Factors Associated with Total Laryngectomy Utilization in Patients with cT4a Laryngeal Cancer
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source and Patient Selection
2.2. Statistical Analysis
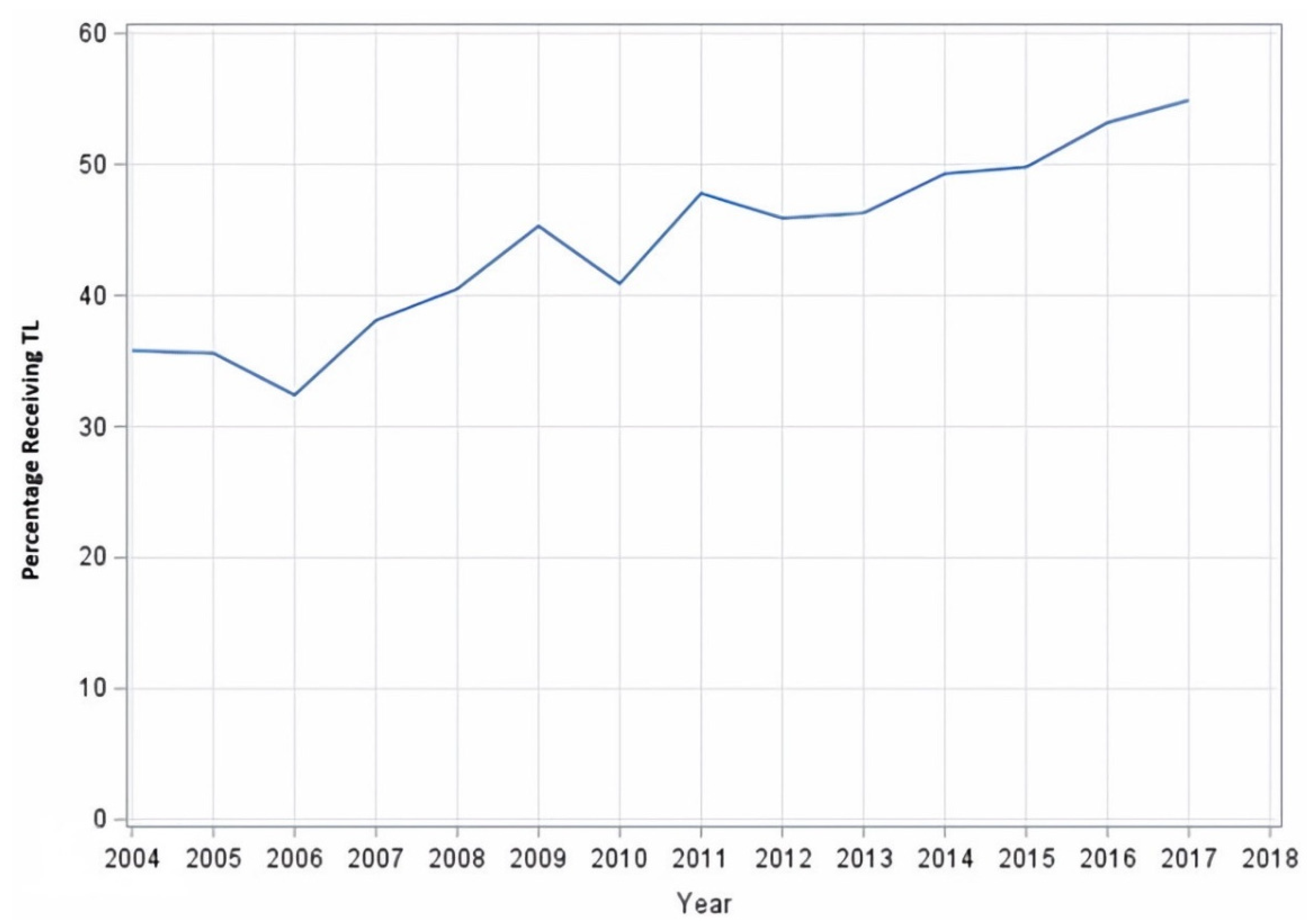
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics. CA Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef] [PubMed]
- Park, J.-O.; Nam, I.-C.; Kim, C.-S.; Park, S.-J.; Lee, D.-H.; Kim, H.-B.; Han, K.-D.; Joo, Y.-H. Sex Differences in the Prevalence of Head and Neck Cancers: A 10-Year Follow-Up Study of 10 Million Healthy People. Cancers 2022, 14, 2521. [Google Scholar] [CrossRef] [PubMed]
- Barul, C.; Fayosse, A.; Carton, M.; Pilorget, C.; Woronoff, A.-S.; Stücker, I.; Luce, D. Occupational exposure to chlorinated solvents and risk of head and neck cancer in men: A population-based case-control study in France. Environ. Health 2017, 16, 77. [Google Scholar] [CrossRef] [PubMed]
- Department of Veterans Affairs Laryngeal Cancer Study Group; Wolf, G.T.; Fisher, S.G.; Hong, W.K.; Hillman, R.; Spaulding, M.; Laramore, G.E.; Endicott, J.W.; McClatchey, K.; Henderson, W.G. Induction Chemotherapy plus Radiation Compared with Surgery plus Radiation in Patients with Advanced Laryngeal Cancer. N. Engl. J. Med. 1991, 324, 1685–1690. [Google Scholar] [CrossRef] [PubMed]
- Forastiere, A.A.; Zhang, Q.; Weber, R.S.; Maor, M.H.; Goepfert, H.; Pajak, T.F.; Morrison, W.; Glisson, B.; Trotti, A.; Ridge, J.A.; et al. Long-Term Results of RTOG 91-11: A Comparison of Three Nonsurgical Treatment Strategies to Preserve the Larynx in Patients with Locally Advanced Larynx Cancer. J. Clin. Oncol. 2013, 31, 845–852. [Google Scholar] [CrossRef]
- Maclean, J.; Cotton, S.; Perry, A. Post-Laryngectomy: It’s hard to swallow: An Australian study of prevalence and self-reports of swallowing function after a total laryngectomy. Dysphagia 2009, 24, 172–179. [Google Scholar] [CrossRef]
- Maclean, J.; Cotton, S.; Perry, A. Dysphagia Following a Total Laryngectomy: The Effect on Quality of Life, Functioning, and Psychological Well-Being. Dysphagia 2009, 24, 314–321. [Google Scholar] [CrossRef]
- Hanna, E.; Sherman, A.; Cash, D.; Adams, D.; Vural, E.; Fan, C.-Y.; Suen, J.Y. Quality of Life for Patients Following Total Laryngectomy vs Chemoradiation for Laryngeal Preservation. Arch. Otolaryngol. Neck Surg. 2004, 130, 875–879. [Google Scholar] [CrossRef]
- Perry, A.; Casey, E.; Cotton, S. Quality of life after total laryngectomy: Functioning, psychological well-being and self-efficacy. Int. J. Lang. Commun. Disord. 2015, 50, 467–475. [Google Scholar] [CrossRef]
- National Comprehensive Cancer Network. Head and Neck Cancers (Version 1.2023). Available online: https://nccn.org/professionals/physician_gls/pdf/head-and-neck.pdf (accessed on 29 January 2023).
- Hoffman, H.T.; Porter, K.; Karnell, L.H.; Cooper, J.S.; Weber, R.S.; Langer, C.J.; Gay, G.; Stewart, A.; Robinson, R.A.; Hoffman, H.T.; et al. Laryngeal Cancer in the United States: Changes in Demographics, Patterns of Care, and Survival. Laryngoscope 2006, 116 Pt 2 (Suppl. S111), 1–13. [Google Scholar] [CrossRef]
