva, R.; et al. Comparison Between 18F-FDG PET-Based and CT-Based Criteria in Non-Small Cell Lung Cancer Patients Treated with Nivolumab. J. Nucl. Med. 2020, 61, 990–998. [Google Scholar] [CrossRef] [PubMed]
- Woolf, S.H.; Grol, R.; Hutchinson, A.; Eccles, M.; Grimshaw, J. Clinical guidelines: Potential benefits, limitations, and harms of clinical guidelines. BMJ 1999, 318, 527–530. [Google Scholar] [CrossRef] [PubMed]
- Annovazzi, A.; Ferraresi, V.; De Rimini, M.L.; Sciuto, R. 18F-FDG PET/CT in the clinical-diagnostic workup of patients treated with immunotherapy: When and how? Clin. Transl. Imaging 2022, 10, 325–329. [Google Scholar] [CrossRef]
- Sachpekidis, C.; Anwar, H.; Winkler, J.; Kopp-Schneider, A.; Larribere, L.; Haberkorn, U.; Hassel, J.C.; Dimitrakopoulou-Strauss, A. The role of interim 18F-FDG PET/CT in prediction of response to ipilimumab treatment in metastatic melanoma. Eur. J. Nucl. Med. Mol. Imaging 2018, 45, 1289–1296. [Google Scholar] [CrossRef]
- Ayati, N.; Sadeghi, R.; Kiamanesh, Z.; Lee, S.T.; Zakavi, S.R.; Scott, A.M. The value of 18F-FDG PET/CT for predicting or monitoring immunotherapy response in patients with metastatic melanoma: A systematic review and meta-analysis. Eur. J. Nucl. Med. Mol. Imaging 2020, 48, 428–448. [Google Scholar] [CrossRef]
- Goldfarb, L.; Duchemann, B.; Chouahnia, K.; Zelek, L.; Soussan, M. Monitoring anti-PD-1-based immunotherapy in non-small cell lung cancer with FDG PET: Introduction of iPERCIST. EJNMMI Res. 2019, 9, 8–10. [Google Scholar] [CrossRef]
- Lopci, E.; Hicks, R.J.; Dimitrakopoulou-Strauss, A.; Dercle, L.; Iravani, A.; Seban, R.D.; Sachpekidis, C.; Humbert, O.; Gheysens, O.; Glaudemans, A.W.J.M.; et al. Joint EANM/SNMMI/ANZSNM practice guidelines/procedure standards on recommended use of [18F]FDG PET/CT imaging during immunomodulatory treatments in patients with solid tumors version 1.0. Eur. J. Nucl. Med. Mol. Imaging 2022, 49, 2323–2341. [Google Scholar] [CrossRef]
- Humbert, O.; Cadour, N.; Paquet, M.; Schiappa, R.; Poudenx, M.; Chardin, D.; Borchiellini, D.; Benisvy, D.; Ouvrier, M.J.; Zwarthoed, C.; et al. 18FDG PET/CT in the early assessment of non-small cell lung cancer response to immunotherapy: Frequency and clinical significance of atypical evolutive patterns. Eur. J. Nucl. Med. Mol. Imaging 2019, 47, 1158–1167. [Google Scholar] [CrossRef]
- Wolchok, J.D.; Hoos, A.; O’Day, S.; Weber, J.S.; Hamid, O.; Lebbé, C.; Maio, M.; Binder, M.; Bohnsack, O.; Nichol, G.; et al. Guidelines for the Evaluation of Immune Therapy Activity in Solid Tumors: Immune-Related Response Criteria. Clin. Cancer Res. 2009, 15, 7412–7420. [Google Scholar] [CrossRef] [PubMed]
