Negative Survival Impact of Occult Lymph Node Involvement in Small HER2-Positive Early Breast Cancer Treated by Up-Front Surgery
Abstract
Simple Summary
Abstract
1. Introduction
2. Methods
2.1. Study Design and Data Source
2.2. Pathological Assessment
2.3. Statistical Analysis
3. Results
3.1. Association of pN Status with Other Clinical and Pathological Features
3.2. Prognostic Impact of pN Status on OS, DFS, RFS, MFS in the Entire Population: Univariate Analysis
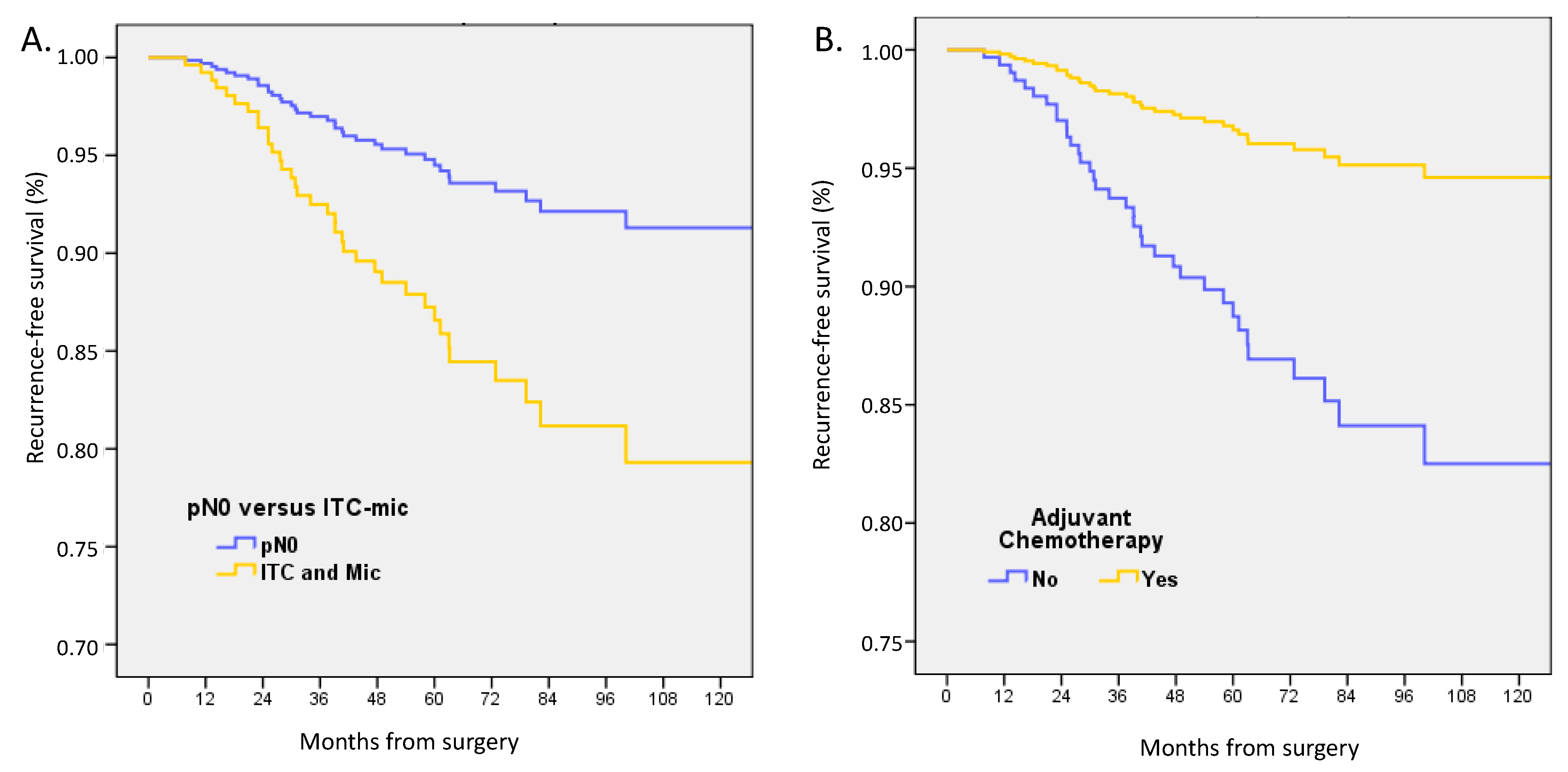
3.3. Prognostic Impact of pN Status on OS, DFS, RFS, MFS in the Entire Population: Multivariate Analyses
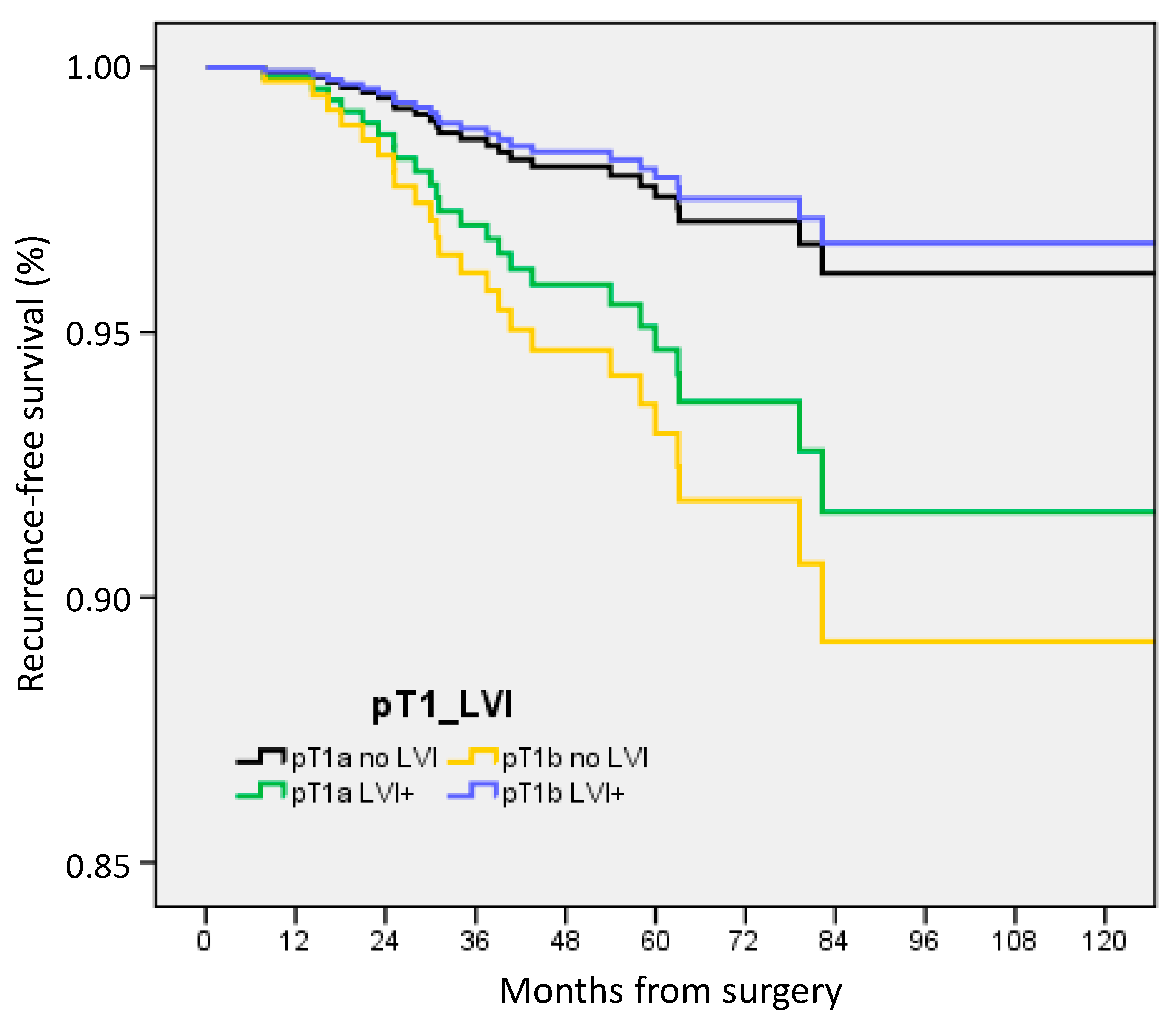
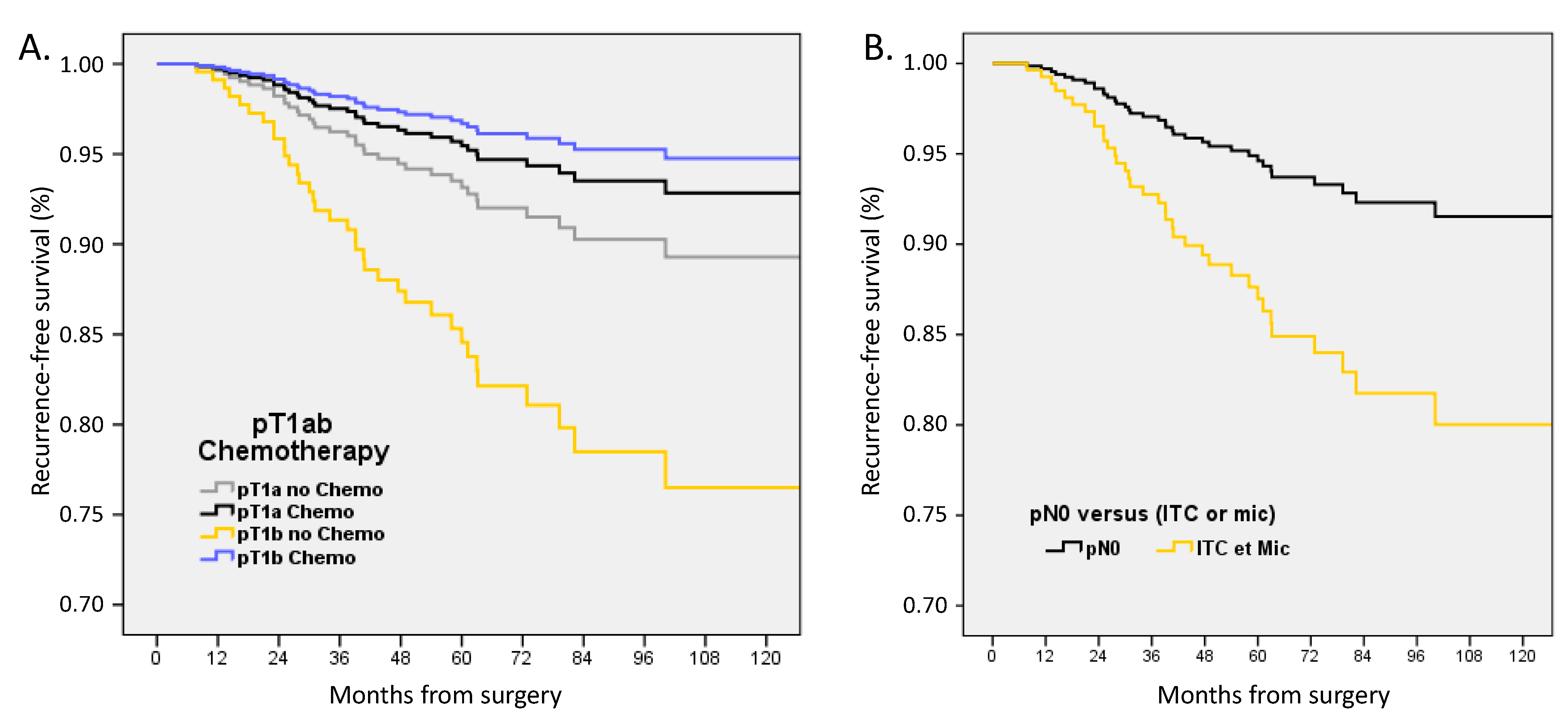
3.4. Subgroup Analysis for pT1a-b Tumors with pN0 or (pN0(i+) and pN1mi)
4. Discussion
4.1. Incidence of pN0(i+) and pN1mi and Non-Sentinel Node (NSN) Involvement Rates
4.2. Prognostic Value of Micro-Metastases in Triple-Negative and ER-Positive/HER2-Negative Patients
Indication of ACt and Trastuzumab in HER2-Positive BC
4.3. Available Literature on HER2-Positive, pT1ab BC
4.4. Negative Impact of LVI
4.4.1. Value of IHC Testing for ITC and Micro-Metastases in Triple-Negative and HER2-Positive BC
4.4.2. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Madsen, E.V.E.; Elias, S.G.; van Dalen, T.; van Oort, P.M.P.; van Gorp, J.; Gobardhan, P.D.; Bongers, V. Predictive factors of isolated tumor cells and micrometastases in axillary lymph nodes in breast cancer. Breast 2013, 22, 748–752. [Google Scholar] [CrossRef] [PubMed]
- Houvenaeghel, G.; Classe, J.-M.; Garbay, J.-R.; Giard, S.; Cohen, M.; Faure, C.; Hélène, C.; Belichard, C.; Uzan, S.; Hudry, D.; et al. Prognostic value of isolated tumor cells and micrometastases of lymph nodes in early-stage breast cancer: A French sentinel node multicenter cohort study. Breast 2014, 23, 561–566. [Google Scholar] [CrossRef] [PubMed]
- Andersson, Y.; Bergkvist, L.; Frisell, J.; de Boniface, J. Long-term breast cancer survival in relation to the metastatic tumor burden in axillary lymph nodes. Breast Cancer Res. Treat. 2018, 171, 359–369. [Google Scholar] [CrossRef]
- Van Roozendaal, L.M.; Schipper, R.J.; Van de Vijver, K.K.B.T.; Haekens, C.M.; Lobbes, M.B.I.; Tjan-Heijnen, V.C.G.; de Boer, M.; Smidt, M.L. The impact of the pathological lymph node status on adjuvant systemic treatment recommendations in clinically node negative breast cancer patients. Breast Cancer Res. Treat. 2014, 143, 469–476. [Google Scholar] [CrossRef] [PubMed]
- Maibenco, D.C.; Dombi, G.W.; Kau, T.Y.; Severson, R.K. Significance of micrometastases on the survival of women with T1 breast cancer. Cancer 2006, 107, 1234–1239. [Google Scholar] [CrossRef] [PubMed]
- Rovera, F.; Fachinetti, A.; Rausei, S.; Chiappa, C.; Lavazza, M.; Arlant, V.; Marelli, M.; Boni, L.; Dionigi, G.; Dionigi, R. Prognostic role of micrometastases in sentinel lymph node in patients with invasive breast cancer. Int. J. Surg. 2013, 11 (Suppl. S1), S73–S78. [Google Scholar] [CrossRef] [PubMed]
- Meattini, I.; Desideri, I.; Saieva, C.; Francolini, G.; Scotti, V.; Bonomo, P.; Greto, D.; Mangoni, M.; Nori, J.; Orzalesi, L.; et al. Impact of sentinel node tumor burden on outcome of invasive breast cancer patients. Eur. J. Surg. Oncol. J. Eur. Soc. Surg. Oncol. Br. Assoc. Surg. Oncol. 2014, 40, 1195–1202. [Google Scholar] [CrossRef]
