Risks Associated with Surgical Treatment for Appendicitis in Hematologic Patients
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
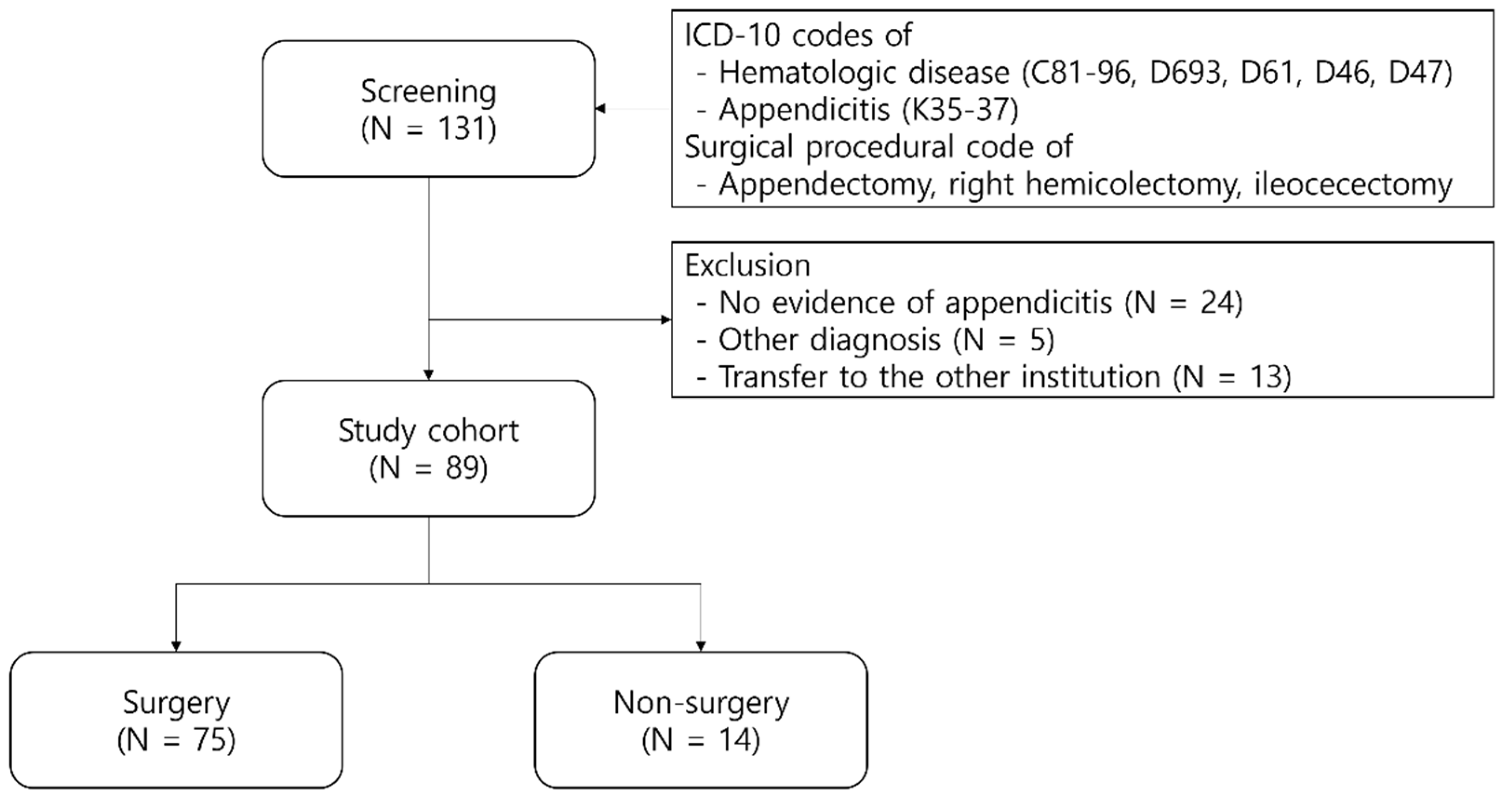
2.1. Study Design and Cohort
2.2. Hematologic Disease Classification
2.3. Patient Selection and Treatment
2.4. Terminologies Used in the Study
2.5. Statistical Analysis
2.6. Ethical Approval and Consent to Participate
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Lee, J.H.; Park, Y.S.; Choi, J.S. The epidemiology of appendicitis and appendectomy in South Korea: National registry data. J. Epidemiol. 2010, 20, 97–105. [Google Scholar] [CrossRef]
- Podda, M.; Poillucci, G.; Pacella, D.; Mortola, L.; Canfora, A.; Aresu, S.; Pisano, M.; Erdas, E.; Pisanu, A.; Cillara, N.; et al. Appendectomy versus conservative treatment with antibiotics for patients with uncomplicated acute appendicitis: A propensity score-matched analysis of patient-centered outcomes (the ACTUAA prospective multicenter trial). Int. J. Color. Dis. 2021, 36, 589–598. [Google Scholar] [CrossRef]
- Ceresoli, M.; Zucchi, A.; Allievi, N.; Harbi, A.; Pisano, M.; Montori, G.; Heyer, A.; Nita, G.E.; Ansaloni, L.; Coccolini, F. Acute appendicitis: Epidemiology, treatment and outcomes- analysis of 16544 consecutive cases. World J. Gastrointest. Surg. 2016, 8, 693–699. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.; Sun, F.; Ai, S.; Wang, J.; Guan, W.; Liu, S. Meta-analysis of studies comparing conservative treatment with antibiotics and appendectomy for acute appendicitis in the adult. BMC Surg. 2019, 19, 110. [Google Scholar] [CrossRef] [PubMed]
- Sallinen, V.; Akl, E.A.; You, J.J.; Agarwal, A.; Shoucair, S.; Vandvik, P.O.; Agoritsas, T.; Heels-Ansdell, D.; Guyatt, G.H.; Tikkinen, K.A. Meta-analysis of antibiotics versus appendicectomy for non-perforated acute appendicitis. Br. J. Surg. 2016, 103, 656–667. [Google Scholar] [CrossRef] [PubMed]
- Flum, D.R.; Davidson, G.H.; Monsell, S.E.; Shapiro, N.I.; Odom, S.R.; Sanchez, S.E.; Drake, F.T.; Fischkoff, K.; Johnson, J.; Patton, J.H.; et al. A Randomized Trial Comparing Antibiotics with Appendectomy for Appendicitis. N. Engl. J. Med. 2020, 383, 1907–1919. [Google Scholar] [CrossRef]
- Moris, D.; Paulson, E.K.; Pappas, T.N. Diagnosis and Management of Acute Appendicitis in Adults: A Review. JAMA 2021, 326, 2299–2311. [Google Scholar] [CrossRef]
- Park, K.B.; Hong, J.; Moon, J.Y.; Jung, J.; Seo, H.S. Relationship Between Appendectomy Incidence and Computed Tomography Scans Based on Korean Nationwide Data, 2003–2017. J. Korean Med. Sci. 2022, 37, e27. [Google Scholar] [CrossRef]