- Chen, A.Y.; Fedewa, S.; Zhu, J. Temporal Trends in the Treatment of Early- and Advanced-Stage Laryngeal Cancer in the United States, 1985-2007. Arch. Otolaryngol. Neck Surg. 2011, 137, 1017–1024. [Google Scholar] [CrossRef] [PubMed]
- Jemal, A.; Tiwari, R.C.; Murray, T.; Ghafoor, A.; Samuels, A.; Ward, E.; Feuer, E.J.; Thun, M.J. Cancer Statistics, 2004. CA Cancer J. Clin. 2004, 54, 8–29. [Google Scholar] [CrossRef] [PubMed]
- Olsen, K.D. Reexamining the treatment of advanced laryngeal cancer. Head Neck 2010, 32, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Walker, B.; Schuurman, N.; Auluck, A.; Lear, S.; Rosin, M. Socioeconomic disparities in head and neck cancer patients’ access to cancer treatment centers. Rural. Remote. Health 2017, 17, 4210. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Choi, S.H.; Terrell, J.E.; Fowler, K.E.; McLean, S.A.; Ghanem, T.; Wolf, G.T.; Bradford, C.R.; Taylor, J.; Duffy, S.A. Socioeconomic and Other Demographic Disparities Predicting Survival among Head and Neck Cancer Patients. PLoS ONE 2016, 11, e0149886. [Google Scholar] [CrossRef]
- Gaubatz, M.E.; Bukatko, A.R.; Simpson, M.C.; Polednik, K.M.; Boakye, E.A.; Varvares, M.A.; Osazuwa-Peters, N. Racial and socioeconomic disparities associated with 90-day mortality among patients with head and neck cancer in the United States. Oral Oncol. 2019, 89, 95–101. [Google Scholar] [CrossRef]
- Rotsides, J.M.; Oliver, J.R.; Moses, L.E.; Tam, M.; Li, Z.; Schreiber, D.; Jacobson, A.S.; Hu, K.S.; Givi, B. Socioeconomic and Racial Disparities and Survival of Human Papillomavirus–Associated Oropharyngeal Squamous Cell Carcinoma. Otolaryngol. Head Neck Surg. 2021, 164, 131–138. [Google Scholar] [CrossRef]
- Gourin, C.G.; Podolsky, R.H. Racial Disparities in Patients with Head and Neck Squamous Cell Carcinoma. Laryngoscope 2006, 116, 1093–1106. [Google Scholar] [CrossRef]
- Hayes, D.N.; Peng, G.; Pennella, E.; Hossain, A.; Carter, G.C.; Muehlenbein, C.; Obasaju, C. An exploratory subgroup analysis of race and gender in squamous cancer of the head and neck: Inferior outcomes for African American males in the LORHAN database. Oral Oncol. 2014, 50, 605–610. [Google Scholar] [CrossRef]
- Peterson, C.E.; Khosla, S.; Chen, L.F.; Joslin, C.E.; Davis, F.G.; Fitzgibbon, M.L.; Freels, S.; Hoskins, K. Racial differences in head and neck squamous cell carcinomas among non-Hispanic black and white males identified through the National Cancer Database (1998–2012). J. Cancer Res. Clin. Oncol. 2016, 142, 1715–1726. [Google Scholar] [CrossRef]
- Bach, P.B.; Cramer, L.D.; Warren, J.L.; Begg, C.B. Racial Differences in the Treatment of Early-Stage Lung Cancer. N. Engl. J. Med. 1999, 341, 1198–1205. [Google Scholar] [CrossRef] [PubMed]
- Esnaola, N.F.; Gebregziabher, M.; Knott, K.; Finney, C.; Silvestri, G.A.; Reed, C.E.; Ford, M.E. Underuse of Surgical Resection for Localized, Non–Small Cell Lung Cancer Among Whites and African Americans in South Carolina. Ann. Thorac. Surg. 2008, 86, 220–227, discussion 227. [Google Scholar] [CrossRef] [PubMed]
- Morris, A.M.; Billingsley, K.G.; Baxter, N.N.; Baldwin, L.-M. Racial disparities in rectal cancer treatment: A population-based analysis. Arch. Surg. 2004, 139, 151–155, discussion 156. [Google Scholar] [CrossRef][Green Version]