- Giuliano, A.E.; Hawes, D.; Ballman, K.V.; Whitworth, P.W.; Blumencranz, P.W.; Reintgen, D.S.; Morrow, M.; Leitch, A.M.; Hunt, K.K.; McCall, L.M.; et al. Association of occult metastases in sentinel lymph nodes and bone marrow with survival among women with early-stage invasive breast cancer. JAMA 2011, 306, 385–393. [Google Scholar] [CrossRef]
- Yang, Z.J.; Yu, Y.; Hou, X.W.; Chi, J.R.; Ge, J.; Wang, X.; Cao, X.C. The prognostic value of node status in different breast cancer subtypes. Oncotarget 2017, 8, 4563–4571. [Google Scholar] [CrossRef]
- Gobardhan, P.D.; Elias, S.G.; Madsen, E.V.E.; van Wely, B.; van den Wildenberg, F.; Theunissen, E.B.M.; Ernst, M.F.; Kokke, M.C.; van der Pol, C.; Borel Rinkes, I.H.M.; et al. Prognostic value of lymph node micrometastases in breast cancer: A multicenter cohort study. Ann. Surg. Oncol. 2011, 18, 1657–1664. [Google Scholar] [CrossRef]
- Weaver, D.L.; Ashikaga, T.; Krag, D.N.; Skelly, J.M.; Anderson, S.J.; Harlow, S.P.; Julian, T.B.; Mamounas, E.P.; Wolmark, N. Effect of occult metastases on survival in node-negative breast cancer. N. Engl. J. Med. 2011, 364, 412–421. [Google Scholar] [CrossRef] [PubMed]
- Hansen, N.M.; Grube, B.; Ye, X.; Turner, R.R.; Brenner, R.J.; Sim, M.-S.; Giuliano, A.E. Impact of micrometastases in the sentinel node of patients with invasive breast cancer. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2009, 27, 4679–4684. [Google Scholar] [CrossRef] [PubMed]
- Maaskant-Braat, A.J.; van de Poll-Franse, L.V.; Voogd, A.C.; Coebergh, J.W.W.; Roumen, R.M.; Nolthenius-Puylaert, M.C.T.; Nieuwenhuijzen, G.A. Sentinel node micrometastases in breast cancer do not affect prognosis: A population-based study. Breast Cancer Res. Treat. 2011, 127, 195–203. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Iqbal, J.; Ginsburg, O.; Giannakeas, V.; Rochon, P.A.; Semple, J.L.; Narod, S.A. The impact of nodal micrometastasis on mortality among women with early-stage breast cancer. Breast Cancer Res. Treat. 2017, 161, 103–115. [Google Scholar] [CrossRef] [PubMed]
- Truong, P.T.; Vinh-Hung, V.; Cserni, G.; Woodward, W.A.; Tai, P.; Vlastos, G.; Member of the International Nodal Ratio Working Group. The number of positive nodes and the ratio of positive to excised nodes are significant predictors of survival in women with micrometastatic node-positive breast cancer. Eur. J. Cancer 2008, 44, 1670–1677. [Google Scholar] [CrossRef] [PubMed]
- Tan, L.K.; Giri, D.; Hummer, A.J.; Panageas, K.S.; Brogi, E.; Norton, L.; Hudis, C.; Borgen, P.I.; Cody, H.S. Occult axillary node metastases in breast cancer are prognostically significant: Results in 368 node-negative patients with 20-year follow-up. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2008, 26, 1803–1809. [Google Scholar] [CrossRef] [PubMed]
- Kuijt, G.P.; Voogd, A.C.; van de Poll-Franse, L.V.; Scheijmans, L.J.E.E.; van Beek, M.W.P.M.; Roumen, R.M.H. The prognostic significance of axillary lymph-node micrometastases in breast cancer patients. Eur. J. Surg. Oncol. J. Eur. Soc. Surg. Oncol. Br. Assoc. Surg. Oncol. 2005, 31, 500–505. [Google Scholar] [CrossRef]
- Grabau, D.; Jensen, M.B.; Rank, F.; Blichert-Toft, M. Axillary lymph node micrometastases in invasive breast cancer: National figures on incidence and overall survival. APMIS Acta Pathol. Microbiol. Immunol. Scand. 2007, 115, 828–837. [Google Scholar] [CrossRef]
- Cox, C.E.; Kiluk, J.V.; Riker, A.I.; Cox, J.M.; Allred, N.; Ramos, D.C.; Dupont, E.L.; Vrcel, V.; Diaz, N.; Boulware, D. Significance of sentinel lymph node micrometastases in human breast cancer. J. Am. Coll. Surg. 2008, 206, 261–268. [Google Scholar] [CrossRef]