- Orsini, S.; Noris, P.; Bury, L.; Heller, P.G.; Santoro, C.; Kadir, R.A.; Butta, N.C.; Falcinelli, E.; Cid, A.R.; Fabris, F.; et al. Bleeding risk of surgery and its prevention in patients with inherited platelet disorders. Haematologica 2017, 102, 1192–1203. [Google Scholar] [CrossRef]
- Kojima, K.; Nakamura, T.; Habiro, T.; Waraya, M.; Hayashi, K.; Ishii, K.I. Laparoscopic Appendectomy for Acute Appendicitis Complicated by Pancytopenia in Two Patients with Hematologic Diseases. J. Anus Rectum Colon 2021, 5, 188–191. [Google Scholar] [CrossRef]
- Arredondo Montero, J.; Bardají Pascual, C.; Antona, G.; Ros Briones, R.; López-Andrés, N.; Martín-Calvo, N. The BIDIAP index: A clinical, analytical and ultrasonographic score for the diagnosis of acute appendicitis in children. Pediatr. Surg. Int. 2023, 39, 175. [Google Scholar] [CrossRef]
- Singh, A.; Pogorelić, Z.; Agrawal, A.; Muñoz, C.M.L.; Kainth, D.; Verma, A.; Jindal, B.; Agarwala, S.; Anand, S. Utility of Ischemia-Modified Albumin as a Biomarker for Acute Appendicitis: A Systematic Review and Meta-Analysis. J. Clin. Med. 2023, 12, 5486. [Google Scholar] [CrossRef] [PubMed]
- Arredondo Montero, J.; Rivero Marcotegui, A.; Bardají Pascual, C.; Antona, G.; Fernández-Celis, A.; López-Andrés, N.; Martín-Calvo, N. Post-Operative Increase in Serum Interleukin-6 Is Associated With Longer Hospital Stay in Children Operated on for Acute Appendicitis: A Pilot Study. Surg. Infect. 2023, 24, 619–624. [Google Scholar] [CrossRef] [PubMed]
- Arredondo Montero, J.; Antona, G.; Rivero Marcotegui, A.; Bardají Pascual, C.; Bronte Anaut, M.; Ros Briones, R.; Fernández-Celis, A.; López-Andrés, N.; Martín-Calvo, N. Discriminatory capacity of serum interleukin-6 between complicated and uncomplicated acute appendicitis in children: A prospective validation study. World J. Pediatr. 2022, 18, 810–817. [Google Scholar] [CrossRef]
- Armand, P.; Gibson, C.J.; Cutler, C.; Ho, V.T.; Koreth, J.; Alyea, E.P.; Ritz, J.; Sorror, M.L.; Lee, S.J.; Deeg, H.J.; et al. A disease risk index for patients undergoing allogeneic stem cell transplantation. Blood 2012, 120, 905–913. [Google Scholar] [CrossRef] [PubMed]
- Dindo, D.; Demartines, N.; Clavien, P.A. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef]
- Glance, L.G.; Blumberg, N.; Eaton, M.P.; Lustik, S.J.; Osler, T.M.; Wissler, R.; Zollo, R.; Karcz, M.; Feng, C.; Dick, A.W. Preoperative thrombocytopenia and postoperative outcomes after noncardiac surgery. Anesthesiology 2014, 120, 62–75. [Google Scholar] [CrossRef] [PubMed]