- Esnaola, N.F.M.; Gebregziabher, M.; Finney, C.M.; Ford, M.E. Underuse of surgical resection in black patients with nonmetastatic colorectal cancer: Location, location, location. Ann. Surg. 2009, 250, 549–557. [Google Scholar] [CrossRef] [PubMed]
- Cooper, G.S.; Yuan, Z.; Landefeld, C.S.; Rimm, A.A. Surgery for colorectal cancer: Race-related differences in rates and survival among Medicare beneficiaries. Am. J. Public Health 1996, 86, 582–586. [Google Scholar] [CrossRef]
- Munir, M.M.; Woldesenbet, S.; Endo, Y.; Moazzam, Z.; Lima, H.A.; Azap, L.; Katayama, E.; Alaimo, L.; Shaikh, C.; Dillhoff, M.; et al. Disparities in Socioeconomic Factors Mediate the Impact of Racial Segregation Among Patients with Hepatopancreaticobiliary Cancer. Ann. Surg. Oncol. 2023, 30, 4826–4835. [Google Scholar] [CrossRef] [PubMed]
- Alty, I.G.; Dee, E.C.; Cusack, J.C.; Blaszkowsky, L.S.; Goldstone, R.N.; Francone, T.D.; Wo, J.Y.; Qadan, M. Refusal of surgery for colon cancer: Sociodemographic disparities and survival implications among US patients with resectable disease. Am. J. Surg. 2021, 221, 39–45. [Google Scholar] [CrossRef]
- Frenkel, C.H.; Brickman, D.S.; Trufan, S.J.; Ward, M.C.; Moeller, B.J.; Carrizosa, D.R.; Sumrall, A.L.; Milas, Z.L. Defining targets to improve care delivery for T4 larynx squamous cell carcinoma. Laryngoscope Investig. Otolaryngol. 2022, 7, 1849–1856. [Google Scholar] [CrossRef]
- Tseng, J.; DiPeri, T.; Chen, Y.; Ben-Shlomo, A.; Shouhed, D.; Phillips, E.H.; Burch, M.; Jain, M. Factors Associated with Non–Operative Management of Resectable Adrenocortical Carcinoma. J. Surg. Res. 2021, 267, 651–659. [Google Scholar] [CrossRef]
- Dursun, F.; Elshabrawy, A.; Wang, H.; Oelsen, J.; Liss, M.; Kaushik, D.; Ramamurthy, C.; Rodriguez, R.; Mansour, A.M. Impact of facility type and volume on survival in patients with metastatic renal cell carcinoma. Can. J. Urol. 2021, 28, 10806–10816. [Google Scholar]
- Du, A.T.; Du, A.T.; Pang, J.C.; Pang, J.C.; Victor, R.; Victor, R.; Meller, L.L.T.; Meller, L.L.T.; Torabi, S.J.; Torabi, S.J.; et al. The Influence of Facility Volume and Type on Skull Base Chordoma Treatment and Outcomes. World Neurosurg. 2022, 166, e561–e567. [Google Scholar] [CrossRef] [PubMed]
- Finks, J.F.; Osborne, N.H.; Birkmeyer, J.D. Trends in Hospital Volume and Operative Mortality for High-Risk Surgery. N. Engl. J. Med. 2011, 364, 2128–2137. [Google Scholar] [CrossRef] [PubMed]
- Birkmeyer, J.D.; Siewers, A.E.; Finlayson, E.V.; Stukel, T.A.; Lucas, F.L.; Batista, I.; Welch, H.G.; Wennberg, D.E. Hospital Volume and Surgical Mortality in the United States. N. Engl. J. Med. 2002, 346, 1128–1137. [Google Scholar] [CrossRef]
- Zattoni, F.; Montebelli, F.; Rossanese, M.; Crestani, A.; Giannarini, G.; Ficarra, V. Should radical prostatectomy be encouraged at any age? A critical non-systematic review. Minerva Urol. Nefrol. 2018, 70, 42–52. [Google Scholar] [CrossRef]
- Raoof, M.; Jacobson, G.; Fong, Y. Medicare Advantage Networks and Access to High-Volume Cancer Surgery Hospitals. Ann. Surg. 2021, 274, e315–e319. [Google Scholar] [CrossRef] [PubMed]