- Andersson, Y.; Frisell, J.; Sylvan, M.; de Boniface, J.; Bergkvist, L. Breast cancer survival in relation to the metastatic tumor burden in axillary lymph nodes. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2010, 28, 2868–2873. [Google Scholar] [CrossRef]
- Tsuda, H. Histological examination of sentinel lymph nodes: Significance of macrometastasis, micrometastasis, and isolated tumor cells. Breast Cancer 2015, 22, 221–229. [Google Scholar] [CrossRef] [PubMed]
- Wada, N.; Imoto, S. Clinical evidence of breast cancer micrometastasis in the era of sentinel node biopsy. Int. J. Clin. Oncol. 2008, 13, 24–32. [Google Scholar] [CrossRef] [PubMed]
- De Boer, M.; van Deurzen, C.H.M.; van Dijck, J.A.A.M.; Borm, G.F.; van Diest, P.J.; Adang, E.M.M.; Nortier, J.W.R.; Rutgers, E.J.T.; Seynaeve, C.; Menke-Pluymers, M.B.E.; et al. Micrometastases or isolated tumor cells and the outcome of breast cancer. N. Engl. J. Med. 2009, 361, 653–663. [Google Scholar] [CrossRef] [PubMed]
- De Boer, M.; van Dijck, J.A.A.M.; Bult, P.; Borm, G.F.; Tjan-Heijnen, V.C.G. Breast cancer prognosis and occult lymph node metastases, isolated tumor cells, and micrometastases. J. Natl. Cancer Inst. 2010, 102, 410–425. [Google Scholar] [CrossRef] [PubMed]
- Colleoni, M.; Rotmensz, N.; Peruzzotti, G.; Maisonneuve, P.; Mazzarol, G.; Pruneri, G.; Luini, A.; Intra, M.; Veronesi, P.; Galimberti, V.; et al. Size of breast cancer metastases in axillary lymph nodes: Clinical relevance of minimal lymph node involvement. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2005, 23, 1379–1389. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.L.; Hoehne, F.M.; Giuliano, A.E. The prognostic significance of micrometastases in breast cancer: A SEER population-based analysis. Ann. Surg. Oncol. 2007, 14, 3378–3384. [Google Scholar] [CrossRef] [PubMed]
- Salhab, M.; Patani, N.; Mokbel, K. Sentinel lymph node micrometastasis in human breast cancer: An update. Surg. Oncol. 2011, 20, e195–e206. [Google Scholar] [CrossRef] [PubMed]
- Jafferbhoy, S.; McWilliams, B. Clinical significance and management of sentinel node micrometastasis in invasive breast cancer. Clin. Breast Cancer 2012, 12, 308–312. [Google Scholar] [CrossRef] [PubMed]
- Cianfrocca, M.; Goldstein, L.J. Prognostic and predictive factors in early-stage breast cancer. Oncologist 2004, 9, 606–616. [Google Scholar] [CrossRef] [PubMed]
- Dowlatshahi, K.; Fan, M.; Anderson, J.M.; Bloom, K.J. Occult metastases in sentinel nodes of 200 patients with operable breast cancer. Ann. Surg. Oncol. 2001, 8, 675–681. [Google Scholar] [CrossRef]
- Perou, C.M.; Sørlie, T.; Eisen, M.B.; van de Rijn, M.; Jeffrey, S.S.; Rees, C.A.; Pollack, J.R.; Ross, D.T.; Johnsen, H.; Akslen, L.A.; et al. Molecular portraits of human breast tumours. Nature 2000, 406, 747–752. [Google Scholar] [CrossRef] [PubMed]
- Cheang, M.C.U.; Voduc, D.; Bajdik, C.; Leung, S.; McKinney, S.; Chia, S.K.; Perou, C.M.; Nielsen, T.O. Basal-like breast cancer defined by five biomarkers has superior prognostic value than triple-negative phenotype. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2008, 14, 1368–1376. [Google Scholar] [CrossRef] [PubMed]
- Reyal, F.; Rouzier, R.; Depont-Hazelzet, B.; Bollet, M.A.; Pierga, J.-Y.; Alran, S.; Salmon, R.J.; Fourchotte, V.; Vincent-Salomon, A.; Sastre-Garau, X.; et al. The Molecular Subtype Classification Is a Determinant of Sentinel Node Positivity in Early Breast Carcinoma. PLoS ONE 2011, 6, e20297. [Google Scholar] [CrossRef] [PubMed]