- Gulack, B.C.; Englum, B.R.; Lo, D.D.; Nussbaum, D.P.; Keenan, J.E.; Scarborough, J.E.; Shapiro, M.L. Leukopenia is associated with worse but not prohibitive outcomes following emergent abdominal surgery. J. Trauma Acute Care Surg. 2015, 79, 437–443. [Google Scholar] [CrossRef]
- Dunne, J.R.; Malone, D.; Tracy, J.K.; Gannon, C.; Napolitano, L.M. Perioperative anemia: An independent risk factor for infection, mortality, and resource utilization in surgery. J. Surg. Res. 2002, 102, 237–244. [Google Scholar] [CrossRef]
- Patel, M.S.; Carson, J.L. Anemia in the preoperative patient. Med. Clin. N. Am. 2009, 93, 1095–1104. [Google Scholar] [CrossRef]
- Sommer, S.P.; Lange, V.; Yildirim, C.; Schimmer, C.; Aleksic, I.; Wagner, C.; Schuster, C.; Leyh, R.G. Cardiac surgery and hematologic malignancies: A retrospective single-center analysis of 56 consecutive patients. Eur. J. Cardiothorac. Surg. 2011, 40, 173–178. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, A.; Schaff, H.V.; Arghami, A.; Bagameri, G.; Cicek, M.S.; Crestanello, J.A.; Daly, R.C.; Greason, K.L.; Pochettino, A.; Rowse, P.G.; et al. Impact of Hematologic Malignancies on Outcome of Cardiac Surgery. Ann. Thorac. Surg. 2021, 111, 1278–1283. [Google Scholar] [CrossRef]
- Nemeh, C.; Hassan, I.N.; Walsh, A.; Iyer, S.; Gitzelmann, C.A. Pediatric Ultrasound Appendicitis Score for the Diagnosis of Acute Appendicitis to Reduce Computed Tomography Scan Utilization. Am. Surg. 2023, 00031348231199172. [Google Scholar] [CrossRef] [PubMed]
- Jain, A.; Mercado, P.D.; Grafton, K.P.; Dorazio, R.A. Outpatient laparoscopic appendectomy. Surg. Endosc. 1995, 9, 424–425. [Google Scholar] [CrossRef]
- Mosquera, C.; Spaniolas, K.; Fitzgerald, T.L. Impact of frailty on approach to colonic resection: Laparoscopy vs. open surgery. World J. Gastroenterol. 2016, 22, 9544–9553. [Google Scholar] [CrossRef] [PubMed]
- Ustun, C. Laparoscopic appendectomy in a patient with acute myelogenous leukemia with neutropenia. J. Laparoendosc. Adv. Surg. Tech. 2007, 17, 213–215. [Google Scholar] [CrossRef] [PubMed]
- Mortellaro, V.E.; Juang, D.; Fike, F.B.; Saites, C.G.; Potter, D.D., Jr.; Iqbal, C.W.; Snyder, C.L.; St Peter, S.D. Treatment of appendicitis in neutropenic children. J. Surg. Res. 2011, 170, 14–16. [Google Scholar] [CrossRef]
- Matzek, L.J.; Hanson, A.C.; Schulte, P.J.; Evans, K.D.; Kor, D.J.; Warner, M.A. The Prevalence and Clinical Significance of Preoperative Thrombocytopenia in Adults Undergoing Elective Surgery: An Observational Cohort Study. Anesth. Analg. 2021, 132, 836–845. [Google Scholar] [CrossRef]