- Aide, N.; Hicks, R.J.; Le Tourneau, C.; Lheureux, S.; Fanti, S.; Lopci, E. FDG PET/CT for assessing tumour response to immunotherapy: Report on the EANM symposium on immune modulation and recent review of the literature. Eur. J. Nucl. Med. Mol. Imaging 2019, 46, 238–250. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Shi, Y.; Zhang, D.; Zhou, Q.; Liu, J.; Chen, M.; Xu, Y.; Zhao, J.; Zhong, W.; Wang, M. Risk factors for immune-related adverse events: What have we learned and what lies ahead? Biomark. Res. 2021, 9, 79. [Google Scholar] [CrossRef]
- Topalian, S.L.; Sznol, M.; McDermott, D.F.; Kluger, H.M.; Carvajal, R.D.; Sharfman, W.H.; Brahmer, J.R.; Lawrence, D.P.; Atkins, M.B.; Powderly, J.D.; et al. Survival, Durable Tumor Remission, and Long-Term Safety in Patients With Advanced Melanoma Receiving Nivolumab. J. Clin. Oncol. 2014, 32, 1020–1030. [Google Scholar] [CrossRef] [PubMed]
- Weber, J.S.; Dummer, R.; De Pril, V.; Lebbé, C.; Hodi, F.S. Patterns of onset and resolution of immune-related adverse events of special interest with ipilimumab: Detailed safety analysis from a phase 3 trial in patients with advanced melanoma. Cancer 2013, 119, 1675–1682. [Google Scholar] [CrossRef] [PubMed]
- Lang, N.; Dick, J.; Slynko, A.; Schulz, C.; Dimitrakopoulou-Strauss, A.; Sachpekidis, C.; Enk, A.H.; Hassel, J.C. Clinical significance of signs of autoimmune colitis in 18F-fluorodeoxyglucose positron emission tomography-computed tomography of 100 stage-IV melanoma patients. Immunotherapy 2019, 11, 667–676. [Google Scholar] [CrossRef]
- Wong, A.N.M.; McArthur, G.A.; Hofman, M.S.; Hicks, R.J. The Advantages and Challenges of Using FDG PET/CT for Response As-sessment in Melanoma in the Era of Targeted Agents and Immunotherapy. Eur. J. Nucl. Med. Mol. Imaging 2017, 44, 67–77. [Google Scholar] [CrossRef]
| Variables | All Patients | Lung Cancer | Malignant Melanoma | Others |
|---|---|---|---|---|
| n | 311 | 177 | 101 | 33 |
| Median age (range), years | 67 (31–89) | 68 (44–86) | 67 (31–89) | 67 (35–84) |
| Type of disease, n (%) | ||||
| Lung cancer | 177 (56.9%) | 177 (100%) | - | - |
| Melanoma | 101 (32.5%) | - | 101 (100%) | - |
| Other solid cancers | ||||
| Genito-urinary | 11 (3.5%) | - | - | 11 (33.3%) |
| Head and neck | 13 (4.2%) | - | - | 13 (39.3%) |
| Breast cancer | 3 (1%) | - | - | 3 (9.2%) |
| Gastrointestinal tract | 6 (2%) | - | - | 6 (18.2%) |
| Comorbidity, n (%) | ||||
| No | 71 (22.8%) | 59 (33%) | 4 (4%) | 8 (24%) |
| Yes | 135 (43.4%) | 84 (48%) | 34 (34%) | 17 (52%) |
| Not available | 105 (33.8%) | 34 (19%) | 63 (63%) | 8 (24%) |
| Treatments before immunotherapy, n (%) | ||||
| No | 18 (5.8%) | 18 (10.2%) | 0 | 0 |
| Yes | ||||
| Surgery | 180 (57.9%) | 54 (30.5%) | 101 (100%) | 25 (75.8%) |
| RT | 46 (14.8%) | 32 (18.1%) | 1 (1%) | 13 (39.4%) |