- Houvenaeghel, G.; Sabatier, R.; Reyal, F.; Classe, J.M.; Giard, S.; Charitansky, H.; Rouzier, R.; Faure, C.; Garbay, J.R.; Daraï, E.; et al. Axillary lymph node micrometastases decrease triple-negative early breast cancer survival. Br. J. Cancer 2016, 115, 1024–1031. [Google Scholar] [CrossRef] [PubMed]
- Sabatier, R.; Jacquemier, J.; Bertucci, F.; Esterni, B.; Finetti, P.; Azario, F.; Birnbaum, D.; Viens, P.; Gonçalves, A.; Extra, J.-M. Peritumoural vascular invasion: A major determinant of triple-negative breast cancer outcome. Eur. J. Cancer 2011, 47, 1537–1545. [Google Scholar] [CrossRef] [PubMed]
- Houvenaeghel, G.; de Nonneville, A.; Cohen, M.; Chopin, N.; Coutant, C.; Reyal, F.; Mazouni, C.; Gimbergues, P.; Azuar, A.-S.; Chauvet, M.-P.; et al. Lack of prognostic impact of sentinel node micro-metastases in endocrine receptor-positive early breast cancer: Results from a large multicenter cohort. ESMO Open 2021, 6, 100151. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, F.; Kyriakides, S.; Ohno, S.; Penault-Llorca, F.; Poortmans, P.; Rubio, I.T.; Zackrisson, S.; Senkus, E. Early breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2019, 30, 1194–1220. [Google Scholar] [CrossRef] [PubMed]
- Houvenaeghel, G.; de Nonneville, A.; Cohen, M.; Viret, F.; Rua, S.; Sabiani, L.; Buttarelli, M.; Charaffe, E.; Monneur, A.; Jalaguier-Coudray, A.; et al. Neoadjuvant Chemotherapy for Breast Cancer: Evolution of Clinical Practice in a French Cancer Center Over 16 Years and Pathologic Response Rates According to Tumor Subtypes and Clinical Tumor Size: Retrospective Cohort Study. J. Surg. Res. 2022, 5, 511–525. [Google Scholar] [CrossRef]
- Houvenaeghel, G.; Cohen, M.; Classe, J.M.; Reyal, F.; Mazouni, C.; Chopin, N.; Martinez, A.; Daraï, E.; Coutant, C.; Colombo, P.E.; et al. Lymphovascular invasion has a significant prognostic impact in patients with early breast cancer, results from a large, national, multicenter, retrospective cohort study. ESMO Open 2021, 6, 100316. [Google Scholar] [CrossRef]
- Houvenaeghel, G.; Lambaudie, E.; Classe, J.-M.; Mazouni, C.; Giard, S.; Cohen, M.; Faure, C.; Charitansky, H.; Rouzier, R.; Daraï, E.; et al. Lymph node positivity in different early breast carcinoma phenotypes: A predictive model. BMC Cancer 2019, 19, 45. [Google Scholar] [CrossRef]
- Houvenaeghel, G.; Cohen, M.; Raro, P.; De Troyer, J.; Gimbergues, P.; Tunon de Lara, C.; Ceccato, V.; Vaini-Cowen, V.; Faure-Virelizier, C.; Marchal, F.; et al. Sentinel node involvement with or without completion axillary lymph node dissection: Treatment and pathologic results of randomized SERC trial. NPJ Breast Cancer 2021, 7, 133. [Google Scholar] [CrossRef] [PubMed]
- De Nonneville, A.; Gonçalves, A.; Zemmour, C.; Classe, J.M.; Cohen, M.; Lambaudie, E.; Reyal, F.; Scherer, C.; Muracciole, X.; Colombo, P.E.; et al. Benefit of adjuvant chemotherapy with or without trastuzumab in pT1ab node-negative human epidermal growth factor receptor 2-positive breast carcinomas: Results of a national multi-institutional study. Breast Cancer Res. Treat. 2017, 162, 307–316. [Google Scholar] [CrossRef] [PubMed]
- De Nonneville, A.; Gonçalves, A.; Zemmour, C.; Cohen, M.; Classe, J.M.; Reyal, F.; Colombo, P.E.; Jouve, E.; Giard, S.; Barranger, E.; et al. Adjuvant chemotherapy in pT1ab node-negative triple-negative breast carcinomas: Results of a national multi-institutional retrospective study. Eur. J. Cancer 2017, 84, 34–43. [Google Scholar] [CrossRef] [PubMed]