- Vonlanthen, R.; Lodge, P.; Barkun, J.S.; Farges, O.; Rogiers, X.; Soreide, K.; Kehlet, H.; Reynolds, J.V.; Käser, S.A.; Naredi, P.; et al. Toward a Consensus on Centralization in Surgery. Ann. Surg. 2018, 268, 712–724. [Google Scholar] [CrossRef]
- Bristow, R.E.; Chang, J.; Ziogas, A.; Randall, L.M.; Anton-Culver, H. High-volume ovarian cancer care: Survival impact and disparities in access for advanced-stage disease. Gynecol. Oncol. 2014, 132, 403–410. [Google Scholar] [CrossRef] [PubMed]
- Nabi, J.; Tully, K.H.; Cole, A.P.; Marchese, M.; Cone, E.B.; Melnitchouk, N.; Kibel, A.S.; Trinh, Q. Access denied: The relationship between patient insurance status and access to high-volume hospitals. Cancer 2021, 127, 577–585. [Google Scholar] [CrossRef]
- Trinh, Q.-D.; Sun, M.; Sammon, J.; Bianchi, M.; Sukumar, S.; Ghani, K.R.; Jeong, W.; Dabaja, A.; Shariat, S.F.; Perrotte, P.; et al. Disparities in access to care at high-volume institutions for uro-oncologic procedures. Cancer 2012, 118, 4421–4426. [Google Scholar] [CrossRef]
- Voora, R.S.; Panuganti, B.A.; Flagg, M.; Nelson, T.; Kotha, N.V.; Qiao, E.M.; Qian, A.S.; Kumar, A.; Stewart, T.F.; Rose, B.; et al. Patterns of Failure After Definitive Treatment of T4a Larynx Cancer. Otolaryngol. Head Neck Surg. 2022, 167, 274–285. [Google Scholar] [CrossRef]
- Grover, S.; Swisher-McClure, S.; Mitra, N.; Li, J.; Cohen, R.B.; Ahn, P.H.; Lukens, J.N.; Chalian, A.A.; Weinstein, G.S.; O’Malley, B.W.; et al. Total Laryngectomy Versus Larynx Preservation for T4a Larynx Cancer: Patterns of Care and Survival Outcomes. Int. J. Radiat. Oncol. Biol. Phys. 2015, 92, 594–601. [Google Scholar] [CrossRef] [PubMed]
- Yang, R.; Lubek, J.; Dyalram, D.; Liu, X.; Ord, R. Head and neck cancer surgery in an elderly patient population: A retrospective review. Int. J. Oral Maxillofac. Surg. 2014, 43, 1413–1417. [Google Scholar] [CrossRef] [PubMed]
- Riall, T.S. What is the Effect of Age on Pancreatic Resection? Adv. Surg. 2009, 43, 233–249. [Google Scholar] [CrossRef] [PubMed]
- Park, S.J.; Mun, J.; Yim, G.W.; Lee, M.; Chung, H.H.; Kim, J.W.; Park, N.H.; Song, Y.S.; Kim, H.S. Is increased chronological age a contraindication to debulking surgery for elderly patients with advanced ovarian cancer? J. Obstet. Gynaecol. 2022, 42, 3254–3259. [Google Scholar] [CrossRef] [PubMed]
- Van Cleave, J.H.; Egleston, B.L.; McCorkle, R. Factors Affecting Recovery of Functional Status in Older Adults after Cancer Surgery. J. Am. Geriatr. Soc. 2011, 59, 34–43. [Google Scholar] [CrossRef] [PubMed]
- Bates, J.E.; Amdur, R.J.; Morris, C.M.; Hitchcock, K.E.; Dziegielewski, P.T.; Boyce, B.J.; Silver, N.L.; Shaw, C.; Mendenhall, W.M. Curative-dose Chemoradiotherapy Versus Total Laryngectomy for Stage T3-T4 Squamous Cell Carcinoma of the Larynx: An “Apples-to-Apples” Analysis of the National Cancer Database. Am. J. Clin. Oncol. 2019, 42, 527–533. [Google Scholar] [CrossRef] [PubMed]
- Megwalu, U.C.; Sikora, A.G. Survival Outcomes in Advanced Laryngeal Cancer. JAMA Otolaryngol. Head Neck Surg. 2014, 140, 855–860. [Google Scholar] [CrossRef]