- Jolissaint, J.S.; Harary, M.; Saadat, L.V.; Madenci, A.L.; Dieffenbach, B.V.; Al Natour, R.H.; Tavakkoli, A. Timing and Outcomes of Abdominal Surgery in Neutropenic Patients. J. Gastrointest. Surg. 2019, 23, 643–650. [Google Scholar] [CrossRef]
- Patel, P.P.; Weller, J.H.; Westermann, C.R.; Cappiello, C.; Garcia, A.V.; Rhee, D.S. Appendectomy and Cholecystectomy Outcomes for Pediatric Cancer Patients with Leukopenia: A NSQIP-Pediatric Study. J. Surg. Res. 2021, 267, 556–562. [Google Scholar] [CrossRef]
- Many, B.T.; Lautz, T.B.; Dobrozsi, S.; Wilkinson, K.H.; Rossoff, J.; Le-Nguyen, A.; Dakhallah, N.; Piche, N.; Weinschenk, W.; Cooke-Barker, J.; et al. Appendectomy Versus Observation for Appendicitis in Neutropenic Children with Cancer. Pediatrics 2021, 147, e2020027797. [Google Scholar] [CrossRef] [PubMed]
| Variables | Non-Surgery (n = 14) | Surgery (n = 75) | p-Value |
|---|---|---|---|
| Age (years) | 39.5 [10.5–62.25] | 44.0 [29–60] | 0.370 |
| Sex | 0.561 | ||
| Male | 7 (50) | 45 (60) | |
| Female | 7 (50) | 30 (40) | |
| BMI (kg/m2) | 18.8 [17.1–23.3] | 22.0 [20.2–23.9] | 0.047 |
| ECOG score | 0.261 | ||
| 0 or 1 | 11 (78.6) | 67 (89.3) | |
| 2 or higher | 3 (21.4) | 8 (10.7) | |
| Comorbidities | |||
| HBP | 2 (14.3) | 9 (12) | 0.811 |
| DM | 0 (0) | 7 (9.3) | 0.234 |
| Cardiovascular | 1 (7.1) | 4 (5.3) | 0.787 |
| Pulmonary | 1 (7.1) | 4 (5.3) | 0.787 |
| Hepatic | 0 (0) | 7 (9.3) | 0.234 |
| Renal | 0 (0) | 5 (6.7) | 0.320 |
| Cerebral | 0 (0) | 1 (1.3) | 0.664 |
| Other malignancy | 0 (0) | 1 (1.3) | 0.664 |
| Others | 1 (7.1) | 10 (13.3) | 0.518 |
| Hematologic disease | 0.708 | ||
| AML | 8 (57.1) | 28 (37.3) | |
| ALL | 3 (21.4) | 12 (16) | |
| MDS | 0 (0) | 2 (2.7) | |
| Lymphoma | 2 (14.3) | 9 (12) | |
| MM | 0 (0) | 7 (9.3) | |
| CML | 1 (7.1) | 13 (17.3) | |
| CLL | 0 (0) | 2 (2.7) | |
| ITP | 0 (0) | 2 (2.7) | |
| Hematologic disease risk | 0.850 | ||
| Low | 5 (35.7) | 31 (41.3) | |
| Intermediate | 8 (57.1) | 35 (46.7) | |
| High | 1 (7.1) | 7 (9.3) | |
| Others | 0 (0) | 2 (2.7) |
| Variables | Non-Surgery (n = 14) | Surgery (n = 75) | p-Value |
|---|---|---|---|
| Diagnosis area | 0.492 | ||
| Emergency room | 10 (71.4) | 59 (78.7) | |
| Inpatient (hematology) | 4 (28.6) | 13 (17.3) | |
| Outpatient clinic | 0 (0) | 3 (4) | |
| Type of appendicitis | 0.355 | ||
| Simple | 7 (50) | 49 (65.3) | |
| Perforated | 2 (14.3) | 12 (16) | |