- Romond, E.H.; Perez, E.A.; Bryant, J.; Suman, V.J.; Geyer, C.E., Jr.; Davidson, N.E.; Tan-Chiu, E.; Martino, S.; Paik, S.; Kaufman, P.A.; et al. Trastuzumab plus adjuvant chemotherapy for operable HER2-positive breast cancer. N. Engl. J. Med. 2005, 353, 1673–1684. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, M.J.; Peron, J.; Frenel, J.-S.; Vano, Y.-A.; Wassermann, J.; Debled, M.; Picaud, F.; Albiges, L.; Vincent-Salomon, A.; Cottu, P.H. Benefit of adjuvant trastuzumab-based chemotherapy in T1ab node-negative HER2-overexpressing breast carcinomas: A multicenter retrospective series. Ann. Oncol. 2013, 24, 916–924. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.L.; Saraf, A.; Lee, S.M.; Zhong, X.; Hibshoosh, H.; Kalinsky, K.; Connolly, E.P. Lymphovascular invasion is an independent predictor of survival in breast cancer after neoadjuvant chemotherapy. Breast Cancer Res. Treat. 2016, 157, 555–564. [Google Scholar] [CrossRef] [PubMed]
- Kurozumi, S.; Joseph, C.; Sonbul, S.; Alsaeed, S.; Kariri, Y.; Aljohani, A.; Raafat, S.; Alsaleem, M.; Ogden, A.; Johnston, S.J.; et al. A key genomic subtype associated with lymphovascular invasion in invasive breast cancer. Br. J. Cancer 2019, 120, 1129–1136. [Google Scholar] [CrossRef] [PubMed]
- He, K.-W.; Sun, J.-J.; Liu, Z.-B.; Zhuo, P.-Y.; Ma, Q.-H.; Liu, Z.-Y.; Yu, Z.-Y. Prognostic significance of lymphatic vessel invasion diagnosed by D2-40 in Chinese invasive breast cancers. Medicine 2017, 96, e8490. [Google Scholar] [CrossRef]
- Hwang, K.-T.; Kim, Y.A.; Kim, J.; Chu, A.J.; Chang, J.H.; Oh, S.W.; Hwang, K.R.; Chai, Y.J. The influences of peritumoral lymphatic invasion and vascular invasion on the survival and recurrence according to the molecular subtypes of breast cancer. Breast Cancer Res. Treat. 2017, 163, 71–82. [Google Scholar] [CrossRef]
- Klingen, T.A.; Chen, Y.; Stefansson, I.M.; Knutsvik, G.; Collett, K.; Abrahamsen, A.L.; Aase, H.; Aas, H.; Aas, T.; Wik, E.; et al. Tumour cell invasion into blood vessels is significantly related to breast cancer subtypes and decreased survival. J. Clin. Pathol. 2017, 70, 313–319. [Google Scholar] [CrossRef]
- Chas, M.; Boivin, L.; Arbion, F.; Jourdan, M.-L.; Body, G.; Ouldamer, L. Clinicopathologic predictors of lymph node metastasis in breast cancer patients according to molecular subtype. J. Gynecol. Obstet. Hum. Reprod. 2018, 47, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Invernizzi, M.; Corti, C.; Lopez, G.; Michelotti, A.; Despini, L.; Gambini, D.; Lorenzini, D.; Guerini-Rocco, E.; Maggi, S.; Noale, M.; et al. Lymphovascular invasion and extranodal tumour extension are risk indicators of breast cancer related lymphoedema: An observational retrospective study with long-term follow-up. BMC Cancer 2018, 18, 935. [Google Scholar] [CrossRef] [PubMed]
- Liao, G.-S.; Hsu, H.-M.; Chu, C.-H.; Hong, Z.-J.; Fu, C.-Y.; Chou, Y.-C.; Golshan, M.; Dai, M.-S.; Chen, T.-W.; De-Chian, C.; et al. Prognostic Role of Lymphovascular Invasion and Lymph Node Status among Breast Cancer Subtypes. J. Med. Sci. 2018, 38, 54. [Google Scholar] [CrossRef]
- Ryu, Y.J.; Kang, S.J.; Cho, J.S.; Yoon, J.H.; Park, M.H. Lymphovascular invasion can be better than pathologic complete response to predict prognosis in breast cancer treated with neoadjuvant chemotherapy. Medicine 2018, 97, e11647. [Google Scholar] [CrossRef] [PubMed]