- O’Neill, C.B.; O’Neill, J.P.; Atoria, C.L.; Baxi, S.S.; Henman, M.C.; Ganly, I.; Elkin, E.B. Treatment complications and survival in advanced laryngeal cancer: A population-based analysis. Laryngoscope 2014, 124, 2707–2713. [Google Scholar] [CrossRef]
- Gourin, C.G.; Conger, B.T.; Sheils, W.C.; Bilodeau, P.A.; Coleman, T.A.; Porubsky, E.S. The Effect of treatment on survival in patients with advanced laryngeal carcinoma. Laryngoscope 2009, 119, 1312–1317. [Google Scholar] [CrossRef]
- Ragin, C.C.; Taioli, E. Survival of squamous cell carcinoma of the head and neck in relation to human papillomavirus infection: Review and meta-analysis. Int. J. Cancer 2007, 121, 1813–1820. [Google Scholar] [CrossRef]
- Fakhry, C.; Westra, W.H.; Li, S.; Cmelak, A.; Ridge, J.A.; Pinto, H.; Forastiere, A.; Gillison, M.L. Improved Survival of Patients with Human Papillomavirus-Positive Head and Neck Squamous Cell Carcinoma in a Prospective Clinical Trial. J. Natl. Cancer Inst. 2008, 100, 261–269. [Google Scholar] [CrossRef] [PubMed]

| Variable | No Total Laryngectomy (n = 6100) | Total Laryngectomy (n = 5049) | Total (n = 11,149) | p-Value | |
|---|---|---|---|---|---|
| Facility Type | Community Cancer Program | 374 (6%) | 146 (3%) | 520 (5%) | <0.001 |
| Comprehensive Community Cancer Program | 2143 (35%) | 978 (20%) | 3121 (28%) | ||
| Academic/Research Program | 2423 (40%) | 3195 (64%) | 5618 (51%) | ||
| Integrated Network Cancer Program | 1107 (18%) | 661 (13%) | 1768 (16%) | ||
| Facility Location | New England | 309 (5%) | 176 (4%) | 485 (4%) | <0.001 |
| Middle Atlantic | 955 (16%) | 683 (14%) | 1638 (15%) | ||
| South Atlantic | 1498 (25%) | 1229 (25%) | 2727 (25%) | ||
| East North Central | 1166 (19%) | 990 (20%) | 2156 (20%) | ||
| East South Central | 599 (10%) | 395 (8%) | 994 (9%) | ||
| West North Central | 399 (7%) | 425 (9%) | 824 (7%) | ||
| West South Central | 506 (8%) | 531 (11%) | 1037 (9%) | ||
| Mountain | 209 (3%) | 140 (3%) | 349 (3%) | ||
| Pacific | 406 (7%) | 411 (8%) | 817 (7%) | ||
| Age at Diagnosis | Mean (SD) | 63 (11.1) | 61 (10.1) | 62 (10.7) | <0.001 |
| Sex | Male | 4808 (79%) | 4176 (83%) | 8984 (81%) | <0.001 |
| Female | 1292 (21%) | 873 (17%) | 2165 (19%) | ||
| Race | White | 4726 (77%) | 3976 (79%) | 8702 (78%) | 0.243 |
| Black | 1212 (20%) | 953 (19%) | 2165 (19%) | ||
| Other/Unknown | 162 (3%) | 120 (2%) | 282 (3%) | ||
| Ethnicity | Non-Hispanic | 5450 (89%) | 4581 (91%) | 10,031 (90%) | 0.001 |
| Hispanic | 367 (6%) | 301 (6%) | 668 (6%) | ||
| Unknown | 283 (5%) | 167 (3%) | 450 (4%) | ||
| Insurance Type | Private Insurance/Managed Care | 1507 (25%) | 1276 (25%) | 2783 (25%) | <0.001 |
| Not Insured | 583 (10%) | 453 (9%) | 1036 (9%) | ||
| Medicaid | 1132 (19%) | 1225 (24%) | 2357 (21%) | ||
| Medicare | 2589 (42%) | 1904 (38%) | 4493 (40%) | ||
| Other Government | 136 (2%) | 96 (2%) | 232 (2%) | ||
| Unknown | 153 (3%) | 95 (2%) | 248 (2%) | ||
| Percentage with No High School Degree | ≥21.0% | 1521 (27%) | 1250 (28%) | 2771 (27%) | 0.107 |
| 13.0–20.9% | 1821 (32%) | 1501 (33%) | 3322 (33%) | ||
| 7.0–12.9% | 1595 (28%) | 1222 (27%) | 2817 (28%) | ||
| <7.0% | 762 (13%) | 547 (12%) | 1309 (13%) | ||