| Periappendiceal abscess | 5 (35.7) | 14 (18.7) | |
| Appendicolith | 1 (8.3) | 5 (6.7) | 0.832 |
| Initial ANC (109/L) | 0.001 | ||
| >1.00 | 6 (42.9) | 61 (81.3) | |
| 0.50~1.00 | 1 (7.1) | 6 (8) | |
| <0.50 | 7 (50) | 8 (10.7) | |
| Initial Hb (g/dL) | 0.261 | ||
| <8.0 | 3 (21.4) | 8 (10.7) | |
| Initial PLT count (109/L) | 0.127 | ||
| >100 | 6 (42.9) | 53 (70.7) | |
| 50~100 | 3 (21.4) | 9 (12) | |
| <50 | 5 (35.7) | 13 (17.3) | |
| Total hospital stay (days) | 16 [6–30.5] | 5 [3–19] | 0.026 |
| In-hospital mortality | 2 (14.3) | 2 (2.7) | 0.115 |
| Variables | No Complication (n = 65) | Complication (n = 10) | p-Value |
|---|---|---|---|
| Hematologic disease risk | 0.240 | ||
| Low | 28 (43.1) | 3 (30) | |
| Intermediate | 31 (47.7) | 4 (40) | |
| High | 5 (7.7) | 2 (20) | |
| Others | 1 (1.5) | 1 (10) | |
| Type of appendicitis | 0.266 | ||
| Simple | 41 (63.1) | 8 (80) | |
| Perforated | 10 (15.4) | 2 (20) | |
| Periappendiceal abscess | 14 (21.5) | 0 (0) | |
| Appendicolith | 3 (4.6) | 2 (20) | |
| Type of surgery | 0.455 | ||
| Appendectomy | 56 (86.2) | 10 (100) | |
| Ileocecectomy | 7 (10.8) | 0 (0) | |
| Right hemicolectomy | 2 (3.1) | 0 (0) | |
| Approach | 0.481 | ||
| Open | 3 (4.6) | 1 (10) | |
| Laparoscopy | 62 (95.4) | 9 (90) | |
| Drain | 34 (52.3) | 4 (40) | 0.469 |
| OP time (min) | 57 [45.0–87.5] | 75 [48.5–87.5] | 0.569 |
| EBL (mL) | 20 [10–50] | 10 [5–36.5] | 0.190 |
| Initial ANC (109/L) | 0.968 | ||
| >1.00 | 53 (81.5) | 8 (80) | |
| 0.50~1.00 | 5 (7.7) | 1 (10) | |
| <0.50 | 7 (10.8) | 1 (10) | |
| Initial Hb (g/dL) | 0.240 | ||
| <8.0 | 8 (12.3) | 0 (0) | |
| Initial PLT count (109/L) | 0.455 | ||
| >100 | 45 (69.2) | 8 (80) | |
| 50~100 | 9 (13.8) | 0 (0) | |
| <50 | 11 (16.9) | 2 (20) | |
| Preoperative ANC (109/L) | 0.407 | ||
| >1.00 | 58 (89.2) | 8 (80) | |
| 0.50~1.00 | 2 (3.1) | 0 (0) | |
| <0.50 | 5 (7.7) | 2 (20) | |
| Preoperative Hb (g/dL) | 0.574 | ||
| <8.0 | 2 (3.1) | 0 (0) | |
| Preoperative PLT count (109/L) | 0.968 | ||
| >100 | 47 (72.3) | 7 (70) | |
| 50~100 | 13 (20) | 2 (20) | |
| <50 | 5 (7.7) | 1 (10) | |
| Total hospital stay (days) | 5 [3–19.5] | 8.5 [6.5–17.0] | 0.210 |
| Postoperative hospital stay (days) | 4 [2.5–7.0] | 7 [4–9.0] | 0.067 |
| In-hospital mortality | 2 (3.1) | 0 (0) | 0.574 |
| Variables | ANC ≥ 1.00 (109/L) (n = 66) | ANC < 1.00 (109/L) (n = 9) | p-Value | PLTs ≥ 100 (109/L) (n = 54) | PLTs < 100 (109/L) (n = 21) | p-Value |
|---|---|---|---|---|---|---|
| Type of surgery | 0.000 | 0.070 | ||||