- Morkavuk, Ş.B.; Güner, M.; Çulcu, S.; Eroğlu, A.; Bayar, S.; Ünal, A.E. Relationship between lymphovascular invasion and molecular subtypes in invasive breast cancer. Int. J. Clin. Pract. 2021, 75, e13897. [Google Scholar] [CrossRef] [PubMed]
- Makower, D.; Lin, J.; Xue, X.; Sparano, J.A. Lymphovascular invasion, race, and the 21-gene recurrence score in early estrogen receptor-positive breast cancer. NPJ Breast Cancer 2021, 7, 20. [Google Scholar] [CrossRef] [PubMed]
- Mutai, R.; Goldvaser, H.; Shochat, T.; Peretz, I.; Sulkes, A.; Yerushalmi, R. Prognostic Value of the Detection of Lymphovascular Invasion in Hormone Receptor-Positive Early Breast Cancer in the Era of Molecular Profiling. Oncology 2019, 96, 14–24. [Google Scholar] [CrossRef]
- Gujam, F.J.A.; Going, J.J.; Edwards, J.; Mohammed, Z.M.A.; McMillan, D.C. The role of lymphatic and blood vessel invasion in predicting survival and methods of detection in patients with primary operable breast cancer. Crit. Rev. Oncol. Hematol. 2014, 89, 231–241. [Google Scholar] [CrossRef]
- Akrida, I.; Mulita, F. The Clinical Significance of HER2 Expression in DCIS. Med. Oncol. 2022, 40, 16. [Google Scholar] [CrossRef]


| All Patients Her2-Positive | pN0 | pN0(i+) | pN1mi | pN1 Macro | Chi 2 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Nb | % | Nb | % | Nb | % | Nb | % | p | ||
| Total | 1047 | 59.1 | 60 | 3.4 | 118 | 6.7 | 546 | 30.8 | ||
| Age | median | 56 | 54 | 54.3 | 54 | |||||
| mean | 56.2 | 53.4 | 55.2 | 55 | ||||||
| Age groups | ≤40 | 113 | 10.8 | 12 | 20.0 | 17 | 14.4 | 77 | 14.1 | 0.007 |
| 40.1–50 | 234 | 22.3 | 12 | 20.0 | 35 | 29.7 | 135 | 24.7 | ||
| 50.1–74.9 | 628 | 60.0 | 32 | 53.3 | 53 | 44.9 | 281 | 51.5 | ||
| ≥75 | 72 | 6.9 | 4 | 6.7 | 13 | 11.0 | 53 | 9.7 | ||
| Tumor size | median | 13 | 15 | 16 | 23.5 | |||||
| mean | 15.1 | 17.1 | 18.9 | 29.9 | ||||||
| pT size groups | <20 mm | 781 | 74.6 | 35 | 58.3 | 72 | 61.0 | 194 | 35.5 | <0.0001 |
| ≥20 mm | 240 | 22.9 | 25 | 41.7 | 43 | 36.4 | 344 | 63.0 | ||
| Unknown | 26 | 2.5 | 0 | 0 | 3 | 2.5 | 8 | 1.5 | ||
| SLNB | No | 113 | 10.8 | 0 | 0 | 4 | 3.4 | 183 | 33.5 | <0.0001 |
| Yes | 934 | 89.2 | 60 | 100 | 114 | 96.6 | 363 | 66.5 | ||
| ALND | No | 829 | 79.2 | 24 | 40.0 | 27 | 22.9 | 47 | 8.6 | <0.0001 |
| Yes | 218 | 20.8 | 36 | 60.0 | 91 | 77.1 | 499 | 91.4 | ||
| Grade SBR | 1 | 103 | 9.8 | 5 | 8.3 | 11 | 9.3 | 23 | 4.2 | <0.0001 |
| 2 | 490 | 46.8 | 33 | 55.0 | 50 | 42.4 | 220 | 40.3 | ||
| 3 | 425 | 40.6 | 21 | 35.0 | 56 | 47.5 | 298 | 54.6 | ||
| Unknown | 29 | 2.8 | 1 | 1.7 | 1 | 0.8 | 5 | 0.9 | ||
| LVI | No | 745 | 71.2 | 32 | 53.3 | 61 | 51.7 | 226 | 41.4 | <0.0001 |
| Yes | 170 | 16.2 | 25 | 41.7 | 52 | 44.1 | 283 | 51.8 | ||
| Unknown | 132 | 12.6 | 3 | 5.0 | 5 | 4.2 | 37 | 6.8 | ||
| Subtype | ER-negative | 331 | 31.6 | 21 | 35.0 | 33 | 28.0 | 225 | 41.2 | 0.001 |
| ER-positive | 715 | 68.4 | 39 | 65.0 | 85 | 72.0 | 321 | 58.8 | ||
| Chemotherapy | No | 345 | 33.0 | 11 | 18.3 | 8 | 6.8 | 34 | 6.2 | <0.0001 |
| Yes | 702 | 67.0 | 49 | 81.7 | 110 | 93.2 | 512 | 93.8 | ||
| Trastuzumab | No | 487 | 46.5 | 20 | 33.3 | 27 | 22.9 | 178 | 32.6 | <0.0001 |
| Yes | 560 | 53.5 | 40 | 66.7 | 91 | 77.1 | 368 | 67.4 | ||
| Endocrine | ||||||||||
| Therapy | No | 385 | 36.8 | 29 | 48.3 | 39 | 33.1 | 246 | 45.1 | 0.002 |
| Yes | 662 | 63.2 | 31 | 51.7 | 79 | 66.9 | 300 | 54.9 | ||
| Surgery | BCS | 758 | 72.4 | 35 | 58.3 | 79 | 66.9 | 260 | 47.6 | <0.0001 |
| Mastectomy | 268 | 25.6 | 25 | 41.7 | 39 | 33.1 | 275 | 50.4 | ||
| Unknown | 21 | 2.0 | 0 | 0 | 0 | 0 | 11 | 2.0 | ||