| Annual Income | 1st Quartile | 1508 (27%) | 1086 (25%) | 2594 (26%) | 0.010 |
| 2nd Quartile | 1564 (28%) | 1271 (29%) | 2835 (28%) | ||
| 3rd Quartile | 1211 (22%) | 1053 (24%) | 2264 (23%) | ||
| 4th Quartile | 1290 (23%) | 1006 (23%) | 2296 (23%) | ||
| County Categorization | Metro | 4812 (81%) | 3836 (78%) | 8648 (80%) | <0.001 |
| Urban | 968 (16%) | 941 (19%) | 1909 (18%) | ||
| Rural | 157 (3%) | 131 (3%) | 288 (3%) | ||
| Distance from patient’s residence to hospital (miles) | <5 | 2125 (35%) | 1429 (28%) | 3554 (32%) | <0.001 |
| 5–30 | 2800 (46%) | 1961 (39%) | 4761 (43%) | ||
| >30 | 1175 (19%) | 1659 (33%) | 2834 (25%) | ||
| Charlson-Deyo Comorbidity Score | 0 | 3942 (65%) | 3119 (62%) | 7061 (63%) | <0.001 |
| 1 | 1475 (24%) | 1399 (28%) | 2874 (26%) | ||
| 2 | 465 (8%) | 375 (7%) | 840 (8%) | ||
| 3+ | 218 (4%) | 156 (3%) | 374 (3%) | ||
| Diagnosis Year | 2004–2010 | 2866 (47%) | 1821 (36%) | 4687 (42%) | <0.001 |
| 2011–2017 | 3234 (53%) | 3228 (64%) | 6462 (58%) | ||
| Primary Site | Glottis | 1342 (22%) | 1581 (31%) | 2923 (26%) | <0.001 |
| Supraglottis | 3065 (50%) | 1631 (32%) | 4696 (42%) | ||
| Subglottis | 235 (4%) | 232 (5%) | 467 (4%) | ||
| Laryngeal Cartilage | 9 (0%) | 4 (0%) | 13 (0%) | ||
| Overlapping sites of the Larynx | 327 (5%) | 726 (14%) | 1053 (9%) | ||
| Larynx, NOS | 1122 (18%) | 875 (17%) | 1997 (18%) | ||
| Clinical nodal stage | N0 | 2478 (52%) | 2640 (63%) | 5118 (57%) | <0.001 |
| N1 | 851 (18%) | 645 (15%) | 1496 (17%) | ||
| N2 | 1218 (25%) | 848 (20%) | 2066 (23%) | ||
| N3 | 230 (5%) | 49 (1%) | 279 (3%) | ||
| Lymphovascular Space Invasion | Not present | 551 (89%) | 2005 (63%) | 2556 (67%) | <0.001 |
| Present | 69 (11%) | 1195 (37%) | 1264 (33%) | ||
| Regional lymph node surgery | No | 5800 (96%) | 441 (9%) | 6241 (56%) | <0.001 |
| Yes | 256 (4%) | 4594 (91%) | 4850 (44%) | ||
| Primary Site Surgery | No | 6014 (100%) | 0 (0%) | 6014 (54%) | <0.001 |
| Yes | 0 (0%) | 5049 (100%) | 5049 (46%) | ||
| Timing of radiation and surgery | No radiation and/or surgery | 5880 (99%) | 1520 (31%) | 7400 (69%) | <0.001 |
| Radiation before surgery | 10 (0%) | 140 (3%) | 150 (1%) | ||
| Radiation after surgery | 30 (1%) | 3219 (66%) | 3249 (30%) | ||
| Chemotherapy | No | 1171 (22%) | 2721 (61%) | 3892 (40%) | <0.001 |
| Yes | 4200 (78%) | 1718 (39%) | 5918 (60%) | ||
| Tumor HPV Category | Negative | 782 (13%) | 781 (16%) | 1563 (14%) | <0.001 |
| Positive | 200 (3%) | 147 (3%) | 347 (3%) | ||
| Unknown | 5075 (84%) | 4108 (82%) | 9183 (83%) | ||
| Total Dose of Radiation (cGy) | Mean (SD) | 7587 (8455) | 6840 (7440.3) | 7183.8 (7928.4) | 0.125 |
| Variable | Odds Ratio | 95% LCI | 95% UCI | p-Value | |
|---|---|---|---|---|---|
| Age | ≤61 years | REF | |||
| >61 years | 0.81 | 0.72 | 0.91 | <0.001 | |
| Facility Type | Community Cancer Program | REF | |||
| Comprehensive Community Cancer Program | 1.10 | 0.85 | 1.41 | 0.477 | |
| Academic/Research Program | 3.06 | 2.39 | 3.92 | <0.001 | |
| Integrated Network Cancer Program | 1.50 | 1.15 | 1.96 | 0.003 | |
| Facility Location | New England | REF | |||
| Middle Atlantic | 1.00 | 0.76 | 1.32 | 0.989 | |