| Chemotherapy | 162 (52.1%) | 135 (76.3%) | 2 (2%) | 26 (78.8%) |
| Combination of local and systematic therapies | 94 (30.2%) | 67 (37.9%) | 3 (3%) | 24 (72.7%) |
| Not available | 9 (2.9%) | 9 (5.1%) | 0 | 0 |
| Type of immunotherapy, n (%) | ||||
| Atezolizumab | 18 (5.8%) | 14 (7.9%) | 0 | 4 (12.1%) |
| Nivolumab | 144 (46.3%) | 82 (46.3%) | 42 (41.6%) | 20 (60.6%) |
| Durvalumab | 1 (0.3%) | 1 (0.6%) | 0 | 0 |
| Ipilimumab | 20 (6.4%) | 0 | 20 (19.8%) | 0 |
| Pembrolizumab | 126 (40.5%) | 79 (44.6%) | 39 (38.6%) | 8 (24.2%) |
| Cemiplimab | 2 (0.6%) | 1 (0.6%) | 0 | 1 (3%) |
| Rate of immunotherapy administration, n (%) | ||||
| Weekly | 2 (0.6%) | 2 (1%) | 0 | 0 |
| Two-weekly | 113 (36.3%) | 76 (42%) | 19 (19%) | 18 (55%) |
| Three-weekly | 140 (45%) | 86 (49%) | 49 (49%) | 5 (15%) |
| Others | 40 (12.9%) | 10 (6%) | 23 (23%) | 7 (21%) |
| Not available | 16 (5.1%) | 3 (2%) | 10 (10%) | 3 (9%) |
| Combination of immunotherapy and other treatments, n (%) | ||||
| No | 253 (81.4%) | 39 (22%) | 13 (12.9%) | 6 (18.2%) |
| Yes | 58 (18.6%) | 138 (78%) | 88 (87.1%) | 27 (81.8%) |
| Variables | All Patients | Lung Cancer | Malignant Melanoma | Others |
|---|---|---|---|---|
| (n = 311) | (n = 177) | (n = 101) | (n = 33) | |
| PET response 1, n (%) | ||||
| CMR | 44 (14.1%) | 17 (9.6%) | 24 (23.8%) | 3 (9.1%) |
| PMR | 101 (32.5%) | 62 (35%) | 24 (23.8%) | 15 (45.5%) |
| SMD | 44 (14.1%) | 33 (18.6%) | 7 (6.9%) | 4 (12.1%) |
| PMD | 122 (39.2%) | 65 (36.7%) | 46 (45.5%) | 11 (33.3%) |
| Treatment response at PET response 1, n (%) | ||||
| Responders (CMR, PMR) | 145 (46.6%) | 79 (44.6%) | 48 (47.5%) | 18 (54.5%) |
| No responders (SMD, PMD) | 166 (53.4%) | 98 (55.4%) | 53 (52.5%) | 15 (45.5%) |
| Disease control at PET response 1, n (%) | ||||
| Disease control | 189 (60.8%) | 112 (63.3%) | 55 (54.5%) | 22 (66.7%) |
| (CMR, PMR, SMD) | ||||
| No disease control (PMD) | 122 (39.2%) | 65 (36.7%) | 46 (45.5%) | 11 (33.3%) |
| Clinical Response 1, n (%) | ||||
| Stable disease | 10 (3.2%) | 5 (3%) | 4 (4%) | 1 (3%) |
| Clinical improvement | 202 (65%) | 119 (67%) | 67 (66%) | 16 (48%) |
| Clinical worsening | 40 (12.9%) | 24 (14%) | 12 (12%) | 4 (12%) |
| Not available | 59 (19%) | 29 (16%) | 18 (18%) | 12 (36%) |
| Clinical response 1, n (%) | ||||
| Responders | 202 (65%) | 119 (67%) | 67 (66%) | 16 (49%) |
| (improvement) | ||||
| No Responders | 50 (16%) | 29 (17%) | 16 (16%) | 5 (15%) |
| (stable + worsening) | ||||
| Not available | 59 (19%) | 29 (16%) | 18 (18%) | 12 (36%) |
| Disease control at Clinical 1, n (%) | ||||
| Disease control | 212 (68.2%) | 124 (70%) | 71 (70%) | 17 (52%) |
| (stable + improvement) | ||||
| No disease control | 40 (12.9%) | 24 (14%) | 12 (12%) | 4 (12%) |
| (worsening) | ||||