| Appendectomy | 59 (89.4) | 7 (77.8) | 49 (90.7) | 17 (81) | ||
| Ileocecectomy | 7 (10.6) | 0 (0) | 5 (9.3) | 2 (9.5) | ||
| Right hemicolectomy | 0 (0) | 2 (22.2) | 0 (0) | 2 (9.5) | ||
| Approach | 0.411 | 0.314 | ||||
| Open | 3 (4.5) | 1 (11.1) | 2 (3.7) | 2 (9.5) | ||
| Laparoscopy | 63 (95.5) | 8 (88.9) | 52 (96.3) | 19 (90.5) | ||
| Drain | 33 (50) | 5 (55.6) | 0.597 | 23 (42.6) | 15 (71.4) | 0.482 |
| OP time (min) | 64.5 [45.0–91.5] | 55.0 [45.0–85.0] | 0.961 | 64.5 [45.0–81.5] | 60.0 [50.0–102.5] | 0.285 |
| EBL (mL) | 20.0 [10.0–50.0] | 10.0 [5.0–65.0] | 0.530 | 20.0 [8.5–50.0] | 20.0 [5.0–60.0] | 0.406 |
| Total hospital stay (days) | 4.5 [3.0–13.5] | 28.0 [10.0–49.5] | 0.007 | 4.0 [3.0–8.0] | 20.0 [7.5–40.0] | <0.001 |
| Postoperative hospital stay (days) | 4 [2.5–7.0] | 10.0 [4.5–44.5] | 0.006 | 3.5 [2.0–6.0] | 7.0 [5.0–13.0] | <0.001 |
| Complication | 8 (12.1) | 2 (22.2) | 0.403 | 7 (13) | 3 (14.3) | 0.880 |
| In-hospital mortality | 1 (1.5) | 1 (11.1) | 0.094 | 0 (0) | 2 (9.5) | 0.022 |
| Univariate | Multivariate | |||||||
|---|---|---|---|---|---|---|---|---|
| Variables | OR | LCI | HCI | p-Value | OR | LCI | HCI | p-Value |
| Age | 0.998 | 0.954 | 1.043 | 0.929 | ||||
| Female sex | 2.015 | 0.324 | 12.517 | 0.452 | ||||
| ECOG 2 or higher | 2.368 | 0.241 | 23.304 | 0.460 | ||||
| Hematologic disease risk: intermediate to high | 20.294 | 1.968 | 209.315 | 0.011 | 14.537 | 1.720 | 122.881 | 0.014 |
| Ileocecectomy or RHC | 32.638 | 1.632 | 652.797 | 0.023 | 22.386 | 1.644 | 304.906 | 0.020 |
| ANC < 1.00 (109/L) | 13.171 | 1.501 | 115.586 | 0.020 | 14.755 | 1.813 | 120.073 | 0.012 |
| PLTs < 100 (109/L) | 11.371 | 1.763 | 73.355 | 0.011 | 10.080 | 1.872 | 54.277 | 0.007 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, S.H.; Park, S.-S.; Seo, H.S. Risks Associated with Surgical Treatment for Appendicitis in Hematologic Patients. Cancers 2023, 15, 5049. https://doi.org/10.3390/cancers15205049
Lee SH, Park S-S, Seo HS. Risks Associated with Surgical Treatment for Appendicitis in Hematologic Patients. Cancers. 2023; 15(20):5049. https://doi.org/10.3390/cancers15205049
Chicago/Turabian StyleLee, Seung Hyun, Sung-Soo Park, and Ho Seok Seo. 2023. "Risks Associated with Surgical Treatment for Appendicitis in Hematologic Patients" Cancers 15, no. 20: 5049. https://doi.org/10.3390/cancers15205049
APA StyleLee, S. H., Park, S.-S., & Seo, H. S. (2023). Risks Associated with Surgical Treatment for Appendicitis in Hematologic Patients. Cancers, 15(20), 5049. https://doi.org/10.3390/cancers15205049