| South Atlantic | 1.24 | 0.94 | 1.62 | 0.124 | |
| East North Central | 1.22 | 0.93 | 1.61 | 0.147 | |
| East South Central | 0.87 | 0.64 | 1.18 | 0.356 | |
| West North Central | 1.58 | 1.16 | 2.16 | 0.004 | |
| West South Central | 1.52 | 1.13 | 2.05 | 0.006 | |
| Mountain | 1.07 | 0.73 | 1.56 | 0.747 | |
| Pacific | 1.46 | 1.08 | 1.97 | 0.014 | |
| Sex | Female | REF | |||
| Male | 1.19 | 1.05 | 1.36 | 0.001 | |
| Ethnicity | Non-Hispanic | REF | |||
| Hispanic | 0.84 | 0.68 | 1.04 | 0.102 | |
| Unknown | 1.04 | 0.82 | 1.33 | 0.732 | |
| Insurance Type | Private Insurance/Managed Care | REF | |||
| Not Insured | 0.91 | 0.75 | 1.10 | 0.337 | |
| Medicaid | 1.31 | 1.12 | 1.52 | <0.001 | |
| Medicare | 0.97 | 0.84 | 1.11 | 0.628 | |
| Other Government | 0.83 | 0.56 | 1.22 | 0.345 | |
| Insurance Status Unknown | 0.66 | 0.48 | 0.93 | 0.016 | |
| Educational Attainment (Percent No High School Degree 2008–2012) | ≥21.0% | REF | |||
| 13.0–20.9% | 1.01 | 0.88 | 1.16 | 0.897 | |
| 7.0–12.9% | 1.01 | 0.85 | 1.18 | 0.950 | |
| <7.0% | 1.00 | 0.80 | 1.23 | 0.962 | |
| Income | 1st Quartile | REF | |||
| 2nd Quartile | 1.13 | 0.97 | 1.32 | 0.110 | |
| 3rd Quartile | 1.20 | 1.00 | 1.42 | 0.045 | |
| 4th Quartile | 1.09 | 0.90 | 1.32 | 0.404 | |
| County Categorization | Metro | REF | |||
| Urban | 0.83 | 0.70 | 0.97 | 0.019 | |
| Rural | 0.75 | 0.54 | 1.04 | 0.085 | |
| Distance from patient’s residence to hospital (miles) | <5 | REF | |||
| 5–30 | 1.35 | 1.19 | 1.53 | <0.001 | |
| >30 | 2.55 | 2.17 | 3.00 | <0.001 | |
| Charlson-Deyo Comorbidity Score | 0 | REF | |||
| 1 | 1.25 | 1.12 | 1.40 | <0.001 | |
| 2 | 1.02 | 0.85 | 1.23 | 0.800 | |
| 3 | 0.74 | 0.57 | 0.97 | 0.031 | |
| Diagnosis Year | 2004–2010 | REF | |||
| 2011–2017 | 1.40 | 1.26 | 1.55 | <0.001 | |
| Primary Site | Glottis | REF | |||
| Supraglottis | 0.51 | 0.45 | 0.58 | <0.001 | |
| Subglottis | 0.86 | 0.68 | 1.09 | 0.202 | |
| Laryngeal cartilage | 0.36 | 0.09 | 1.49 | 0.159 | |
| Overlapping lesions of larynx | 1.99 | 1.65 | 2.40 | <0.001 | |
| Larynx, NOS | 0.76 | 0.66 | 0.88 | <0.001 | |
| Clinical nodal stage | N0 | REF | |||
| N1 | 0.78 | 0.68 | 0.89 | <0.001 | |
| N2 | 0.67 | 0.59 | 0.76 | <0.001 | |
| N3 | 0.21 | 0.15 | 0.30 | <0.001 | |
| Tumor HPV Category | Negative | REF | |||
| Positive | 0.80 | 0.57 | 1.12 | 0.195 | |
| Unknown | 0.88 | 0.76 | 1.02 | 0.094 |
| Variable | Hazard Ratio (95% CI) | p-Value | |
|---|---|---|---|
| Facility Type | Community Cancer Program | REF | |
| Comprehensive Community Cancer Program | 1.05 (0.92, 1.20) | 0.472 | |
| Academic/Research Program | 0.99 (0.86, 1.13) | 0.825 | |
| Integrated Network Cancer Program | 1.01 (0.88, 1.17) | 0.880 | |
| Age | ≤61 years | REF | |
| >61 years | 1.32 (1.23, 1.42) | <0.001 | |
| Sex | Female | REF | |
| Male | 1.13 (1.05, 1.21) | 0.002 | |
| Race | White | REF | |
| Black | 0.97 (0.90, 1.05) | 0.424 | |
| Other/unknown | 0.87 (0.72, 1.05) | 0.154 | |
| Ethnicity | Non-Hispanic | REF | |
| Hispanic | 0.88 (0.77, 1.01) | 0.069 | |
| Unknown | 1.11 (0.98, 1.27) | 0.110 | |
| Insurance Type | Private Insurance/Managed Care | REF | |
