Evaluation of Antibody Responses in Patients with B-Cell Malignancies after Two and Three Doses of Anti-SARS-CoV-2 S Vaccination—A Retrospective Cohort Study
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Determination of Antibody Levels
2.3. Statistical Analyses
3. Results
3.1. Patient Population
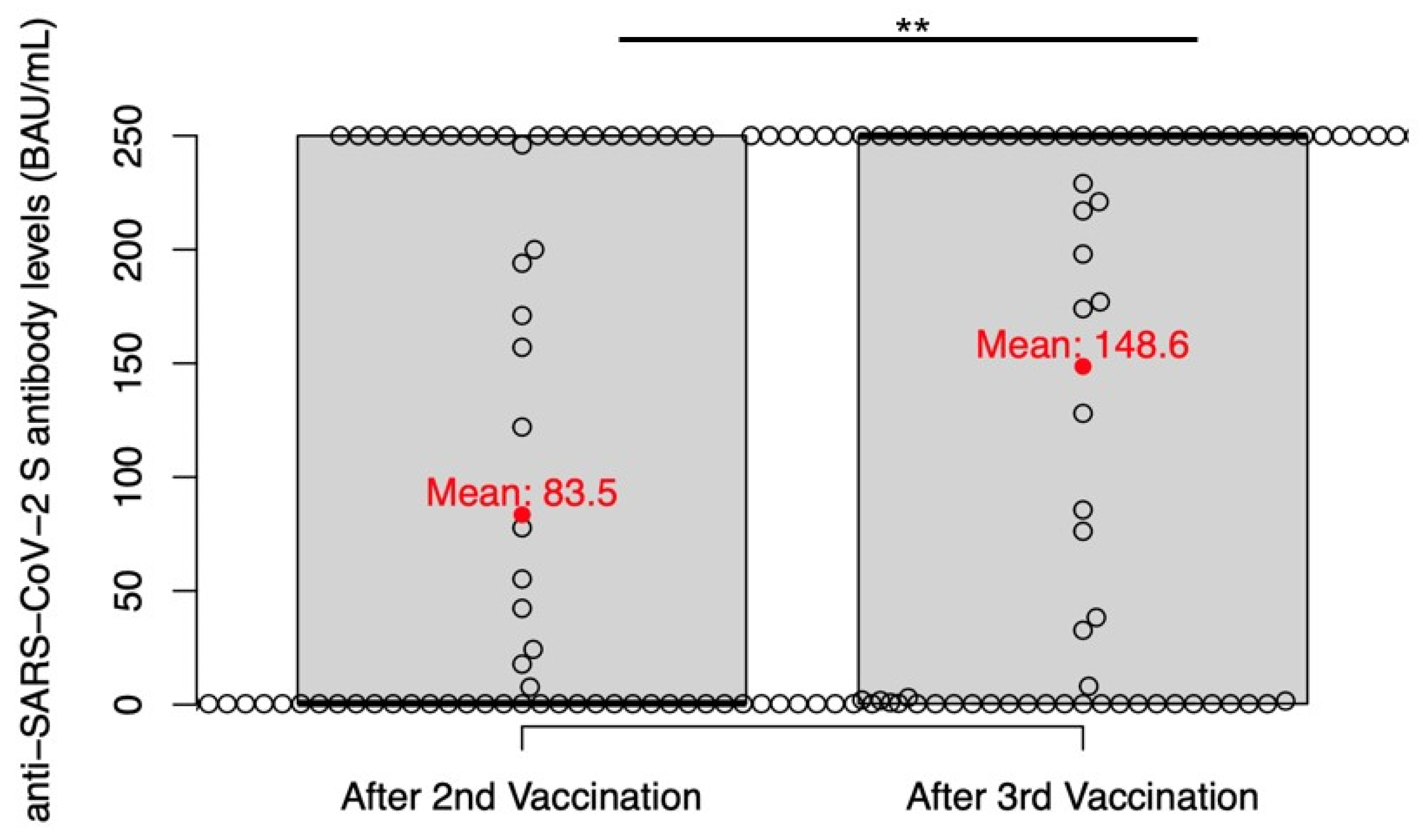
3.2. Anti-SARS-CoV-2 S Antibody Levels in Patients with B-Cell Malignancies
3.3. Seroconversion according to Treatment Modality
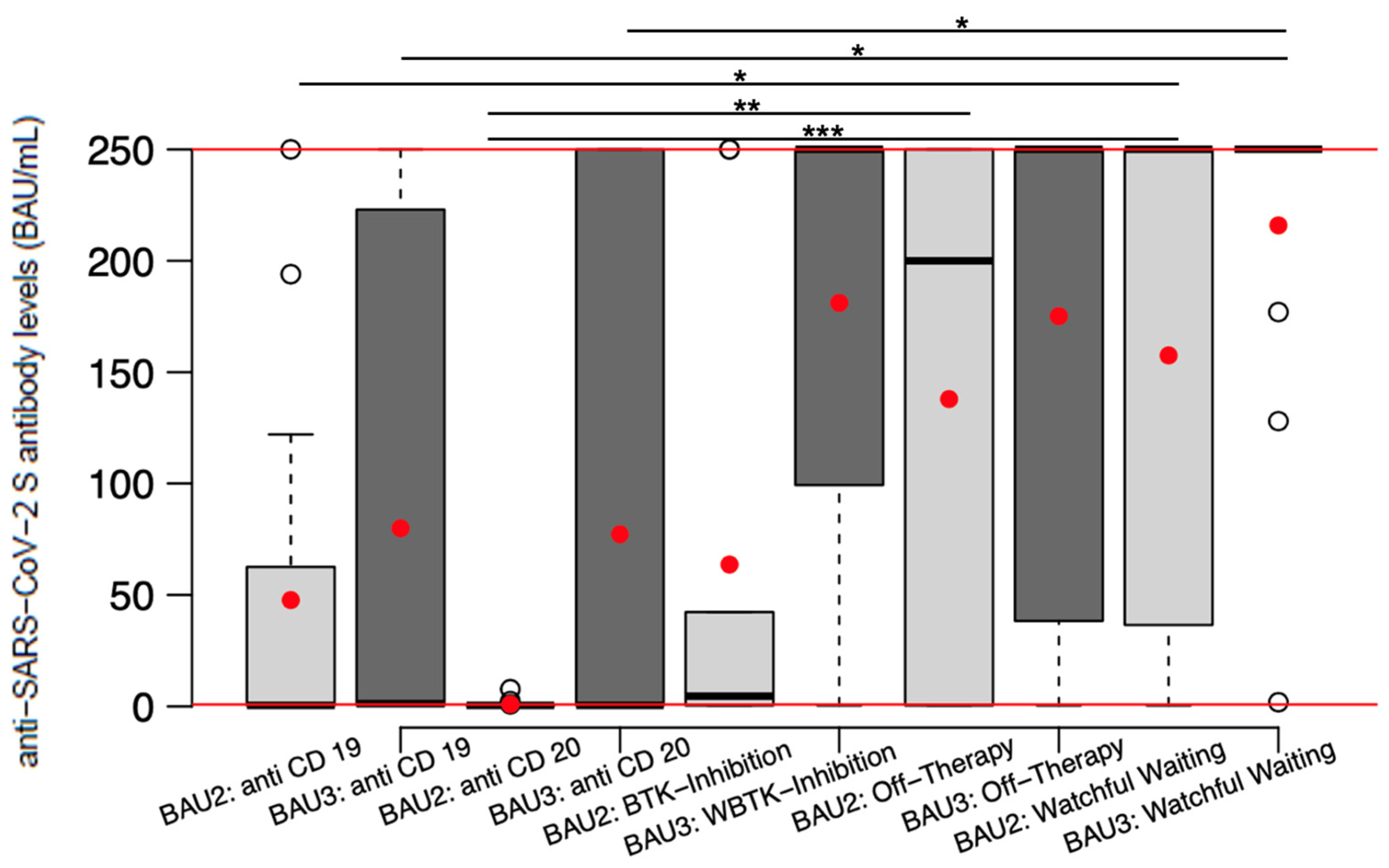
3.4. Impact of Oncologic Treatment on Anti-SARS-CoV-2 S Vaccine Immune Responses
3.5. Multivariate Analysis of Factors Influencing Anti-SARS-CoV-2 S Vaccine-Induced Antibody Responses
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Liebers, N.; Speer, C.; Benning, L.; Bruch, P.M.; Kraemer, I.; Meissner, J.; Schnitzler, P.; Kräusslich, H.G.; Dreger, P.; Mueller-Tidow, C.; et al. Humoral and cellular responses after COVID-19 vaccination in anti-CD20-treated lymphoma patients. Blood 2022, 139, 142–147. [Google Scholar] [CrossRef] [PubMed]
- Francis, A.I.; Ghany, S.; Gilkes, T.; Umakanthan, S. Review of COVID-19 vaccine subtypes, efficacy and geographical distributions. Postgrad. Med. J. 2022, 98, 389–394. [Google Scholar] [CrossRef] [PubMed]
- Singer, J.; Le, N.S.; Mattes, D.; Klamminger, V.; Hackner, K.; Kolinsky, N.; Scherb, M.; Errhalt, P.; Kreye, G.; Pecherstorfer, M.; et al. Evaluation of Antibody Responses to COVID-19 Vaccines among Solid Tumor and Hematologic Patients. Cancers 2021, 13, 4312. [Google Scholar] [CrossRef] [PubMed]
- Crombie, J.L.; Sherman, A.C.; Cheng, C.-A.; Ryan, C.E.; Zon, R.; Desjardins, M.; Baker, P.; McDonough, M.; Izaguirre, N.; Bausk, B.; et al. Activity of mRNA COVID-19 vaccines in patients with lymphoid malignancies. Blood Adv. 2021, 5, 3062–3065. [Google Scholar] [CrossRef]
- Noori, M.; Azizi, S.; Abbasi Varaki, F.; Nejadghaderi, S.A.; Bashash, D. A systematic review and meta-analysis of immune response against first and second doses of SARS-CoV-2 vaccines in adult patients with hematological malignancies. Int. Immunopharmacol. 2022, 110, 109046. [Google Scholar] [CrossRef]