| Not available | 59 (19%) | 29 (16%) | 18 (18%) | 12 (36%) |
| PET response 2, n (%) | ||||
| CMR | 41 (13.2%) | 13 (7%) | 26 (26%) | 2 (6%) |
| PMR | 34 (10.9%) | 18 (10%) | 12 (12%) | 4 (12%) |
| SMD | 42 (13.5%) | 26 (15%) | 12 (12%) | 4 (12%) |
| PMD | 82 (26.4%) | 44 (25%) | 27 (27%) | 11 (33%) |
| Not available | 112 (36%) | 76 (42%) | 35 (35%) | 12 (36%) |
| Treatment response at PET response 2, n (%) | ||||
| Responders (CMR, PMR) | 75 (24.1%) | 31 (17.5%) | 38 (37.6%) | 6 (18.2%) |
| No responders (SMD, PMD) | 124 (39.9%) | 70 (39.5%) | 39 (38.6%) | 15 (45.5%) |
| Not available | 112 (36%) | 76 (42%) | 24 (24%) | 12 (36.4%) |
| Disease control at PET response 2, n (%) | ||||
| Disease control | 117 (37.6%) | 57 (32%) | 50 (50%) | 10 (30%) |
| (CMR, PMR, SMD) | ||||
| No disease control (PMD) | 82 (26.4%) | 44 (25%) | 27 (27%) | 11 (33%) |
| Not available | 112 (36%) | 76 (42%) | 24 (24%) | 12 (36%) |
| Clinical Response 2, n (%) | ||||
| Stable disease | 119 (38.3%) | 55 (31%) | 50 (50%) | 14 (42%) |
| Clinical improvement | 17 (5.5%) | 10 (6%) | 7 (7%) | 0 |
| Clinical worsening | 37 (11.9%) | 21 (12%) | 14 (14%) | 2 (6%) |
| Not available | 138 (44.4%) | 91 (51%) | 24 (24%) | 17 (52%) |
| Clinical response 2, n (%) | ||||
| Responders (improvement) | 17 (5.5%) | 10 (6%) | 7 (7%) | 0 |
| No Responders | 136 (50.1%) | 76 (43%) | 64 (69%) | 16 (48%) |
| (stable + worsening) | ||||
| Not available | 138 (44.4%) | 91 (51%) | 24 (24%) | 17 (52%) |
| Clinical disease control 2 (categorical data), n (%) | ||||
| Disease control | 136 (43.7%) | 65 (37%) | 57 (57%) | 14 (42%) |
| (Stable, improvement) | ||||
| No disease control | 37 (11.9%) | 21 (12%) | 14 (14%) | 2 (6%) |
| (worsening) | ||||
| Not available | 138 (44.4%) | 91 (51%) | 30 (30%) | 17 (52%) |
| PET response 3, n (%) | ||||
| CMR | 25 (8%) | 4 (2%) | 17 (17%) | 4 (12%) |
| PMR | 8 (2.6%) | 4 (2%) | 2 (2%) | 2 (6%) |
| SMD | 35 (11.3%) | 19 (11%) | 12 (12%) | 4 (12%) |
| PMD | 34 (10.9%) | 17 (10%) | 14 (14%) | 3 (9%) |
| Not available | 209 (67.2%) | 133 (75%) | 56 (55%) | 20 (61%) |
| Treatment response at PET response 3, n (%) | ||||
| Responders (CMR, PMR) | 33 (10.6%) | 8 (4.5%) | 19 (18.8%) | 6 (18.2%)] |
| No responders (SMD, PMD) | 69 (22.2%) | 15 (8.5%) | 26 (25.7%) | 7 (21.2%) |
| Not available | 209 (67.2%) | 133 (75%) | 56 (55.4%) | 20 (60.6%) |
| Disease control at PET response 3, n (%) | ||||
| Disease control | 68 (21.9%) | 27 (15%) | 31 (31%) | 10 (30%) |
| (CMR, PMR, SMD) | ||||
| No disease control (PMD) | 34 (10.9%) | 17 (10%) | 14 (14%) | 3 (9%) |
| Not available | 209 (67.2%) | 133 (75%) | 56 (55%) | 20 (61%) |
| Clinical Response 3, n (%) | ||||
| Stable disease | 69 (22.2%) | 26 (15%) | 33 (33%) | 10 (30%) |