| Radiotherapy | No | 195 | 18.6 | 11 | 18.3 | 12 | 10.2 | 23 | 4.2 | <0.0001 |
| Yes (1449) | 780 | 74.5 | 49 | 81.7 | 106 | 89.8 | 514 | 94.1 | ||
| Unknown | 72 | 6.9 | 0 | 0 | 0 | 0 | 9 | 1.6 | ||
| RNI * | No | 477 | 72.5 | 19 | 50.0 | 26 | 28.9 | 39 | 8.5 | <0.0001 |
| Yes | 181 | 27.5 | 19 | 50.0 | 64 | 71.1 | 422 | 91.5 | ||
| Follow-up | median | 58.79 | 62.70 | 67.00 | 63.95 | |||||
| Recurrence | No | 970 | 92.6 | 54 | 90.0 | 104 | 88.1 | 444 | 81.3 | <0.0001 |
| Yes | 77 | 7.4 | 6 | 10.0 | 14 | 11.9 | 102 | 18.7 | ||
| Metastases | No | 1001 | 95.9 | 57 | 95.0 | 106 | 90.6 | 458 | 84.5 | <0.0001 |
| Yes | 43 | 4.1 | 3 | 5.0 | 11 | 9.4 | 84 | 15.5 | ||
| Death | No | 994 | 94.9 | 58 | 96.7 | 115 | 97.5 | 470 | 86.1 | <0.0001 |
| Yes | 53 | 5.1 | 2 | 3.3 | 3 | 2.5 | 76 | 13.9 | ||
| All Patients | Cox OS | Cox DFS | Cox RFS | Cox MFS | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HR | CI 95% | p | HR | CI 95% | p | HR | CI 95% | p | HR | CI 95% | p | ||
| Age groups | ≤40 | 1 | 1 | 1 | 1 | ||||||||
| 40.1–50 | 0.842 | 0.41–1.74 | 0.643 | 0.767 | 0.49–1.21 | 0.256 | 0.721 | 0.45–1.15 | 0.172 | 0.852 | 0.49–1.47 | 0.566 | |
| 50.1–74.9 | 1.768 | 0.97–3.21 | 0.061 | 1.056 | 0.72–1.56 | 0.783 | 0.840 | 0.56–1.26 | 0.402 | 1.377 | 0.86–2.19 | 0.178 | |
| ≥75 ≥ | 4.918 | 2.38–10.17 | <0.0001 | 2.157 | 1.30–3.58 | 0.003 | 1.265 | 0.71–2.26 | 0.427 | 2.796 | 1.57–4.99 | 0.001 | |
| pT size groups | <20 mm | 1 | 1 | 1 | 1 | ||||||||
| ≥20 mm | 1.687 | 1.12–2.55 | 0.013 | 1.605 | 1.20–2.15 | 0.002 | 1.684 | 1.22–2.33 | 0.002 | 1.868 | 1.34–2.61 | <0.0001 | |
| LVI | No | 1 | 1 | 1 | 1 | ||||||||
| Yes | 2.122 | 1.42–3.17 | <0.0001 | 1.520 | 1.14–2.03 | 0.004 | 1.401 | 1.02–1.93 | 0.038 | 1.813 | 1.32–2.50 | <0.0001 | |
| Subtype | ER-negative | 1 | 1 | 1 | 1 | ||||||||
| ER-positive | 0.683 | 0.48–0.97 | 0.032 | 0.682 | 0.53–0.88 | 0.004 | 0.649 | 0.49–0.87 | 0.003 | 0.798 | 0.60–1.07 | 0.130 | |
| pN status | pN0 | 1 | 1 | 1 | 1 | ||||||||
| pN0(i+) | 0.440 | 0.11–1.84 | 0.261 | 0.780 | 0.34–1.80 | 0.560 | 1.120 | 0.48–2.61 | 0.793 | 0.494 | 0.15–1.59 | 0.236 | |
| pN1mi | 0.414 | 0.13–1.36 | 0.147 | 1.138 | 0.64–2.03 | 0.663 | 1.556 | 0.86–2.82 | 0.146 | 1.114 | 0.58–2.16 | 0.748 | |
| pN1macro | 1.583 | 1.00–2.50 | 0.048 | 1.737 | 1.25–2.41 | 0.001 | 2.044 | 1.42–2.95 | <0.0001 | 1.824 | 1.26–2.64 | 0.001 | |
| Surgery | BCS | 1 | 1 | 1 | 1 | ||||||||
| Mastectomy | 1.369 | 0.94–2.00 | 0.104 | 1.081 | 0.82–1.43 | 0.583 | 1.016 | 0.75–1.38 | 0.922 | 1.345 | 0.99–1.83 | 0.060 | |
| Unknown | 1.806 | 0.64–5.06 | 0.261 | 1.126 | 0.49–2.58 | 0.780 | 0.980 | 0.36–2.69 | 0.970 | 1.633 | 0.70–3.78 | 0.252 | |
| Chemotherapy | No | 1 | 1 | 1 | 1 | ||||||||
| Yes | 0.536 | 0.33–0.87 | 0.012 | 0.500 | 0.36–0.70 | <0.0001 | 0.556 | 0.37–0.83 | 0.004 | 0.533 | 0.36–0.79 | 0.002 | |
| pT1a-b | pN0 | pN0(i+) & pN1mi | Chi 2 | |||
|---|---|---|---|---|---|---|
| Nb | % | Nb | % | p | ||
| 426 | 89.9 | 48 | 10.1 | |||
| Grade | 1 | 57 | 13.4 | 5 | 10.4 | 0.887 |
| 2 | 222 | 52.1 | 27 | 56.2 | ||
| 3 | 129 | 30.3 | 15 | 31.2 | ||
| unknown | 18 | 4.3 | 1 | 2.1 | ||
| Age | ≤40 | 35 | 8.2 | 9 | 18.8 | 0.035 |
| 40.1–50 | 90 | 21.1 | 14 | 29.2 | ||
| 50.1–74.9 | 279 | 65.5 | 23 | 47.9 | ||
| ≥75 | 22 | 5.2 | 2 | 4.2 | ||
| Subtype | ER- | 169 | 39.7 | 22 | 45.8 | 0.250 |
| ER+ | 257 | 60.3 | 26 | 54.2 | ||
| Chemotherapy | No | 218 | 51.2 | 11 | 22.9 | <0.0001 |
| Yes | 208 | 48.8 | 37 | 77.1 | ||
| Surgery | BCS | 320 | 75.1 | 30 | 62.5 | 0.031 |
| Mastectomy | 93 | 21.8 | 18 | 37.5 | ||