- Re, D.; Seitz-Polski, B.; Brglez, V.; Carles, M.; Graça, D.; Benzaken, S.; Liguori, S.; Zahreddine, K.; Delforge, M.; Bailly-Maitre, B.; et al. Humoral and cellular responses after a third dose of SARS-CoV-2 BNT162b2 vaccine in patients with lymphoid malignancies. Nat. Commun. 2022, 13, 864. [Google Scholar] [CrossRef]
- Šušol, O.; Hájková, B.; Zelená, H.; Hájek, R. Third dose of COVID-19 vaccine restores immune response in patients with haematological malignancies after loss of protective antibody titres. Br. J. Haematol. 2022, 197, 302–305. [Google Scholar] [CrossRef] [PubMed]
- Nakagama, Y.; Chi, S.G.; Minami, Y.; Watanabe, R.; Yamagishi, M.; Atsuko, U.; Kido, Y. Patients with B-cell malignancies experience reduced antibody responses with class switching defect following BNT162b2 SARS-CoV-2 vaccination. J. Infect. Chemother. 2022, 29, 112–114. [Google Scholar] [CrossRef]
- Roeker, L.E.; Knorr, D.A.; Pessin, M.S.; Ramanathan, L.V.; Thompson, M.C.; Leslie, L.A.; Zelenetz, A.D.; Mato, A.R. Anti-SARS-CoV-2 antibody response in patients with chronic lymphocytic leukemia. Leukemia 2020, 34, 3047–3049. [Google Scholar] [CrossRef]
- Diefenbach, C.; Caro, J.; Koide, A.; Grossbard, M.; Goldberg, J.D.; Raphael, B.; Hymes, K.; Moskovits, T.; Kreditor, M.; Kaminetzky, D.; et al. Impaired Humoral Immunity to SARS-CoV-2 Vaccination in Non-Hodgkin Lymphoma and CLL Patients. medRxiv 2021. [Google Scholar] [CrossRef]
- Terpos, E.; Gavriatopoulou, M.; Fotiou, D.; Giatra, C.; Asimakopoulos, I.; Dimou, M.; Sklirou, A.D.; Ntanasis-Stathopoulos, I.; Darmani, I.; Briasoulis, A.; et al. Poor Neutralizing Antibody Responses in 132 Patients with CLL, NHL and HL after Vaccination against SARS-CoV-2: A Prospective Study. Cancers 2021, 13, 4480. [Google Scholar] [CrossRef] [PubMed]
- Terpos, E.; Fotiou, D.; Karalis, V.; Ntanasis-Stathopoulos, I.; Sklirou, A.D.; Gavriatopoulou, M.; Malandrakis, P.; Iconomidou, V.A.; Kastritis, E.; Trougakos, I.P.; et al. SARS-CoV-2 humoral responses following booster BNT162b2 vaccination in patients with B-cell malignancies. Am. J. Hematol. 2022, 97, 1300–1308. [Google Scholar] [CrossRef] [PubMed]
- Herishanu, Y.; Rahav, G.; Levi, S.; Braester, A.; Itchaki, G.; Bairey, O.; Dally, N.; Shvidel, L.; Ziv-Baran, T.; Polliack, A.; et al. Efficacy of a third BNT162b2 mRNA COVID-19 vaccine dose in patients with CLL who failed standard 2-dose vaccination. Blood 2022, 139, 678–685. [Google Scholar] [CrossRef] [PubMed]