| Clinical improvement | 7 (2.3%) | 3 (2%) | 3 (3%) | 1 (3%) |
| Clinical worsening | 9 (2.9%) | 4 (2%) | 4 (4%) | 1 (3%) |
| Not available | 226 (72.7%) | 144 (81%) | 61 (61%) | 21 (64%) |
| Clinical response 3, n (%) | ||||
| Responders (improvement) | 7 (2,3%) | 3 (12%) | 3 (3%) | 1 (3%) |
| No Responders | 78 (25%) | 30 (17%) | 37 (37%) | 11 (33%) |
| (stable + worsening) | ||||
| Not available | 226 (72.7%) | 144 (81%) | 61 (60%) | 21 (64%) |
| Clinical Disease control 3, n (%) | ||||
| Disease control | 76 (24.4%) | 29 (16%) | 36 (36%) | 11 (33%) |
| (Stable, improvement) | ||||
| No disease control (worsening) | 9 (2.9%) | 4 (2%) | 4 (4%) | 1 (3%) |
| Not available | 226 (72.7%) | 144 (81%) | 61 (61%) | 21 (64%) |
| PET response 4, n (%) | ||||
| CMR | 9 (2.9%) | 2 (1%) | 4 (45) | 3 (9%) |
| PMR | 7 (2.3%) | 6 (3%) | 1 (1%) | 0 |
| SMD | 12 (3.9%) | 6 (3%) | 4 (4%) | 2 (6%) |
| PMD | 18 (5.8%) | 9 (5%) | 6 (6%) | 3 (9%) |
| Not available | 265 (85.2%) | 154 (87%) | 86 (85%) | 25 (76%) |
| Treatment response at PET response 4, n (%) | ||||
| Responders (CMR, PMR) | 16 (5.1%) | 8 (4.5%) | 5 (5%) | 3 (9.1%) |
| No responders (SMD, PMD) | 30 (9.6%) | 15 (8.5%) | 10 (9.9%) | 5 (15.2%) |
| Not available | 265 (85.2%) | 154 (87%) | 86 (85.1%) | 25 (75.8%) |
| Disease control at PET response 4, n (%) | ||||
| Disease control | 28 (9%) | 14 (8%) | 9 (9%) | 5 (15%) |
| (CMR, PMR, SMD) | ||||
| No disease control (PMD) | 18 (5.8%) | 9 (5%) | 6 (6%) | 3 (9%) |
| Not available | 265 (85.2%) | 155 (87%) | 86 (85%) | 25 (76%) |
| Clinical Response 4, n (%) | ||||
| Stable disease | 33 (10.6%) | 15 (8%) | 14 (14%) | 4 (12%) |
| Clinical improvement | 3 (1%) | 1 (1%) | 1 (1%) | 1 (3%) |
| Clinical worsening | 4 (1.3%) | 2 (1%) | 2 (2%) | 2 (6%) |
| Not available | 271 (87.1%) | 159 (90%) | 84 (83%) | 26 (79%) |
| Clinical response 4, n (%) | ||||
| Responders (improvement) | 3 (1%) | 1 (0.4%) | 1 (1%) | 1 (3%) |
| No Responders | 37 (11.9%) | 17 (9.6%) | 16 (16%) | 6 (18%) |
| (stable + worsening) | ||||
| Not available | 271 (87.1%) | 159 (90%) | 84 (83%) | 26 (79%) |
| Clinical disease control 4, n (%) | ||||
| Disease control | 36 (11.6%) | 16 (9%) | 15 (16%) | 5 (15%) |
| (Stable, improvement) | ||||
| No disease control (worsening) | 4 (1.3%) | 2 (1%) | 0 | 2 (6%) |
| Not available | 271 (87.1%) | 159 (90%) | 84 (83%) | 26 (79%) |
| PET response 5, n (%) | ||||
| CMR | 5 (1.6%) | 1 (1%) | 2 (2%) | 2 (6%) |
| PMR | 1 (0.3%) | 1 (1%) | 0 | 0 |
| SMD | 8 (2.6%) | 5 (3%) | 3 (3%) | 0 |
| PMD | 9 (2.9%) | 4 (2%) | 2 (2%) | 3 (9%) |
| Not available | 288 (92.6%) | 166 (94%) | 94 (93%) | 28 (85%) |
| Treatment response at PET response 5, n (%) | ||||
| Responders (CMR, PMR) | 6 (1.9%) | 2 (1.1%) | 2 (2%) | 2 (6.1%) |