| unknown | 13 | 3.1 | 0 | 0 | ||
| LVI | No | 308 | 72.3 | 31 | 64.6 | <0.0001 |
| Yes | 36 | 8.5 | 14 | 29.2 | ||
| unknown | 82 | 19.2 | 3 | 6.2 | ||
| Chemotherapy: Regression | OR | CI 95% | p | |
|---|---|---|---|---|
| Grade | 1 | 1 | ||
| 2 | 3.834 | 1.83–8.04 | <0.0001 | |
| 3 | 12.822 | 5.64–29.16 | <0.0001 | |
| Subtype | Type_Mol(1) | 2.118 | 1.31–3.42 | 0.002 |
| Age | ≤40 | 1 | ||
| 40.1–50 | 0.411 | 0.16–1.05 | 0.063 | |
| 50.1–74.9 | 0.273 | 0.12–0.65 | 0.003 | |
| ≥75 | 0.101 | 0.03–0.38 | 0.001 | |
| LVI | No | 1 | ||
| Yes | 6.721 | 2.27–19.90 | 0.001 | |
| unknown | 0.334 | 0.18–0.60 | <0.0001 | |
| pT size | pT1b | 3.189 | 1.98–5.13 | <0.0001 |
| pN | pN0(i+) & pN1mi | 2.137 | 0.94–4.88 | 0.071 |
| pT1a-b pN0 or pN0(i+) & pN1mi | Cox OS | Cox DFS | Cox RFS | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| HR | CI 95% | p | HR | CI 95% | p | HR | CI 95% | p | ||
| Age groups | ≤40 | 1 | 1 | 1 | ||||||
| 40.1–50 | 0.00–1306 | 0.969 | 0.387 | 0.15–1.03 | 0.057 | 0.418 | 0.15–1.15 | 0.090 | ||
| 50.1–74.9 | 4.134 | 0.42–40.7 | 0.224 | 0.445 | 0.20–0.98 | 0.043 | 0.336 | 0.14–0.80 | 0.014 | |
| ≥75 | 19.643 | 1.67–230.5 | 0.018 | 1.020 | 0.33–3.17 | 0.973 | 0.237 | 0.03–1.95 | 0.181 | |
| pT size groups | pT1a | 1 | 1 | 1 | ||||||
| pT1b | 1.940 | 0.72–5.20 | 0.187 | 1.718 | 0.94–3.13 | 0.077 | 1.747 | 0.87–3.53 | 0.120 | |
| LVI | No | 1 | 1 | 1 | ||||||
| Yes | 2.168 | 0.40–11.74 | 0.369 | 0.983 | 0.33–2.96 | 0.976 | 0.566 | 0.13–2.52 | 0.455 | |
| Subtype | ER-positive | 1 | 1 | 1 | ||||||
| ER-negative | 1.246 | 0.50–3.09 | 0.635 | 1.677 | 0.95–2.97 | 0.077 | 1.667 | 0.84–3.31 | 0.144 | |
| pN status | pN0 | 1 | 1 | 1 | ||||||
| pN0(i+)/pN1mi | 0.764 | 0.09–6.50 | 0.806 | 1.843 | 0.79–4.31 | 0.158 | 2.548 | 1.06–6.13 | 0.037 | |
| Chemotherapy | No | 1 | 1 | 1 | ||||||
| Yes | 0.259 | 0.07–0.97 | 0.046 | 0.272 | 0.13–0.56 | <0.0001 | 0.288 | 0.13–0.65 | 0.003 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Houvenaeghel, G.; Cohen, M.; Martino, M.; Reyal, F.; Classe, J.-M.; Chauvet, M.-P.; Colombo, P.-E.; Heinemann, M.; Jouve, E.; Gimbergues, P.; et al. Negative Survival Impact of Occult Lymph Node Involvement in Small HER2-Positive Early Breast Cancer Treated by Up-Front Surgery. Cancers 2023, 15, 4567. https://doi.org/10.3390/cancers15184567
Houvenaeghel G, Cohen M, Martino M, Reyal F, Classe J-M, Chauvet M-P, Colombo P-E, Heinemann M, Jouve E, Gimbergues P, et al. Negative Survival Impact of Occult Lymph Node Involvement in Small HER2-Positive Early Breast Cancer Treated by Up-Front Surgery. Cancers. 2023; 15(18):4567. https://doi.org/10.3390/cancers15184567
Chicago/Turabian StyleHouvenaeghel, Gilles, Monique Cohen, Marc Martino, Fabien Reyal, Jean-Marc Classe, Marie-Pierre Chauvet, Pierre-Emmanuel Colombo, Mellie Heinemann, Eva Jouve, Pierre Gimbergues, and et al. 2023. "Negative Survival Impact of Occult Lymph Node Involvement in Small HER2-Positive Early Breast Cancer Treated by Up-Front Surgery" Cancers 15, no. 18: 4567. https://doi.org/10.3390/cancers15184567
APA StyleHouvenaeghel, G., Cohen, M., Martino, M., Reyal, F., Classe, J.-M., Chauvet, M.-P., Colombo, P.-E., Heinemann, M., Jouve, E., Gimbergues, P., Azuar, A.-S., Coutant, C., Gonçalves, A., & de Nonneville, A. (2023). Negative Survival Impact of Occult Lymph Node Involvement in Small HER2-Positive Early Breast Cancer Treated by Up-Front Surgery. Cancers, 15(18), 4567. https://doi.org/10.3390/cancers15184567