- Roeker, L.E.; Knorr, D.A.; Thompson, M.C.; Nivar, M.; Lebowitz, S.; Peters, N.; Deonarine, I.; Momotaj, S.; Sharan, S.; Chanlatte, V.; et al. COVID-19 vaccine efficacy in patients with chronic lymphocytic leukemia. Leukemia 2021, 35, 2703–2705. [Google Scholar] [CrossRef]
- Ikeda, D.; Terao, T.; Fukumoto, A.; Uesugi, Y.; Tabata, R.; Kuzume, A.; Tsushima, T.; Miura, D.; Narita, K.; Takeuchi, M.; et al. Antibody status following booster vaccination against SARS-CoV-2 virus in patients with haematologic malignancies. Br. J. Haematol. 2022. [Google Scholar] [CrossRef]
- Ollila, T.A.; Masel, R.H.; Reagan, J.L.; Lu, S.; Rogers, R.D.; Paiva, K.J.; Taher, R.; Burguera-Couce, E.; Zayac, A.S.; Yakirevich, I.; et al. Seroconversion and outcomes after initial and booster COVID-19 vaccination in adults with hematologic malignancies. Cancer 2022, 128, 3319–3329. [Google Scholar] [CrossRef]
- Funakoshi, Y.; Yakushijin, K.; Ohji, G.; Hojo, W.; Sakai, H.; Watanabe, M.; Kitao, A.; Miyata, Y.; Saito, Y.; Kawamoto, S.; et al. Promising Efficacy of a Third Dose of mRNA SARS-CoV-2 Vaccination in Patients Treated with Anti-CD20 Antibody Who Failed 2-Dose Vaccination. Vaccines 2022, 10, 965. [Google Scholar] [CrossRef]
- Lim, S.H.; Stuart, B.; Joseph-Pietras, D.; Johnson, M.; Campbell, N.; Kelly, A.; Jeffrey, D.; Turaj, A.H.; Rolfvondenbaumen, K.; Galloway, C.; et al. Immune responses against SARS-CoV-2 variants after two and three doses of vaccine in B-cell malignancies: UK PROSECO study. Nat. Cancer 2022, 3, 552–564. [Google Scholar] [CrossRef]
- Gressens, S.B.; Fourati, S.; Le Bouter, A.; Le Bras, F.; Dupuis, J.; Hammoud, M.; El Gnaoui, T.; Gounot, R.; Roulin, L.; Belhadj, K.; et al. Anti-SARS-CoV-2 antibody response after 2 and 3 doses of BNT162b2 mRNA vaccine in patients with lymphoid malignancies. Clin. Microbiol. Infect. 2022, 28, 885.e7–885.e11. [Google Scholar] [CrossRef]
- Greenberger, L.M.; Saltzman, L.A.; Senefeld, J.W.; Johnson, P.W.; DeGennaro, L.J.; Nichols, G.L. Anti-spike antibody response to SARS-CoV-2 booster vaccination in patients with B cell-derived hematologic malignancies. Cancer Cell 2021, 39, 1297–1299. [Google Scholar] [CrossRef]