| No responders (SMD, PMD) | 17 (5.5%) | 9 (5.1%) | 5 (5%) | 3 (9.1%) |
| Not available | 288 (92.6%) | 166 (94%) | 94 (93%) | 28 (84.8%) |
| Disease control at PET response 5, n (%) | ||||
| Disease control | 14 (4.5%) | 7 (4%) | 5 (5%) | 2 (6%) |
| (CMR, PMR, SMD) | ||||
| No disease control (PMD) | 9 (2.9%) | 4 (2%) | 2 (2%) | 3 (9%) |
| Not available | 288 (92.6%) | 166 (94%) | 94 (93%) | 28 (85%) |
| Clinical Response 5, n (%) | ||||
| Stable disease | 20 (6.4%) | 10 (6%) | 7 (7%) | 3 (9%) |
| Clinical worsening | 2 (0.7%) | 0 | 1 (1%) | 1 (3%) |
| Not available | 289 (92.9%) | 167 (94%) | 93 (92%) | 29 (88%) |
| Clinical response 5, n (%) | ||||
| Responders (improvement) | 0 | 0 | 0 | 0 |
| No Responders | 22 (7.1%) | 10 (6%) | 8 (8%) | 4 (12%) |
| (stable + worsening) | ||||
| Not available | 289 (92.9%) | 167 (94%) | 93 (92%) | 29 (88%) |
| Clinical disease control, n (%) | ||||
| Disease control | 20 (6.4%) | 10 (6%) | 7 (7%) | 3 (9%) |
| (Stable, improvement) | ||||
| No disease control (worsening) | 2 (0.6%) | 0 | 1 (1%) | 1 (3%) |
| Not available | 289 (92.9%) | 167 (94%) | 93 (92%) | 29 (88%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Evangelista, L.; Bianchi, A.; Annovazzi, A.; Sciuto, R.; Di Traglia, S.; Bauckneht, M.; Lanfranchi, F.; Morbelli, S.; Nappi, A.G.; Ferrari, C.; et al. ITA-IMMUNO-PET: The Role of [18F]FDG PET/CT for Assessing Response to Immunotherapy in Patients with Some Solid Tumors. Cancers 2023, 15, 878. https://doi.org/10.3390/cancers15030878
Evangelista L, Bianchi A, Annovazzi A, Sciuto R, Di Traglia S, Bauckneht M, Lanfranchi F, Morbelli S, Nappi AG, Ferrari C, et al. ITA-IMMUNO-PET: The Role of [18F]FDG PET/CT for Assessing Response to Immunotherapy in Patients with Some Solid Tumors. Cancers. 2023; 15(3):878. https://doi.org/10.3390/cancers15030878
Chicago/Turabian StyleEvangelista, Laura, Andrea Bianchi, Alessio Annovazzi, Rosa Sciuto, Silvia Di Traglia, Matteo Bauckneht, Francesco Lanfranchi, Silvia Morbelli, Anna Giulia Nappi, Cristina Ferrari, and et al. 2023. "ITA-IMMUNO-PET: The Role of [18F]FDG PET/CT for Assessing Response to Immunotherapy in Patients with Some Solid Tumors" Cancers 15, no. 3: 878. https://doi.org/10.3390/cancers15030878
APA StyleEvangelista, L., Bianchi, A., Annovazzi, A., Sciuto, R., Di Traglia, S., Bauckneht, M., Lanfranchi, F., Morbelli, S., Nappi, A. G., Ferrari, C., Rubini, G., Panareo, S., Urso, L., Bartolomei, M., D’Arienzo, D., Valente, T., Rossetti, V., Caroli, P., Matteucci, F., ... De Rimini, M. L. (2023). ITA-IMMUNO-PET: The Role of [18F]FDG PET/CT for Assessing Response to Immunotherapy in Patients with Some Solid Tumors. Cancers, 15(3), 878. https://doi.org/10.3390/cancers15030878
