| Not Insured | 1.12 (1.00, 1.26) | 0.056 | |
| Medicaid | 1.32 (1.20, 1.44) | <0.001 | |
| Medicare | 1.52 (1.40, 1.65) | <0.001 | |
| Other Government | 1.43 (1.16, 1.78) | 0.001 | |
| Insurance Status Unknown | 1.26 (1.04, 1.53) | 0.016 | |
| Percentage with No High School Degree | ≥21.0% | REF | |
| 13.0–20.9% | 1.04 (0.96, 1.13) | 0.314 | |
| 7.0–12.9% | 1.07 (0.98, 1.18) | 0.124 | |
| <7.0% | 0.95 (0.84, 1.07) | 0.374 | |
| Annual Income | 1st Quartile | REF | |
| 2nd Quartile | 0.99 (0.91, 1.08) | 0.780 | |
| 3rd Quartile | 1.03 (0.94, 1.14) | 0.524 | |
| 4th Quartile | 1.11 (1.00, 1.23) | 0.061 | |
| Distance from patient’s residence to hospital (miles) | <5 | REF | |
| 5–30 | 0.94 (0.87, 1.00) | 0.061 | |
| >30 | 0.97 (0.89, 1.05) | 0.448 | |
| Charlson-Deyo Comorbidity Score | 0 | REF | |
| 1 | 1.11 (1.04, 1.19) | <0.001 | |
| 2 | 1.46 (1.32, 1.61) | <0.001 | |
| 3+ | 1.41 (1.21, 1.64) | <0.001 | |
| Diagnosis Year | 2004–2010 | REF | |
| 2011–2017 | 0.94 (0.88, 1.00) | 0.049 | |
| Primary Site | Glottis | REF | |
| Supraglottis | 1.09 (1.01, 1.17) | 0.031 | |
| Subglottis | 1.15 (1.00, 1.32) | 0.058 | |
| Laryngeal cartilage | 0.97 (0.43, 2.16) | 0.933 | |
| Overlapping lesions of larynx | 1.16 (1.04, 1.29) | 0.009 | |
| Larynx, NOS | 1.29 (1.19, 1.40) | <0.001 | |
| Clinical nodal stage | N0 | REF | |
| N1 | 1.10 (1.02, 1.20) | 0.014 | |
| N2 | 1.41 (1.31, 1.51) | <0.001 | |
| N3 | 1.77 (1.52, 2.05) | <0.001 | |
| Total Laryngectomy | No | REF | |
| Yes | 0.50 (0.47, 0.54) | <0.001 | |
| Radiation | No | REF | |
| Yes | 0.49 (0.46, 0.53) | <0.001 | |
| Chemotherapy | No | REF | |
| Yes | 0.94 (0.87, 1.01) | 0.079 | |
| Tumor HPV Status | Negative | REF | |
| Positive | 0.68 (0.53, 0.86) | 0.002 | |
| Unknown | 1.00 (0.91, 1.10) | 0.962 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ritter, A.R.; Yildiz, V.O.; Koirala, N.; Baliga, S.; Gogineni, E.; Konieczkowski, D.J.; Grecula, J.; Blakaj, D.M.; Jhawar, S.R.; VanKoevering, K.K.; et al. Factors Associated with Total Laryngectomy Utilization in Patients with cT4a Laryngeal Cancer. Cancers 2023, 15, 5447. https://doi.org/10.3390/cancers15225447
Ritter AR, Yildiz VO, Koirala N, Baliga S, Gogineni E, Konieczkowski DJ, Grecula J, Blakaj DM, Jhawar SR, VanKoevering KK, et al. Factors Associated with Total Laryngectomy Utilization in Patients with cT4a Laryngeal Cancer. Cancers. 2023; 15(22):5447. https://doi.org/10.3390/cancers15225447
Chicago/Turabian StyleRitter, Alex R., Vedat O. Yildiz, Nischal Koirala, Sujith Baliga, Emile Gogineni, David J. Konieczkowski, John Grecula, Dukagjin M. Blakaj, Sachin R. Jhawar, Kyle K. VanKoevering, and et al. 2023. "Factors Associated with Total Laryngectomy Utilization in Patients with cT4a Laryngeal Cancer" Cancers 15, no. 22: 5447. https://doi.org/10.3390/cancers15225447
APA StyleRitter, A. R., Yildiz, V. O., Koirala, N., Baliga, S., Gogineni, E., Konieczkowski, D. J., Grecula, J., Blakaj, D. M., Jhawar, S. R., VanKoevering, K. K., & Mitchell, D. (2023). Factors Associated with Total Laryngectomy Utilization in Patients with cT4a Laryngeal Cancer. Cancers, 15(22), 5447. https://doi.org/10.3390/cancers15225447