- Krekeler, C.; Reitnauer, L.; Bacher, U.; Khandanpour, C.; Steger, L.; Boeckel, G.R.; Klosner, J.; Tepasse, P.R.; Kemper, M.; Hennies, M.T.; et al. Efficacy of COVID-19 Booster Vaccines in Patients with Hematologic Malignancies: Experiences in a Real-World Scenario. Cancers 2022, 14, 5512. [Google Scholar] [CrossRef] [PubMed]
- Haggenburg, S.; Hofsink, Q.; Lissenberg-Witte, B.I.; Broers, A.E.C.; van Doesum, J.A.; van Binnendijk, R.S.; den Hartog, G.; Bhoekhan, M.S.; Haverkate, N.J.E.; Burger, J.A.; et al. Antibody Response in Immunocompromised Patients With Hematologic Cancers Who Received a 3-Dose mRNA-1273 Vaccination Schedule for COVID-19. JAMA Oncol. 2022, 8, 1477–1483. [Google Scholar] [CrossRef] [PubMed]
- Benjamini, O.; Gershon, R.; Bar-Haim, E.; Lustig, Y.; Cohen, H.; Doolman, R.; Kedmi, M.; Ribakovsky, E.; Kneller, A.; Hod, T.; et al. Cellular and humoral response to the fourth BNT162b2 mRNA COVID-19 vaccine dose in patients with CLL. Eur. J. Haematol. 2023, 110, 99–108. [Google Scholar] [CrossRef] [PubMed]



| Type of Vaccine | 1st Vaccination | 2nd Vaccination | 3rd Vaccination | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Vaxzevria®, AstraZeneca | 13 | 16.3 | 13 | 16.3 | 3 | 3.8 |
| Comirnaty®, BioNTech/Pfizer | 38 | 47.5 | 38 | 47.5 | 57 | 71.3 |
| COVID-19 Vaccine Moderna®, Moderna | 29 | 36.3 | 29 | 36.3 | 18 | 22.5 |
| COVID-19 Vaccine Janssen®, Janssen | 1 | 1.3 | ||||
| Missing | - | - | - | - | 1 | 1.3 |
| 80 | 100 | 80 | 100 | 80 | 100 | |
| Patient Group | Factor | Unstandardized Coefficients Beta | p-Value | Adjusted R2 | F-Value |
|---|---|---|---|---|---|
| Second vaccine | Intercept | 202.700 | 0.007 | 0.29 | 5.5 |
| Anti-CD20 treatment | −30.280 | 0.399 | - | - | |
| BTKi | 36.081 | 0.401 | - | - | |
| Off-therapy | 101.252 | 0.004 | - | - | |
| Watchful-waiting | 128.047 | 0.002 | - | - | |
| Sex | −1.129 | 0.961 | - | - | |
| Age | −2.192 | 0.045 | - | - | |
| Vaccination scheme | −37.875 | 0.096 | - | - | |
| Third vaccine | Intercept | 198.281 | 0.022 | 0.17 | 3.1 |
| Anti-CD20 treatment | 12.564 | 0.772 | - | - | |
| BTKi | 114.136 | 0.025 | - | - | |
| Off-therapy | 106.009 | 0.007 | - | - | |
| Watchful-waiting | 151.565 | 0.001 | - | - | |
| Sex | −4.699 | 0.859 | - | - | |
| Age | −1.650 | 0.195 | - | - | |
| Vaccination scheme | −28.018 | 0.279 | - | - | |
| Seroconversion after second vaccine | Intercept | 1.708 | 6.01 × 10−6 | 0.20 | 3.7 |
| Anti-CD20 treatment | −0.128 | 0.455 | - | - | |
| BTKi | 0.293 | 0.156 | - | - | |
| Off-therapy | 0.285 | 0.082 | - | - | |
| Watchful-waiting | 0.626 | 0.002 | - | - | |
| Sex | 0.064 | 0.558 | - | - | |
| Age | −0.005 | 0.305 | - | - | |
| Vaccination scheme | −0.157 | 0.148 | - | - | |
| Seroconversion after third vaccine | Intercept | 1.745 | 1.61 × 10−6 | 0.16 | 2.9 |
| Anti-CD20 treatment | −0.038 | 0.823 | - | - | |
| BTKi | 0.279 | 0.157 | - | - | |
| Off-therapy | 0.319 | 0.037 | - | - | |
| Watchful-waiting | 0.515 | 0.005 | - | - | |
| Sex | −0.046 | 0.659 | - | - | |
| Age | −0.002 | 0.646 | - | - | |
| Vaccination scheme | −0.171 | 0.094 | - | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wirth, S.R.M.; Podar, K.; Pecherstorfer, M.; Wohlfarth, P.; Jaeger, U.; Singer, J. Evaluation of Antibody Responses in Patients with B-Cell Malignancies after Two and Three Doses of Anti-SARS-CoV-2 S Vaccination—A Retrospective Cohort Study. Cancers 2023, 15, 524. https://doi.org/10.3390/cancers15020524
Wirth SRM, Podar K, Pecherstorfer M, Wohlfarth P, Jaeger U, Singer J. Evaluation of Antibody Responses in Patients with B-Cell Malignancies after Two and Three Doses of Anti-SARS-CoV-2 S Vaccination—A Retrospective Cohort Study. Cancers. 2023; 15(2):524. https://doi.org/10.3390/cancers15020524
Chicago/Turabian StyleWirth, Stella Rosa Maria, Klaus Podar, Martin Pecherstorfer, Philipp Wohlfarth, Ulrich Jaeger, and Josef Singer. 2023. "Evaluation of Antibody Responses in Patients with B-Cell Malignancies after Two and Three Doses of Anti-SARS-CoV-2 S Vaccination—A Retrospective Cohort Study" Cancers 15, no. 2: 524. https://doi.org/10.3390/cancers15020524
APA StyleWirth, S. R. M., Podar, K., Pecherstorfer, M., Wohlfarth, P., Jaeger, U., & Singer, J. (2023). Evaluation of Antibody Responses in Patients with B-Cell Malignancies after Two and Three Doses of Anti-SARS-CoV-2 S Vaccination—A Retrospective Cohort Study. Cancers, 15(2), 524. https://doi.org/10.3390/cancers15020524








